Abstract
Evidence suggesting that central nervous system γ-aminobutyric acid (GABA) concentrations are reduced in patients with major depressive disorder (MDD) has been present since at least 1980, and this idea has recently gained support from more recent magnetic resonance spectroscopy data. These observations have led to the assumption that MDD’s underlying etiology is tied to an overall reduction in GABA-mediated inhibitory neurotransmission. In this paper, we review the mechanisms that govern GABA and glutamate concentrations in the brain, and provide a comprehensive and critical evaluation of the clinical data supporting reduced GABA neurotransmission in MDD. This review includes an evaluation of magnetic resonance spectroscopy data, as well as data on the expression and function of the GABA-synthesizing enzyme glutamic acid decarboxylase, GABA neuron-specific cell markers, such as parvalbumin, calretinin and calbindin, and the GABAA and GABAB receptors in clinical MDD populations. We explore a potential role for glial pathology in MDD-related reductions in GABA concentrations, and evidence of a connection between neurosteroids, GABA neurotransmission, and hormone-related mood disorders. Additionally, we investigate the effects of GABAergic pharmacological agents on mood, and demonstrate that these compounds have complex effects that do not universally support the idea that reduced GABA neurotransmission is at the root of MDD. Finally, we discuss the connections between serotonergic and GABAergic neurotransmission, and show that two serotonin-focused antidepressants – the selective serotonin-reuptake inhibitor fluoxetine and the multimodal antidepressant vortioxetine – modulate GABA neurotransmission in opposing ways, despite both being effective MDD treatments. Altogether, this review demonstrates that there are large gaps in our understanding of the relationship between GABA physiology and MDD, which must be remedied with more data from well-controlled empirical studies. In conclusion, this review suggests that the simplistic notion that MDD is caused by reduced GABA neurotransmission must be discarded in favor of a more nuanced and complex model of the role of inhibitory neurotransmission in MDD.
Introduction
Major depressive disorder (MDD) is a heterogeneous, highly prevalent, and severe psychiatric disorder that affects more than 350 million people worldwide, and is currently thought to be the leading contributor to the global disease burden.Citation1 Although classically conceived as a disorder of mood, MDD is also associated with a high degree of cognitiveCitation2 and functional disability, resulting in high socioeconomic burden due to the direct costs of treatment and indirect costs, such as unemployment or reduced productivity of the patient and their caregivers. Patients with MDD are more likely to be unemployed than healthy controls, and those that are employed are more likely to be absent.Citation3 In fact, recent estimates suggest that MDD costs $24 billion yearly in the US in absenteeism and reduced productivity alone.Citation3
The advancement of pharmacotherapies for MDD over the last several decades has resulted in a broad set of effective options for treating patients with MDD. However, a bourgeoning line of evidence suggests that although currently available monoamine-centered antidepressant treatments, such as selective serotonin-reuptake inhibitors (SSRIs) and serotonin–norepinephrine reuptake inhibitors (SNRIs) induce clinically relevant improvements in mood for most MDD patients, the cognitive and functional disability associated with this disease tend to persist.Citation4 Furthermore, these treatments are altogether ineffective for a large subset of depressed patients, and for many others symptom relief is delayed by several weeks after the start of treatment. These issues highlight the strong need to advance our understanding of MDD’s biological underpinnings, in order to find novel treatments capable of resolving these unmet clinical needs.
MDD has unquestionably a heterogeneous set of biological underpinnings, and this is reflected by the numerous etiological theories about MDD, which include theories implicating altered regulation of monoamine neurotransmission,Citation5 sleep,Citation6 and excitatory glutamatergic neurotransmission.Citation7 Another accreting narrative has recently suggested that dysregulation of the inhibitory amino acid neurotransmitter γ-aminobutyric acid (GABA) is involved in the etiology of MDD, with the broad theme that MDD is related to reduced inhibitory GABA neurotransmission. This review seeks to present a critical evaluation of the clinical evidence supporting dysregulated GABA neurotransmission in MDD, the potential for treating MDD using GABAergic mechanisms, and the possibility that serotonergic antidepressants may act in part via modulation of GABAergic neurotransmission.
Regulation of GABA and glutamate in the central nervous system
Before reviewing the data on GABA’s role in MDD, we first summarize the mechanisms by which GABA and the closely related excitatory amino acid neurotransmitter glutamate are synthesized, inactivated and catabolized in the central nervous system (CNS).
