Abstract
Background
The objective of the study is to develop a scoring system for predicting a 90-day re-exacerbation in hospitalized patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD).
Methods
A total of 176 consecutive hospitalized patients with AECOPD were included. The sociodemographic characteristics, status before acute exacerbation (AE), presentations of and treatment for the current AE, and the re-exacerbation in 90 days after discharge from hospital were collected.
Results
The re-exacerbation rate in 90 days was 48.9% (86 out of 176). It was associated with the degree of lung function impairment (Global initiative for chronic Obstructive Lung Disease [GOLD] grades), frequency of AE in the previous year, and parameters of the current AE, including pleural effusion, use of accessory respiratory muscles, inhaled long-acting β-2-agonists, inhaled corticosteroids, controlled oxygen therapy, noninvasive mechanical ventilation, and length of hospital stay, but was not associated with body mass index, modified Medical Research Council scale, or chronic obstructive pulmonary disease assessment test. A subgroup of ten variables was selected and developed into the re-exacerbation index scoring system (age grades, GOLD grades, AE times in the previous year, pleural effusion, use of accessory respiratory muscles, noninvasive mechanical ventilation, controlled oxygen therapy, inhaled long-acting β-2-agonists and inhaled corticosteroids, and length of hospital stay). The re-exacerbation index showed good discrimination for re-exacerbation, with a C-statistic of 0.750 (P<0.001).
Conclusion
A comprehensive assessment integrating parameters of stable chronic obstructive pulmonary disease, clinical presentations at exacerbation, and treatment showed a strong predictive capacity for short-term outcome in patients with AECOPD. Further studies are required to verify these findings.
Introduction
Chronic obstructive pulmonary disease (COPD) is one of major health care issues worldwide and is associated with high social and economic burdens, which will continue to increase until 2030.Citation1 Clinically, exacerbations are the most important events in the history of the disease. Although many individual factors are reported to be associated with an increased long-term mortality in patients with COPD, the multidimensional index, such as the BODECitation2 (body mass index [BMI], airflow obstruction, dyspnea, and exercise capacity), BODEXCitation3 (BMI, airflow obstruction, dyspnea, and previous severe exacerbations), ADOCitation4 (age, dyspnea, and airflow obstruction), and DOSECitation5 (dyspnea, airflow obstruction, smoking status, and exacerbation frequency), has improved the prognostic capacity beyond individual variables. However, to our knowledge, few studies have demonstrated prognostic value in the short term after an acute exacerbation of chronic obstructive pulmonary disease (AECOPD) except CODEX (comorbidity, obstruction, dyspnea, and previous severe exacerbations).
CODEX was designed to predict mortality and hospital readmission in 3–12 months after discharge of patients hospitalized for AECOPD.Citation6 It did not include the clinical severity parameters and the treatment in exacerbation, which could be important to evaluate the short-term risk for relapse of the disease. Roche et alCitation7 conducted an observational prospective study to develop a simple rule for the prediction of poor outcome in patients with AECOPD. Their clinical severity index included cyanosis, impaired neurological status, lower limb edema, asterixis, and use of accessory inspiratory or expiratory muscles and predicted the in-hospital mortality with a satisfied sensitivity and specificity.
Therefore, the present study was conducted to assess determinants of 90-day re-exacerbation, including clinical presentation and treatment in the current exacerbation as well as the status before exacerbation in hospitalized patients for AECOPD. A prediction score was built. It provided clinicians with simple and reliable criteria for the identification of patients at risk of re-exacerbation in short term and helped to strengthen the medical education and support after discharge from hospital.
Methods
Ethics
All procedures were approved by the Ethics Committee of Zhongshan Hospital (Shanghai, People’s Republic of China), and informed consent was obtained from all the patients.
Study design
The present prospective observational study was conducted in Zhongshan Hospital, Shanghai, People’s Republic of China. All consecutive patients hospitalized in the respiratory medical ward or intensive care unit between November 2013 and February 2014 with a diagnosis of AECOPD were included. Included patients were followed until 90 days after discharge from the hospital.
