 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Cardiovascular diseases, osteoporosis, and depression are identified comorbidities of chronic obstructive pulmonary disease (COPD), but there have been few reports of chronic kidney disease (CKD) as a comorbidity of COPD. The objective of this study was to investigate the prevalence of CKD in COPD patients using estimated glomerular filtration rate (eGFR) based on creatinine (Cr) and cystatin C (Cys) levels.
Methods
The prevalence of CKD and the values of various CKD-related parameters were compared between 108 stable COPD outpatients (COPD group) and a non-COPD control group consisting of 73 patients aged 60 years or more without a history of COPD or kidney disease. CKD was defined as an eGFR less than 60 mL/min/1.73 m2.
Results
The Cr level was significantly higher in the COPD group, but eGFR based on serum Cr (eGFRCr) was not significantly different between the two groups (73.3±25.3 vs 79.7±15.5 mL/min/1.73 m2). The Cys level was significantly higher and eGFR based on serum Cys (eGFRCys) was significantly lower in the COPD group (60.0±19.4 vs 74.0±13.5 mL/min/1.73 m2, P<0.0001). The prevalence of CKD evaluated based on eGFRCr was 31% in the COPD group and 8% in the non-COPD group with an odds ratio of 4.91 (95% confidence interval, 1.94–12.46, P=0.0008), whereas the evaluated prevalence based on eGFRCys was 53% in the COPD group and 15% in the non-COPD group with an odds ratio of 6.30 (95% confidence interval, 2.99–13.26, P<0.0001), demonstrating a higher prevalence of CKD when based on eGFRCys rather than on eGFRCr.
Conclusion
CKD is a comorbidity that occurs frequently in COPD patients, and we believe that renal function in Japanese COPD patients should preferably be evaluated based not only on Cr but on Cr in combination with Cys.
Keywords:
Introduction
Chronic obstructive pulmonary disease (COPD) is a systemic disease with various comorbidities and is associated with underlying systemic inflammation.Citation1–Citation3 Because the comorbidities of COPD affect disease severity and prognosis, the screening and treatment of comorbidities are key to the control of COPD.Citation4,Citation5 Cardiovascular diseases (CVD), osteoporosis, and depression are considered to be representative comorbidities of COPD,Citation6 but chronic kidney disease (CKD) has been minimally investigated in this context. Advanced age and smoking as well as COPD are risk factors for CKD, which is also known to be an important risk factor for CVD.Citation7–Citation10
A recent report that a high rate of microalbuminuria was detected in COPD patients has focused attention on the correlation between COPD and CKD. It has also been pointed out that CKD may be missed if, in elderly COPD patients with decreased muscle mass, the diagnosis is based on creatinine (Cr) levels alone.Citation11–Citation16 Cystatin C (Cys) has attracted attention as a biomarker that reflects early renal dysfunction,Citation17–Citation21 and a formula to determine the estimated glomerular filtration rate (eGFR) based on Cys levels has been proposed in addition to the conventional estimation formula based on Cr levels.Citation22,Citation23 The Japanese Society of Nephrology adopted this new estimation formula in 2012.Citation24,Citation25 In this study, we measured both serum Cr and serum Cys levels to investigate the prevalence of CKD in COPD patients from the perspective of renal function.
