Abstract
Background
Forced expiratory volume in 1 second (FEV1) grades severity of COPD and predicts survival. We hypothesize that the inspiratory capacity/total lung capacity (IC/TLC) ratio, a sensitive measure of static lung hyperinflation, may have a significant association with survival in an emphysematous phenotype of COPD.
Objectives
To access the association between IC/TLC and survival in an emphysematous phenotype of COPD.
Methods
We performed a retrospective analysis of a large pulmonary function (PF) database with 39,050 entries, from April 1978 to October 2009. Emphysematous COPD was defined as reduced FEV1/forced vital capacity (FVC), increased TLC, and reduced diffusing capacity of the lungs for carbon monoxide (DLCO; beyond 95% confidence intervals [CIs]). We evaluated the association between survival in emphysematous COPD patients and the IC/TLC ratio evaluated both as dichotomous (≤25% vs >25%) and continuous predictors. Five hundred and ninety-six patients had reported death dates.
Results
Univariate analysis revealed that IC/TLC ≤25% was a significant predictor of death (hazard ratio [HR]: 2.39, P<0.0001). Median survivals were respectively 4.3 (95% CI: 3.8–4.9) and 11.9 years (95% CI: 10.3–13.2). Multivariable analysis revealed age (HR: 1.19, 95% CI: 1.14–1.24), female sex (HR: 0.69, 95% CI: 0.60–0.83), and IC/TLC ≤25% (HR: 1.69, 95% CI: 1.34–2.13) were related to the risk of death. Univariate analysis showed that continuous IC/TLC was associated with death, with an HR of 1.66 (95% CI: 1.52–1.81) for a 10% decrease in IC/TLC.
Conclusion
Adjusting for age and sex, IC/TLC ≤25% is related to increased risk of death, and IC/TLC as a continuum, is a significant predictor of mortality in emphysematous COPD patients.
Introduction
COPD represents an important public health challenge that is both treatable and preventable.Citation1 Currently, COPD is the fourth leading cause of death worldwide and is expected to be the third leading cause of death by 2020.Citation2 Despite efforts from the medical community, the Centers for Disease Control (CDC) reports that smoking rates in the US have only slightly declined since 1997 from 24.7% to 20.8%.Citation3 With COPD prevalence increasing, accurate assessments of COPD comorbidities and mortality are needed.Citation4–Citation25 COPD results from the interplay between genetic susceptibility and exposure to environmental stimuli.Citation26
In 1977, Fletcher and Peto described the natural history of COPD, including its relationship with smoking and decline in forced expiratory volume in 1 second (FEV1).Citation27 Since that time, COPD has been characterized as a poorly reversible airflow limitation, most often defined by FEV1.Citation8 Historically, the reduction in FEV1 has been used to define the severity of COPD and frequently cited as an important predictor of mortality.Citation24 Additionally, FEV1 is frequently targeted as a clinical endpoint in COPD clinical trials.Citation28–Citation34 Other clinical measurements such as inspiratory capacity (IC), 6-minute walk test (6MWT), the BODE index (body mass index, airflow obstruction, dyspnea, and exercise), and dyspnea questionnaires may have stronger associations with mortality than FEV1.Citation7,Citation12–Citation16,Citation19,Citation24,Citation35–Citation39
Several publications have focused on the use of the IC/total lung capacity (TLC) ratio, a measure of static lung hyperinflation, which has been shown to be strongly associated with exercise-associated dynamic hyperinflation as well as exercise tolerance.Citation4,Citation8,Citation38,Citation40 Additionally, studies evaluating the use of resting IC have also demonstrated a strong association between IC and functional exercise limitation in COPD patients.Citation41,Citation42 In 2004, Casanova et al evaluated the role of the IC/TLC ratio, in conjunction with the BODE index and FEV1.Citation7 Their cohort consisted of 689 patients (95% male) with 183 deaths (178 males and five females) with a median follow-up less than 3 years; their results suggested that when compared to FEV1 and the BODE index, an IC/TLC ratio of ≤25% offered the best combined sensitivity and specificity for predicting all-cause mortality in COPD patients.Citation7 We hypothesize that the IC/TLC ratio is associated with risk of death, when used to evaluate a large cohort over an extended period of follow-up and could be a useful clinical tool in assessing patients with an emphysematous phenotype of COPD.
