Abstract
Background
This study was conducted to explore whether the effect of edaravone (5-methyl-2-phenyl-2,4-dihydro-3H-pyrazol3-one, EDR) can ameliorate renal warm ischemia-reperfusion injury (IRI) by modulating endoplasmic reticulum stress (ERS) and its downstream effector after cardiac arrest (CA) and cardiopulmonary resuscitation (CPR) in a rat model.
Methods
The rats (n=10) experienced anaesthesia and intubation followed by no CA inducement were defined as the Sham group. Transoesophageal alternating current stimulation was employed to establish 8 min of CA followed by conventional CPR for a resuscitation model. The rats with successful restoration of spontaneous circulation (ROSC) randomly received EDR (3 mg/kg, EDR group, n=10) or equal volume normal saline solution (the NS group, n=10). At 24 hr after ROSC, serum creatinine (SCR), blood urea nitrogen (BUN) levels, and cystatin-C (Cys-C) levels were determined and the protein level of glucose-regulated protein (GRP78), C/EBP homologous protein (CHOP), extracellular signal-regulated kinase (ERK), phosphorylated extracellular signal-regulated kinase 1/2 (p-ERK1/2), Bax/Bcl-2, and caspase-3 were detected by Western blot method.
Results
At 24 hrs after ROSC, SCR, BUN and Cys-C were obviously increased and the proteins expression, including GRP78, CHOP and p-ERK1/2, cleaved-caspase 3 Bax/Bcl-2 ratio, were significantly upregulated in the NS group compared with the Sham group (p<0.05). The remarkable improvement of these adverse outcomes was observed in the EDR group (p<0.05).
Conclusion
In conclusion, we found that EDR ameliorates renal warm IRI by downregulating ERS and its downstream effectors in a rat AKI model evoked by CA/CPR. These data may provide evidence for future therapeutic benefits of EDR against AKI induced by CA/CPR.
Introduction
During ischemia, multiple signalling pathways, which are closely relative with inflammatory and metabolic, play pro-apoptosis roles in cells.Citation1 However, the subsequent blood perfusion restoration may course more severe injury known as ischemia-reperfusion injury (IRI). Renal ischaemia-reperfusion injury (IRI) is known as one of the most common causes of acute kidney injury (AKI) and secondary to various clinical conditions, such as kidney grafting and resuscitation.Citation2,Citation3 Reactive oxygen species (ROS) play an important role in the development of IRI. It has been reported that ROS burst induces endoplasmic reticulum stress (ERS), mitogen-activated protein kinases (MAPK) and cell death.Citation4,Citation5
ER is an intracellular organelle that plays a pivotal role in protein synthesis and folding, Ca2+ storage and signalling.Citation6 As ER is stimulated by Ca2+ overload, ischaemia or hypoxia, its homeostasis changes followed by ERS.Citation7 Growing evidences showed that when the stimuli is excessive or persistent, ERS of renal tubule epithelial cells is an initial response and plays a major pathogenic role in renal IRI.Citation8–Citation10 Thus, ERS inhibition may be a novel treatment for renal IRI.
Extracellular signal-regulated kinase 1/2 (ERK1/2) is a MAPK that is phosphorylated rapidly following renal injury.Citation11 As a downstream effector mechanism of ERS, activation of ERK1/2 has been suggested to be a regulator of renal IRI.Citation12–Citation15 For example, ERS may course cell death at least by a classical BAX/BAK-dependent apoptotic response that can be inhibited by the ERK1/2 signalling pathway.Citation16 However, it is unclear whether the ERS could modulate the ERK signalling pathways to ameliorate renal warm IRI evoked by the process of cardiac arrest/cardiopulmonary resuscitation (CA/CPR).
Edaravone (5-methyl-2-phenyl-2,4-dihydro-3H-pyrazol3-one, EDR) is a novel free-radical scavenger that has been shown to prevent ERS induced by hypoxia and ischaemia.Citation17,Citation18 Although EDR is identified most recently as a protective factor for the development of renal IRI caused by renal arterial or hilar clamping,Citation19–Citation21 poor evidence can answer that whether EDR has the same protective effect in renal warm IRI evoked by CA/CPR. Experimental evidence suggests that GRP78 and CHOP activation is correlated with apoptosis as an ERS downstream event in renal IRI, and ERK activation is an important downstream mechanism of ERS. Therefore, we aimed to verify the hypothesis that EDR play a protective role on renal IRI by downregulated GRP78/CHOP/ERK pathway in a rat CA/CPR model.
Materials and Methods
Preparation of Experimental Rats
This animal study was approved by the Animal Ethics Committee of Guangxi Medical University (Animal Experimental Ethical Inspection no. 201811030). All animals received treatment in strict adherence to the National Research Council’s 1996 Guidelines for the Care and Use of Laboratory Animals. Anaesthetics were titrated in all surgical procedures to avoid unnecessary pain. Male Sprague-Dawley rats weighing 200–230 g were purchased from the Experimental Animal Center of Guangxi Medical University (China, Nanning). Animals were maintained at constant temperature (23 ± 2°C) with a 12 h light-dark cycle and free access to water and food.
