Abstract
We report a case of 22-year-old primigravida presented to Women’s Hospital – Hamad Medical Corporation emergency with severe epigastric pain, nausea, and vomiting. On admission, she was dehydrated with remarkably worsening symptoms. Laboratory findings revealed significantly elevated liver enzymes with unknown etiology. Her past medical history showed an admission for nausea and vomiting 3 weeks previously and she was discharged on antiemetics, and esomeprazole for the first time. Due to the predominantly elevated liver enzymes, the clinical pharmacist discussed the possibility of esomeprazole-induced adverse effects and suggested to suspend esomeprazole based on the evidence from literature review. The liver enzymes showed a substantial improvement within days after the discontinuation of the drug; however, a rechallenge was not done since it could have adversely affected the mother or the fetus. Using the Naranjo Adverse Drug Reaction Probability scales, the adverse reaction due to esomeprazole was classified as “probably”.
Introduction
Drug-induced hepatic toxicity is one of the most common causes of liver injury, accounting for almost one-half of all the liver failure and mimics all forms of liver disease. Approximately >1000 medications have been reported to cause liver disease at least one time. However, majority of these liver diseases subside after suspension of the drug, while very few of them have been reported to cause a permanent harm. The majority of drug-induced hepatic adverse events are unpredictable and are either immune-mediated hypersensitivity reactions or idiosyncratic.Citation1,Citation2
Esomeprazole is an S-isomer of omeprazole and is generally considered safe and effective to treat acid suppression during pregnancy.Citation3–Citation5 However, US Food and Drug Administration classified it as Category C, which explains that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies on humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.Citation6
We report a case of probable esomeprazole-induced transient liver injury (elevated liver transaminases, i.e., alanine transaminase [ALT] and aspartate transaminase [AST]) in a pregnant woman which resolved after discontinuation of the suspected drug. A literature search of standard databases (MEDLINE, Embase, and Cumulative Index to Nursing and Allied Health Literature) conducted in September 2015 did not identify any similar reports in pregnant population.
Impact on practice
Health professionals treating hyperemesis gravidarum or gastric refluxes should be aware of potential esomeprazole-induced liver toxicities.
Liver enzyme levels should be carefully monitored while prescribing esomeprazole to a pregnant woman.
Case presentation
No informed consent was required from the patient to publish this report due to its anonymous nature. This waiver of informed consent and all approvals to publish and present this case was obtained from the Medical Research Centre at Hamad Medical Corporation (HMC).
A 22-year-old primigravida in her first trimester presented to Women’s Hospital – HMC emergency with acute epigastric pain, nausea, and nonbilious vomiting more than four times in last 24 hours. Her past medical history revealed that 3 weeks previously (considered as Day 0 in ), she was admitted to the hospital and was diagnosed as hyperemesis gravidarum and was later discharged on pyridoxine, metoclopramide, and esomeprazole. The patient had no known diagnosis of liver injury/disease prior to the onset of this illness and denied history of any recreational drug use, nonprescription, or use of herbal supplements. Prior to current admission (Day 1), she was taking esomeprazole 40 mg twice daily, metoclopramide suppositories 20 mg twice daily, and pyridoxine 40 mg orally once daily and had no history of drug allergies or other adverse drug reactions.
Figure 1 Elevated liver enzymes with esomeprazole.
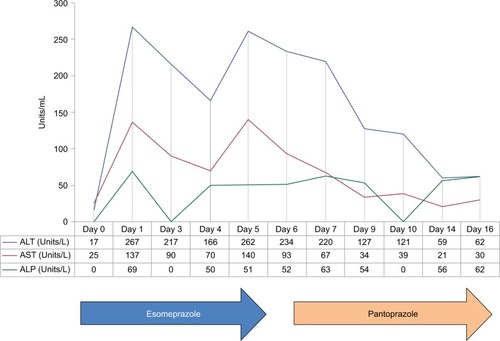
At this time, the patient continued to complain of significant nausea, vomiting, poor appetite, significant weight loss, and darkish yellow urine. On examination, she was dehydrated, no signs of ascites or edema, impalpable spleen; however, severe tenderness was observed in the epigastric area. Laboratory investigation revealed significantly elevated ALT (267 Units/L) and AST (137 Units/L; ). HIV testing was negative. A deferential diagnosis was made as Mallory–Weiss tear (diagnosed clinically) and hyperemesis gravidarum versus viral/autoimmune liver disease or drug-induced liver injury (DILI). Viral hepatitis screening test and other tests including anti-smooth muscle antibody, antimitochondria antibody, antinuclear antibody, and antiliver kidney microsomal antibodies were done.
