Abstract
Purpose
Ciprofol is a recently developed short-acting gamma-aminobutyric acid receptor agonist with a higher potency than that of propofol. As a new sedative drug, there are few clinical studies on ciprofol. We sought to examine the safety and efficacy of ciprofol use for general anesthesia in neurosurgical individuals undergoing neurosurgical surgery with intraoperative neurophysiological monitoring (IONM).
Patients and Methods
This single-center, non-inferiority, single-blind, randomized controlled trial was conducted from September 13, 2022 to September 22, 2023. 120 patients undergoing elective microvascular decompression surgery (MVD) with IONM were randomly assigned to receive either ciprofol or propofol. The primary outcome of this study was the amplitude of intraoperative compound muscle action potential decline, and the secondary outcome included the indexes related to neurophysiological monitoring and anesthesia outcomes.
Results
The mean values of the primary outcome in the ciprofol group and the propofol group were 64.7±44.1 and 53.4±35.4, respectively. Furthermore, the 95% confidence interval of the difference was −25.78 to 3.12, with the upper limit of the difference being lower than the non-inferiority boundary of 6.6. Ciprofol could achieve non-inferior effectiveness in comparison with propofol in IONM of MVD. The result during anesthesia induction showed that the magnitude of the blood pressure drop and the incidence of injection pain in the ciprofol group were significantly lower than those in the propofol group (P<0.05). The sedative drug and norepinephrine consumption in the ciprofol group was significantly lower than that in the propofol group (P<0.05).
Conclusion
Ciprofol is not inferior to propofol in the effectiveness and safety of IONM and the surgical outcome. Concurrently, ciprofol is more conducive to reducing injection pain and improving hemodynamic stability, which may be more suitable for IONM-related surgery, and has a broad application prospect.
Introduction
Intraoperative neurophysiological monitoring (IONM) has become a routine monitoring method in functional neurosurgery. Microvascular decompression (MVD) of the facial nerve under neurophysiological monitoring is the first choice for possible radical treatment of hemifacial spasm. Clinical studies have confirmed that the application of IONM in MVD of the facial nerve was beneficial in improving surgical efficacy and reducing the probability of facial and auditory nerve injury.Citation1,Citation2
Intravenous anesthesia is often used in surgery requiring IONM. Propofol is one of the most commonly used intravenous anesthetic sedative drugs in clinical practice, but has a great impact on respiration and circulation. Studies have shown that propofol can reduce blood pressure by 15–40% in patients, especially in the elderly.Citation3–5 Due to the limited anatomical structure of the MVD surgical approach, it takes a long time to separate the nerve and blood vessels. At the same time, most patients are middle-aged and elderly and are prone to hypotension. Perioperative blood pressure fluctuates frequently, and repeated use of vasoactive drugs is not conducive to the recovery of patients.Citation6 Meanwhile, the inhibitory effect on respiration and pain of the injection site caused by propofol causes great trouble to anesthesiologists.Citation7–9 There is a need to acquire an alternative drug for clinical anesthesiologists to choose from so that safety and comfort can be advanced without sacrificing efficacy.
Ciprofol (HSK3486, produced by the Haisco Pharmaceutical Group Co. Ltd, Liao Ning, China), is a short-acting gamma-aminobutyric acid (GABA) receptor agonist developed in recent years, which has anesthetic and sedative effects. The special cyclopropyl and chiral structures enhance the stereoscopic effect of ciprofol, which has higher efficacy than that of propofol.Citation10,Citation11 In vitro studies have shown that ciprofol can bind to GABAA receptors 4–5 times more than can propofol, and has relatively lower lipophilicity and a more suitable spatial volume as compared with propofol.Citation12–14 Promise has been shown for ciprofol in intravenous general anesthesia and patient sedation. Studies have shown that ciprofol 0.4–0.6 mg/kg and propofol 1.5–2.5 mg/kg induce similar anesthetic effects and have similar recovery time.Citation15 The plasma concentrations of ciprofol shows a three-phase elimination characteristic, and the corresponding half-lives are 2.0 min (t1/2, α), 34.9 min (t1/2, β) and 6.2 h (t1/2, γ), respectively. Ciprofol is mainly metabolized in the liver through oxidation, glucuronic acid binding and sulfuric acid binding, which has no dose-dependent trend. Phase I cytochrome P450(CYP)2B6 and Phase II glucuronate transferase (UGT) are the main metabolic enzymes of ciprofol, with contribution rates of 24.5% and 54.0%, respectively.Citation16 Plenty of preclinical and clinical studies have shown that ciprofol has a dose-related sedative and hypnotic effect, as well as a rapid onset and metabolism, and the success rate of induction and sedation anesthesia is comparable to that of propofol.Citation13,Citation17 The adverse side effects observed after treatment with ciprofol and propofol were similar, mainly affecting the respiratory and cardiovascular systems. Recent evidence has shown that ciprofol, which has a lower aqueous free drug concentration, reveals a lower incidence of injection pain and adverse events than does propofol.Citation18–20 However, as a new sedative drug, ciprofol has insufficient experience in the application of long-term surgery, and there remains a lack of clinical evidence regarding whether it affects IONM. Therefore, we designed this prospective study to explore the safety and efficacy of ciprofol for general anaesthesia, with propofol as the control, in participants undergoing MVD for the facial nerve with IONM.