Experimental Cardiac Arrest Rat Model
Animal Preparation
All rats fasted for 12 h but had free access to water before the operation. Experimental rats were intraperitoneally injected with sodium pentobarbital (45 µg/g) for anaesthesia, and an additional dose of 10 µg/g was supplemented at hourly intervals. Standard Lead II Electrocardiograph was used to monitor heart rhythm. A twenty-gauge catheter containing 5 IU/mL of sodium heparin saline was inserted into the right femoral vein for drug delivery, and another identical catheter was inserted into the right femoral artery for haemodynamic monitoring. Pressure transducers were connected to a four-channel physiological recorder (BL-420 E Biosystems, Chengdu Technology & Market Co. Ltd., China). After the 5 mins baseline electrocardiograph and physiologic measurements, temperature probes were placed into the rectum. During the experiment, the rectal temperature was adjusted to approximately 37°C using a heat lamp or ice pack.
Renal Warm Ischemia-Reperfusion Injury Induced by the Cardiac Arrest/Cardiopulmonary Resuscitation Model
The rat cardiac arrest (CA) model was established according to our previously reported method.Citation22 Briefly, CA was induced by alternating current (12 V) from a stimulator through a pacing electrode placed in the oesophagus, as confirmed by a decrease in mean arterial pulse pressure (<10 mmHg) and by the appearance of asystole on the electrocardiograph (ECG). Cardiopulmonary resuscitation was initiated 8 min after the induction of CA with mechanical chest compressions (180 per minute) and effective ventilation (TV 8 mL/kg, respiration rate 40/min, and positive end-expiratory pressure 0 cm H2O, oxygen concentration 100%) using a small animal ventilator with capacity control mode. After 1 min of CPR, one dose of epinephrine (0.4 µg/g) was given through the left femoral vein catheter. When ROSC was clarified by ECG activity with visible systoleCitation23 and mean arterial pressure (MAP) ≥ 50 mmHg for ≥1 min, chest compressions were stopped. If ROSC is not achieved within 3 min of the onset of cardiopulmonary resuscitation, it is defined as a failure, and the animal is excluded from the study. After achieving ROSC, rats randomly received edaravone (3 mg/kg, n=10, EDR group) or equal volume normal saline solution (n=10, NS group). The sham-operated rats only received the same experimental preparation without CA induction (n=10). The rats were individually fed in cages with dry litter and placed in a quiet room with air conditioning-adjusted temperature (room temperature 26°C).
Renal Function Analysis
The serum of the experimental rats was taken from the carotid artery at 24 h after ROSC. The values of serum creatinine (SCR), blood urea nitrogen (BUN), and cystatin-C (Cys-C) were monitored in the Department of Laboratory, the Second Affiliated Hospital of Guangxi Medical University.
Western Blot Analysis
Rats from each experimental group were anaesthetized and then sacrificed to take kidneys for Western blot detection at 24 hrs after ROSC. The expression levels of GRP 78, p-PERK, and CHOP in renal tissues were assessed by Western blot analysis. The prepared kidney tissues were weighed and homogenized in a glass homogenizer containing 1:10 (w/v) ice-cold whole cell lysis buffer (Beyotime Biotechnology, China, P0013B). The lysed protein was collected and centrifuged at 14,000 × g for 15 mins at 4°C. The BCA Protein Assay Kit (Beyotime Biotechnology, China, P0010) was used to determine total tissue protein concentration. The tissue total protein (10–20 µL) of protein lysates was separated by 10–15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and then transferred to PVDF membranes (Millipore, USA, 0.22-μm pore diameter). The membranes were blocked with PBST containing 5% bovine serum albumin for 1 h and then incubated with primary antibody overnight at 4°C. β-Actin was used for normalization. The primary antibodies were as follows: primary antibodies ERK 1/2 (ab184699) and p-ERK1/2 (ab76299) were purchased from Abcam Plc, Cambridge, UK, and MFN2(11925). β-Actin (CST, 4970S), GRP 78 (CST, 3183S), CHOP (CST, 2895S), Bax (CST, 14796S), Bcl-2 (Abcam, 182858), and GAPDH (Abcam, 181602). The membrane was washed three times with PBST and then incubated with secondary antibody (Cell Signalling Technology, USA, #5151, 1:15,000). Membranes were quantified by using a Western blot detection system with a Li-cor Odyssey Scanner imaging densitometer, and the results of the bands detected were quantified using ImageJ software (v1.33, NIH, Bethesda, MD, USA).
Statistical Analysis
All data are expressed as the mean ± standard deviations. Statistical analysis software is SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables between groups were compared using the Student’s t-test. Groups were compared using one-way ANOVA followed by the Student–Newman–Keul test for post hoc comparisons. p < 0.05 was considered statistically significant.