Inclusion and exclusion criteria
Patients with AECOPD were included, which was defined as an acute event characterized by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication.Citation8,Citation9 The symptoms include deteriorating cough, wheeze or shortness of breath, increased sputum volume, purulent or mucopurulent sputum, and fever. Some patients may have insomnia, drowsiness, depression, fatigue, and mental disorder. The diagnosis of COPD was according to the Global initiative for chronic Obstructive Lung Disease (GOLD) spirometry definition.Citation10 The exclusion criteria include patients who had comorbidities of pulmonary embolism, congestive heart failure, pneumothorax or pleurisy, asthma, bronchiectasis, heart failure, thromboembolic disease, or restrictive respiratory insufficiency. When any of these diagnoses appeared on the discharge diagnosis of the medical charts, the subject was excluded.
Data collection
Status before the current acute exacerbation (pre-acute exacerbation condition)
The data collected related to sociodemographic characteristics: age, sex, and occupation. The smoking history and the number of hospitalizations during the previous year were obtained by questionnaire. Dyspnea was assessed using a modified Medical Research Council (mMRC) scale.Citation11 Health status impairment was assessed by the COPD assessment test (CAT).Citation12 The latest spirometry before enrollment of this study, including forced expiratory volume in 1 second (FEV1), forced expiratory volume in 1 second percent of predicted (FEV1%), forced vital capacity percent, inspiratory capacity percent, and vital capacity percent were recorded. The measurements were performed according to the guidelines of the American Thoracic Society.Citation13 The classification of airflow limitation severity (GOLD stages) was divided by the recommended cutoff values in 2014 GOLD.Citation10 The validated Charlson index was used to determine the degree of comorbidity.Citation14
Exacerbation status and treatment in the hospital
Data were collected regarding the duration of the exacerbation, length of stay in the hospital, clinical presentations at the onset of the AECOPD including presence of cyanosis, impaired neurological status, lower limb edema, asterixis, use of accessory respiratory muscles, pleural effusion, auscultatory findings, and the results of arterial blood gas analysis and treatment options including inhalation therapy, mechanical ventilation, and supplemental oxygen.
Follow-up
Data were collected regarding vital status, re-exacerbation frequency in 90 days after discharge from hospital by telephone call. The re-exacerbation in the follow-up was defined as an event characterized by a sustained worsening of respiratory symptoms for at least 2 days, requiring a visit to a doctor or the emergency department (ED) and/or antibiotics treatment or systemic steroids or both. Patients experiencing very mild respiratory symptoms not requiring any medical intervention were not regarded as having re-exacerbated in the follow-up.
Statistical analysis
Data are presented as mean ± standard deviation (SD), median (interquartile range [IQR]), or percentage. The outcome of interest was re-exacerbation (including death) in 90 days after discharge from the hospital. The differences in variables between patients with and without re-exacerbation were established using chi-square test for categorical variables and Student’s t-test or Mann–Whitney U-test for continuous variables. Then, status before acute exacerbation (AE), symptoms and signs at the onset of the AE, as well as treatment options were analyzed by univariate logistical analysis to show whether they were associated with an increased risk of re-exacerbation. The variables associated with re-exacerbation with a P-value of <0.05 were aggregated into a scoring system called re-exacerbation index (re-AE INDEX). The points assigned to each risk factor were weighted by dividing the individual β coefficient by the smallest β coefficient significantly different from 0 and rounding to the nearest integer. The point threshold of the AE frequency in the previous year was adopted according to Almargo et al’s study.Citation6 A score was calculated for each participant by adding the points corresponding to each risk factor.
Finally, multivariate analyses were performed; an enter procedure using a logistic regression model was applied. The scoring systems (re-AE INDEX) was analyzed to investigate its associations with risk of re-exacerbation adjusted by three models. The first one was adjusted by age, sex, and smoking history. CAT and mMRC was added in the second one. Charlson index was included in the third model.
