Abstract
COPD patients have an increased prevalence of osteoporosis (OP) compared with healthy people. Physical inactivity in COPD patients is a crucial risk factor for OP; the COPD assessment test (CAT) is the newest assessment tool for the health status and daily activities of COPD patients. This study investigated the relationship among daily physical activity (DPA), CAT scores, and bone mineral density (BMD) in COPD patients with or without OP. This study included 30 participants. Ambulatory DPA was measured using actigraphy and oxygen saturation by using a pulse oximeter. BMD was measured using dual-energy X-ray absorptiometry. OP was defined as a T-score (standard deviations from a young, sex-specific reference mean BMD) less than or equal to −2.5 SD for the lumbar spine, total hip, and femoral neck. We quantified oxygen desaturation during DPA by using a desaturation index and recorded all DPA, except during sleep. COPD patients with OP had lower DPA and higher CAT scores than those of patients without OP. DPA was significantly positively correlated with (lumbar spine, total hip, and femoral neck) BMD (r=0.399, 0.602, 0.438, respectively, all P<0.05) and T-score (r=0.471, 0.531, 0.459, respectively, all P<0.05), whereas CAT scores were significantly negatively correlated with (total hip and femoral neck) BMD (r=−0.412, −0.552, respectively, P<0.05) and (lumbar spine, total hip, and femoral neck) T-score (r=−0.389, −0.429, −0.543, respectively, P<0.05). Low femoral neck BMD in COPD patients was related to high CAT scores. Our results show no significant difference in desaturation index, low SpO2, and inflammatory markers (IL-6, TNF-α, IL-8/CXCL8, CRP, and 8-isoprostane) between the two groups. Chest physicians should be aware that COPD patients with OP have low DPA and high CAT scores.
Introduction
COPD pathology involves both the lungs and extra-pulmonary abnormalities, such as skeletal muscle wasting, cachexia, diabetes, and anemia.Citation1 COPD is also characterized by low-grade systemic inflammation caused by circulating inflammatory mediators, such as IL-6, TNF-α, IL-8/CXCL8, and CRP, and leukocytes are increased or activated in stable disease conditions.Citation2,Citation3 Lee et alCitation4 found that intracellular oxidative stress was increased in patients with severe COPD. Moreover, sedentary behavior is believed to be crucial to the development of skeletal muscle weakness in COPD patients. Physical activity in daily life is known to be reduced because of multifactorial causes and worsened prognosis in COPD patients. As the disease progresses, COPD patients have an increased prevalence of osteoporosis (OP) compared with healthy people.Citation5,Citation6 Low bone mineral density (BMD) leading to OP is common in COPD patients.Citation7 OP is a systemic skeletal disease characterized by low BMD caused by microarchitectural changes in the bone. These changes lead to an increased susceptibility to fractures.Citation8 A strong association exists between COPD and OP because of common risk factors such as age, low body mass index (BMI), history of smoking, systemic inflammation, systemic corticosteroid use, and inactivity.Citation9 Large variations have been found in the physical activity levels of COPD patients.Citation10,Citation11 Katajisto et al observed high levels of physical inactivity and increased patient perception of dyspnea in COPD patients.Citation12
The COPD assessment test (CAT) is the newest assessment tool for the health status and daily activities of COPD patients.Citation13 Validation studies have shown that it has properties similar to those of St George’s Respiratory Questionnaire.Citation12,Citation13 This instrument has been noted for its ease of useCitation14 and contains eight items including cough, phlegm, chest tightness, breathlessness walking up hills/stairs, activity limitations at home, confidence leaving home, sleep, and energy.Citation15 This study investigated the relationship among daily physical activity (DPA), CAT scores, and BMD in COPD patients with or without OP.
Methods
Study design and patients
We recruited COPD patients from the pulmonary outpatient unit of a medical center. COPD diagnosis was based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.Citation16 COPD patients with a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of <70% of the predicted value were eligible to participate in this study. Those who had acute infection or exacerbation and used systemic (oral) corticosteroids were excluded. Thirty patients were eligible and consented to participate in this study. All participants were ambulatory, in stable conditions, and undergoing standard pharmacological treatment. The study protocol was approved by the Ethics Committee of the Chang-Gung Memorial Hospital (100-2225A3), and all participants provided informed written consent before being enrolled.