Results
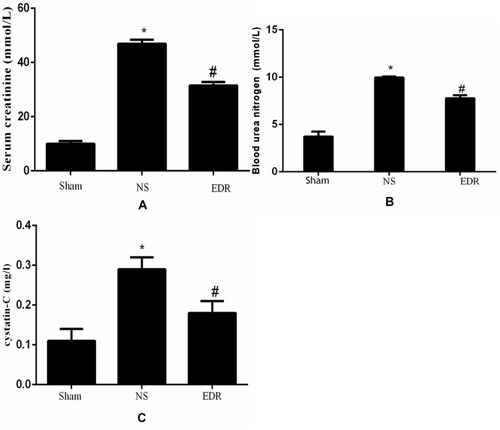
Edaravone Improves Renal Function After CA/CRP
To examine the kidney function, we compared Cys-C, SCR, BUN and Cys-C in all groups. The values of Cys-C, SCR and BUN were significantly increased in NS group compared with the Sham group (p < 0.05), suggesting an adverse outcome of renal function. Treatment of edaravone obviously decreased the level of Cys-C, SCR and BUN (p < 0.05), suggesting a protective effect on renal function ().
Figure 1 Comparison of SCR (A), BUN (B), and Cys-C (C) among the 3 groups. Data are expressed as the mean ± SD (n = 10 for each group). *P<0.05 Vs the Sham group, #P<0.05 Vs the NS group.
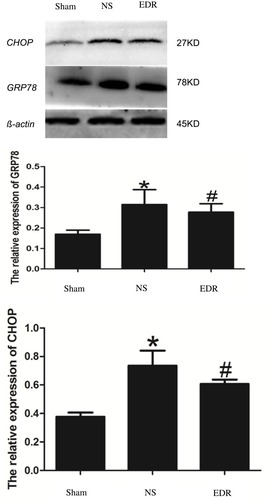
EDR Reduced Endoplasmic Reticulum Stress Induced by CA/CPR
We perform the Western blot detection to determine the effect of EDR on the endoplasmic reticulum stress (ERS) induced by CA/CPR. The result showed that the expression of glucose-regulated protein (GRP78) and C/EBP homologous protein (CHOP) presented remarkable upregulation in the NS group (p < 0.05), while treatment of EDR significantly reduced the level of GRP78 and CHOP (p < 0.05). ().
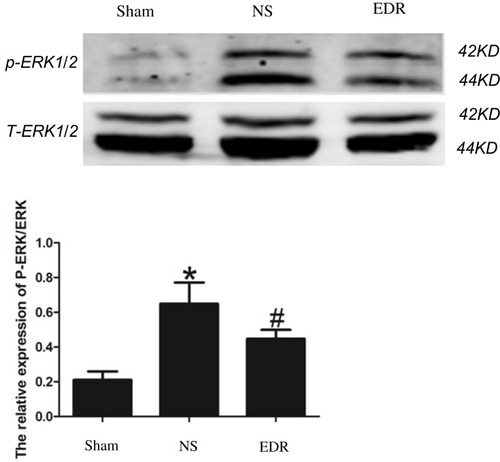
EDR Inhibits Phosphorylation of Extracellular Signal-Regulated Kinase 1/2
As shown in , compared with the sham group, p-ERK1/2 was significantly elevated in the NS group (p < 0.05), while the expression of p-ERK1/2 was reduced in EDR group (p < 0.05).
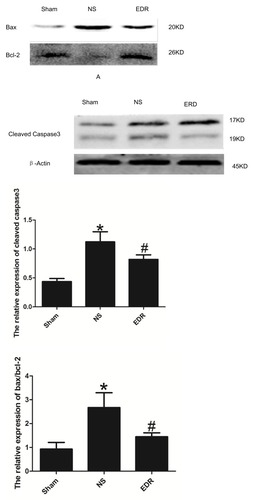
EDR Decreases Caspase-3 and the Bax/Bcl-2 Ratio
Compared with the Sham group, cleaved caspase-3 and the Bax/Bcl-2 ratio were significantly upregulated in the NS group (p < 0.05); by the contrast, the expression of cleaved caspase-3 and the Bax/Bcl-2 ratio were significantly decreased in the EDR group. (p < 0.05). ().
Discussion
In this study, we found that renal warm ischaemia/reperfusion injury (IRI) induced by cardiac arrest/cardio-pulmonary resuscitation (CA/CPR) substantially upregulated the expression of Glucose Regulated Protein 78 (GRP78) and C/EBP-homologous protein (CHOP) at 24 hrs post-ROSC. EDR treatment ameliorated renal dysfunction and protected against renal damage, including a significant reduction in SCR, BUN, and Cys-C. Compared to the NS group, GRP78, CHOP, p-ERK1/2, caspase-3 expression and Bax/Bcl-2 ratio were significantly decreased in the EDR group, suggesting protective effect of EDR against endoplasmic reticulum stress (ERS) and apoptosis.