Subjects and methods
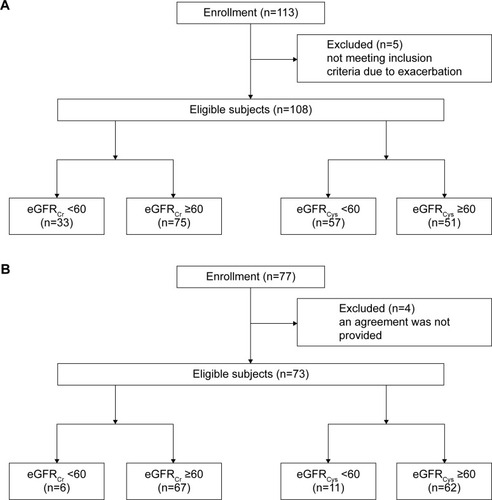
In this study, 108 stable COPD outpatients who visited our hospital between May 2011 and April 2012 were compared with a non-COPD control group consisting of 73 outpatients (who visited our hospital during the same period) aged 60 years or more who did not have a history of COPD or kidney disease (). Written informed consent was obtained from all subjects of this study. Levels of hemoglobin, blood urea nitrogen, Cr, Cys, and brain natriuretic peptide were evaluated. CKD was defined as an eGFR of less than 60 mL/min/1.73 m2. COPD was diagnosed based on spirometry when the FEV1/FVC was less than 70% after inhalation of a bronchodilator, and the severity of airflow obstruction was judged according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.Citation6 eGFR was calculated based on serum Cr and serum Cys levels using the following estimation formulas adopted by the Japanese Society of Nephrology in 2012:
eGFR based on serum Cr (eGFRCr) level:
(1)
(2)
eGFR based on serum Cys (eGFRCys) level:
(3)
(4)
Figure 1 Consolidated standards of reporting trials flowchart.
Abbreviations: COPD, chronic obstructive pulmonary disease; eGFRCr, estimated glomerular filtration rate based on Cr (mL/min/1.73 m2); eGFRCys, estimated glomerular filtration rate based on Cys (mL/min/1.73 m2).
For statistical analyses, the t-test and Fisher’s exact test were used as intergroup tests, and the correlation between the prevalence of CKD and the severity of airflow obstruction was tested using the Cochran–Armitage trend test. The odds ratio between the COPD group and the non-COPD group was calculated with regard to the prevalence of CKD. A P-value of <0.05 was considered statistically significant. This study was approved by the Ethics Committee of the Kanamecho Hospital (approval number 1110). The study was registered with the following registration identification: R000017166 on August 10, 2014.
Results
Patient characteristics are summarized in . The COPD group had significantly higher mean age (74.3±7.1 [COPD] vs 71.8±7.3 [non-COPD] years, P=0.0214), more male patients (P<0.0001), and a longer smoking history (P<0.0001) than the non-COPD group. Body-mass index (BMI) was significantly lower in the COPD group (21.1±3.1 vs 23.7±2.4 kg/m2, P<0.0001). Regarding comorbidities, the prevalence of hypertension, diabetes mellitus, and dyslipidemia were significantly higher in the non-COPD group, but the prevalence of CVD and bronchial asthma were significantly higher in the COPD group. Biochemical testing indicated significantly higher levels of blood urea nitrogen, Cr, Cys, and brain natriuretic peptide in the COPD group (). The eGFR did not significantly differ between the two groups when estimated using the formula based on serum Cr (eGFRCr, 73.3±25.3 vs 79.7±15.5 mL/min/1.73 m2), but the eGFR was significantly lower in the COPD group when estimated using the formula based on serum Cys (eGFRCys, 60.0±19.4 vs 74.0±13.5 mL/min/1.73 m2, P<0.0001). The prevalence of CKD, which was defined as an eGFR less than 60 mL/min/1.73 m2, was 31% (33 of 108 patients) in the COPD group and 8% (six of 73 patients) in the non-COPD group (see ) when evaluated with eGFRCr, indicating a significantly higher prevalence of CKD in the COPD group (P=0.0004) with an odds ratio of 4.91 (95% confidence interval, 1.94–12.46, P=0.0008). When evaluated with eGFRCys, the prevalence of CKD was 53% (57 of 108 patients) in the COPD group and 15% (eleven of 73 patients) in the non-COPD group, indicating a significantly higher prevalence in the COPD group (P<0.0001) with an odds ratio of 6.30 (95% confidence interval, 2.99–13.26, P<0.0001). Note that the prevalence evaluated with eGFRCys was higher than that evaluated with eGFRCr. No significant correlation was found between the severity of airflow obstruction and the prevalence of CKD in the COPD group ().