Procedures and measurements
Each participant was personally interviewed to collect demographic, lifestyle (dietary and exercise patterns; use of coffee, tobacco, alcohol, and other drugs; and occupation), and disease-related data. The CAT was administered, and the weight and height of patients were measured according to standard methods. Body weight was measured to the nearest 0.1 kg with participants standing barefoot and wearing light indoor clothing, and height was measured to the nearest 0.1 cm. BMI was calculated according to the formula: weight (kg)/height2 (m2). Body fat (%) was measured using bioelectrical impedance analysis (BF-800 Body Fat Monitor, TANITA, Tokyo, Japan). Fat-free mass (FFM) was calculated by subtracting body weight from fat mass. Fat-free mass index (FFMI) was calculated according to the formula: FFM (kg)/height2 (m2).Citation2,Citation17 Serum samples were obtained and were stored at −80°C for laboratory measurements.
Pulmonary function parameters were assessed using the Vitalograph Spirotac V™. FEV1 and FVC were measured, and FEV1/FVC was calculated.
Oxygen saturation was measured during DPA. We monitored oxygenation by using an oximeter (WristOx; Nonin Medical, Inc., MN, USA), and daily activity was assessed using a MicroMini-Motionlogger® actigraph.Citation18 Patients underwent ambulatory recordings, producing 24-hour continuous data, and daily card records were maintained. DPA refers to the total activity amount subtracted from sleep time. We used a desaturation index (DSI) or % time for oxygen saturation, which was <90% during the recording.Citation19
Lumbar spine, total hip, and femoral neck BMDs were assessed using dual-energy X-ray bone densitometry to identify OP risk. BMD was categorized according to the World Health Organization (WHO) criteria.Citation20 Normal BMD was considered to be within 1 standard deviation (SD) of the average reference value for healthy young adults (T-score). OP was defined as a T-score less than or equal to −2.5 SD for the lumbar spine and the total hip in any variable.
We used enzyme-linked immunosorbent assays to determine the serum levels of TNF-α, IL-6, CRP (R&D Systems, Inc., Minneapolis, MN, USA), and 8-isoprostane (MyBio-Source, San Diego, CA, USA) according to manufacturer instructions.
Statistical analyses
The results were statistically analyzed using SPSS for Windows 19.0 (SPSS Inc., Chicago, IL, USA) and Prism 5. Descriptive data are expressed as mean ± SD or percentage. Continuous variables were compared using Student’s t-test, and categorical variables were compared between the two groups by using the chi-square test. Pearson’s correlation was used to evaluate the strength of the relationship among BMD, age, anthropometric indicators, actigraphy activity, and CAT scores. Multiple linear regression analysis was used to determine the independent factors associated with BMD (g/cm2) at the lumbar spine, total hip, and femoral neck sites. We collected the demographic data of COPD patients. Subsequently, we used a simple linear regression model to identify potential significant factors and then use multivariate analysis to confirm the independent variables. In these methods, the variables selected were age, disease severity (FEV1, % predicted), BMI, FFMI, CAT scores, and DPA. Statistical significance for all evaluations was set at P<0.05.
Results
Descriptive statistics are listed in . The mean age was similar between COPD patients without and with OP (71.7±9.1 vs 70.2±9.0 years, P>0.05). Most participants without and with OP had a history of smoking (11/11 and 18/19, respectively); anthropometric indicators, including BMI and FFMI, were significantly higher in patients without OP than that of those with OP (27.7±4.2 vs 23.5±3.9 kg/m2; 19.3±2.3 vs 17.4±2.1 kg/m2, all P<0.01). CAT scores were significantly different between those without and with OP (5.0±3.8 vs 8.1±5.8, P<0.05). No significant differences were observed in pulmonary function, including FEV1, FVC, and FEV1/FVC, between the groups (P>0.05). BMDs at the lumbar spine, total hip, and femoral neck sites were significantly different between patients without and with OP (1.05±0.05 vs 0.86±0.04, P<0.05; 0.95±0.04 vs 0.73±0.03, P<0.001; 0.82±0.04 vs 0.62±0.02, P<0.001).