Methods
We performed a retrospective analysis of a large pulmonary function (PF) database, consisting of 39,050 entries, from our institution, which encompasses a broad patient population of inpatients and outpatients from April 1978 to October 2009. Cedars-Sinai Medical Center Institutional Review Board approval (Pro-00012916) was obtained for the study. We evaluated the IC/TLC ratio and its association with survival. All available studies were evaluated, which consisted of 39,050 entries. We defined COPD patients with an emphysematous phenotype as those with a reduced FEV1/FVC ratio, increased TLC, and reduced diffusing capacity of the lungs for carbon monoxide (DLCO; all beyond 95% confidence intervals) using established normal values.Citation42–Citation44 If the same patient had multiple PF studies, only the first recorded PF was included in the study analysis. Lastly, patients were excluded if they were under the age of 18 years. Using the Social Security National Death Index (SSNDI), we established absolute dates of death. If the subject did not have a reported date of death in the SSNDI, they were assumed to be alive 8 weeks prior to the date that the SSNDI was queried. Univariate analysis was completed to evaluate the relationship between IC/TLC ratio and survival. Additionally, disease severity was graded using the FEV1 as defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.Citation46 Body mass index (BMI) was treated as ordered categories (BMI: <20 low, ≥20–25 normal, ≤25 overweight/obese). As done previously in the NETT trial, DLCO was treated as a binary variable, with a cut-off of <22%.Citation47 Finally, multivariable analysis assessing the associations of age, sex, FEV1, DLCO, IC, and BMI in conjunction with the IC/TLC ratio was performed. All studies were performed on equipment manufactured by the SensorMedics Corporation. IC measurements were made during the enhanced spirometry section with deep inspiration occurring after a period of stable tidal breathing; all tests were performed according to the American Thoracic Society (ATS) criteria. Single-breath DLCO measurements were made according to ATS criteria with a 10-second breath-hold; correction for hemoglobin was not performed. TLC was measured using plethysmography as per ATS criteria. Forced expiratory spirometry was obtained pre- and post-spirometry; plethysmography was obtained post-bronchodilator.
Numerical variables were summarized by mean and standard deviation or median and interquartile range (IQR), as appropriate, depending on the normality of the distribution. Group differences on numerical variables were assessed by Student’s t-tests (normality was satisfied) or the Wilcoxon rank-sum test (normality was violated). Categorical variables were summarized by frequency and percentage and compared across groups by the chi-square test or Fisher’s exact test, as appropriate. Survival was estimated by the Kaplan–Meier method. Group differences in survival were assessed by the log-rank test. Survival differences across ordinal explanatory variables were assessed by trend tests. Factors associated with the risk of death were assessed by multivariable Cox proportional hazards models. The proportional hazards assumption was assessed by the supremum test and by analysis of Schoenfeld residuals. Hazard ratios (HRs) and their associated 95% CIs were reported where possible. Two-sided P-values were reported for all comparisons. Statistical calculations were made using SAS software (v9.1.3; SAS Institute Inc., Cary, NC, USA).
Results
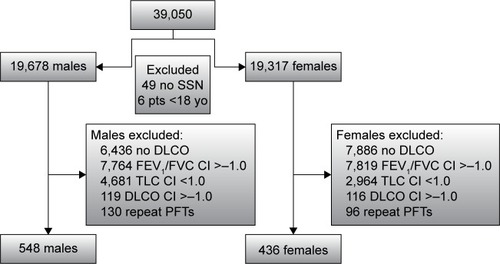
Our database consisted of 39,050 PF tests; 14,322 were excluded because they had no DLCO recorded. The remaining 24,728 PFs that were excluded, either did not meet criteria for obstruction or were repeat PF tests. Nine-hundred and eighty-four patient PFs meeting criteria were analyzed (). The study cohort consisted of 436 females and 548 males. Five hundred and ninety-six subjects had reported dates of death.