Materials and Methods
Study Design and Participants
This single-center, non-inferiority, single-blind, randomized controlled trial was conducted from September 13, 2022 to September 22, 2023 in the South District of the First Affiliated Hospital of University of Science and Technology of China (USTCH) in compliance with the Declaration of Helsinki. The protocol of this study was approved by the Ethical Committees of USTCH, Hefei, China, Registration number 2022-KY-196 (Chairman: Prof. Zuojun Shen). Informed consent was obtained from all participants prior to enrolment. The trial was registered with the Trial Registry center before being conducted (ChiCTR2200063638).
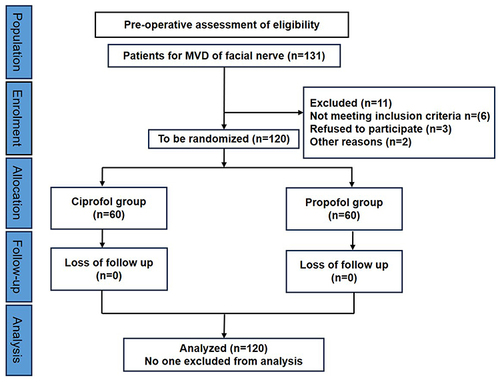
A total of 120 patients were enrolled in this study and randomly assigned to the ciprofol group and the propofol group at a ratio of 1:1, with 60 patients in each group. The trial adopts a single-blind design. Although ciprofol and propofol were identical in terms of the dosage form and colour, blinding the clinical anesthesiologists was difficult during this procedure. Patients and data analysts were unaware of the group assignments.
Inclusion criteria included: In the 18–70 age range; American Society of Anesthesiologists (ASA) classes II to III; Initial surgery for unilateral hemifacial spasm (HFS); IONM was used to monitor abnormal muscle response (AMR) and compound muscle action potential (CMAP). Exclusion criteria included: Secondary hemifacial spasm; With neuromuscular dysfunction; Allergic to anesthetics such as ciprofol and propofol; Abnormal liver and kidney function; Long-term use of sedatives and hypnotics; Body mass index above 30.
Anesthesia Procedures
After the patient arrived at the operating room, the venous access was opened and the vital signs of the patient were monitored. Patients qualified by the Allen test underwent a radial artery puncture and an indwelling catheter. A bispectral index (BIS) monitor was applied before induction. Furthermore, the train of four (TOF) mode of the muscle relaxation monitor was used to monitor intraoperative muscle relaxation. All participants received 200–300 mL of Ringer’s solution before the induction of anesthesia with either ciprofol or propofol. The injection dosage of ciprofol (0.4 mg/kg) and propofol (2.0 mg/kg) was administered to completion of tracheal intubation while the BIS value was lower than 60, followed by intravenous sufentanil 0.4 ug/kg and rocuronium 0.9 mg/kg. Tracheal intubation was performed until the TOF ratio equalled 0. Ventilation parameters were adjusted to maintain PETCO2 35~45 mmHg (1 mmHg = 0.133 kPa). Anesthesia was maintained via continuous intravenous infusion of remifentanil 0.1–0.3 ug/kg/min with either ciprofol or propofol. Patients in the ciprofol group were maintained with ciprofol at an initial rate of 0.8 mg kg-1 h-1, and the infusion rate ranged from 0.3–2.4 mg kg-1 h-1. The propofol group was given an initial rate of 5.0 mg kg-1 h-1, and the infusion rate ranged from 3–12 mg kg-1 h-1. A muscle relaxant was not used after induction, and the muscle relaxant effect was monitored using a muscle relaxant monitor in real time.