The patients were divided into three groups depending upon the tertile of the re-AE INDEX score, and the re-exacerbation rate was compared among groups.
Model discrimination was assessed using the C-statistic, which is analogous to the area under the receiver operating characteristic curve.Citation15
Results
Patient characteristics
A total of 210 consecutive patients with AECPOD were considered for enrollment. Among them, 30 were excluded for lack of spirometry data and four for refusing to participate. Finally, a number of 176 patients with AECOPD were enrolled in the present study. describes the demographic characteristics of the population and gives details of medical history and patients’ condition at the AE. The median age of these patients was 71 years (IQR: 65, 77), with a predominance of male (81.8%). The differences in these values between patients without re-exacerbation and those with re-exacerbation in 90 days are shown in . Re-exacerbation data in 90 days after discharge were collected from 176 case patients by telephone call (none was lost in the follow-up), 86 of whom had at least one re-exacerbation (48.9%, including death of ten patients). The value of FEV1 before AE was lower in patients with re-exacerbation than those without re-exacerbation, but the difference did not reach statistical significance. However, the distribution of the GOLD grade in these two populations was quite different. More patients with re-exacerbation had a higher GOLD grade, which reflected the severity of airflow limitation (P=0.003). The other variables of spirometry (forced vital capacity percent, inspiratory capacity percent, and so on) were not statistically different between these two groups. The patients with re-exacerbation did not show more severe dyspnea (mMRC), worse health status impairment measured by CAT, or more coexisting conditions (Charlson index). As for the status of and treatment for the current AE, comorbidity of pleural effusion implied more chance to re-exacerbate in the following days. Patients with re-exacerbation showed a trend to have a lower arterial oxygen pressure (P=0.085). A higher proportion of patients with re-exacerbation used accessory respiratory muscles compared with those without re-exacerbation (38.4% vs 23.3%, P=0.031). Less patients with re-exacerbation received inhaled long-acting β-2-agonists (LABA; 58.1% vs 76.6%, P=0.009) and inhaled corticosteroids (ICS; 59.3% vs 76.6%, P=0.013), whereas many patients with re-exacerbation received controlled oxygen therapy (90.3% vs 77.8%, P=0.004), and noninvasive mechanical ventilation (37.2% vs 22.2%, P=0.029).
Table 1 Characteristics of the patients according to whether they had re-exacerbation
Risk factors associated with re-exacerbation in 90 days after discharge from hospital
shows factors associated with re-exacerbation on univariate logistic regression analysis when the variates (age categories, sex, BMI, GOLD grades, AE frequency in the previous year, etc) were individually integrated into the model. Re-exacerbation in 90 days was associated with age categories, GOLD stages, use of accessory respiratory muscles, pleural effusion, noninvasive mechanical ventilation, controlled oxygen therapy, and inhaled LABA, ICS, and length of hospital stay but was not associated with BMI or spirometry variables in stable stage (FEV1%, forced vital capacity percent, and inspiratory capacity percent). The CODEX was not significantly associated with re-exacerbation in our cohort (P=0.118).
Table 2 Risk of re-exacerbation by univariate logistic regression analysis
Based on these analyses, a subgroup of ten variables (age grades, GOLD grades, AE frequency in the previous year, pleural effusion, use of accessory respiratory muscles, noninvasive mechanical ventilation, controlled oxygen therapy, inhaled LABA, inhaled ICS, and length of hospital stay) was selected and was developed into the re-AE INDEX scoring system (). Other variables in were also assessed to enter into the re-AE INDEX scoring system but failed to increase the specificity and sensitivity; thus, they were excluded in the final re-AE INDEX scoring system. Each variable was assigned points if it had an unfavorable effect on the outcome. The variables of inhaled LABA and ICS had protective effects. Therefore, minus one point was given to these two factors. The median value for the re-AE INDEX in the study was 7 (IQR: 6, 9) (). The patients who were more likely to re-exacerbate had a higher re-AE INDEX compared with those who were not (9 [7, 10] vs 7 [5, 8], P<0.001).