Figure 1 Patient flow chart.
Baseline characteristics are reported in . As displayed in , there were notable differences between the ‘dead’ and ‘alive’ groups. ‘Alive’ patients were younger, had a higher BMI, a higher FEV1/FVC ratio, and higher predicted FEV1 with a larger percentage being defined as having mild COPD. In regards to lung volumes, ‘alive’ patients had a slightly lower TLC, higher DLCO, higher IC, and had better IC/TLC ratios than patients in the ‘dead’ group.
Table 1 Baseline characteristics and univariate analysis
The potential predictors of all-cause mortality are shown in and .
Table 2 Univariate analysis
Table 3 Multivariable analysis
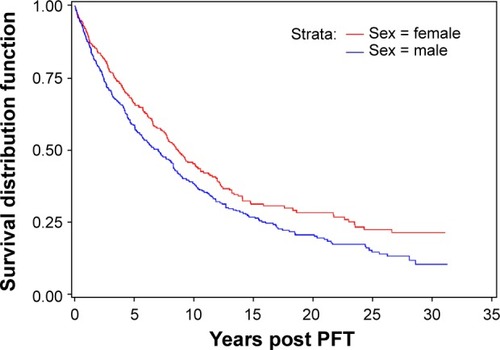
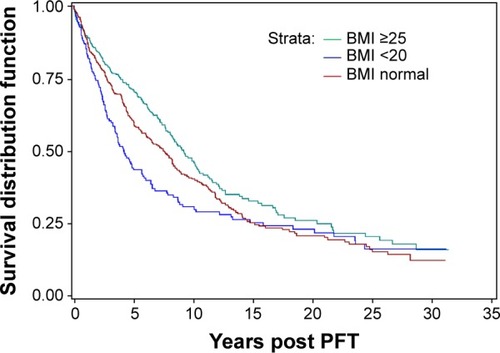
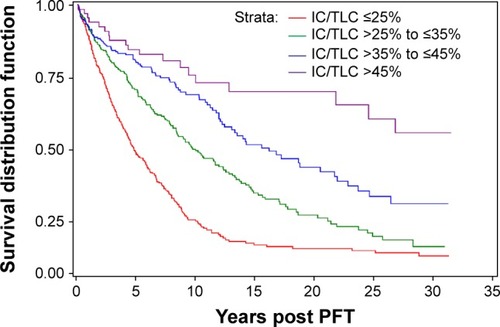
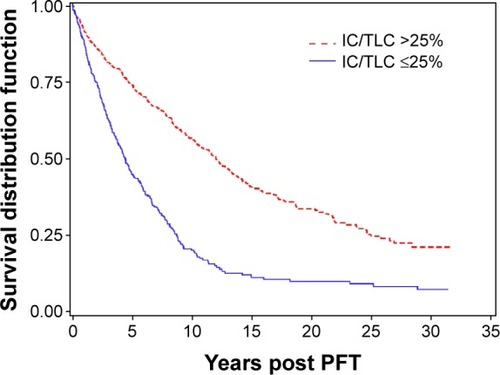
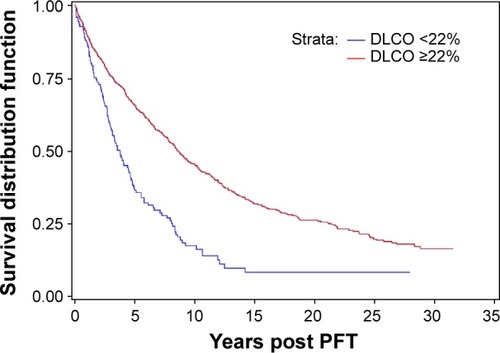
Univariate analysis revealed that IC/TLC, % DLCO, sex, age, BMI, IC, and FEV1 were all significantly associated with survival (; , , and ). Using an IC/TLC ≤25% compared to IC/TLC >25%, there was a significant decrease in survival (HR: 2.39, 95% CI: 2.03–2.82, P<0.0001). The median survival was 4.3 years for IC/TLC ≤25% (95% CI: 3.8–4.9 years) versus 11.9 years for IC/TLC >25% (95% CI: 10.3–13.2 years). Five-year survival for IC/TLC ≤25% versus IC/TLC >25% was 43.9% (95% CI: 38.7%–49.0%) versus 73.4% (95% CI: 69.6%–76.9%), respectively. Additionally, a DLCO <22% versus a DLCO ≥22% was associated with an increased risk of death (HR: 