Table 1 Characteristics of the patients with COPD
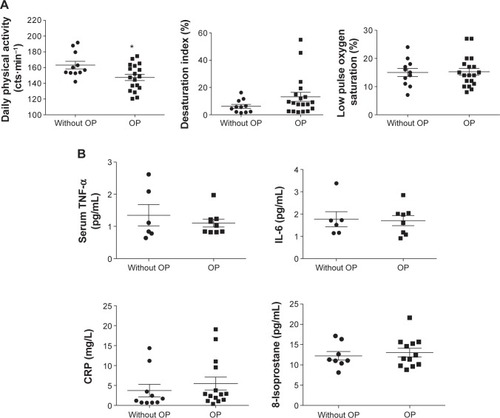
shows that COPD patients with OP had significantly lower DPA (P=0.0193) than that of those without OP; however, no significant differences were observed in DSI and low SpO2 (P=0.1330 and 0.8946) between the two groups. indicates that TNF-α (1.35±0.33 vs 1.10±0.12, P>0.05), IL-6 (1.77±0.34 vs 1.55±0.26, P>0.05), CRP (3.72±1.55 vs 5.49±1.63, P>0.05), and 8-isoprostane (12.25±1.08 vs 13.04±1.06, P>0.05) were not significantly different between COPD patients without and with OP.
Figure 1 Comparison between OP and without OP.
Abbreviations: OP, osteoporosis; cts·min−1, counts per minute.
lists the Pearson’s correlation coefficients of BMD, anthropometric indicators, actigraphy activity, and CAT scores in COPD patients. Age and disease severity (FEV1%) were not significantly correlated with BMD (all P>0.05). Anthropometric indicators (BMI and FFMI) were all significantly correlated with BMD at the lumbar spine, total hip, and femoral neck sites (r=0.701, 0.761, and 0.643; 0.666, 0.719, and 0.628, respectively, all P<0.01). CAT scores were significantly negatively correlated with total hip and femoral neck BMD (r=−0.412, P<0.05; r=−0.552, P<0.01, respectively). DPA was significantly correlated with BMD at the lumbar spine, total hip, and femoral neck sites (r=0.399, 0.602, and 0.438, respectively, all P<0.05). DSI and low SpO2 were not significantly correlated with lumbar spine, total hip, and femoral neck BMD (all P>0.05).
Table 2 Pearson’s correlation coefficients (r) of the bone mineral density, actigraphy activity, and CAT in the patients with COPD (n=30)
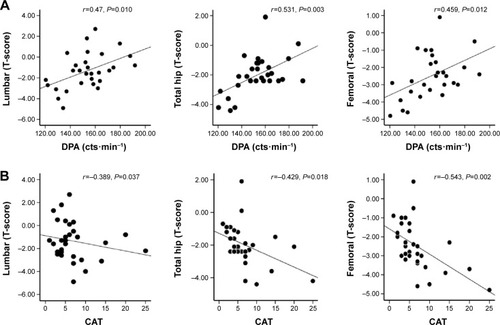
shows that DPA was significantly correlated with lumbar spine, total hip, and femoral neck T-scores (r=0.471, P=0.010; r=0.531, P=0.003; r=0.459, P=0.012, respectively). indicates that CAT scores were significantly negatively correlated with lumbar spine, total hip, and femoral neck T-scores (r=−0.389, P=0.037; r=−0.429, P=0.010; r=−0.543, P=0.002, respectively).
Figure 2 Pearson’s correlation scores of CAT and DPA assessments.
Abbreviations: CAT, COPD assessment test; DPA, daily physical activity; cts·min−1, counts per minute.
shows the multiple linear regression analysis of BMD in COPD patients. Although age, FEV1%, BMI, FFMI, CAT scores, and DPA were subjected to multivariate stepwise linear regression analysis, only BMI and CAT scores were independent factors for BMD. Low BMI was associated with low total hip BMD (β=0.744, P=0.050). A high CAT score was associated with low femoral neck BMD (β=−0.384, P=0.021).
Table 3 Linear regression analysis of bone mineral density in the patients with COPD (N=30)
Discussion
This study revealed two main findings in COPD patients with OP: 1) low DPA and high CAT scores and 2) a relationship between femoral neck BMD and CAT scores.