In our previous study, rats subjected to CA/CPR presented with excessive ROS production in the brain tissue.Citation5 Overdose of ROS-induced ERS, which plays an important role in the development of several organ IRI in rats.Citation24–Citation26 while EDR can be used to reduce or block ROS-induced ERS to reduce organ IRI.Citation27 Hence, the purpose of our current study is to investigate the renal protective potential of EDR, a potent free-radical scavenger against renal warm IRI induced by CA/CPR.
The current data are consistent with previous results demonstrating that EDR pre-treatment protects against warm IRI in a variety of tissues and organs, including the heart and brain.Citation28,Citation29 In addition, a recent clinical study suggests that EDR may be a useful medication to protect kidney function in patients with acute ischaemic stroke.Citation21 Overall, our findings are consistent with recently published data demonstrating that EDR exerts beneficial effects against organ ischaemic damage, including renal IRI.Citation30 As mentioned in the previous study, the animal model of the protective effect of EDR on renal IRI is mostly due to clamping of the renal artery or renal pedicle. However, there may be high incidence of vascular injury, infection, hilar injury, venous congestion, cold renal ischaemia during animal operation, and the observation period is only at the early phase of reperfusion.Citation31–Citation33 Importantly, these models did not fully mimic the most common clinical features of AKI after ROSC. Hence, we used the methods of transoesophageal alternating current stimulation to establish 8 min of CA in a rat model followed by conventional CPR to avoid the adverse effects and create a model of renal warm IRI that is close to clinical characteristics.
As an ERS downstream event, activation of GRP78/CHOP pathway is the key cellular response of ERS-induced apoptosis.Citation9,Citation34,Citation35 Downregulation of GRP78/CHOP by intermedin significantly decreased apoptosis.Citation10 In addition, a previous study revealed that EDR ameliorated early renal dysfunction and injury evoked by ischaemia/reperfusion in mice subjected to 45 min of bilateral renal IRI.Citation33 However, it is unclear whether EDR exerts protection against ERS in renal warm IRI evoked by CA/CPR. Our current research showed that EDR can ameliorate renal warm IRI by down-regulating GRP78 and CHOP expression, which was similar with previous studies regarding with EDR protection on dilated cardiomyopathy, spatial memory,Citation28,Citation29 cerebral ischaemiaCitation36 and autoimmune myocarditis.Citation37
Studies have suggested that EDR can alleviate oxidative damage by inhibiting ERK1/2 activation.Citation38,Citation39 ERK1/2 is a member of the MAPK family, which plays an important role in cell survival and death.Citation40 Inhibition of ERK by EDR can alleviate oxidative damage. What is more, the ERK1/2 signalling pathway has also been shown to be involved in ERS-mediated apoptosis.Citation41,Citation42 Studies have demonstrated that IR dramatically increases phosphorylated ERK1/2 levels in the kidney.Citation43,Citation44 In addition, multiple studies proved that ERK activation was commonly protective in renal IRI.Citation44,Citation45 By the contrast, IRI dramatically increased phosphorylated ERK1/2 expression and promoted apoptosis have also been reported.Citation46 In our present work, we found that the expression of phosphorylated ERK1/2 was significantly elevated which accompanied with renal function decrease at 24 h after ROSC in NS group. This result was consistent with our previous research, in which we found that inhibiting the expression of phosphorylated ERK1/2 can protect the brain from IRI in rat experienced CA/CPR.Citation47
Apoptosis is widely considered to be the main mechanism that induces cell death in renal IRI.Citation48,Citation49 Bax and caspase-3 are the most important downstream effectors for the ERK pathwayCitation50,Citation51 that have also been demonstrated to involve in ERS-induced apoptosis.Citation52–Citation54 In renal cells, ischaemia activates BaxCitation55 and inhibits Bcl-2,Citation56 resulting in an increased Bax/Bcl-2 ratio.Citation57 On the other hand, caspases are well-known drivers of apoptotic cell death, cleaving cellular proteins that provide critical links in cell regulatory networks controlling dying cells.Citation58 Active caspase-3 leads to DNA fragmentation and formation of apoptotic bodies.Citation59 Caspase-3 and Bax have been demonstrated to mediate ERS-induced apoptosis.Citation52–Citation54 Our previous study demonstrated that inhibition of ischaemia-induced ERK1/2 kinase activity can reduce Bax and caspase-3 expression and improve organ function.Citation47 In the present study, we showed that EDR treatment decreased phosphorylation of ERK1/2 and apoptotic parameters including caspase-3 and the Bax/Bcl-2 ratio. These results suggested a reno-protective effect of EDR on a CA/CPR model. As mentioned previously, ERK activation is an important downstream mechanism of ERS.Citation12 We hold the opinion that EDR acts as an anti-apoptotic agent by downregulating GRP78/CHOP/ERK signal pathway.