Table 3 Variables and point values used for the computation of the re-AE INDEX
In an exploratory analysis, the various components of the re-AE INDEX were assigned with different weights (). The points assigned to each of these predictors using β coefficients were as follows:
0: age <65 years, 1: 65–70 years, 2: 71–77 years, 3: >77 years.
0: GOLD grade 1, 1: GOLD grade 2, 2: GOLD grade 3, 3: GOLD grade 4.
0: without AE in the previous year, 1: 1 to 2 times AE in the previous year, 2: more than 3 times AE in the previous year.
0: no pleural effusion, 2: pleural effusion.
0: no use of accessory respiratory muscles, 1: use of accessory respiratory muscles.
0: no use of noninvasive mechanical ventilation, 1: use of noninvasive mechanical ventilation.
0: no controlled oxygen therapy, 2: controlled oxygen therapy.
0: no inhaled ICS, −1: inhaled ICS.
0: no inhaled LABA, −1: inhaled LABA.
0: length of hospital stay ≤10 days, 1: 11–20 days, 2: 21–30 days, 3: >30 days.
Re-AE INDEX as an independent factor associated with re-exacerbation
Re-AE INDEX was strongly associated with risk of re-exacerbation in 90 days after discharge (P<0.001) by the univariate analysis (). The Re-AE INDEX was adjusted by three kinds of models (). When it was adjusted by age, sex, smoking history, CAT in stable COPD, mMRC in stable COPD, and Charlson index, the Re-AE INDEX was statistically independently associated with re-exacerbation in 90 days (P<0.001; odds ratio =1.709; 95% CI =1.389–2.101; ).
Table 4 Risk of re-exacerbation for re-AE INDEX by multivariate logistic regression analysis
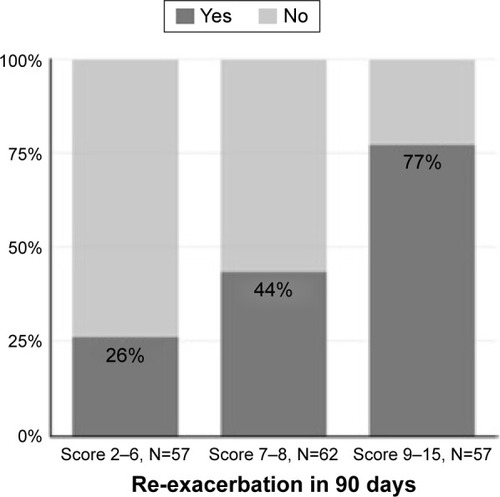
As mentioned in the statistical analysis section, a three-grade re-AE INDEX (2–6 scores, 7–8 scores, and 9–15 scores) was constructed on the basis of increment of scores. shows the increasing risk of re-exacerbation with the increment of re-AE INDEX scores. In the patients with a score of 9–15, 77% of them had at least one time of re-exacerbation in the following 90 days after discharge. For the patients with a score less than 6, the chance was only 26%. Patients with a higher score of re-AE INDEX had more chances to re-exacerbate compared with those with lower scores.
Comparisons with other index and variables
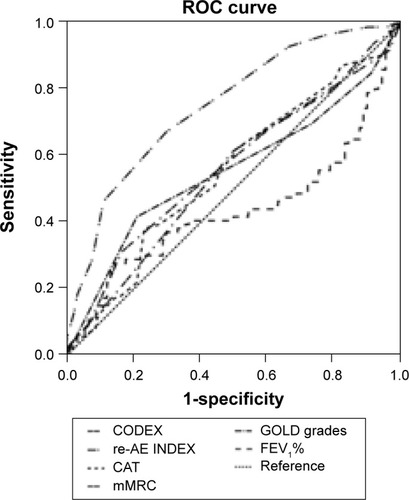
The prediction efficacy is depicted using the C-statistic and sensitivity and specificity. Risk of re-exacerbation strongly increased with increasing score of re-AE INDEX in the cohort. The INDEX showed good discrimination for re-exacerbation, with a C-statistic of 0.750 (P<0.001, , ). In our cohort, CODEX did not show statistical significance (P=0.107). CAT, mMRC, GOLD stages, or FEV1% could not efficiently predict the outcome of re-exacerbation in 90 days after discharge (P>0.05, , ).