2.08, 95% CI: 1.68–2.57, P<0.0001). The median survival for a DLCO <22% was 3.77 years (95% CI: 2.94–4.60 years). Females had reduced risk of death (HR: 0.78, 95% CI: 0.66–0.92, P=0.003). Median survival for females was 8.7 years (95% CI: 7.7–10.1 years) versus 7.0 years for males (95% CI: 5.7–8.2 years). A 5-year increase in age revealed a 23% increased risk of death (HR: 1.23, 95% CI: 1.18–1.28, P<0.0001). Compared to a normal BMI (≥20 to <25, the reference level), patients with a BMI <20 were at greater risk of death (HR: 1.22, 95% CI: 0.99–1.51, P=0.068). However, a BMI ≥25 appeared to be protective (HR: 0.81, 95% CI: 0.67–0.97, P=0.022). An IC ≥80% was associated with a reduced risk of death (HR: 0.48, 95% CI: 0.41–0.57, P<0.0001). Lastly, FEV1 was evaluated using moderate COPD disease, as defined by GOLD criteria, as the reference group: patients with mild COPD were less likely to die (HR: 0.48, 95% CI: 0.35–0.65, P<0.001); however, both severe (HR: 1.38, 95% CI: 1.11–1.70, P=0.003) and very severe COPD (HR: 1.81, 95% CI: 1.46–2.23, P<0.0001) patients were at increased risk of death.
Figure 2 Survival by predicted FEV1 level as defined by GOLD criteria.
Abbreviations: FEV1, forced expiratory volume in 1 second; GOLD, Global Initiative for Chronic Obstructive Lung Disease; PFT, pulmonary function test.
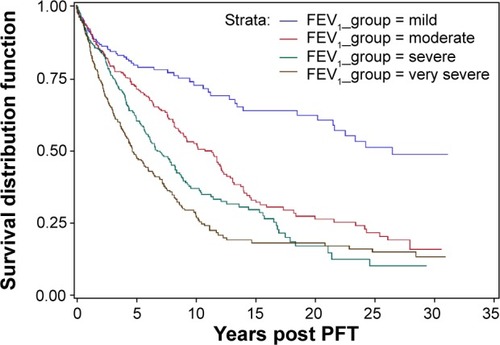
Figure 3 Patient survival by IC/TLC.
Abbreviations: IC, inspiratory capacity; TLC, total lung capacity; PFT, pulmonary function test.