Graphene was discovered in 2004 and its application in nanomaterials has been developing rapidly for drug delivery.Citation60 Graphene nanomaterials can enhance the efficacy in chemotherapy applications,Citation61 increase drug loading capacity,Citation62 and presents no toxicity to cells.Citation63 In addition, some improved graphene nanomaterials are able to cross the cell membrane and then accumulated more in the cell cytoplasm compared with the traditional ones. The capacity of transmembrane makes it possible to delivery drug to the targeted organ or cells more effectively.Citation64 Furthermore, a series of triggered drug delivery systems consist of graphene have been reported. The systems realize controlling drug delivery remotely and adjusting dosing regimens on demand.Citation65,Citation66 Therefore, it is worth to determine whether delivery of EDR targeting renal with graphene nanomaterials could obtain a better outcome in renal warm ischemia-reperfusion injury post CA/CPR.
In conclusion, we found that EDR ameliorates renal warm IRI by downregulating ERS and its downstream effectors in a rat AKI model evoked by CA/CPR. These data may provide evidence for future therapeutic benefits of EDR against AKI induced by CA/CPR.
Ethics Approval and Consent to Participate
The present study was approved by the Committee on the Ethics of Animal Experiments and Human Subject Research of the Guangxi Medical University.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
Zhao-yin Fu reports grants from National Natural Science Foundation of China and Scientific Research and Technological Development Project of Qinzhou City, during the conduct of the study. The authors report no other conflicts of interest in this work.
Funding
The research was supported by the National Natural Science Foundation of China (grant no.81860333) and Scientific Research and Technological Development Project of Qinzhou City (grant no.201616814).
References
- AntoniaL, PasqualeD, AntonioC, et al. Ischemia-reperfusion induces glomerular and tubular activation of proinflammatory and antiapoptotic pathways: differential modulation by rapamycin. J Am Soc Nephrol. 2004;15(10):2675. doi:10.1097/01.ASN.0000139932.00971.E415466272
- BastinAJ, OstermannM, SlackAJ, DillerGP, FinneySJ, EvansTW. Acute kidney injury after cardiac surgery according to risk/injury/failure/loss/end-stage, acute kidney injury network, and kidney disease: improving global outcomes classifications. J Crit Care. 2013;28(4):389–396. doi:10.1016/j.jcrc.2012.12.00823743540
- PericoN, CattaneoD, SayeghMH, RemuzziG. Delayed graft function in kidney transplantation. Lancet. 2004;364(9447):1814–1827. doi:10.1016/S0140-6736(04)17406-015541456
- InagiR. Endoplasmic reticulum stress in the kidney as a novel mediator of kidney injury. Nephron Exp Nephrol. 2009;112(1):e1–e9. doi:10.1159/00021057319342868
- Nguyen ThiPA, ChenMH, LiN, ZhuoXJ, XieL. PD98059 protects brain against cells death resulting from ROS/ERK activation in a cardiac arrest rat model. Oxid Med Cell Longev. 2016;2016(10):1–13. doi:10.1155/2016/3723762
- BravoR, ParraV, GaticaD, et al. Endoplasmic reticulum and the unfolded protein response: dynamics and metabolic integration. Int Rev Cell Mol Biol. 2013;301(301):215–290.23317820
- AsmaMB, Mohamed AmineZ, ThierryH, et al. Attenuation of endoplasmic reticulum stress and mitochondrial injury in kidney with ischemic postconditioning application and trimetazidine treatment. J Biomed Sci. 2012;19(1):71. doi:10.1186/1423-0127-19-7122853733
- MontieHL, KayaliF, HaezebrouckAJ, RossiNF, DegraciaDJ. Renal ischemia and reperfusion activates the eIF 2 alpha kinase PERK. Biochim Biophys Acta. 2005;1741(3):314–324. doi:10.1016/j.bbadis.2005.04.00715936177