Lower DPA in COPD patients with OP than in those without OP
This study found that COPD patients with OP had significantly lower DPA than that of those without OP. Physical inactivity is a crucial risk factor for OP, and previous studies have suggested that exercise can prevent bone loss.Citation21,Citation22 The etiology of reduced DPA in COPD patients is multifactorial;Citation23,Citation24 sedentary lifestyles, severe COPD, higher dyspnea severity, worse leg muscle function, and long-term oxygen therapy use were independently associated with lower physical activity.Citation21 These patients may experience dyspnea during exertion, which can lead to a vicious cycle of inactivity, deconditioning, and further increased dyspnea on exertion.Citation12,Citation25 Each of these outcomes, including disability, deconditioning, and low physical activity, has been associated with low BMD and increased fracture risk.Citation26 Our results are further supported by the finding that most of the COPD patients with OP demonstrated lower DPA than did those without OP.
BMD at different sites and OP in COPD patients
COPD and OP share common risk factors, and the relationship among these conditions is complicated. Men with COPD or asthma had lower total hip, femoral neck, and spine BMD compared with healthy controls after adjustment for age, clinic site, BMI, and smoking.Citation27 In 2011, Duckers et al enrolled 30 clinically stable male ex-smokers with COPD and 15 age-matched ex-smoker controls. Their results demonstrated that hip BMD was lower in COPD patients; however, lumbar spineCitation28 measurements were not different. This finding may reflect physical deconditioning or different bone compositions. After adjustment age, sex and FEV1 (%) matched COPD patients with and without OP, our study determined that BMDs at the lumbar spine, total hip, and femoral neck sites were lower in COPD patients with OP. We also observed that patients with OP had lower DPA than that of those without OP. The Cochrane database confirmed that aerobics, weight-bearing, and resistance exercises are effective for improving BMD of the spine in postmenopausal women, and walking improves the BMD of the hip.Citation29 Our study found that DPA was significantly positively correlated with lumbar spine, total hip, and femoral neck BMD (weight-bearing sites). Although a correlation between DPA and BMD was not confirmed in multivariate analysis, the result that might be due to under power, the relation could not be completely excluded in the present study. It is worth testing this with a larger number with adequate power and, more importantly the causative effect. This result is likely supported by the previous finding on the association of reduced physical activity with bone loss in elderly COPD patients. We not only suggest exercise training but also encourage physical activity in COPD patients.
Health status and OP in COPD patients
The CAT has been recommended for assessing the effect of COPD on the health status and daily activities.Citation13 In 2015, Sundh et alCitation30 found several comorbid conditions in COPD patients; in particular, OP was associated with health-related quality of life, as reflected by CAT scores and EuroQol-5 dimension results. In 2014, Watanabe et alCitation31 demonstrated an association between CAT scores and bone loss. We determined that CAT scores were significantly negatively correlated with BMD and DPA. For example, we revealed a relationship between femoral neck BMD and CAT scores but not DPA.
Approximately 35%–60% of patients with moderate-to-severe COPD have low BMIs or evidence of weight loss.Citation32 Previous studies have found that low BMI and FFMI are significantly correlated with OP and BMD.Citation25,Citation33,Citation34 One study suggested that weight loss is a major contributor to decreased BMD in patients with advanced COPD.Citation31 In 2010, Coin et al found that BMIs <25 kg/m2 in COPD patients may indicate OP.Citation35 Our study determined that COPD patients with OP had significantly lower BMI (23.5±3.9 kg/m2) and FFMI (17.4±2.1 kg/m2) than of those without OP.
