Abstract
Idiosyncratic reactions to a large number of drugs have been reported to cause choroidal detachment and secondary angle-closure glaucoma (ACG). We report a case of bilateral acute ACG and peculiar choroidal effusion following administration of oral acetazolamide immediately after cataract surgery. Few cases of acute secondary ACG with choroidal effusion and anterior shift of the lens-iris diaphragm have been associated with acetazolamide compared with other sulfonamides. As far as we are aware, posterior involvement with retinal folds and papillary edema due to acetazolamide has not been described before.
Introduction
Acetazolamide, a sulfonamide-derived medication, is frequently used in patients after cataract surgery.Citation1
It is a member of the class of antihypertensive drugs and is specifically indicated in the treatment of glaucoma, epilepsy, benign intracranial hypertension (pseudotumor cerebri), altitude sickness, cystinuria, and ectasia.Citation2–Citation4 Acetazolamide acts as an inhibitor of the enzyme carbonic anhydrase and is therefore applied in ophthalmology to control primary or postsurgical secondary ocular hypertension.Citation5
This medication and other sulfa drugs have been documented to cause, very rarely, idiosyncratic reactions characterized by transient myopia, ciliary body edema, uveal effusions, and anterior rotation of the lens-iris diaphragm, which causes secondary angle-closure glaucoma (ACG).Citation6 Unfortunately, the angle closure occurs without pupillary block, so that topical miotics and peripheral iridectomy are not helpful.Citation7 In contrast, stopping the offending agent and controlling the intraocular pressure (IOP) with the administration of drugs allows rapid resolution of signs and symptoms. This reaction has been frequently documented after topiramate administration, an antiepileptic agent also used to treat migraine,Citation8,Citation9 while only rarely after acetazolamide.Citation10–Citation12
Here, we report a case of ciliary body edema after administration of acetazolamide causing bilateral ACG, as already described in the literature.Citation11,Citation12 However, in our case we found a massive choroidal effusion with posterior retinal folds and papillary edema. The existent literature reporting ciliary body edema after administration of acetazolamide do not describe these features at the posterior pole.Citation6–Citation13
Case report
A 71-year-old white male had routine cataract surgery and intraocular lens implantation under local anesthetic in his right eye (RE) in the late afternoon. He was prescribed a single oral dose of acetazolamide (250 mg) before sleeping to prevent rise of IOP. The patient took the acetazolamide pill at 11 pm (4 hours after cataract surgery). About 3 hours later, he woke up because of severe pain and found he had reduced vision in both eyes, so was referred to our first-aid hospital.
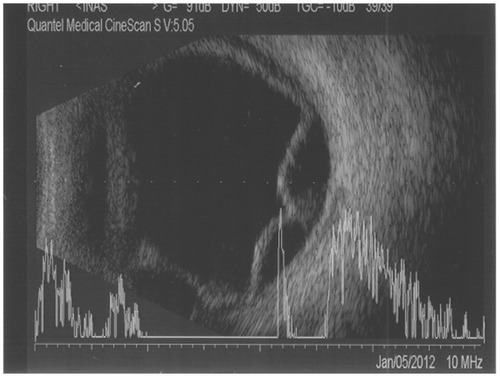
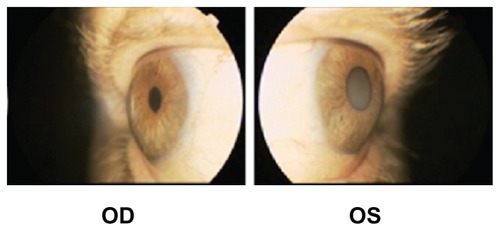
Upon examination, the patient’s best-corrected visual acuity was 3/50 in the RE and 2/50 in left eye (LE), with corrections of −4.50 D in the RE and −1.25 D in the LE. Both eyes showed congestion and edema of the inferior bulbar conjunctiva, heavy cloudy cornea, and a very shallow anterior chamber (). The intraocular lens was shifted forward. IOP was 52 mmHg in the RE and 60 mmHg in the LE. Gonioscopy revealed 360-degree appositional angle closure with a convex iris configuration in both eyes. Fundus examination was impossible due to opaque media. A diagnosis of ACG was made and the patient was admitted to the hospital. He was immediately administered mannitol 2 mg/kg intravenously and acetazolamide orally, together with topical steroids and β-blockers.