The BIS value was maintained at 40–60 by adjusting the infusion rate of propofol or ciprofol during the operation. During the operation, when the fluctuation of blood pressure exceeded 20% of baseline value, the rate of sedatives and remifentanil was adjusted first under the premise of stable anesthesia. If the hemodynamic changes continued to worsen or did not improve after 5min, norepinephrine 8ug was administered intravenously. Then the intravenous pump was continued, and the dosage of norepinephrine was adjusted according to the blood pressure monitoring. Norepinephrine consumption was recorded eventually.
Flurbiprofen axetil 50 mg and palonosetron 0.25 mg were intravenously injected 30 min before the end of surgery. After the wound was sutured, the infusion of ciprofol and propofol was stopped. Patients were then transferred to the post-anesthesia care unit (PACU) for anesthesia resuscitation. The tracheal tube was extubated while the indications for extubation were met. After the Aldrete score ≥9, patients were transferred to the general ward.
Intraoperative Neurophysiological Monitoring
After tracheal intubation, the patient was adjusted to the lateral position, and neurophysiological monitoring electrodes were implanted. When the room temperature was controlled at 25°C and the skin temperature was lower than 30°C, AMR and CMAP stimulation electrodes were placed according to the international electroencephalogram system standard (10–20). A pair of subcutaneous needle electrodes were placed at the orbicularis oculi muscle and the mentalis muscle of the affected side, respectively. The stimulating electrode was placed at the midpoint of the connection between the canthus and the external auditory canal, and the ground electrode was placed on the shoulder on the surgical side at the same time. A high-frequency multiple electrical stimulation mode was used, and the stimulation parameters were as follows: the wave width was 0.2 ms, the stimulation intensity was 1–30 mA, and the stimulation frequency was 1 Hz. When the TOF ratio of the muscle relaxation monitor recovered at more than 90%, AMR and CMAP waveform monitoring were performed by electrophysiological monitoring doctors on Neuroelectrophysiological diagnostic system (Nicoli Scientific Instrument Co. LTD, Guangzhou, China).
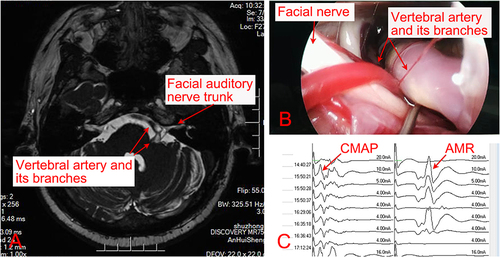
The stable AMR waveform was taken as the baseline before durotomy, and the AMR waveform and the stimulation threshold were continuously monitored. Meanwhile, the CMAP waveform was observed before durotomy, and stimulation was gradually increased until the maximum amplitude of CMAP was elicited as the baseline. Then the stimulation value was recorded. At the later time points, the same amount of stimulation was used for nerve electrical stimulation, and the CMAP amplitude was recorded. ().
Efficacy Outcomes
Measures were recorded during the procedure at the following time points: before anesthesia (T0), before tracheal intubation (T1), immediately after tracheal intubation (T2), after the lateral position (T3), after skin incision (T4), before dura mater incision (T5), before cerebrospinal fluid release (T6), after cerebrospinal fluid release (T7), during microvascular decompression (T8), after microvascular decompression (T9), after dura mater closure (T10), and at the end of the operation (T11).
Primary Outcomes
The CMAP amplitude at T5–T10 was recorded, and the amplitude at T5 was used as the base value. The difference in amplitude between each time point and T5 was calculated for all patients. The mean difference in amplitude between T10 and T5 was used as the primary outcomes. The success rate of intraoperative AMR monitoring was recorded.
Secondary Outcomes
For all patients, the heart rate, mean blood pressure, BIS value, and other indicators were recorded at each time point. The satisfaction of IONM physicians, intubation reaction rate, pain on injection rate, complication rate, anesthesia duration, operation duration, recovery time from anesthesia, PACU duration, dosage of main anesthetic drugs (propofol, remifentanil, ciprofol), dosage of vasoactive drugs (norepinephrine) were recorded too.