Inflammation in COPD also leads to a protein catabolic state. FFM is significantly decreased in these patients.Citation36 COPD patients appear to be under a state of continuous systemic inflammation, as suggested by the high levels of CRP, oxidative stress, and other (pro-) inflammatory mediators. Systemic inflammation is associated with OP; a recent study determined that IL-6 is also involved in the regulation of bone turnover and OP development.Citation37 A study assessing the association between systemic inflammation and insulin resistance showed increased insulin resistance in COPD patients compared with healthy people; TNF-α is a well-known stimulator of osteoclastic bone resorption and is involved in postmenopausal OP.Citation38 The most crucial factor in this inflammatory process is smoking. Smoking directly induces systemic damage by lowering the pH of bone tissue, resulting in absorption of bone salts;Citation39 however, it also has indirect systemic effects by the induction of an inflammatory response in the lungs with the production of systemic inflammatory mediators with effects on bone.Citation40 Our results showed no significant differences in all inflammatory markers between the two groups (); these results may be because of ex-smoking in our patients.
A previous study found that low BMD was related to the severity of COPD.Citation30 In 2007, Vrieze et alCitation25 observed that the prevalence of OP was 0% at the GOLD II stage, 9.6% at the GOLD III stage, and 17.9% at the GOLD IV stage. At the GOLD IV stage, 75% of the patients had low BMD. Jørgensen et alCitation41 found that 68% of 62 COPD patients with a mean FEV1 of 33% had osteopenia or OP. Our study determined that BMD was not significantly correlated with FEV1 (%). This may be because the prevalence of OP was only 10% at the GOLD IV stage.
Limitations
This study has some limitations. First, this study had a small sample size and used CAT scores to retrospectively estimate power (43%); although power was low, the CAT scores were still significantly different between the two groups (). Overall, the scores should be investigated further. Second, the study sample was drawn from one hospital. No control group was used for comparison or to analyze the severity of the effects. Third, the present study involved only 24-hour ambulatory actigraphy and oximetry. The applicability of these results to longer periods of actigraphy and oximetry requires further investigation. Fourth, most patients referred to this center were male; hence, we could not assess the effect of sex. Finally, this study could have benefited from using one device to simultaneously record oxygenation and DPA.
Conclusion
Our study determined that low DPA and high CAT scores were significantly correlated with low BMD and OP, especially between femoral neck BMD and high CAT scores in COPD patients. Future studies are necessary to longitudinally assess determinants of OP in COPD patients.
Acknowledgments
The authors wish to thank the patients and personnel of the hospital unit for their cooperation during the course of this study. The study was supported by grants from the Chang Gung Memorial Hospital (CMRPG3B0011~3), Ministry of Science and Technology (MOST 103-2314-B-038-066-), and the Taipei Medical University (TMU102-AE1-B45).
Disclosure
The authors declare that they have not had any financial compensation and report no conflict of interest in this work.
References
- KiyokawaHMuroSOgumaTImpact of COPD exacerbations on osteoporosis assessed by chest CT scanCOPD20129323524222360380
- GanWQManSFSenthilselvanASinDDAssociation between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysisThorax200459757458015223864
- VernooyJHKucukaycanMJacobsJALocal and systemic inflammation in patients with chronic obstructive pulmonary disease: soluble tumor necrosis factor receptors are increased in sputumAm J Respir Crit Care Med200216691218122412403691
- LeeKYHoSCChanYFReduced nuclear factor-kappa B repressing factor: a link toward systemic inflammation in COPDEur Respir J201240486387322441735
- Graat-VerboomLWoutersEFSmeenkFWCurrent status of research on osteoporosis in COPD: a systematic reviewEur Respir J200934120921819567604
- LeechJADulbergCKellieSPatteeLGayJRelationship of lung function to severity of osteoporosis in womenAm Rev Respir Dis1990141168712297189
- BiskobingDMCOPD and osteoporosisChest2002121260962011834678
- CummingsSRBatesDBlackDMClinical use of bone densitometry: scientific reviewJAMA2002288151889189712377088
- LehouckABoonenSDecramerMJanssensWCOPD, bone metabolism, and osteoporosisChest2011139364865721362651