Table 1 Patient characteristics
Table 2 Blood biochemistry and estimated glomerular filtration rates
Table 3 Prevalence of CKD in the COPD patient group and the non-COPD patient group
Table 4 Prevalence of CKD by GOLD classification
Discussion
CKD, a concept that includes all chronic kidney damage or dysfunction, regardless of the primary disease, was proposed by the National Kidney Foundation in the USA in 2002. CKD is defined as the persistence of a decline in renal function to a glomerular filtration rate (GFR) less than 60 mL/min/1.73 m2 or findings that suggest renal impairment (eg, proteinuria) for 3 months or more. It has been reported that the prognosis of CKD depends on the primary disease and that CKD is an important risk factor for CVD.Citation26
CKD has risk factors in common with COPD, such as smoking and advanced age, and it has been pointed out that CKD is associated with underlying chronic inflammation. In addition, CKD has many characteristics in common with COPD, such as dependence of patient prognosis on CVD as a comorbidity. Although CKD has not attracted much attention as a comorbidity of COPD, there have recently been several reports showing that chronic renal failure (CRF) and microalbuminuria occur at a high rate in COPD patients, suggesting a correlation between COPD and CKD.Citation11–Citation16
Past studies have evaluated CKD based on Cr levels and microalbuminuria, but no study to date has evaluated CKD based on Cys. Whereas Cr is a byproduct of muscle metabolism, Cys is a low-molecular-weight protein secreted from nucleated cells throughout the body. Cys is filtered by the renal glomeruli without forming complexes and is mostly reabsorbed and metabolized in the renal proximal tubule. Serum Cys concentration is known to increase as a reflection of early renal impairment, and thus Cys has attracted attention as an intrinsic marker for the detection of early renal impairment; this approach has the advantage that Cys levels are not affected by muscle mass.Citation17–Citation21 The Japanese Society of Nephrology recommends eGFRCys over eGFRCr as an index reflecting the early reduction of renal function in patients with low muscle mass.
In the present study, eGFR did not differ between the COPD group and the non-COPD group when using the estimation formula based on serum Cr (eGFRCr), but the COPD group had significantly reduced eGFR when the estimation formula based on serum Cys (eGFRCys) was used. The prevalence of CKD was 31% in the COPD group when evaluated with eGFRCr, but a higher prevalence of 53% was obtained when eGFRCys was used. Thus, the present results support the utility of eGFRCys over eGFRCr as an index of early reduction in renal function.
Incalzi et alCitation14 pointed out the possibility that many COPD patients suffer from concealed CRF, with Cr levels, and thus eGFRCr, remaining at normal levels. This can occur because, although the capacity of the kidneys to remove Cr is impaired, the patient’s reduced muscle mass results in a lower Cr production rate. They also reported that the prevalence of CRF was higher in the COPD group when elderly COPD patients aged 65 years or more were compared with age-matched outpatients as the control group. In their report, the prevalence of CRF in the COPD group was 43% when concealed CRF and overt CRF were combined, and was significantly higher than the prevalence in the control group (23.4%). In our results, when evaluated with eGFRCr, the CKD prevalence in the COPD group was 31%, which was lower than the 43% figure reported by Incalzi et al but when evaluated with eGFRCys, our prevalence rose to 53%, which was higher than that of the aforementioned study. Because BMI in the COPD patients examined by Incalzi et al (mean BMI: 27.4 kg/m2) was far higher than that in our patients (mean BMI: 21.1 kg/m2), it is possible that this difference in BMI contributed to the difference in prevalence. Given that the prevalence of CKD also increased from 8% to 15% in the non-COPD group when eGFRCys, rather than eGFRCr, was used in our study, it may be more accurate to use the estimation formula based on Cys when reduced renal function is evaluated in elderly Japanese patients with reduced skeletal muscle mass.