Criteria for Efficacy Assessment
In the trial, recovery time from anesthesia was defined as the time from drug withdrawal at the end of surgery to a Ramsay score of 2 or less. Operation duration time was defined as the time from skin incision to skin suture. Intubation response in the study was defined as an increase in mean arterial pressure and/or heart rate greater than 20% of the baseline value within 1 min after intubation.Citation21 The criteria for successful AMR monitoring were as follows: Typical AMR waves could be detected when the offending vessel compressing the root of the facial nerve was detected by the surgeon; When the surgeon placed a spacer between the offending vessel and the compressed facial nerve, the AMR wave disappeared. The efficacy evaluation criteria were as follows: Complete disappearance of symptoms as the cure; The symptoms basically disappeared, and only under certain circumstances, such as emotional stress, were they significantly relieved occasionally. The symptoms were reduced, but there were still daily attacks as partial remission; No change or worsening of symptoms was considered to be ineffective. Both the cure and marked remission were considered to be effective.
Sample Size Calculation
This non-inferiority study was based on the Primary outcome, and the sample size was calculated according to the comparison of the means of the two samples of the measurement data. In our pilot study, the difference between the amplitude of CMAP at the T10 time point and the T5 time point in the ciprofol group was 49.59, with a standard deviation of 33.02, while the mean amplitude of the propofol group was 37.02, and the standard deviation was 33.49. The non-inferiority value was set as 1/5 of the standard deviation, with a power of 80% and an α value of 0.025, β = 0.20. The sample ratio of the two groups was 1:1, with a dropout rate of 20%. According to the formula method, the sample size of each group was about 59 cases, and 60 cases were finally included in the experimental group, with a total number of 120 cases.Citation22
Statistical Analysis
Data analysis was performed using SPSS 26.0 (IBM Corp). Continuous variables were tested for normal distribution using the Shapiro–Wilk test. The primary outcome was described using the mean ± standard deviation, and the comparison between the two groups was performed using an independent sample T test. The measurement data conforming to a normal distribution were expressed as the mean ± standard deviation, and an independent sample T test was used to compare the means of the two samples (such as recovery time from anesthesia, PACU duration, hospitalization costs, et al). Measurement data with a non-normal distribution were expressed as the median and the interquartile range, and a comparison between the two samples was performed using the Mann–Whitney U rank sum test (such as age, body mass index, sedative consumption, remifentanil dosage, norepinephrine consumption, procedure duration, anesthesia duration, postoperative hospital stay, et al). Categorical data were compared using the chi-square test or Fisher’s exact probability test (such as monitoring success rate, efficiency of surgery, intubation reaction rate, pain on injection). P < 0.05 was considered to be statistically significant.
Results
Patient Disposition and Baseline Characteristics
A total of 131 patients with HFS who underwent microvascular decompression under IONM were screened: 125 were eligible, five were excluded for various reasons, and 120 underwent randomization. All participants were randomly assigned to the two groups, with no losses or dropouts (). The basic information of all enrolled patients is shown in . There were no significant differences in baseline data between the two groups. The incidence of left HFS accounted for 61.7% (74/120) of all patients, with the proportion of women being 63.3% (76/120).
Table 1 Details of the Participating Patients
Efficacy
The mean values of the primary outcome in the ciprofol group and the propofol group were 64.7 ± 44.1 and 53.4 ± 35.4, respectively. Moreover, the 95% confidence interval of the difference was −25.78 to 3.12, with the upper limit of the difference being lower than the non-inferiority boundary of 6.6. At the same time, there was no statistically significant difference between the two groups in the monitoring success rate, the efficiency of surgery, and the satisfaction of IONM physicians (P>0.05) (). Ciprofol could achieve non-inferior effectiveness in comparison with propofol in IONM of MVD surgery.
Table 2 Primary and Second Outcomes of Patients
The result during anesthesia induction showed that the magnitude of the blood pressure drop and the incidence of injection pain in the ciprofol group were significantly lower than those in the propofol group (P<0.05), while the incidence of intubation reaction and the bradycardia rate were not significantly different between the two groups (P>0.05). ().
