Abstract
Lanthanum carbonate is an efficacious noncalcium, nonresin phosphate-binder that is being increasingly used in chronic kidney disease stage 5 (CKD-5) dialysis patients. Available evidence has indicated that QT interval changes correlate with mortality in healthy subjects and in dialysis patients. Experimental studies have suggested the possibility that lanthanum carbonate may produce prolongation of the QT interval. This is not accepted by other authors. There is no data confirming this in prospective clinical studies. The goal of this study was to verify the effect of lanthanum carbonate on the QT interval of the electrocardiogram (EKG) tracing.
Material and methods
We studied 25 hemodialyzed patients. After a six-month run-in period, with aluminum-hydroxide, lanthanum carbonate was administered at increasing doses: 500 mg twice a day for week 1; 750 mg, twice daily during week 2; 1000 mg twice daily during week 3; and 1000 mg three times daily during week 4. EKGs were recorded on patients prior to and 3 hours following each dialysis treatment. Assessments were made of differences in body weight; systolic blood pressure; diastolic blood pressure; length of PR and QRS complex; heart rate; QT; QT-c; QT-d; and axis of wave P, QRS complex and T using lanthanum carbonate at increasing doses.
Results
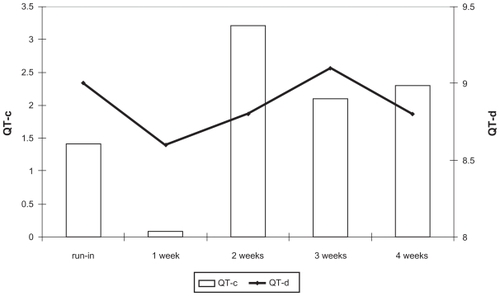
QT-c is before dialysis session during run-in 431 ± 20 msec with variation by −9 to + 1 msec (P = not significant [NS]) during lanthanum use; and 437 ± 25 msec after dialysis session with variation by −6 to −1 msec (P = NS) during lanthanum use. Any difference was observed during study among before and after dialysis session in QT-c (difference by 0.09 to 3.2%) (P = NS); and QT-d (difference by 8.6 to 9.1%) (P = NS).
Conclusion
Our study shows that lanthanum carbonate administration, at increasing doses, did not modify the EKG parameters. This effect is observed both in predialysis and in postdialysis recordings. Further studies are necessary with more prolonged observations.
Introduction
As documented by the United States Renal Data System, congestive heart failure and sudden death are the most frequent causes of cardiovascular death in chronic kidney disease stage 5 (CKD-5), followed by acute myocardial infarction, stroke, and peripheral arterial disease (http://www.usrds.org/2006/ref/H_morte_06.pdf). Different factors have been investigated to explain the pathogenesis of cardiac arrhythmias that lead to sudden cardiac death (SCD) in hemodialysis.Citation1 In particular, coronary artery disease (CAD), arterial hypertension, congestive heart failure, autonomic neuropathy and uremic cardiomyopathies might induce a significant cardiac remodeling that affects number and functionality of cardiac ion channels.Citation1 Specifically, it has been postulated that patients undergoing hemodialysis might experience a progressive diminution and inhibition of the potassium channels that might lead to a reduction of the “cardiac repolarization reserve”.Citation1 In addition, several drugs and the acute changes in levels of serum calcium and potassium that occur during a dialysis session further exacerbate the risk of cardiac arrhythmias as documented by changes in the QT tract on electrocardiogram (EKG) (http://www.qtdrugs.org).Citation2–Citation5
Some experimental studiesCitation6,Citation7 have suggested the possibility that lanthanum carbonate may produce extension of QT intervals. This is not accepted by other authors.Citation8,Citation9 Lanthanum carbonate is an efficacious noncalcium, nonresin phosphate-binder increasingly used in CKD-5 dialysis- patients; and there is no data confirming this in prospective clinical studies.
The goal of this study was to verify the effect of lanthanum carbonate on QT interval changes on EKG recordings in patients with CKD-5 undergoing hemodialysis.
Materials and methods
A total of 25 CKD-5 hemodialysis patients participated this four-week study. Following a six-month run-in period with aluminum-hydroxide, patients received lanthanum carbonate. Aluminum hydroxide is not a preferred phosphate-binder in our dialysis center. It was used in this study protocol because it is known not to influence QT interval changes. The temporary use of aluminum hydroxide did not cause dementia or other neurological disease in the patients. All patients introduced the lanthanum carbonate dose as prescribed, and this is shown by the blood phosphorus and confirmed by radiographies of the abdomen that showed the presence of lanthanum.
Lanthanum carbonate was administered at a dose 500 mg twice daily during week 1; 750 mg twice daily during week 2; 1000 mg twice a day during week 3; and 1000 mg three times daily during week 4. The dose of lanthanum carbonate was increased regardless of serum phosphate in order to investigate the influence of the drug and if there was a dose response.
EKGs were run on each patient before and three-hours after each dialysis session. The EKG reader was blinded to the lanthanum carbonate dose.