- MiRN, KimJI, SangJH, LeeTJ, ParkKM. C/EBP homologous protein (CHOP) gene deficiency attenuates renal ischemia/reperfusion injury in mice. Biochim Biophys Acta. 2015;1852(9):1895–1901. doi:10.1016/j.bbadis.2015.06.00426071644
- WangY, TianJ, QiaoX, et al. Intermedin protects against renal ischemia-reperfusion injury by inhibiting endoplasmic reticulum stress. BMC Nephrol. 2015;16(1):169. doi:10.1186/s12882-015-0157-726498843
- MasakiT. Activation of the extracellular-signal regulated protein kinase pathway in human glomerulopathies. J Am Soc Nephrol. 2004;15(7):1835–1843. doi:10.1097/01.ASN.0000130623.66271.6715213271
- HungCC, IchimuraT, StevensJL, BonventreJV. Protection of renal epithelial cells against oxidative injury by endoplasmic reticulum stress preconditioning is mediated by ERK1/2 activation. J Biol Chem. 2003;278(31):29317–29326. doi:10.1074/jbc.M30236820012738790
- AlderliestenM, DeGM, OldenampsenJ, et al. Extracellular signal-regulated kinase activation during renal ischemia/reperfusion mediates focal adhesion dissolution and renal injury. Am J Pathol. 2007;171(2):452–462. doi:10.2353/ajpath.2007.06080517620366
- ChoiDE, JeongJY, ChoiH, et al. ERK phosphorylation plays an important role in the protection afforded by hypothermia against renal ischemia-reperfusion injury. Surgery. 2017;161(2):444–452. doi:10.1016/j.surg.2016.07.02827590616
- LiuWH, LiuHB, GaoDK, et al. ABCG2 protects kidney side population cells from hypoxia/reoxygenation injury through activation of the MEK/ERK pathway. Cell Transplant. 2013;22(10):1859–1868. doi:10.3727/096368912X65720623032069
- DarlingNJ, BalmannoK, CookSJ. ERK1/2 signalling protects against apoptosis following endoplasmic reticulum stress but cannot provide long-term protection against BAX/BAK-independent cell death. PLoS One. 2017;12(9):e0184907. doi:10.1371/journal.pone.018490728931068
- KikuchiK, TakeshigeN, MiuraN, et al. Beyond free radical scavenging: beneficial effects of edaravone (Radicut) in various diseases. Exp Ther Med. 2012;3(1):3. doi:10.3892/etm.2011.35222969835
- QiX, OkumaY, HosoiT, NomuraY. Edaravone protects against hypoxinlschemia-lnduced endoplasmic reticulum dysfunction. J Pharmacol Exp Ther. 2004;311(1):388–393. doi:10.1124/jpet.104.06908815178695
- TaharaM, NakayamaM, JinMB, et al. A radical scavenger, edaravone, protects canine kidneys from ischemia-reperfusion injury after 72 hours of cold preservation and autotransplantation. Transplantation. 2005;80(2):213–221. doi:10.1097/01.TP.0000165092.07375.C916041266
- MatsuyamaM, HayamaT, FunaoK, et al. Treatment with edaravone improves the survival rate in renal warm ischemia-reperfusion injury using rat model. Transplant Proc. 2006;38(7):2199–2200. doi:10.1016/j.transproceed.2006.06.07716980041
- KamouchiM, SakaiH, KiyoharaY, MinematsuK, HayashiK, KitazonoT. Acute kidney injury and edaravone in acute ischemic stroke: the Fukuoka Stroke Registry. J Stroke Cerebrovasc Dis. 2013;22(8):e470–e476. doi:10.1016/j.jstrokecerebrovasdis.2013.05.01823800495
- ChenM-H, LiuT-W, XieL, et al. A simpler cardiac arrest model in rats. Am J Emerg Med. 2007;25(6):623–630. doi:10.1016/j.ajem.2006.11.03317606086
- DengG, YonchekJC, QuillinanN, et al. A novel mouse model of pediatric cardiac arrest and cardiopulmonary resuscitation reveals age-dependent neuronal sensitivities to ischemic injury. J Neurosci Methods. 2014;222:34–41. doi:10.1016/j.jneumeth.2013.10.01524192226
- JassemW, HeatonND. The role of mitochondria in ischemia|[sol]|reperfusion injury in organ transplantation. Kidney Int. 2004;66(2):514–517. doi:10.1111/j.1523-1755.2004.761_9.x15253700
- TothA, NicksonP, MandlA, BannisterML, TothK, ErhardtP. Endoplasmic reticulum stress as a novel therapeutic target in heart diseases. Cardiovasc Haematol Disord. 2007;7(3):205–218.