In addition, a multivariable analysis was preformed to assess the associations of age, sex, FEV1, % DLCO, IC, and BMI in conjunction with the IC/TLC ratio. Analysis revealed that age (5-year increase in age), sex, IC/TLC ≤25%, FEV1, BMI <20, and DLCO <22% remained statistically significant factors associated with the risk of death (). Patients with a DLCO <22% had an increased risk of death when compared to patients with a DLCO ≥22% (HR: 1.28, 95% CI: 1.01–1.61, P=0.043) (). Compared to a normal BMI (≥20 to <25, the reference level), patients with a BMI <20 were at greater risk of death (HR: 1.22, 95% CI: 0.97–1.53, P=0.089). In contrast, a BMI ≥25 appeared to be protective (HR: 0.81, 95% CI: 0.67–0.97, P=0.022) (). Lastly, FEV1 was evaluated using moderate COPD disease, as defined by GOLD criteria, as the reference group. Patients with mild COPD were less likely to die (HR: 0.66, 95% CI: 0.48–0.90, P=0.009). Additionally, neither severe (HR: 1.01, 95% CI: 0.80–1.27, P=0.95) nor very severe COPD (HR: 1.06, 95% CI: 0.79–1.41, P=0.71) patients were at increased risk of death, compared to the moderate group in the multivariate analysis. In summary, increasing age, IC/TLC ≤25%, DLCO <22%, and a BMI <20 were associated with increased risk of death. Female sex and a higher BMI were protective.
Figure 5 Patient survival by DLCO.
Abbreviations: DLCO, diffusing capacity of the lungs for carbon monoxide; PFT, pulmonary function test.
Lastly, we completed a univariate analysis of the IC/TLC ratio as a continuous predictor of the risk of death. Over the entire range of IC/TLC (8%–63%), a 10% decrease in IC/TLC was associated with a 66% increase in the risk of death (HR: 1.66, 95% CI: 1.52–1.81, P<0.0001). For clinical applicability, we categorized the ratio into four levels: IC/TLC >45% (the reference level), >35% to ≤45%, >25% to ≤35%, and ≤25% (; ). Compared to patients with IC/TLC >45%, patients with IC/TLC >35% to ≤45% were at 76% increased risk of death (HR: 1.76, 95% CI: 1.07–2.89); patients with IC/TLC >25% to ≤35% were at 182% increased risk of death (HR: 2.82, 95% CI: 1.76–4.53); and patients with IC/TLC ≤25% were at 423% increased risk of death (HR: 5.23, 95% CI: 3.28–8.35). Median survivals (95% CI) were 4.3 (3.8–4.9) years for patients with IC/TLC ≤25%, 8.9 (7.7–10.5) years for patients with IC/TLC >25% to ≤35%, and 14.1 (11.9–18.7) years for patients with IC/TLC >35% to ≤45%. Median survival was not yet reached in patients with IC/TLC >45% (30-year survival estimate 52.3%).
Table 4 IC/TLC ratio in levels
Discussion
Using an IC/TLC ratio of ≤25%, a representation of static lung hyperinflation, we were able to demonstrate that the IC/TLC ratio correlated with risk of death in patients with an emphysematous phenotype of COPD. Patients with an IC/TLC ratio ≤25% had a median survival of 4.3 years versus 11.9 years for those patients with an IC/TLC ≤25%. The use of the IC/TLC ratio, as a single predictor variable, in patients with COPD, will allow clinicians to better evaluate and risk-stratify patients with an emphysematous phenotype of COPD.
In the 35 years since Fletcher and Peto described the natural history of COPD, our understanding about the disease process has been an ongoing development.Citation27 Although initial studies supported FEV1 as the best predictor of COPD mortality,Citation47 more recent literature has revealed that a variety of factors are more accurate predictors of mortality than FEV1.Citation7,Citation12–Citation16,Citation19,Citation24,Citation34–Citation39 Interest has been shown in the role of the vitamin D pathway in COPD, with vitamin D deficiency correlating with the risk of COPD.Citation26
In addition to IC/TLC and FEV1, we also examined the relationship of IC, age, BMI, DLCO, and sex ( and ) and their associations with the risk of death. Specifically, our multivariable analysis demonstrated that IC alone was not a reliable predictor of mortality, contrary to what has been previously reported in a milder COPD population.Citation24 We were able to demonstrate that age and BMI were associated with risk of death but did not demonstrate as clear an association as the IC/TLC. In regards to sex, Kaplan–Meier analysis revealed that females had a survival advantage when compared directly to males with COPD. Ringbaek et al previously reported that when compared to standardized mortality rates expected in the general population, it appeared that females with COPD actually have more years of life lost than their male counterparts.Citation21 Furthermore, when examining the DLCO, we found a significant association with risk of death. However, our cohort had only 126 patients with a DLCO ≤22%.