Safety
There was no statistically significant difference between the two groups in terms of operation duration and anesthesia duration. During the surgical procedure, the sedative drug and norepinephrine consumption in the ciprofol group was significantly lower than that in the propofol group (P<0.05). The two groups could achieve a similar stable anesthetic effect for the duration and proportion when BIS was maintained at 40–60 (). In addition, the ciprofol group exhibited a non-inferior performance to that of the propofol group in terms of the postoperative complications rate, the postoperative hospital stay and the hospitalization cost.
Table 3 Surgical and Anesthetic Drug Related Outcomes of Patients
Discussion
This prospective randomized controlled study was performed during elective MVD of the facial nerve with IONM under general anaesthesia. Although it was total intravenous anaesthesia, there was no intraoperative awareness in both groups, which may be related to the application of BIS monitoring. In this trial, there was no significant difference between the two groups in terms of the duration and proportion of BIS values between 40 and 60 during anesthesia maintenance (P > 0.05), indicating that ciprofol was non-inferior to propofol in terms of sedation during general anaesthesia. While the dosage of sedative drugs used in the ciprofol group was significantly lower than that in the propofol group, it suggests that the efficacy of ciprofol in maintaining BIS 40–60 may be higher than that of propofol. Compared with propofol, ciprofol had a comparable operation time, PACU duration, postoperative hospital stay, and postoperative nausea and vomiting rate (P > 0.05). Patients in the ciprofol group had a shorter recovery time than that of the control group (P<0.05), while the operation duration and anesthesia duration were similar between the two groups (P>0.05). Theoretically, the metabolism time of ciprofol is not faster than that of propofol, which may be due to the effect of propofol accumulation during the long operation time. Compared with propofol, the unit price of ciprofol was more expensive, while the amount of intraoperative consumption was lower. There was no significant difference in hospitalization costs between the two groups, indicating that ciprofol did not increase the additional economic burden of patients. These results indicate that ciprofol can be safely used in the maintenance of anesthesia during general anaesthesia, and is not inferior to propofol in terms of the intraoperative sedation and anesthesia effect.
IONM has a profound effect on the diagnosis and treatment of hemifacial spasm during microvascular decompression. AMR, CMAP, and auditory evoked potential are the main electrophysiological monitoring indicators during MVD. AMR is a characteristic electrophysiological manifestation of HFS. When one branch of the affected side nerve is stimulated during surgery, the evoked EMG response can be recorded in the other branch, which is called AMR (). AMR is helpful in identifying the offending vessels and in judging whether the decompression is adequate and whether the offending vessels are missed.Citation23 CMAP and auditory evoked potential can sensitively reflect the effects of a local operation and drugs on nerve function. Intraoperative electrophysiological monitoring is of great help in improving the efficacy of MVD and reducing complications.Citation1,Citation24 However, the accuracy of electrophysiological monitoring is highly susceptible to external factors. Studies have shown that inhaled anesthetics such as isoflurane, sevoflurane, desflurane, etc. have a significant inhibitory effect on IONM.Citation25 Generally, intravenous drugs such as propofol and remifentanil have a little effect on IONM at common doses, while muscle relaxants have a great effect on IONM. Therefore, total intravenous anesthesia with less muscle relaxants is often used for surgery that requires electrophysiological monitoring. Changes in the dosage and usage of anesthetic drugs may lead to adverse events such as body movement, bucking, and intraoperative awareness. Therefore, in order to reduce the influence of IONM and ensure a comfortable and safe surgical environment, the choice of anesthetic drugs is particularly important. The results of this trial show that ciprofol is non-inferior to propofol in terms of electrophysiological and surgical outcomes. The reduction of the CMAP amplitude in the ciprofol group was non-inferior to that in the propofol group (64.7±44.1 vs 53.4±35.4), and the upper limit of the 95% confidence interval (−25.78 to 3.12) of the difference between the two groups was below the non-inferiority boundary of 6.6. There was no significant difference in the success rate of electrophysiological monitoring, the effective rate of surgery, the satisfaction rate of monitoring, and neurological complications between the ciprofol group and the propofol group (P > 0.05). The results indicate that ciprofol can be safely used in electrophysiological monitoring of MVD surgery without affecting the results of IONM.