- TroostersTSciurbaFBattagliaSPhysical inactivity in patients with COPD, a controlled multi-center pilot-studyRespir Med201010471005101120167463
- WatzHWaschkiBMeyerTPhysical activity in patients with COPDEur Respir J200933226227219010994
- KatajistoMKupiainenHRantanenPPhysical inactivity in COPD and increased patient perception of dyspneaInt J Chron Obstruct Pulmon Dis2012774375523152679
- JonesPWHardingGBerryPDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
- TsiligianniIGvan der MolenTMoraitakiDAssessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ)BMC Pulm Med2012122022607459
- JonesPWTabbererMChenWHCreating scenarios of the impact of COPD and their relationship to COPD Assessment Test (CAT) scoresBMC Pulm Med2011114221835018
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- HsuMFHoSCKuoHPMini-nutritional assessment (MNA) is useful for assessing the nutritional status of patients with chronic obstructive pulmonary disease: a cross-sectional studyCOPD201411332533224475999
- GrutschJFWoodPADu-QuitonJValidation of actigraphy to assess circadian organization and sleep quality in patients with advanced lung cancerJ Circadian Rhythms20119421592392
- CasanovaCHernandezMCSanchezATwenty-four-hour ambulatory oximetry monitoring in COPD patients with moderate hypoxemiaRespir Care200651121416142317134522
- No authors listedPrevention and management of osteoporosisWorld Health Organ Tech Rep Ser20039211164 back cover15293701
- de KamDSmuldersEWeerdesteynVSmits-EngelsmanBCExercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trialsOsteoporos Int200920122111212519421702
- SarkarMBhardwajRMadabhaviIKhatanaJOsteoporosis in chronic obstructive pulmonary diseaseClin Med Insights Circ Respir Pulm Med2015952125788838
- PittaFTroostersTProbstVSPotential consequences for stable chronic obstructive pulmonary disease patients who do not get the recommended minimum daily amount of physical activityJ Bras Pneumol200632430130817268729
- PalangePForteSOnoratiPVentilatory and metabolic adaptations to walking and cycling in patients with COPDJ Appl Physiol (1985)20008851715172010797134
- VriezeAde GreefMHWijkstraPJWempeJBLow bone mineral density in COPD patients related to worse lung function, low weight and decreased fat-free massOsteoporos Int20071891197120217347789
- HendersonNKWhiteCPEismanJAThe roles of exercise and fall risk reduction in the prevention of osteoporosisEndocrinol Metab Clin North Am19982723693879669143
- DamTTHarrisonSFinkHABone mineral density and fractures in older men with chronic obstructive pulmonary disease or asthmaOsteoporos Int20102181341134919816753
- DuckersJMEvansBAFraserWDLow bone mineral density in men with chronic obstructive pulmonary diseaseRespir Res20111210121812978
- HoweTESheaBDawsonLJExercise for preventing and treating osteoporosis in postmenopausal womenCochrane Database Syst Rev20117CD00033321735380
- SundhJJohanssonGLarssonKComorbidity and health-related quality of life in patients with severe chronic obstructive pulmonary disease attending Swedish secondary care unitsInt J Chron Obstruct Pulmon Dis20151017318325653516
- WatanabeRTanakaTAitaKOsteoporosis is highly prevalent in Japanese males with chronic obstructive pulmonary disease and is associated with deteriorated pulmonary functionJ Bone Miner Metab201533439240024996527
- BerryJKBaumCReversal of chronic obstructive pulmonary disease-associated weight loss: are there pharmacological treatment options?Drugs200464101041105215139785
- BoltonCEIonescuAAShielsKMAssociated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2004170121286129315374843
- IncalziRACaradonnaPRanieriPCorrelates of osteoporosis in chronic obstructive pulmonary diseaseRespir Med200094111079108411127495
- CoinASergiGMarinSPredictors of low bone mineral density in elderly males with chronic obstructive pulmonary disease: the role of body mass indexAging Male201013214214720429721
- VestboJPrescottEAlmdalTBody mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart StudyAm J Respir Crit Care Med20061731798316368793
- BoltonCEEvansMIonescuAAInsulin resistance and inflammation – A further systemic complication of COPDCOPD20074212112617530505
- ForliLMellbyeOJHalseJCytokines, bone turnover markers and weight change in candidates for lung transplantationPulm Pharmacol Ther200821118819517419084
- DaniellHWOsteoporosis and smokingJAMA197222155095067964
- AgustiAGNogueraASauledaJSystemic effects of chronic obstructive pulmonary diseaseEur Respir J200321234736012608452
- JorgensenNRSchwarzPHolmeIThe prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional studyRespir Med2007101117718516677808