Our study had a number of strengths. To our knowledge, it is the first study to evaluate mortality over 34 years of reported data in an emphysematous phenotype of COPD. Additionally, our cohort consisted of 44.3% (436) females, and to date, is one of the largest cohorts of females used to evaluate COPD mortality. We used an easily identifiable IC/TLC cut-off of 25%, which has previously been validated.Citation7
The study does have limitations. It is a PF test-based study, assumptions about the patients’ clinical phenotype were made on the basis of PF data, and no smoking history or radiological data were available. We did not evaluate or compare the BODE index or 6MWT. On the other hand, we did evaluate other well-defined variables including age, BMI, and FEV1 in the analysis. We did not have PaO2 values, therefore could not evaluate/correlate the degree of hypoxemia and its role in survival. The study inclusion criteria required a DLCO for the patient to be included in the analysis. In doing so, we eliminated patients who may have obstructive disease secondary to asthma, but undoubtedly removed many patients with COPD. We did not evaluate specific cause of death as previous studies have done, which prevented us from excluding patients that died from nonrespiratory events.
Our study demonstrates that the IC/TLC ratio ≤25% is strongly related to risk of death in an emphysematous phenotype of COPD patients. When compared to FEV1 and other previously accepted variables, IC/TLC was a better predictor of survival in both univariate and multivariate analysis. Specifically, we found FEV1 to be weakly associated with survival. When using patients with moderate severity as the reference group, those patients with mild disease were noted to have improved survival. Patients with severe and very severe disease did not have a statistically significant difference in mortality when compared to those individuals with moderately severe disease.
We believe that the reduced IC/TLC ratio, reflective of static lung hyperinflation, plays an important role in patients with an emphysematous phenotype of COPD. As hyperinflation progresses, patients experience increasing dyspnea and reduced exercise capacity. Dynamic lung hyperinflation is associated with increasing end-expiratory lung volumes, which is associated with airflow limitation and loss of elastic recoil. In COPD, emphysematous changes in the lung are secondary to destruction of the elastic tissue in the lung parenchyma. As the lung parenchyma loses it elasticity, lung recoil is reduced, resulting in a compensatory increase in functional reserve capacity (FRC); as the FRC increases, the IC is reduced.Citation49 Therefore, in patients with COPD, the relationship between IC and TLC gradually declines as static lung hyperinflation increases. We found that the IC/TLC ratio strongly correlates with risk of death. In addition to risk of death, static lung hyperinflation has been reported to correlate with exercise capacity and cardiac performance in patients with COPD, thus adding to the clinical use of the IC/TLC ratio.
Previous studies of COPD patients often refer to the FEV1 and its rate of decline to define treatment success or failure. Current treatment guidelines are based on the GOLD-defined FEV1, an endpoint that we found to have little correlation with survival. We believe that the IC/TLC ratio may be a more relevant variable for such analysis, possible arguing for further studies.
In conclusion, a significant number of COPD patients have PF tests that include measurement of lung volumes. The IC/TLC ratio, like the BODE index, has demonstrated a correlation with COPD survival, is easy to obtain, and should be considered in the assessment of patients with an emphysematous phenotype of COPD.
Disclosure
The authors report no conflicts of interest in this work.