Because a greater proportion of elderly COPD patients have a lower BMI in Japan compared to that in the West, the presence of CKD may be underestimated if evaluation is based on Cr only, which is dependent on muscle mass. We thus consider it more appropriate to evaluate eGFR based on both Cr and Cys levels. It has been reported that the Cys is not affected by the skeletal muscle volume, but by the somatic fat volume. It has also been identified that adipocytes may secrete Cys, although the underlying molecular mechanism is still unclear. Therefore, the Cys and eGFRcys may be affected by adiposity and overestimated in obese individuals with an extremely high BMI,Citation23 and use of Cys for the evaluation of CKD in COPD patients may not be adequate in Western countries where obese patients are seen at a high frequency.
The diagnosis of CKD in COPD patients may be useful in several ways. For example, CKD is a risk factor for the development of CVD, a representative comorbidity of COPD, and the presence of CKD may be related to the prognosis of COPD patients.
In recent years, Cys has been regarded as an index of arteriosclerosis, and it has been reported that Cys levels correlate with the development of cardiovascular events and patient life expectancy as a factor independent of CKD.Citation27–Citation33 Kiyosue et alCitation31 studied patients who underwent coronary angiography and reported that severe coronary artery disease might be present in patients who were considered to be at low risk based on an eGFR calculated from serum Cr, but who had a high Cys level; they concluded that Cys is useful as a marker for the severity of coronary artery disease as well as a marker for CKD.
Furthermore, CKD may be partially involved in the mechanism of anemia, a comorbidity of COPD, via impaired erythropoietin production. CKD is known to result in impaired metabolism of bone and minerals, which may be correlated with osteoporosis in COPD patients.
A limitation of this study is that CKD was diagnosed based on eGFR calculated from serum Cr and serum Cys levels without an assessment of microalbuminuria or other parameters. We could not perform urine testing for microalbuminuria in all the patients for reasons related to insurance coverage. The morbidity of CKD might have increased if we had performed microalbuminuria measurement in all the patients. Age, BMI, and smoking history were not matched between COPD and non-COPD groups, although these factors may have an impact on the GFR. Moreover, the subjects included only outpatients at our hospital and the study was based on a single medical institution. It is possible that age and severity were biased due to the small number of subjects; it is therefore desirable that the prevalence of CKD as a comorbidity of COPD be investigated further in a multicenter study.
The results of this study indicate that CKD is a comorbidity that occurs at a high rate in COPD patients; it is important that the presence of CKD should not be missed because CKD may influence the treatment and prognosis of patients. It is possible that the prevalence of CKD will be underestimated if Japanese COPD patients are diagnosed based only on serum Cr levels, considering that most of these patients are of advanced age and have reduced skeletal muscle mass and low BMI. Thus, it is considered more appropriate to evaluate CKD based on serum Cys levels in Japanese COPD patients.
Author contributions
All authors contributed to the study design, collection and interpretation of data, preparation of manuscript drafts, and approved the final version of the manuscript to be published.
Disclosure
The authors report no conflict of interest in this study.
References
- AgustíAGNogueraASauledaJSalaEPonsJBusquestsXSystemic effects of chronic obstructive pulmonary diseaseEur Respir J200321234736012608452
- BarnesPJCelliBRSystemic manifestations and comorbidities of COPDEur Respir J20093351165118519407051
- SorianoJBVisickGTMuellerovaHPayvandiNHansellALPatterns of comorbidities in newly diagnosed COPD and asthma in primary careChest200512842099210716236861
- ManninoDMThornDSwensenAHolguinFPrevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPDEur Respir J200832496296918579551
- SinDDAnthonisenNRSorianoJBAgustiAGMortality in COPD: Role of comorbiditiesEur Respir J20062861245125717138679