Figure 1 Anterior segment of the left and right eye (which underwent cataract surgery) showing the absence of the anterior chamber, observed during slit lamp examination, and choroidal congestion.
Later in the morning, his IOP was 32 mmHg in the RE and 36 mm Hg in the LE. Nd:YAG laser iridotomy was performed in the LE, but had a poor effect on anterior chamber depth and ocular hypertension.
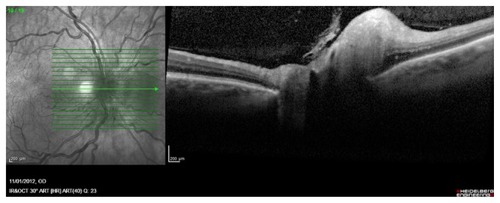
B-scan ultrasonography () showed bilateral choroidal effusion with forward displacement of the anterior segment. Fundus examination was characterized by bilateral peripheral choroidal detachment () and papillary swelling. Posterior optical coherence tomography scans confirmed papillary edema () together with retinal folds and nerve fiber layer thickening.
Figure 3 Choroidal detachment observed during fundus examination using indirect Schepens ophthalmoscopy.
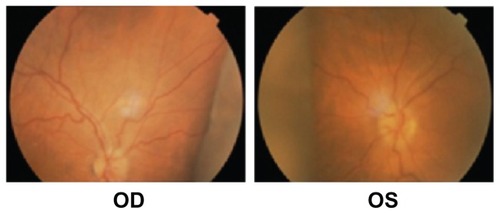
Figure 4 Papillary edema and nerve fiber layer thickening observed during optical coherence tomography examination (right eye).
Acetazolamide was suspected as the cause of the bilateral angle closure, thus was discontinued. The clinical manifestations gradually improved and, 3 days later, the patient’s IOP was 14 mmHg in the RE and 16 mmHg in the LE, his best-corrected visual acuity was 10/10 in the RE and 7/10 in the LE (because of pre-existing lens opacities), and the myopic shift had receded.
A month later, the patient underwent cataract surgery of the LE without the use of any sulfonamide medication and, as evidenced by optical coherence tomography scans, had no complications.
Discussion
Few cases of acute secondary ACG with choroidal effusion and anterior shift of the lens-iris diaphragm have been associated with acetazolamide compared with other sulfonamidesCitation6,Citation10–Citation12 and there have been only a few reports of posterior retinal-fold involvement due to topiramate and hydrochlorothiazide.Citation13,Citation14 As far as the authors are aware, papillary edema has never been reported associated with sulfa drugs and posterior involvement with retinal folds and papillary edema due to acetazolamide has not been described.
The retinal folds in our patient were caused by the action of the retinal pigment epithelium inhibiting further progression of fluid from the choroidal space into the retina and inextensible scleral coat. His papillary edema was caused by the absence of any barrier in the prelaminar region that could inhibit the diffusion of fluid from the choroid into the papilla and peripapillary region. This fluid diffusion was also responsible for the nerve fiber layer thickening.
Acetazolamide can cause a paradoxical adverse reaction, provoking cilio-choroidal effusion and massive involvement of the anterior and posterior segment.Citation6–Citation14
Although topical formulations of carbonic anhydrase enzyme inhibitors, such as dorzolamide, have been developed,Citation15 we chose to administer oral acetazolamide because of its well-known ability to reduce acute elevated IOP. As acute elevated IOP is sight threatening, this justified the administration of the acetazolamide, with its associated risk of rare ocular and systemic side effects. Indeed, topical dorzolamide acts only on the carbonic anhydrase enzymes present in ciliary processes of the eye, reducing aqueous flow by 17% and IOP by up to 23% as monotherapy.Citation16–Citation19 In contrast, acetazolamide alone reduces these parameters by 30%Citation16–Citation19 thanks to its diuretic properties and indirect osmotic effect that leads to vitreous dehydration together with hyperosmotic agents. Furthermore, it has been shown to act on the outward permeability of the blood–retina barrier.Citation20
In prescribing acetazolamide, all specialists and general practitioners should be aware of this side effect of the drug and refer patients to ophthalmologists. At the same time, ophthalmologists should be able, by obtaining an accurate case history, to make a correct differential diagnosis between primary acute ACG and this rare secondary pharmacological adverse reaction.