Table 5 Comparison of predictive capacity of re-exacerbation among indexes and single variables by C-statistics
Figure 2 ROC curves for the re-AE INDEX, CODEX, GOLD grades, mMRC, CAT, and FEV1%.
Abbreviations: ROC, receiver operating characteristic; Re-AE INDEX, re-exacerbation index; CODEX, comorbidity, obstruction, dyspnea, and previous severe exacerbations; GOLD, Global initiative for chronic Obstructive Lung Disease in stable COPD; mMRC, modified Medical Research Council scale in stable COPD; CAT, COPD assessment test in stable COPD; FEV1%, forced expiratory volume in 1 second percent of predicted in stable COPD.
Discussion
Although identifying patients who will re-exacerbate in a short term after discharge from the hospital is clearly an increasingly important issue of concern for both the clinician and patients, few studies aimed at identifying the corresponding clinical predictors. To the authors’ knowledge, this is the first prospective study to investigate predictive factors, including clinical presentations and treatment options for 90-day re-exacerbation in patients with hospitalized AECOPD after their discharge. Patients with higher degree of lung function impairment, frequent AE in the previous year, and more severe disease at presentation were more likely to re-exacerbate later. Patients receiving adequate treatment (inhaled LABA and ICS) had fewer exacerbations after discharge. The main aim of the present study is the identification of simple, easily accessible, and strong predictors for re-exacerbation in hospitalized patients with AECOPD. By combining these predictors, we developed a simple grading system for AECOPD: the re-AE INDEX. The re-AE INDEX could help in identifying patients who require posthospital support and monitoring in order to delay next exacerbation.
As mentioned in the “Results” section, this score of re-AE INDEX was easy to calculate. We believe that the re-AE INDEX is useful because it includes GOLD grades that quantify the degree of lung function impairment, the clinical presentation of AE that captures the patient’s severity, and the treatment in the present AE that expresses the influence of treatment to the following consequences of patients with AECOPD. GOLD spirometry grading systems have been used in a large body of data,Citation16,Citation17 which show an increase in risk of exacerbations with worsening of airflow limitation. Roche et alCitation7 conducted an observational prospective study to develop a simple rule for the prediction of poor outcome in patients presenting to EDs with initially non-life-threatening COPD exacerbations. Their primary end point was in-hospital outcomes. Their severity index included use of accessory inspiratory or expiratory muscles which is concordant with what was discovered in the present study and supported the rationality of including use of accessory respiratory muscles in the re-AE INDEX. Univariate regression analysis showed the application of controlled oxygen therapy, and noninvasive mechanical ventilation was associated with increasing risk of re-exacerbation; thus, they were interpreted as the surrogate of the disease severity. The effect of age as an additional prognostic factor is well described in hospital mortalityCitation18 or 30 or 90 days mortality.Citation19,Citation20 Age ≥65 years was adopted into the CURB65 scores which was designed to predict mortality risk in community-acquired pneumonia and was proved to significantly predict risk of death during the hospital admission and at 30 days in patients with AECOPD.Citation20 Stone et al showed older people admitted with AECOPD had more severe symptoms and comorbidity prior to exacerbation and higher in-patient/90-day mortality following exacerbation.Citation21 In our study, every ten years of age increased the risk of re-exacerbation in 90 days after discharge from hospital (OR =1.359). Therefore, age category was selected as a parameter of the re-AE INDEX, which increased the sensitivity and specificity of the predictive power compared with that without age category (data not shown).