- HayashiT, SaitoA, OkunoS, FerranddrakeM, DoddRL, ChanPH. Damage to the endoplasmic reticulum and activation of apoptotic machinery by oxidative stress in ischemic neurons. J Cereb Blood Flow Metab. 2005;25(1):41–53. doi:10.1038/sj.jcbfm.960000515678111
- SrinivasanK, SharmaSS. Edaravone offers neuroprotection in a diabetic stroke model via inhibition of endoplasmic reticulum stress. Basic Clin Pharmacol Toxicol. 2012;110(2):133–140. doi:10.1111/j.1742-7843.2011.00763.x21752197
- ArumugamS, ThandavarayanRA, VeeraveeduPT, et al. Beneficial effects of edaravone, a novel antioxidant, in rats with dilated cardiomyopathy. J Cell Mol Med. 2012;16(9):2176–2185. doi:10.1111/jcmm.2012.16.issue-922268705
- TianA, MaH, ZhangR, CuiY, WanC. Edaravone improves spatial memory and modulates endoplasmic reticulum stress-mediated apoptosis after abdominal surgery in mice. Exp Ther Med. 2017;14(1):355–360. doi:10.3892/etm.2017.448928672938
- KaraaM, KuyucuY, TuliA, TapO. The effect of edaravone on ischemia–reperfusion injury in rat ovary. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):197–202. doi:10.1016/j.ejogrb.2012.02.02622445304
- ChuaHR, GlassfordN, BellomoR. Acute kidney injury after cardiac arrest. Resuscitation. 2012;83(6):721–727. doi:10.1016/j.resuscitation.2011.11.03022155699
- DiPR, ImpellizzeriD, MondelloP, et al. Palmitoylethanolamide reduces early renal dysfunction and injury caused by experimental ischemia and reperfusion in mice. Shock. 2012;38(4):356–366. doi:10.1097/SHK.0b013e318267bbb922772472
- ChiazzaF, ChegaevK, RogazzoM, et al. A nitric oxide-donor furoxan moiety improves the efficacy of edaravone against early renal dysfunction and injury evoked by ischemia/reperfusion. Oxid Med Cell Longev. 2015;2015:804659. doi:10.1155/2015/80465925834700
- WangCL, LiuC, NiuLL, WangLR, HouLH, CaoXH. Surfactin-induced apoptosis through ROS-ERS-Ca2+-ERK pathways in HepG2 cells. Cell Biochem Biophys. 2013;67(3):1433–1439. doi:10.1007/s12013-013-9676-723733672
- ZhangK, KaufmanRJ. From endoplasmic-reticulum stress to the inflammatory response. Nature. 2008;454(7203):455–462. doi:10.1038/nature0720318650916
- QiX, OkumaY, HosoiT, NomuraY. Edaravone protects against hypoxia/ischemia-induced endoplasmic reticulum dysfunction. J Pharmacol Exp Ther. 2004;311(1):388–393. doi:10.1124/jpet.104.06908815178695
- ShimazakiH, WatanabeK, VeeraveeduPT, et al. The antioxidant edaravone attenuates ER-stress-mediated cardiac apoptosis and dysfunction in rats with autoimmune myocarditis. Free Radic Res. 2010;44(9):1082–1090. doi:10.3109/10715762.2010.49990420815771
- KawasakiT, KitaoT, NakagawaK, et al. Nitric oxide‐induced apoptosis in cultured rat astrocytes: protection by edaravone, a radical scavenger. Glia. 2010;55(13):1325–1333. doi:10.1002/glia.20541
- ZhaoZY, LuanP, HuangSX, et al. Edaravone protects HT22 neurons from H2O2-induced apoptosis by inhibiting the MAPK signaling pathway. CNS Neurosci Ther. 2013;19(3):163–169. doi:10.1111/cns.1204423253171
- KimEK, ChoiEJ. Pathological roles of MAPK signaling pathways in human diseases. Biochim Biophys Acta. 2010;1802(4):396–405. doi:10.1016/j.bbadis.2009.12.00920079433
- HuP, HanZ, CouvillonAD, ExtonJH. Critical role of endogenous Akt/IAPs and MEK1/ERK pathways in counteracting endoplasmic reticulum stress-induced cell death. J Biol Chem. 2004;279(47):49420–49429. doi:10.1074/jbc.M40770020015339911
- Cheng-ChiehH, TakaharuI, StevensJL, BonventreJV. Protection of renal epithelial cells against oxidative injury by endoplasmic reticulum stress preconditioning is mediated by ERK1/2 activation. J Biol Chem. 2003;278(31):29317–29326. doi:10.1074/jbc.M30236820012738790
- ParkKM, KramersC, Vayssier-TaussatM, ChenA, BonventreJV. Prevention of kidney ischemia/reperfusion-induced functional injury, MAPK and MAPK kinase activation, and inflammation by remote transient ureteral obstruction. J Biol Chem. 2002;277(3):2040–2049. doi:10.1074/jbc.M10752520011696540
- ZouYR, ZhangJ, WangJ, PengL, LiGS, WangL. Erythropoietin receptor activation protects the kidney from ischemia/reperfusion-induced apoptosis by activating ERK/p53 signal pathway. Transplant Proc. 2016;48(1):217–221. doi:10.1016/j.transproceed.2016.01.00926915871