Disclosure
The authors declare no conflicts of interest in this work.
References
- Fogagnolo P Centofanti M Figus M Short-term changes in intraocular pressure after phacoemulsification in glaucoma patients Ophthalmologica 2012 228 3 154 158 22572718
- Kassamali R Sica DA Acetazolamide: a forgotten diuretic agent Cardiol Rev 2011 19 6 276 278 21983315
- Leaf DE Goldfarb DS Mechanisms of action of acetazolamide in the prophylaxis and treatment of acute mountain sickness J Appl Physiol 2007 102 4 1313 1322 17023566
- Celebisoy N Gökçay F Sirin H Akyürekli O Treatment of idiopathic intracranial hypertension: topiramate vs acetazolamide, an open-label study Acta Neurol Scand 2007 116 5 322 327 17922725
- Carta F Scozzafava A Supuran CT Sulfonamides: a patent review (2008 – 2012) Expert Opin Ther Pat 2012 22 7 747 758 22697257
- Lee GC Tam CP Danesh-Meyer HV Myers JS Katz LJ Bilateral angle closure glaucoma induced by sulphonamide-derived medications Clin Experiment Ophthalmol 2007 35 1 55 58 17300572
- Lachkar Y Bouassida W Drug-induced acute angle closure glaucoma Curr Opin Ophthalmol 2007 18 2 129 133 17301614
- Desai CM Ramchandani SJ Bhopale SG Ramchandani SS Acute myopia and angle closure caused by topiramate, a drug used for prophylaxis of migraine Indian J Ophthalmol 2006 54 3 195 197 16921218
- Fraunfelder FW Fraunfelder FT Keates EU Topiramate-associated acute, bilateral, secondary angle-closure glaucoma Ophthalmology 2004 111 1 109 111 14711721
- Mancino R Varesi C Cerulli A Aiello F Nucci C Acute bilateral angle-closure glaucoma and choroidal effusion associated with acetazolamide administration after cataract surgery J Cataract Refract Surg 2011 37 2 415 417 21241929
- Parthasarathi S Myint K Singh G Mon S Sadasivam P Dhillon B Bilateral acetazolamide-induced choroidal effusion following cataract surgery Eye (Lond) 2007 21 6 870 872 17293785
- Senthil S Garudadri C Rao HB Maheshwari R Bilateral simultaneous acute angle closure caused by sulphonamide derivatives: a case series Indian J Ophthalmol 2010 58 3 248 252 20413935
- Guier CP Elevated intraocular pressure and myopic shift linked to topiramate use Optom Vis Sci 2007 84 12 1070 1073 18091300
- Roh YR Woo SJ Park KH Acute-onset bilateral myopia and ciliochoroidal effusion induced by hydrochlorothiazide Korean J Ophthalmol 2011 25 3 214 217 21655050
- Mincione F Scozzafava A Supuran CT The development of topically acting carbonic anhydrase inhibitors as antiglaucoma agents Curr Pharm Des 2008 14 7 649 654 18336310
- Sugrue MF The pharmacology of antiglaucoma drugs Pharmacol Ther 1989 43 1 91 138 2675131
- Supuran CT Carbonic anhydrases: novel therapeutic applications for inhibitors and activators Nat Rev Drug Discov 2008 7 2 168 181 18167490
- Sugrue MF Pharmacological and ocular hypotensive properties of topical carbonic anhydrase inhibitors Prog Ret Eye Res 2000 19 1 87 112
- Maus TL Larsson LI McLaren JW Brubaker RF Comparison of dorzolamide and acetazolamide as suppressors of aqueous humor flow in humans Arch Ophthalmol 1997 115 1 45 49 9006424
- Takahashi J Mori F Hikichi T Yoshida A Effect of acetazolamide on outward permeability of blood-retina barrier using differential vitreous flyorophotometry Curr Eye Res 2001 23 3 166 170 11803477