This reaction (elevated liver enzymes) was identified by the clinical pharmacist who discussed the possibility of an esomeprazole-induced adverse effect. The outcome of the discussion resulted in discontinuing esomeprazole (Day 5) and replacing it with oral pantoprazole 40 mg twice daily. This change in therapy had almost immediate impact, with liver enzymes having dropped predominantly in successive days, without any other intervention. Approximately 3 days (Day 7) after stopping esomeprazole, subsequent laboratory reports demonstrated that patient’s AST, ALT, and alkaline phosphatase were significantly reduced. The patient reported a substantial improvement in her activity levels with resolution of nausea and vomiting and epigastric pain, and she was discharged on Day 10. On discharge, she was prescribed with pantoprazole 40 mg and metoclopramide suppositories 20 mg and was asked to follow-up after a week. During her subsequent follow-up visit on Day 16, the liver functions were found to be normal.
Using the Naranjo Adverse Drug Reaction Probability scales, a score of 6 was obtained indicating a “probable” adverse reaction due to esomeprazole. The patient was instructed never to rechallenge herself with esomeprazole and instructed to report it as a medication adverse reaction in the future.
Discussion
To our knowledge, this is the first published report of oral esomeprazole-induced liver injury in a pregnant patient. While the pathophysiology of DILI is poorly understood, some of the possible mechanisms for drug-induced hepatotoxicity include 1) impaired intracellular calcium hemostasis, leading to disassembly of actin fibrils and resulting in bulging of cell membrane to cause rupture and cell lysis; 2) Drug-induced hepatotoxicity is also caused due to loss of villous processes and the disruption of transport pumps, for example, MRP3 that prevents the excretion of bilirubin and other organic compounds; 3) Sometimes due to stimulation of apoptotic pathways by tumor necrosis factor alpha (TNF-α), receptor or Fas may trigger the cascade of intercellular caspases. Certain drugs are known to cause mitochondrial dysfunction by reducing the ATP production and disturbing the respiratory chain enzyme and hence causing hepatic toxicity. DILI is known as the most common cause of liver injury and main cause of drug withdrawal. It is known that >50% of all acute liver failures and ~10% of all acute hepatitis cases are due to drugs.Citation2,Citation7,Citation8 There are two main types of hepatic toxicity, one is the immune response to the drug trigger and the other is direct action of the drug itself. Esomeprazole induces drug injury and is more of a direct toxicity because when the drug is withdrawn, the pathologic findings were resolved. Authors have also assumed the role of immune system in the current case because of the delayed nature of the reaction and resolution. Although, direct destruction of liver epithelium by drugs has been reported previously with acetaminophen, it might also occur in other medications. This type of injury may result in altered salt homeostasis, mitochondrial dysfunction, and cell death. Rechallenge here is not recommended since a recurrent injury may be more severe than the first episode and might adversely affect the fetus too.
A search on UK MHRA and MedEffect Canada and a literature review of standard databases (MEDLINE, Embase, and Cumulative Index to Nursing and Allied Health Literature) conducted in September 2015 did not identify any similar reports in pregnant women. Rare but previously reported esomeprazole-induced liver injury has occurred in male population or with other underlining conditions; however, no such reports were reported in pregnant population till date.
Capitain et alCitation9 reported liver toxicity in a patient receiving chemotherapy, for breast cancer, after single administration of esomeprazole. Upon withdrawal of esomeprazole, liver enzymes returned to normal even after the continuation of the chemotherapy. In another two studies, omeprazole was the main cause of DILI reported.Citation10,Citation11 A similar case of transient hepatic injury that resolved soon after esomeprazole was discontinued following a negative work up against viral infection or autoimmune disease, the dose-dependent elevation of ALT and AST, and return of liver enzymes to normal after switching to another proton pump inhibitor (PPI) (omeprazole) was also reported.