In addition, if COPD treatments prove to modify the risk of outcome, they could also be considered for scoring indices.Citation22 Patients treated with ICS and/or LABA had a lower risk of death than patients using neither of these types of treatment.Citation23 Inhaled LABA was proved to be effective in the treatment of AECOPD.Citation24–Citation26 In Segreti et al’s study, 5-day therapy with indacaterol 300 µg once daily significantly improved pulmonary function and reduced respiratory rate, suggesting an amelioration of AECOPD.Citation26 Administration of corticosteroids in COPD exacerbations could shorten recovery time and improve lung function and arterial hypoxemia. Nebulised budesonide alone was recommended as an alternative to oral corticosteroids in the treatment of exacerbations.Citation27–Citation29 Early initiation of ICS and/or inhaled LABA in hospitalized patients showed protective effect for re-exacerbations in our analysis.
It should be noted that the presence of pleural effusion at the onset of AECOPD served as a component of the re-AE INDEX score. It can be easily identified on the chest radiological investigation and could be due to hypoproteinemia or elevated hydrostatic pressure of pulmonary vascular system, which would contribute to the severity of AECOPD.
The re-AE INDEX may provide comprehensive information of the outcome. Its prediction efficacy depicted by the C-statistic was satisfactory, especially considering the simplicity of the score. CODEX was calculated according to the reported methodCitation6 in the present study. In fact, the C-statistic of re-AE INDEX was higher than that of CODEX (0.570 vs 0.750, ). CODEX did not accurately predict the outcome of 90 days in our cohort. The potential factor may be the population of Almargo et al’s study had several different characteristics compared with those of ours. They had 11.5% patients discharged from the ED without requiring conventional hospitalization. Patients discharged directly from the ED were younger, with a higher FEV1 and fewer comorbidities (all P<0.01).Citation6 The FEV1% of their subjects was also higher than that of our patients, which may imply that the severity of their patients is less compared with that in our study. Of course, Almargo et al’s study provided strong verification of several parameters included in the present study. AE frequency in the previous year and obstruction of air flow assessed by the grades of FEV1% were proved to be useful predictors of the short-term outcome both in our and Almargo et al’s study. The threshold of AE frequency in the previous year was concordant with that in CODEX.
In the present study, we added neither mMRC questionnaire, which was considered as the assessment of the severity of breathlessness, nor CAT, which is an eight-item unidimensional measure of health status impairment in COPD as the elements of re-AE INDEX. We did not find any difference of mMRC or CAT between the patients with re-exacerbation and those without. Although we tried to enter mMRC and CAT into the univariate logistic regression analysis, these two factors were not related with the outcome of re-exacerbation in 90 days after discharge of AECOPD. Patients were also assessed into A, B, C, and D groups according to spirometry, CAT test, or mMRC results and exacerbation frequency in the previous year recommended by GOLD, 2014.Citation10 There was no statistical difference of the distribution of the combined COPD assessment (A, B, C, and D groups) between patients with and without re-exacerbation in 90 days after discharge (chi-square test, P=0.402). Therefore, we did not include the combined COPD assessment (A, B, C, and D groups) as one variable in our re-AE index. The patient’s perception of dyspnea had the huge heterogeneity, in which a high score of mMRC do not mean the high risk of re-exacerbation.Citation10 Although the GOLD and the American Thoracic Society recommend that a patient’s perception of dyspnea be included in assessing the risk of re-exacerbation for COPD,Citation10 they also stress that other parameters such as GOLD grades and exacerbation history would influence the following outcome. At the same time, we admitted that different design of the study including patient populations, settings, duration of follow-up, variables collected, and statistical methods will affect the sensitivity and specificity of the prognostic factors. The mMRC was verified to be a useful predictor of the outcome of patients with stable COPD and included into the BODE, ADO, BODEx, DOSE indexes, which served as predictors for long-term mortality (BODE: 52 months,Citation2 BODEx: 80 months,Citation3 ADO: 3 yearsCitation4 and DOSE: 9 years).