Increasing evidence has shown that intraoperative hypotension is associated with an increased rate of organ damage to the heart, kidneys, brain, and other organs, and increases mortality in patients with high risk factors.Citation26,Citation27 A meta-analysis showed that patients with HFS were more likely to develop hypertension than were other populations.Citation28 The majority of our patients were middle-aged or older, and 43 patients (35.8%) had hypertension. The results of this trial showed that the application of ciprofol in MVD surgery under IONM had more advantages in terms of hemodynamic stability. The dosage of norepinephrine in the ciprofol group was significantly lower than that in the control group (P < 0.05). This advantage can also be explained by the results of the trial, in which patients in the ciprofol group had a significantly lower decrease in blood pressure during anesthesia induction than did those in the propofol group. At the same time, the incidence of induced injection pain in the ciprofol group was lower, which was more in line with the concept of comfort. The satisfaction score after induction by the anesthesiologists in the ciprofol group (80%) was higher than that in the propofol group (70%) (P>0.05). The advantages of ciprofol in terms of blood pressure stability and induction comfort partly indicate that ciprofol is more suitable for MVD surgery under IONM than propofol.
A limitation of this study is that only MVD procedures of functional neurosurgery were included; safety and efficacy in other tumour resection procedures that require IONM need to be further evaluated. In addition, the patient’s postoperative nausea and vomiting may be related to intracranial hypotension caused by the intraoperative release of cerebrospinal fluid. Because this study was not designed to assess nausea and vomiting, the incidence of nausea and vomiting during postoperative hospital stay and preventive measures should be further analyzed in future studies.
Conclusion
In conclusion, ciprofol and propofol can be safely used in microvascular decompression surgery with IONM. Ciprofol is not inferior to propofol in terms of the effectiveness of IONM and the surgical outcome. Concurrently, ciprofol has more advantages in inducing comfort and hemodynamic stability in comparison with propofol, which may be more suitable for IONM-related surgery, and has a broad application prospect.
Institutional Review Board Statement
This study was reviewed and approved by the Ethical Committees of the First Affiliated Hospital of USTC.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
Assistance with the study: none
This study was funded by Beijing Kangmeng charity Foundation (S063B). The funders had no role from study design to submission of the paper for publication. I would like to express my gratitude to Rongrong Yan for her assistance with the research design and paper writing.
Data Sharing Statement
Data are available from the corresponding author (Juan Li) on reasonable request.
Additional information
Funding
References
- Park SK, Joo BE, Park K. Intraoperative Neurophysiological Monitoring during Microvascular Decompression Surgery for Hemifacial Spasm. J Korean Neurosurg Soc. 2019;62(4):367–375.
- Nugroho SW, Perkasa SAH, Gunawan K, et al. Predicting outcome of hemifacial spasm after microvascular decompression with intraoperative monitoring: a systematic review. Heliyon. 2021;7(2):e06115.
- Simons SHP, van der Lee R, Reiss IKM, et al. Clinical evaluation of propofol as sedative for endotracheal intubation in neonates. Acta Paediatr. 2013;102(11):e487–e492.
- Ferrier DC, Kiely J, Luxton R. Propofol detection for monitoring of intravenous anaesthesia: a review. J Clin Monit Comput. 2022;36(2):315–323.
- Chan VW, Chung FF. Propofol infusion for induction and maintenance of anesthesia in elderly patients: recovery and hemodynamic profiles. J Clin Anesth. 1997;8(4):317–323.
- Jiang C, Qian H, Luo S, et al. Vasopressors induce passive pulmonary hypertension by blood redistribution from systemic to pulmonary circulation. Basic Res Cardiol. 2017;112(3):21.
- Euasobhon P, Dej-Arkom S, Siriussawakul A, et al. Lidocaine for reducing propofol-induced pain on induction of anesthesia in adults. Cochrane Database Syst Rev. 2016;2(2).
- Desousa KA. Pain on propofol injection: causes and remedies. Indian J Pharmacol. 2016;48(6):617–623.
- Jiang J, Jiao Y, Gao P, et al. Propofol differentially induces unconsciousness and respiratory depression through distinct interactions between GABAA receptor and GABAergic neuron in corresponding nuclei. Acta Biochim Biophys Sin (Shanghai). 2021;53(8):1076–1087.