References
- Centers for Disease Control and Prevention (CDC)Deaths from chronic obstructive pulmonary disease United States, 2000–2005MMWR Morb Mortal Wkly Rep200857451229123219008792
- XuJQKochanekKDMurphySLTejeda-VeraBDeaths: Final Data for 2007 National Vital Statistics Reports5819Hyattsville, MDNational Health Center for Health Statistics2010 Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_19.pdfAccessed January 20, 2015
- Centers for Disease Control and Prevention (CDC)Cigarette smoking among adults – United States, 2006MMWR Morb Mortal Wkly Rep200756441157116117989644
- AlbuquerqueALNeryLEVillaçaDSInspiratory fraction and exercise impairment in COPD patients with GOLD stages II–IIIEur Respir J200628593994416870665
- BourdinABurgelPRChanezPGarciaGPerezTRocheNRecent advances in COPD: pathophysiology, respiratory physiology and clinical aspects, including comorbiditiesEur Respir J200918114198212
- CalverlyPMAndersonJACelliBTORCH investigatorsSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med200735677578917314337
- CasanovaCCoteCMarinJMDistance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPDChest2008134474675218625667
- CasanovaCCoteCde TorresJPInspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171659159715591470
- Soler-CataluñaJJMartínez-GarcíaMARomán SánchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- CelliBRVestboJJenkinsCRInvestigators of the TORCH StudySex differences in mortality and clinical expressions of patients with chronic obstructive pulmonary disease. The TORCH experienceAm J Respir Crit Care Med2011183331732220813884
- CelliBRDecramerMKestenSLiuDMehraSTashkinDPUPLIFT Study InvestigatorsMortality in the 4-year trial of tiotropium (UPLIFT) in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20091801094895519729663
- CelliBartolome RPredictors of mortality in COPDRespir Med201010477377920417082
- CoteCGPinto-PlataVKasprzykKDordellyLJCelliBRThe 6-min walk distance, peak oxygen uptake, and mortality in COPDChest200713261778178517925409
- FanVSCurtisJRTuSPMcDonellMBFihnSDAmbulatory Care Quality Improvement Project InvestigatorsUsing quality of life to predict hospitalization and mortality in patients with obstructive lung diseasesChest2002122242943612171813
- MartinezFJFosterGCurtisJLNETT Research GroupPredictors of mortality in patients with emphysema and severe airflow obstructionAm J Respir Crit Care Med2006173121326133416543549
- NishimuraKIzumiTTsukinoMOgaTDyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPDChest200212151434144012006425
- OgaTNishimuraKTsukinaMHealth status measured with the CRQ does not predict mortality in COPDEur Respir J20022051147115112449167
- OgaTNishimuraKTsukinoMSatoSHajiroTAnalysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health statusAm J Respir Crit Care Med2003167454454912446268
- Pinto-PlatoVMCoteCCabralHTaylorJCelliBRThe 6-min walk distance: change over time and value as a predictor of survival in severe COPDEur Respir J2004231283314738227
- SabinoPGSilvaBMBrunettoAFNutritional status is related to fat-free mass, exercise capacity and inspiratory strength in severe chronic obstructive pulmonary disease patientsClinics (Sao Paulo)201065659960520613936
- RingbaekTSeersholmNViskumKStandardised mortality rates in females and males with COPD and asthmaEur Respir J200525589189515863648
- SinDDAnthonisenNRSorianoJBAgustiAGMortality in COPD: role of comorbiditiesEur Respir J20062861245125717138679
- SinDDWuLAndersonJAInhaled corticosteroids and mortality in chronic obstructive pulmonary diseaseThorax2005601299299716227327
- TantucciCDonatiPNicosiaFInspiratory capacity predicts mortality in patients with chronic obstructive pulmonary diseaseRespir Med2008102461361918083020
- de TorresJPCoteCGLópezMVSex differences in mortality in patients with COPDEur Respir J200933352853519047315
- DecramerMJanssensWMiravitllesMChronic obstructive pulmonary diseaseLancet201237998231341135122314182