There are some limitations of this study. First, the aim of the study was to develop a scoring system to identify the patients at risk of re-exacerbation in a short term after discharge from hospital. Obviously, the spirometry data are mandatory elements in the present study. Hence, patients without the spirometry data were excluded from the study, and this may exclude those patients with very high severity who could not complete spirometry. However, excluding patients in the end stage of the disease would not impair the power of re-AE INDEX in identifying patients at high risk of re-exacerbation because GOLD grading was one of the components of the index. Moreover, the importance of preventing frequent re-exacerbations, which were considered the markers of deterioration, is well acknowledged.Citation30 Another limitation of our study is that we lacked the date of 6 minutes walking distance. Therefore, we could not calculate BODE index from our study cohort. Although BODE index was widely used, it was designed to evaluate the long-term mortality of patients with COPD. We compared the re-AE INDEX with CODEX whose purpose was identical with that of the present study. The prediction power of re-AE INDEX was superior to that of CODEX in our cohort. We also calculated BODEx, ADO, and DOSE and made a comparison with re-AE INDEX by the receiver operating characteristic curve analysis. The prediction power of re-AE INDEX for re-exacerbation in 90 days after discharge from hospital was superior to that of other indexes (data not shown). Third, this is an observational, un-validated study. We lack another similar population with AECOPD to confirm our finding in the present study, which weakened the power of re-AE INDEX in prediction of re-exacerbation. Finally, the re-exacerbation status during the 90 days after discharge was investigated as a binary parameter. Therefore, we could not carry out the analysis of the association of re-AE INDEX and re-exacerbation frequency.
Conclusion
In conclusion, a comprehensive re-AE INDEX integrating parameters of stable COPD and clinical presentations at the onset of exacerbation and treatment showed a strong predictive capacity for short-term outcome in patients with AECOPD. The index could serve as a tool to identify those at high risk of re-exacerbation. Further studies are required to verify these findings.
Author contributions
Drs Dong Liu, Jing Zhang contributed to the experimental design, study conduct, data analysis, and drafting and revising the manuscript; Drs Shao-Hua Peng, Si-Hong Bai and Hai-Xia Liu contributed to the data collection and revising manuscript. Prof Jie-Ming Qu contributed to the experimental design, interpretation of data and revising the manuscript. All authors had full access to all study data and had final responsibility for the decision to submit for publication. All have reviewed the manuscript and approved the final version for submission. All the authors ensured that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Acknowledgments
We thank Dr Guo-Zhu Geng for his excellent statistical contribution to this study. This study was supported by Zhuo-Xue project of Fudan University and The National Natural Science Foundation (Nos 81470231 and 81200033).
Disclosure
The authors report no conflicts of interest in this work.