Esomeprazole is the S-isomer of omeprazole. Both esomeprazole and pantoprazole are metabolized through CYP 450 enzymes, and they are known enzyme inhibitors for their own metabolism. Therefore, higher areas under the curve (AUC) are attained with continuous use. Once metabolized, hydroxy, 5-O-desmethyl, and sulfone metabolites are formed. However, the formation of hydroxy metabolite is slower, and the formation of the other two metabolites is more rapid in esomeprazole compared to pantoprazole.Citation12 Hence, the formation of metabolites might explain the toxic effect on the liver and support the direct liver injury over immune reaction. Pantoprazole has not shown a similar metabolism and does not inhibit its metabolism. The diversity in metabolic pathways may explain in part the different consequence on liver functions between PPIs.Citation12,Citation13
Conclusion
A case of probable esomeprazole-induced transient liver injury in pregnant women was reported. It is important for health care professionals to be aware of this rare but significantly harm producing event in pregnancy. This case has been reported to Medication Safety Office and Drug Information services – Women’s Hospital Medication safety office and Drug Information services. Authors recommend that future cases of suspected esomeprazole-induced hepatotoxicity should be reported and efforts to delineate the mechanism of injury should be undertaken.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. BT is a Doctoral (PhD) Researcher from RGU, UK, and Clinical Pharmacy Specialist at HMC and was involved in manuscript writing and literature review. MGM is a senior researcher at Weil Cornell Medical College, Qatar, and Clinical Pharmacist at HMC, he intervened in the case and was involved in manuscript writing. WEK is the medication safety officer at HMC and was involved in the Naranjo Scale Evaluation, data analysis and revision of manuscript. MAH and PAR are senior administrators at HMC and were involved in writing the initial proposal, rewriting and editing manuscript. RMW, SBH, and KO are obstetric physicians whose contributions were vital in the clinical interventions made, and writing up for the discussion and reviewing the histological and other laboratory interpretation.
Acknowledgments
Authors would like to acknowledge GI team, Hamad Medical Corporation for their valuable clinical decisions and Dr Thaslim Abdul Rahman, Robert Gordon University, UK, for his assistance in the case report. Authors would further like to thank Dr Doua Al Saad for her contribution to the case report.
Disclosure
The authors report no conflicts of interest in this work.
References
- ZimmermanHJHepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the LiverPhiladelphiaLippincott Williams & Wilkins1999
- KaplowitzNDrug-induced liver disordersDrug Safety200124748349011444721
- SpencerCMFauldsDEsomeprazoleDrugs2000602321329 discussion 330–110983736
- DaviesMWiltonLVShakirSASafety profile of esomeprazoleDrug Safety200831431332318366242
- MajithiaRJohnsonDAAre proton pump inhibitors safe during pregnancy and lactation?Drugs201272217117922239714
- The U.S. Food and Drug Administration [homepage on the Internet]Nexium (Esomeprazole Magnesium)2015 Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm431648.htmAccessed September 28, 2015
- FontanaRJHayashiPHGuJIdiosyncratic drug-induced liver injury is associated with substantial morbidity and mortality within 6 months from onsetGastroenterology2014147196.e108.e24681128
- LeeWMDrug-induced hepatotoxicityN Engl J Med2003349547448512890847
- CapitainOLortholaryAAbadie-LacourtoisieSCytolytic hepatitis and esomeprazole during chemotherapyPresse Med200534171235123616230965
- KourySStoneCLa ChariteDOmeprazole and the development of acute hepatitisEur J Emerg Med1998544674709919455
- SuganoKKinoshitaYMiwaHTakeuchiTEsomeprazole NSAID Preventive Study GroupSafety and efficacy of long-term esomeprazole 20 mg in Japanese patients with a history of peptic ulcer receiving daily non-steroidal anti-inflammatory drugsBMC Gastroenterol2013135423530709
- AnderssonTHassan-AlinMHasselgrenGRöhssKWeidolfLPharmacokinetic studies with esomeprazole, the (S)-isomer of omeprazoleClin Pharmacokinet200140641142611475467
- Romero-GomezMOteroMSuarez-GarciaEDiazEGFobeloMCastro-FernandezMAcute hepatitis related to omeprazoleAm J Gastroenterol19999441119112010201510