Patients were included if they were adults over the age of 18 years on hemodialysis treatment and currently on phosphate-binders. Exclusion criteria included concomitant acute illness or history of cardiac arrhythmia, liver dysfunction and hypothyroidism, and use of drugs that prolong the QT interval. Written informed consent was obtained from all participants before study-related procedures were performed and after approval from each institutional Ethical Review Board. All procedures involved in the study were conducted in adherence to the Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects.
Investigators were instructed to control blood pressure (≤130/80 mmHg), anemia (hemoglobin [Hb] > 11 g/dL, transferrin saturation [TSAT] > 20%), acidosis (bicarbonate [HCO3] between 20–24 mmol/L), diabetes (glycated hemoglobin [HbA1c] < 7.0%), dyslispidemia (total cholesterol <200 mg/dL; low-density lipoprotein [LDL] cholesterol <100 mg/dL; triglycerides < 180 mg/dL), and parameters of bone mineral metabolism (serum phosphorous, calcium, and intact parathyroid hormone [iPTH] between 2.5–5.0 mg/dL; 8.0–9.9 mg/dL, and 150–300 pg/mL respectively) according to current guidelines.
Routine biochemical laboratory measurements were obtained at baseline and at six months intervals. All blood samples were taken before the midweek dialysis session and after 12 hours fasting. Serum parameters of mineral metabolism, electrolytes, inflammation, anemia, liver function, and dialysis adequacy were performed by the facilities’ usual laboratories.
The bath of dialysis contained calcium at dose of 1.25 mmol/L and potassium at dose of 3 mmol/L.
QT interval and QT dispersion was assessed on a 12-channel recorder (Esaote-Biomedicals, Genova, Italy) at a paper speed and gain of 25 mm/sec and 10 mm/mV, respectively. Citation10 The QT interval was measured by one single observer as the distance between the beginning of the QRS complex and the end of the T wave. Moreover, each QT interval was also corrected for the heart rate using the Bazett’s formula (QTc = QT/RR). The difference between the maximum QTc and the minimum QTc was also calculated and represents the corrected QT interval dispersion (QTcd). The P, QRS, and T axes were measured. The electrocardiograms were effected before and three hours after the second weekly dialysis session.
Statistical methods
Demographic, clinical and laboratory characteristics were collected at enrollment and at the end of study.
Data are expressed as mean ± standard deviation unless otherwise specified. A t-test was used to compare the run-in period and the end of the study. Analysis of variance (ANOVA) were used to verify the variations of QT-c and QT-d, and axis of P wave, QRS complex, and T wave during the lanthanum administration. A P-value of less than 0.05 was considered statistically significant.
Results
Demographic, clinical and laboratory characteristics of patients are summarized in . Patients were 66.2 ± 8.5 years of age, 68% were males, 44% had cerebro-cardio-vascular disease, 84% with hypertension, and 32% were diabetic. Serum phosphorus dropped by the end of the study (P < 0.001); and LDL-cholesterol increased following lanthanum carbonate use (P < 0.018). shows the data weekly collected in the predialysis session during run-in and following the study: any difference there is regarding BW;SBP; DBP; length of PR and QRS complex; heart rate; QT; QT-c; QT-d; and axis of wave P, QRS complex, and T in patients using lanthanum carbonate at increased doses.
Table 1 Demographic and clinical characteristic of the study cohort
Table 2 The EKG data following study in predialysis
Similarly, shows the data collected weekly in postdialysis sessions: showing any difference there is regarding BW; SBP; DBP; length of PR and QRS complex; heart rate; QT; QT-c; QT-d; and axis of wave P, QRS complex, and T using lanthanum carbonate at increase doses.
Table 3 The electrocardiogram data following study in postdialysis
Particularly, QT-c was generated prior to the dialysis session during run-in 431 ± 20 msec with variation by −9 to +1 msec (P = not significant [NS]) during lanthanum carbonate use; and 437 ± 25 msec after the dialysis session with a variation by −6 to −1 msec (P = NS) during lanthanum carbonate use. shows the differences during the study before and after the dialysis session in QT-c (difference by 0.09 to 3.2%) (P = NS); and QT-d (difference by 8.6 to 9.1%) (P = NS).
Discussion
Previous papers have indicated that the QT interval correlates with mortality in healthy subjects.Citation11–Citation15 Similar observations have been shown in dialysis patients.Citation16,Citation17 Several papers have demonstrated that dialysis treatment increases the QT interval.Citation1–Citation5 Specifically, it has been postulated that patients undergoing hemodialysis might experience a progressive diminution and inhibition of the potassium channels that might lead to a reduction of the “cardiac repolarization reserve”.Citation1 Nonetheless, several routinely-used drugs can increase the QT interval, such as cisapride,Citation18,Citation19 erythromycin,Citation20 antipsychotic drugs,Citation21 sotalol and quinidine,Citation22 ibuprofen,Citation23 and aliskerin.Citation24 Patients on dialysis treatment must use phosphatebinders. Lanthanum carbonate is an oral noncalcium, nonresin phosphate-binder widely used in end-stage renal disease. Experimental studiesCitation6,Citation7 have suggested the possibility that lanthanum carbonate may produce extension of the QT interval. This evidence isn’t accepted by other authors.Citation8,Citation9 To date, we have no clinical studies focused on the effects of lanthanum carbonate on QT interval changes in dialysis patients.
