Abstract
We report an educational autopsy case of combined pulmonary fibrosis and emphysema. Radiological patterns of the upper lung were considered as mostly emphysema, but pathological observation revealed significant interstitial fibrosis of usual interstitial pneumonia as a major pathology. The patient eventually developed acute exacerbation of background interstitial pneumonia. Careful radiological and pathological correlation of the current case indicates that regions with distal acinar emphysema on computed tomography image may possess histologically marked dense fibrosis of lethal interstitial pneumonia.
Keywords:
Introduction
Historically, pulmonary emphysema is a classic condition of obstructive disease while pulmonary fibrosis is a prototype of restrictive disease. These two conditions had been considered as diseases of different spectrums. However, coexistence of pulmonary emphysema and fibrosis has been reported increasingly during recent years, in which Cottin et al proposed a new concept of combined pulmonary fibrosis and emphysema (CPFE) as a distinctive condition of diffuse lung disease.Citation1 Cases with such combined condition have been widely recognized,Citation2,Citation3 however, in the current American Thoracic Society/European Respiratory Society (ATS/ERS) statement of idiopathic interstitial pneumonias, CPFE is described as an example of coexisting patterns comprising a heterogeneous population of patients and a syndrome which does not achieve a consensual understanding in the societies.Citation4
An increasing number of publications describe combination of emphysema and interstitial fibrosis as having frequent association with carcinomas and pulmonary hypertension.Citation5–Citation8 Accurate recognition of background interstitial fibrosis may have high clinical importance considering the risk of lethal acute exacerbation. The biological relationship between emphysema and interstitial fibrosis is still uncertain and whether they are two different diseases simply associated with cigarette smoking or diseases of one spectrum. In that sense, studies of careful radiological and pathological correlation of combined emphysema and fibrosis cases are needed.
Clinical history
An 83-year old male with smoking history of 63 pack years was diagnosed with interstitial lung disease by chest radiograph at 76 years of age. Before presentation he had also recently been diagnosed with rheumatoid arthritis based on 2010 Rheumatoid Arthritis Classification and had been on low dose of prednisolone (5 mg/day).Citation9 He then presented with respiratory symptoms after 2 weeks and pulmonary medicine specialists were consulted. He was treated with antibiotics under clinical diagnosis of infectious pneumonia, but did not respond well to treatment and further presented with right chest pain and fatigue a week later. At that time, he also developed renal dysfunction. Due to the serum elevation of myeloperoxidase anti-neutrophil cytoplasmic antibody (MPO-ANCA), the patient was suspected to have ANCA-related glomerular nephritis and was administered high dose methylprednisolone (500 mg/day). Computed tomography (CT) images were taken at the time of admission revealing a right lower lobe mass, which was biopsied and confirmed to be pulmonary adenocarcinoma. Due to the advanced stage of the carcinoma and patient’s poor performance status, best supportive care was selected. Two weeks after admission, pulmonary dysfunction rapidly progressed to respiratory failure, resulting in his passing 1 month after admission. His FiO2/PaO2 level at that time was 60 mmHg. Pulmonary function test was not performed due to the poor physical status of the patient. Serological test at the time of admission indicated the following abnormalities: CRP 16.56 mg/dL; KL-6- 520.8 U/mL; MPO-ANCA-257 IU/mL; antinuclear antibody ×160.
Radiological findings
CT images taken at the time of admission showed paraseptal and centriacinar emphysema with mild reticulation predominantly in both upper lobes (). Fine and coarse reticulation with mild bronchiectasis and honeycomb-like cystic airspaces were also seen with basal and peripheral predominance (), which were originally considered to be a combination of upper-zone simple emphysema and lower-zone pulmonary fibrosis. At the top of the right lower lobe, a lobulated solid mass of adenocarcinoma was seen (). The marginal zone of emphysematous areas was relatively clear and irregular compared to “simple” emphysema (). Some areas of emphysema were admixed with reticulation, and fine reticulations and limited ground glass opacification were seen adjacent to the low attenuation areas.
Figure 1 HRCT images of the case.
Abbreviation: HRCT, high-resolution computed tomography.

Pathological findings
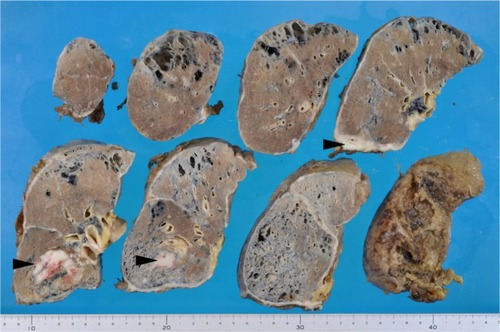
By gross pathology, subpleural cystic changes were obvious throughout craniocaudal levels, most prominent in the lower lungs. Remaining lung areas were yellow to brown in color with solid appearance ().