- KyriazisI, KagadisGC, KallidonisP, et al. PDE5 inhibition against acute renal ischemia reperfusion injury in rats: does vardenafil offer protection? World J Urol. 2013;31(3):597–602. doi:10.1007/s00345-012-0980-423143734
- MrVDB, KapellerR, PrattJC, ChangJH, BurakoffSJ. The extracellular signal-regulated kinase pathway is required for activation-induced cell death of T cells. J Biol Chem. 1999;274(16):11178–11185. doi:10.1074/jbc.274.16.1117810196203
- Nguyen ThiPA, ChenMH, LiN, ZhuoXJ, XieL. PD98059 protects brain against cells death resulting from ROS/ERK activation in a cardiac arrest rat model. Oxid Med Cell Longev. 2016;2016:3723762. doi:10.1155/2016/372376227069530
- KalogerisT, BainesCP, KrenzM, KorthuisRJ. Chapter Six – cell Biology of Ischemia/Reperfusion Injury. Int Rev Cell Mol Biol. 2012;298:229–317.22878108
- MoriS, SawadaT, OkadaT, KubotaK. Erythropoietin and its derivative protect the intestine from severe ischemia/reperfusion injury in the rat. Surgery. 2008;143(4):556–565. doi:10.1016/j.surg.2007.12.01318374054
- LuZ, XuS. ERK1/2 MAP kinases in cell survival and apoptosis. IUBMB Life. 2010;58(11):621–631. doi:10.1080/15216540600957438
- WhitlockBB, GardaiS, FadokV, BrattonD, HensonPM. Differential roles for αMβ2 integrin clustering or activation in the control of apoptosis via regulation of Akt and ERK survival mechanisms. J Cell Biol. 2000;151(6):1305–1320. doi:10.1083/jcb.151.6.130511121444
- NakagawaT, ZhuH, MorishimaN, et al. Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature. 2000;403(6765):98–103. doi:10.1038/4751310638761
- JimboA, FujitaE, KourokuY, et al. ER stress induces caspase-8 activation, stimulating cytochrome c release and caspase-9 activation. Exp Cell Res. 2003;283(2):156–166. doi:10.1016/S0014-4827(02)00033-212581736
- ZongWX, ChiL, GeorgiaH, et al. Bax and Bak can localize to the endoplasmic reticulum to initiate apoptosis. J Cell Biol. 2003;162(1):59–69. doi:10.1083/jcb.20030208412847083
- HavasiA, LiZ, WangZ, et al. Hsp27 inhibits bax activation and apoptosis via a phosphatidylinositol 3-Kinase-dependent mechanism. J Biol Chem. 2008;283(18):12305–12313. doi:10.1074/jbc.M80129120018299320
- ChienCT, ChangTC, TsaiCY, ShyueSK, LaiMK. Adenovirus-mediated bcl-2 gene transfer inhibits renal ischemia/reperfusion induced tubular oxidative stress and apoptosis. Am J Transplant. 2015;5(6):1194–1203.
- Dae EunC, YoungJJ, Beom JinL, et al. Pretreatment of sildenafil attenuates ischemia-reperfusion renal injury in rats. Am J Physiol Renal Physiol. 2009;297(2):362–370. doi:10.1152/ajprenal.90609.2008
- WigleJC, EstlackLE, SchusterKJ. Retinal illumination to protect against laser damage. Spienewsroom. 2013.
- CaoG, PeiW, LanJ, et al. Caspase-activated DNase/DNA fragmentation factor 40 mediates apoptotic DNA fragmentation in transient cerebral ischemia and in neuronal cultures. J Neurosci. 2001;21(13):4678. doi:10.1523/JNEUROSCI.21-13-04678.200111425895
- GoenkaS, SantV, SantS. Graphene-based nanomaterials for drug delivery and tissue engineering. J Controlled Release. 2014;173(1):75–88. doi:10.1016/j.jconrel.2013.10.017
- ZhangL, XiaJ, ZhaoQ, LiuL, ZhangZ. Functional graphene oxide as a nanocarrier for controlled loading and targeted delivery of mixed anticancer drugs. Small. 2010;6(4):537–544. doi:10.1002/smll.v6:420033930
- YangX, ZhangX, MaY, YiH, WangY, ChenY. Superparamagnetic graphene oxide–fe3O4nanoparticles hybrid for controlled targeted drug carriers. J Mater Chem. 2009;19(18):2710–2714. doi:10.1039/b821416f
- PanY, BaoH, SahooNG, WuT, LiL. Water‐soluble Poly(N‐isopropylacrylamide)–graphene sheets synthesized via click chemistry for drug delivery. Adv Funct Mater. 2011;21(14):2754–2763. doi:10.1002/adfm.201100078
- OliveiraE, MacedoC, CollaresC, Sakamoto-HojoE, DonadiE, PassosG. Quantum-dot-conjugated graphene as a probe for simultaneous cancer-targeted fluorescent imaging, tracking, and monitoring drug delivery. Bioconjug Chem. 2013;24(3):387–397. doi:10.1021/bc300480923425155
- DinggengH, XiaoxiaoH, KeminW, ZhenZ, XueY, XuecaiL. Remote-controlled drug release from graphene oxide-capped mesoporous silica to cancer cells by photoinduced pH-jump activation. Langmuir. 2014;30(24):7182–7189. doi:10.1021/la501075c24924411
- YinPT, ShahS, ChhowallaM, LeeKB. Design, synthesis, and characterization of graphene-nanoparticle hybrid materials for bioapplications. Chem Rev. 2015;115(7):2483–2531. doi:10.1021/cr500537t25692385