Our study shows that acute lanthanum carbonate administration, at increasing doses, does not modify the EKG parameters. This effect is observed both in predialysis and in postdialysis recordings. It underlines the absence of negative effects of lanthanum carbonate on the QT interval in acute administration of the drug for a four-week time period with increasing doses.
A few limitations have to be taken into account when these results are interpreted. Indeed, the relatively small sample size and the low reproducibility of the mean QT dispersion limit the ability to generalize these findings. However, the same patients represent the control group, and it isn’t temerity to draw conclusions from only 25 patients on dialysis, just considering the enormous diversity of these patients. The time of lanthanum carbonate administration was short, but the data demonstrated, diversely from preliminary pathophysiology data, that acute administration did not increase the QT interval.
Furthermore, though prospective, this is not a randomized trial and potential confounders might have influenced our results. Therefore further studies are required to confirm that the chronic use of lanthanum carbonate does not increase the QT interval.
Disclosure
The authors report no conflicts of interest in this work.
References
- GussakIGussakHMSudden cardiac death in nephrology: focus on acquired long QT syndromeNephrol Dial Transplant200722121417093009
- StewartGAGansevoortRTMarkPBElectrocardiographic abnormalities and uremic cardiomiopathyKidney Int20056721722615610245
- MorrisSTWGaliatsouEGStewartGAQT dispersion before and after hemodialysisJ Am Soc Nephrol19991601639890322
- CovicADiaconitaMGusbeth-TatomirPHemodialysis increases QT interval but not QTc dispersion in ESRD patients without manifest cardiac diseaseNephrol Dial Tranplant20021721702177
- GenovesiSDossiCViganòMRElectrolyte concentration during haemodialysis and QT interval prolongation in uraemic patientsEuropace20081077177718287086
- PalaszACzekajPToxicological and cytophysiological aspects of lanthanides actionActa Biochimica Polonica2000471107111411996100
- PrzywaraDBhaveSBhaveAActivation of K channels by lanthanum contributes to the block of neurotransmitter release in chick and rat sympathetic neuronsJ Membr Biol19921251551621552563
- HutchisonAJBarnettMEKrauseRKwanJTCSiamiGALanthanum carbonate treatment, for up to 6 years, is not associated with adverse effects on the liver in patients with chronic kidney disease Stage 5 receiving hemodialysisClin Nephrol20097128629519281739
- ShigematsuTLanthanum carbonate effectively controls serum phosphate without affecting serum calcium levels in patients undergoing hemodialysisTher Apher Dial2008121556118257813
- GlancyJMWestonPJBhullarHKReproducibility and automatic measurement of QT dispersionEur Heart J199617103510398809521
- StrausSMJMKorsJADe BruinMLProlonged QTc interval and risk of sudden cardiac death in a population of older adultsJ Am Coll Cardiol20064736236716412861
- ElmingHHolmEJunLThe prognostic value of the QT interval and QT interval dispersion in all-cause and cardiac mortality and morbidity in a population of Danish citizensEur Heart J199819139114009792266
- DekkerJMSchoutenEGKlootwijkPAssociation between QT interval and coronary heart disease in middle-aged and elderly men. The Zupten studyCirculation1994907797858044948
- SchoutenEGDekkerJMMeppelinkPQT interval prolongation predicts cardiovascular mortality in an apparently healthy populationCirculation199184151615231914093
- MontanezARuskinJNHebertPRProlonged QTc interval and risks of total and cardiovascular mortality and sudden death in the general populationArch Intern Med200416494394815136301
- BeaubienERPylypchukGBAkhtarJBiemHJValue of corrected QT interval dispersion in identifying patients initiating dialysis at increased risk of total and cardiovascular mortalityAm J Kidney Dis20023983484211920351
- WuVYulinLWuKQT interval dispersion in dialysis patientsNephrology20051010911015877667
- HentgesMJGundersonBWLewisMJRetrospective analysis of cisapride-induced QT changes in ESRD patientsNephrol Dial Transplant2000151814181811071970
- MathisASCosteasCBaroneJARetrospective analysis of the effects of cisapride on the QT interval and QT dispersion in chronic hemodialysis patientsAm J Kidney Dis2001381284129111728962
- ObergKCBaumanJLQT interval prolongation and torsade de punta due to erythromycin lactobionatePharmacotherapy1995156876928602374
- HaddadPMAndersonIMAntipsychotic-related QTc prolongation, torsade de punta and sudden deathDrugs2002621649167112109926
- TongKLLauYSTeoWSA case series of drug-induced long QT syndrome and torsade de puntaSingapore Med J20014256657011989578
- YangZWangHZhengYPossible arrhythmiogenic mechanism produced by ibuprofenActa Pharm Sinica200829421429
- PeitzGJMaleskerMASojkaSGAliskerin-induced QT interval prolongationSouth Med J200910241141219279548