- FletcherCPetoRThe natural history of chronic airflow obstructionBMJ19771607716451648871704
- JenkinsCRJonesPWCalverleyPMEfficacy of salmeterol/fluticasone by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH studyRespir Res2009105919566934
- CelliBRThomasNEAndersonJAEffects of pharmacotherapy on rate of decline of lung function in chronic obstructive pulmonary disease: results from the TORCH studyAm J Respir Crit Care Med2008178433233818511702
- DecramerMCelliBRKestenSLystigTMehraSTashkinDPUPLIFT investigatorsEffect of triotropium on outcomes in patients with moderate chronic obstructive pulmonary disease (UPLIFT): a prespecified subgroup analysis of a randomised controlled trialLancet200937496961171117819716598
- GanWQManSFSenthilselvanASinDDAssociation between chronic obstructive pulmonary disease and systemic inflammation: a systemic review and a meta-anaylsisThorax200459757458015223864
- MiravitllesMAnzuetoAInsights into interventions in managing COPD patients: lessons from the TORCH and UPLIFT studiesInt J Chron Obstruct Pulmon Dis2009418520119516917
- SorianoJBSinDDZhangXA pooled analysis of FEV1 decline in COPD patients randomized to inhaled corticosteroids or placeboChest2007131368268917356080
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- GlaabTVogelmeierCBuhlROutcome measures in chronic obstructive pulmonary disease (COPD): strengths and limitationsRespir Res2010117920565728
- FreitasCGPereiraCAViegasCAInspiratory capacity, exercise limitations, markers of severity, and prognostic factors in chronic obstructive pulmonary diseaseJ Bras Pneumol200733438939617982530
- LandboCPrescottELangePVestboJAlmdalTPPrognostic value of nutritional status in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199916061856186110588597
- MarinJMCarrizoSJGasconMSanchezAGallegoBCelliBRInspiratory capacity, dynamic hyperinflation, breathlessness, and exercise performance during the 6-minute-walk test in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200116361395139911371407
- PuhanMAGarcia-AymerichJFreyMExpansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO indexLancet2009374969170471119716962
- VassauxCTorre-BouscouletLZeineldineSEffects of hyperinflation on the oxygen pulse as a marker of cardiac performance in COPDEur Respir J20083251275128218550609
- DiazOVillafrancaCGhezzoHRole of inspiratory capacity on exercise tolerance in COPD patients with and without tidal expiratory flow limitations at restEur Respir J200016212561276
- O’DonnellDERevilleSMWebbKADynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2001164577077711549531
- CrapoROMorrisAHClaytonPDNixonCRLung volumes in healthy nonsmoking adultsBull Eur Physiopathol Respir19821834194257074238
- MillerAThortonJCWarshawRAndersonHTeirsteinASSelikoffIJSingle breath diffusing capacity in a representative sample of the population of Michigan, a large industrial state. Predicted values, lower limits of normal, and frequencies of abnormality by smoking historyAm Rev Respir Dis198312732702776830050
- PauwelsRABuistASCalverleyPMJenkinsCRHurdSSGOLD Scientific CommitteeGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summaryAm J Respir Crit Care Med200116351256127611316667
- Rationale and Design of The National Emphysema Treatment Trial: a prospective randomized trial of lung volume reduction surgery. The National Emphysema Treatment Trial Research GroupChest199911661750176110593802
- AnthonisenNRSkeansMAWiseRAManfredJKannerREConnettJELung Health Study Research GroupThe effects of smoking cessation intervention on 14.5-year mortalityAnn Intern Med2005142423323915710956
- FergusonGTWhy does the lung hyperinflate?Proc Am Thorac Soc20063217617916565428
- National Heart, Lung, and Blood InstituteGlobal Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease: NHLBI/NIH Workshop ReportBethesda, MDNational Heart, Lung, and Blood Institute2001 Available from: http://www.goldcopd.org/uploads/users/files/GOLDWkshp2001pdfAccessed January 20, 2015