Figure 2 Gross appearance of the right lung.
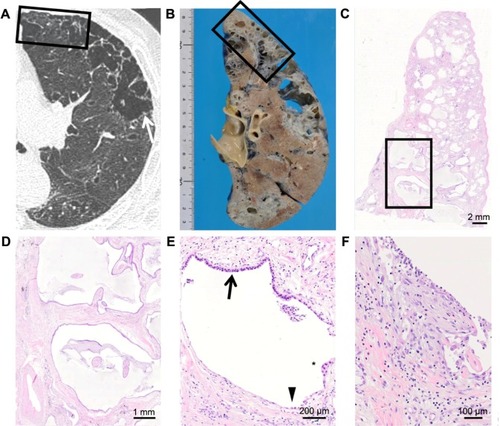
Histologically, lower lungs indicated numerous cystic spaces corresponding to honeycomb cysts bilaterally, in which several cystic spaces were surrounded by dense fibrosis and filled with mucus. Most of these cysts were covered by the columnar bronchiolar type epithelia. Right lower lobe showed emphysematous lesions radiologically and macroscopically, but microscopic observation revealed marked interstitial fibrosis and smooth muscle hyperplasia (). Patchy, peripheral-dominant dense fibrosis was observed. Fibroblastic foci were inconspicuous but found in the wall of honeycomb cysts. Right upper lobe appearing to be non-fibrotic tissue radiologically also demonstrates focal interstitial fibrosis and smooth muscle hyperplasia (). Furthermore, left upper lobe indicates paraseptal emphysema with minimal reticulation in the radiological observation. However, it turned out to have remarkable fibrotic changes histologically corresponding to usual interstitial pneumonia ().
Figure 3 Computed tomography images and their corresponding histological images of right lower lobe.
Notes: (A) Computed tomography image shows coarse reticulation with honeycomb-like clustered cystic airspaces. Squared area corresponds to microscopic observation (C). (B) A gross picture of the same lesion. Squared area corresponds to microscopic observation (C). (C) Microscopic observation revealed cystic spaces and interstitial fibrosis. Arrowheads indicate areas corresponding to honeycomb cysts.
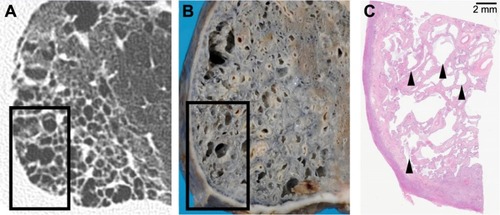
Figure 4 Computed tomography images and their corresponding histological images of right upper lobe.
Notes: (A) Computed tomography image shows subtle fine reticulation (arrow) which can be identified with careful observations. (B) A gross picture of the same area. (C) Microscopic observation of squared area in (A, B). (D) Close-up of the squared area in (C) revealed significant interstitial fibrosis.
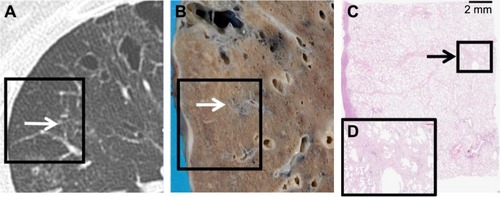
Figure 5 Computed tomography images and their corresponding histological images of left upper lobe.
Discussion
Histopathological analysis of the autopsied CPFE case revealed a surprising discordance between the impression of CT images and pathological findings. CT images of lower lung areas showed reticular shadow corresponding to pulmonary fibrosis. However, CT images of upper lung areas were originally considered to be simple emphysema. On the other hand, histological evaluation at autopsy revealed unexpected dense fibrosis of usual interstitial pneumonia (UIP) pattern both in the upper and lower lung areas.
This discrepancy is clinically important and should not be overlooked; in other words, pulmonologists and radiologists need to be informed of this as a warning. To our best knowledge, no case reports have been done on an acute exacerbation of diffuse alveolar damage due to emphysema alone. On the other hand, it is well known that a significant number of cases with pulmonary fibrosis, mainly UIP, accompanies acute respiratory failure leading to death.
As is described as characteristic histological patterns corresponding to the interstitial fibrosis seen in the smokers’ lung, airspace enlargement with fibrosis (AEF) and smoking related interstitial fibrosis were reported.Citation10,Citation11 Although AEF and smoking related interstitial fibrosis are classified as subclinical conditions and clinically unimportant complications in the latest guidelines,Citation4 two thirds of AEF cases are associated with UIP fibrosis, as Kawabata et al., report in their manuscript.Citation11 Alternatively, majority of cases indicate the combination of AEF and UIP. Another critical problem of this context is that there is no consensus of how to diagnose and treat the patients with subtle interstitial fibrosis among “mostly emphysema” cases. Distinction between emphysema and interstitial fibrosis is difficult, and the clinical border of the two conditions seen within the same case is vague. Emphysema and pulmonary fibrosis were considered to be two different diseases, but the possibility that they are on common spectrum still remains. Recently, Stanley et al found mutations in TERT gene in emphysema patients.Citation12 TERT gene mutation is also known as a mutation responsible for familial pulmonary fibrosis, and their report may explain why these two conditions are difficult to separate in certain cases.