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Updated 2010Global Initiative for Chronic Obstructive Lung Disease, Inc2010 [cited April 1, 2011]. Available from: http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdfAccessed April 1, 2011
- CooperRGEffect of tobacco smoking on renal functionIndian J Med Res2006124326126817085829
- McAlisterFAEzekowitzJTonelliMArmstrongPWRenal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort studyCirculation200410981004100914769700
- GoASChertowGMFanDMcCullochCEHsuCYChronic kidney disease and the risks of death, cardiovascular events, and hospitalizationN Engl J Med2004351131296130515385656
- ManjunathGTighiouartHIbrahimHLevel of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the communityJ Am Coll Cardiol2003411475512570944
- van GestelYRChoncholMHoeksSEAssociation between chronic obstructive pulmonary disease and chronic kidney disease in vascular surgery patientsNephrol Dial Transplant20092492763276719369691
- TerzanoCContiVDi StefanoFComorbidity, hospitalization, and mortality in COPD: results from a longitudinal studyLung2010188432132920066539
- CasanovaCde TorresJPNavarroJMicroalbuminuria and hypoxemia in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201018281004101020558625
- IncalziRACorsonelloAPedoneCChronic renal failure: a neglected comorbidity of COPDChest2010137483183719903974
- ChandraDStammJAPalevskyPMThe relationship between pulmonary emphysema and kidney function in smokersChest2012142365566222459775
- CorsonelloAAntonelli IncalziRPistelliRPedoneCBustacchiniSLattanzioFComorbidities of chronic obstructive pulmonary diseaseCurr Opin Pulm Med201117Suppl 1S21S2822209926
- HojsRBevcSAntolincBGorenjakMPuklavecLSerum cystatin C as an endogenous marker of renal function in the elderlyInt J Clin Pharmacol Res2004242–3495415689051
- CollEBoteyAAlvarezLSerum cystatin C as a new marker for noninvasive estimation of glomerular filtration rate and as a marker for early renal impairmentAm J Kidney Dis2000361293410873868
- DharnidharkaVRKwonCStevensGSerum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysisAm J Kidney Dis200240222122612148093
- YashiroMKamataTSegawaHKadoyaYMurakamiTMusoEComparisons of cystatin C with creatinine for evaluation of renal function in chronic kidney diseaseClin Exp Nephrol200913659860419585181
- HojsRBevcSEkartRGorenjakMPuklavecLSerum cystatin C as an endogenous marker of renal function in patients with mild to moderate impairment of kidney functionNephrol Dial Transplant20062171855186216524933
- HojsRBevcSEkartRGorenjakMPuklavecLSerum cystatin C-based formulas for prediction of glomerular filtration rate in patients with chronic kidney diseaseNephron Clin Pract20101142c118c12619887832
- VupputuriSFoxCSCoreshJWoodwardMMuntnerPDifferential estimation of CKD using creatinine- versus cystatin C-based estimating equations by category of body mass indexAm J Kidney Dis2009536993100119394726
- MatsuoSImaiEHorioMRevised equations for estimated GFR from serum creatinine in JapanAm J Kidney Dis200953698299219339088
- HorioMImaiEYasudaYWatanabeTMatsuoSCollaborators Developing the Japanese Equation for Estimated GFR. GFR estimation using standardized serum cystatin C in JapanAm J Kidney Dis201361219720322892396
- LeveyASde JongPECoreshJThe definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference reportKidney Int2011801172821150873
- SchiffrinELLipmanMLMannJFChronic kidney disease: effects on the cardiovascular systemCirculation20071161859717606856
- KoenigWTwardellaDBrennerHRothenbacherDPlasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rateClin Chem200551232132715563478
- ShlipakMGKatzRSarnakMJCystatin C and prognosis for cardiovascular and kidney outcomes in elderly persons without chronic kidney diseaseAnn Intern Med2006145423724616908914
- LeeMSaverJLHuangWHChowJChangKHOvbiageleBImpact of elevated cystatin C level on cardiovascular disease risk in predominantly high cardiovascular risk populations: a meta-analysisCirc Cardiovasc Qual Outcomes20103667568320923994
- KiyosueAHirataYAndoJPlasma cystatin C concentration reflects the severity of coronary artery disease in patients without chronic kidney diseaseCirc J201074112441244720921817
- PeraltaCAKatzRSarnakMJCystatin C identifies chronic kidney disease patients at higher risk for complicationsJ Am Soc Nephrol201122114715521164029
- DammanKvan der HarstPSmildeTDUse of cystatin C levels in estimating renal function and prognosis in patients with chronic systolic heart failureHeart201298431932422038544