References
- MathersCDLoncarDProjections of global mortality and burden of disease from 2002 to 2030PLoS Med2006311e44217132052
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- Soler-CataluñaJJMartínez-GarcíaMASánchezLSTorderaMPSánchezPRSevere exacerbations and BODE index: two independent risk factors for death in male COPD patientsRespir Med2009103569269919131231
- PuhanMAGarcia-AymerichJFreyMExpansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO indexLancet2009374969170471119716962
- JonesRCDonaldsonGCChavannesNHDerivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE IndexAm J Respir Crit Care Med2009180121189119519797160
- AlmagroPSorianoJBCabreraFJWorking Group on COPD, Spanish Society of Internal MedicineShort- and medium-term prognosis in patients hospitalized for COPD exacerbation: the CODEX indexChest2014145597298024077342
- RocheNZureikMSoussanDNeukirchFPerrotinDUrgence BPCO (COPD Emergency) Scientific CommitteePredictors of outcomes in COPD exacerbation cases presenting to the emergency departmentEur Respir J200832495396118508819
- Rodriguez-RoisinRToward a consensus definition for COPD exacerbationsChest20001175 suppl 2398s401s10843984
- CelliBRBarnesPJExacerbations of chronic obstructive pulmonary diseaseEur Respir J20072961224123817540785
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for Diagnosis, Management, and Prevention of COPD2015 Available from: http://www.goldcopd.org/Accessed January 1, 2015
- MahlerDAHarverAA factor analysis of dyspnea ratings, respiratory muscle strength, and lung function in patients with chronic obstructive pulmonary diseaseAm Rev Respir Dis19921452 pt 14674701736759
- JonesPWHardingGBerryPWiklundIChenWHKline LeidyNDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
- American Thoracic SocietyLung function testing: selection of reference values and interpretative strategiesAm Rev Respir Dis19911445120212181952453
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognositic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- HanleyJAMcNeilBJThe meaning and use of the area under a receiver operating characteristic (ROC) curveRadiology1982143129367063747
- AaronSDDonaldsonGCWhitmoreGAHurstJRRamsayTWedzichaJATime course and pattern of COPD exacerbation onsetThorax201267323824322008189
- LeivsethLBrumptonBMNilsenTIMaiXMJohnsenRLanghammerAGOLD classifications and mortality in chronic obstructive pulmonary disease: the HUNT Study, NorwayThorax2013681091492123611880
- DransfieldMTRoweSMJohnsonJEBaileyWCGeraldLBUse of beta blockers and the risk of death in hospitalised patients with acute exacerbations of COPDThorax200863430130517951276
- ConnollyMJLoweDAnsteyKBritish Thoracic Society and the Royal College of Physicians Clinical Effectiveness Evaluation Unit (CEEu)Admissions to hospital with exacerbations of chronic obstructive pulmonary disease: effect of age related factors and service organisationThorax2006611084384816928716
- ChangCLSullivanGDKaralusNCMillsGDMcLachlanJDHancoxRJPredicting early mortality in acute exacerbation of chronic obstructive pulmonary disease using the CURB65 scoreRespirology201116114615120920140
- StoneRALoweDPotterJMBuckinghamRJRobertsCMPurseyNJManaging patients with COPD exacerbation: does age matter?Age Ageing201241446146822454133
- MoonsKGRoystonPVergouweYGrobbeeDEAltmanDGPrognosis and prognostic research: what, why, and how?BMJ2009338b37519237405
- GudmundssonGGislasonTLindbergEMortality in COPD patients discharged from hospital: the role of treatment and co-morbidityRespir Res2006710916914029
- CazzolaMDi PernaFD’AmatoMCalifanoCMateraMGD’AmatoGFormoterol Turbuhaler for as-needed therapy in patients with mild acute exacerbations of COPDRespir Med2001951191792111716207
- CazzolaMMateraMGLong-acting beta(2) agonists as potential option in the treatment of acute exacerbations of COPDPulm Pharmacol Ther200316419720112850121
- SegretiAFioriECalzettaLThe effect of indacaterol during an acute exacerbation of COPDPulm Pharmacol Ther201326663063423578980
- MaltaisFOstinelliJBourbeauJComparison of nebulized budesonide and oral prednisolone with placebo in the treatment of acute exacerbations of chronic obstructive pulmonary disease: a randomized controlled trialAm J Respir Crit Care Med2002165569870311874817
- GunenHHacievliyagilSSYetkinOGulbasGMutluLCInEThe role of nebulised budesonide in the treatment of exacerbations of COPDEur Respir J200729466066717251232
- StällbergBSelroosOVogelmeierCAnderssonEEkströmTLarssonKBudesonide/formoterol as effective as prednisolone plus formoterol in acute exacerbations of COPD. A double-blind, randomised, non-inferiority, parallel-group, multicentre studyRespir Res2009101119228428
- HurstJRVestboJAnzuetoAEvaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary diseaseN Engl J Med2010363121128113820843247