Connective tissue disease, especially rheumatoid arthritis, is well known to be associated with pulmonary fibrosis. However, connective tissue disease-associated pulmonary fibrosis and idiopathic pulmonary fibrosis are often difficult to distinguish from one another.Citation13 Similar situation applies to MPO-ANCA-related pulmonary fibrosis.Citation14 However, there is a limited number of manuscripts describing the relationships between CPFE and autoimmune diseases including ANCA, thereby making the clear recognition of biological effect difficult,Citation15–Citation17 calling for further research in this field.
Cases with CPFE are known to have significantly higher risks of carcinoma association.Citation8 This is an important factor to mention to pulmonologists, in order to urge careful observation of follow-up radiographs when patients present without any known carcinomas. As for cases that are already diagnosed with lung cancer, general surgical pathologists may focus only on staging and differentiating the histological types of cancer but not on observing background lung pathologies. Considering the risk of lethal acute exacerbation of pulmonary fibrosis, careful evaluation of radiographs to judge presence of background interstitial fibrosis is important. Some fibrosis mixed with emphysema may be subclinical and unimportant. However, pulmonary fibrosis generally possesses risks of acute exacerbation. Therefore, detection of fibrosis in the wall of emphysematous cysts as seen in the present case is critical.
Conclusion
We have examined an autopsy case showing emphysema and pulmonary fibrosis, in which the patient developed diffuse alveolar damage as an acute exacerbation. Radiological and pathological correlation of the current case indicates that simple emphysema on CT may possess characteristics of usual interstitial pneumonia histologically, which can later lead to lethal acute exacerbation.
Disclosure
The authors report no conflicts of interest in this work.
References
- CottinVNunesHBrilletPYCombined pulmonary fibrosis and emphysema: a distinct underrecognised entityEur Respi J2005264586593
- DoddaVRSalazar-SchicchiJSpiroPCombined pulmonary fibrosis and emphysemaRespir Care201257346747022004839
- TakahashiMFukuokaJNittaNImaging of pulmonary emphysema: a pictorial reviewInt J Chron Obstruct Pulmon Dis20083219320418686729
- TravisWDCostabelUHansellDMAn official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumoniasAm J Respir Crit Care Med2013188673374824032382
- UsuiKTanaiCTanakaYNodaHIshiharaTThe prevalence of pulmonary fibrosis combined with emphysema in patients with lung cancerRespirology201116232633121114711
- SuginoKOtaHFukasawaYUekusaTHommaSPathological characteristics in idiopathic nonspecific interstitial pneumonia with emphysema and pulmonary hypertensionRespirol Case Rep201312394225473539
- CottinVClinical case: Combined pulmonary fibrosis and emphysema with pulmonary hypertension – clinical managementBMC Res Notes20136Suppl 1S223734851
- JankowichMDRoundsSICombined pulmonary fibrosis and emphysema syndrome: a reviewChest2012141122223122215830
- AletahaDNeogiTSilmanAJ2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiativeAnn Rheum Dis20106991580158820699241
- KatzensteinALMukhopadhyaySZanardiCDexterEClinically occult interstitial fibrosis in smokers: classification and significance of a surprisingly common finding in lobectomy specimensHum Pathol201041331632520004953
- KawabataYHoshiEMuraiKSmoking-related changes in the background lung of specimens resected for lung cancer: a semiquantitative study with correlation to postoperative courseHistopathology200853670771419102010
- StanleySEChenJJPodlevskyJDTelomerase mutations in smokers with severe emphysemaJ Clin Invest2015125256357025562321
- TabataKFukuokaJHistopathologic features of usual interstitial pneumonia and related patterns: what is important for radiologists?Semin Ultrasound CT MR201435121124480138
- TanakaTOtaniKEgashiraRInterstitial pneumonia associated with MPO-ANCA: clinicopathological features of nine patientsRespir Med2012106121765177022992339
- TzouvelekisAZacharisGOikonomouAIncreased incidence of autoimmune markers in patients with combined pulmonary fibrosis and emphysemaBMC Pulm Med2013133123697753
- CottinVNunesHMouthonLCombined pulmonary fibrosis and emphysema syndrome in connective tissue diseaseArthritis Rheum201163129530420936629
- HommaSSuzukiASatoKPulmonary involvement in ANCA-associated vasculitis from the view of the pulmonologistClin Exp Nephrol201317566767123188194