- Qin L, Ren L, Wan S, et al. Design, synthesis, and evaluation of novel 2,6-disubstituted phenol derivatives as general anesthetics. J Med Chem. 2017;60(9):3606–3617.
- Bian Y, Zhang H, Ma S, et al. Mass balance, pharmacokinetics and pharmacodynamics of intravenous HSK3486, a novel anesthetic, administered to healthy subjects. Br J Clin Pharmacol. 2021;87(1):93.
- Liu Y, Yu X, Zhu D, et al. Safety and efficacy of ciprofol vs. propofol for sedation in intensive care unit patients with mechanical ventilation: a multi-center, open label, randomized, Phase 2 trial. Chin Med J (Engl). 2022;135(9):1043–1051.
- Liu Y, Chen C, Liu N, et al. Efficacy and Safety of Ciprofol Sedation in ICU Patients with Mechanical Ventilation: a Clinical Trial Study Protocol. Adv Ther. 2021;38(10):5412–5423.
- Hu C, Ou X, Teng Y, et al. Sedation Effects Produced by a Ciprofol Initial Infusion or Bolus Dose Followed by Continuous Maintenance Infusion in Healthy Subjects: a Phase 1 Trial. Adv Ther. 2021;38(11):5484–5500.
- Ludhrook G, Li FQ, Sleigh J, et al. Assessments of onset and duration of drug effects and pharmacokinetics by dose level of HSK3486, a new sedative-hypnotic agent, in healthy female/male subjects: a phase I multiarm randomized controlled clinical trial. Anesth Analg. 2021;133(1):e16.
- Bian YC, Zhang H, Ma S, et al. Mass balance, pharmacokinetics and pharmacodynamics of intravenous HSK3486, a novel anaesthetic, administered to healthy subjects. Br J Clin Pharmacol. 2021;87(1):93–105.
- Teng Y, Ou M, Wang X, et al. Efficacy and safety of ciprofol for the sedation/anesthesia in patients undergoing colonoscopy: phase IIa and IIb multi-center clinical trials. Eur J Pharm Sci. 2021;164:105904.
- Li X, Yang D, Li Q, et al. Safety, pharmacokinetics, and pharmacodynamics of a single bolus of the γ-aminobutyric acid (GABA) receptor potentiator HSK3486 in healthy Chinese elderly and non-elderly. Front Pharmacol. 2021;12:1–11.
- Lu M, Liu J, Wu X, et al. Ciprofol: a Novel Alternative to Propofol in Clinical Intravenous Anesthesia? Biomed Res Int. 2023;2023:7443226.
- Chen X, Guo P, Yang L, et al. Comparison and clinical value of ciprofol and propofol in intraoperative adverse reactions, operation, resuscitation, and satisfaction of patients under painless gastroenteroscopy anesthesia. Contrast Media Mol Imaging. 2022;2022:9541060.
- Kakkar A, Tyagi A, Nabi N, et al. Comparison of clonidine and dexmedetomidine for attenuation of laryngoscopy and intubation response - A randomized controlled trial. Clin Anesth. 2016;33:283–288.
- Jia H, Deng W, Wang S. Design Ang Statistical Analysis of Clinical Trials. 2th ed. Bei Jing: People’s Medical Publishing House; 2022.
- Song H, Xu S, Fan X, et al. Prognostic value of lateral spread response during microvascular decompression for hemifacial spasm. J Int Med Res. 2019;47(12):6120–6128.
- Jeon C, Jung NY, Kim M, et al. Intraoperative Monitoring of the Facial Nerve during Microvascular Decompression for Hemifacial Spasm. Life (Basel). 2023;13(7):1616.
- Sahinovic MM, Gadella MC, Shils J, et al. Anesthesia and intraoperative neurophysiological spinal cord monitoring. Curr Opin Anaesthesiol. 2021;34(5):590–596.
- Saugel B, Bebert EJ, Briesenick L, et al. Mechanisms contributing to hypotension after anesthetic induction with sufentanil, propofol, and rocuronium: a prospective observational study. J Clin Monitor Comput. 2021;36:341–347.
- Wesselink EM, Kappen TH, Torn HM, et al. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121:706–721.
- Leong JL, Li HH, Chan LL, et al. Revisiting the link between hypertension and hemifacial spasm. Sci Rep. 2016;6:21082.