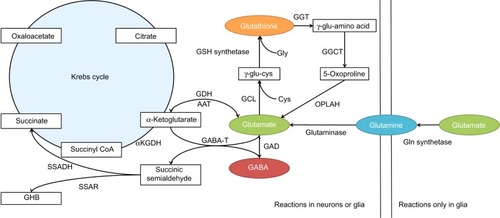
GABA synthesis
GABA is produced in the CNS via decarboxylation of glutamate, in a reaction catalyzed by glutamic acid decarboxylase (GAD; ). This process is thought to occur overwhelmingly in neurons, with glia producing essentially no GABA via this metabolic pathway.Citation8 In general, GAD’s enzymatic activity is thought to be regulated through two processes: 1) the level of enzyme expression, and 2) the degree of association with its cofactor – pyridoxal phosphate (PLP).Citation9
Figure 1 Amino acid neurotransmitter synthesis and catabolism. The synthesis and catabolism of GABA and glutamate are tightly interconnected in the brain.
GAD is known to have two separate isoforms in the mammalian CNS – the 65 kDa isoform (GAD65) and the 67 kDa isoform (GAD67) – which are encoded by different genes, have separate patterns of intracellular expression, and are functionally regulated by dissimilar mechanisms. Immunolabeling studies have suggested that GAD65 is located primarily in synaptic terminals, where it is associated with the production of GABA for classical Ca2+-dependent exocytotic release. The majority of GAD65 is dissociated from PLP under normal circumstances, and can markedly increase its activity as demand for synaptic GABA release increases.Citation10 Therefore, the association with its cofactor, rather than the level of expression, appears to be the primary mechanism regulating the metabolic activity of GAD65 in the CNS.Citation9
In contrast, GAD67 is expressed throughout the cytosol, and is primarily associated with PLP under normal conditions. Therefore, rather than being regulated by its association with PLP, GAD67’s enzymatic activity is regulated by its level of expression. Moreover, GAD67’s ubiquitous cytosolic expression and high levels of association with PLP have led to an interpretation that this isoform is primarily involved in cellular metabolic activities via the GABA shunt,Citation8 and is responsible for the majority of the GABA synthesis in the brain.Citation9 However, it has been suggested that cytosolic GABA can be released into the extracellular space via a Ca2+-independent, nonexocytotic mechanism mediated by high-affinity GABA carriers.Citation9 If true, then it is possible that GAD67 plays a role in inhibitory neurotransmission via the stimulation of extrasynaptic GABA receptors. Additionally, it may be that a portion of GAD67-derived GABA is involved in classical exocytotic release, given that GAD65 and GAD67 are both expressed in axon terminals. Therefore, it is not clear based on currently available data whether GABA originating from GAD65 and GAD67 constitutes fully discrete intracellular pools with firmly separated physiological roles.Citation11
GABA inactivation and catabolism
After being released into the extracellular space, GABA is primarily inactivated via reuptake transport, a process that is driven in the CNS by the GABA-selective reuptake transporters GAT-1 and GAT-3.Citation12 GABA transporter proteins can either be expressed on neurons or glial cells. In neurons, the recaptured GABA can either be repackaged for vesicular release or catabolized via the GABA shunt (), while GABA captured by glia will largely be catabolized.
Whether it occurs in neurons or glia, GABA catabolism is mediated primarily through the enzyme GABA transaminase (GABA-T). GABA-T is a PLP-dependent enzyme that requires both GABA and α-ketoglutarate as cosubstrates, yielding glutamate and succinic semialdehyde (SSA) as reaction products (). SSA can either be metabolized into γ-hydroxybutyric acid (GHB), which can have a role in modulating GABAB receptors, or it can be dehydrogenated into succinate.Citation12 GABA that has been dehydrogenated to succinate via SSA dehydrogenase is then thought to enter the Krebs cycle, where it plays a role in cellular energy metabolism.
Glutamate synthesis
Glutamate may be somewhat unique among central neurotransmitters, in that it has a multiplicity of neurochemical pathways by which it can be produced (). Within the CNS, the majority of glutamate is produced from glutamine via the enzyme glutaminase. However, glutamate can also be produced from α-ketoglutarate via several enzymes, including aspartate aminotransferase, or in the GABA shunt via GABA-T. Additionally, central glutamate stores can be derived, at least in part, from the glutathione-cycle metabolite 5-oxoproline.Citation13
Glutamate inactivation and catabolism
As with GABA, neuron-released glutamate is primarily inactivated by uptake from the synapse via high-affinity transport mechanisms. In the case of neurons, this process is mediated by excitatory amino acid transporter (EAAT)-3 in humans (known as excitatory amino acid carrier 1 in rodents), while for glial cells it is mediated via EAAT1/2 (in rodents, glial uptake is mediated by the glutamate aspartate transporter or glutamate transporter 1, respectively). Glutamate that is captured in glial cells is catabolized into glutamine by glutamine synthetase, which is then transported to neurons to be remade into glutamate. This so-called glutamate–glutamine cycle is thought to be the primary source of neuron-released glutamate,Citation14 and may also represent a major source of the glutamate that is used to produce GABA.Citation15 Glutamate also has multiple catabolic pathways, which are depicted in .
Evidence for altered GABAergic neurotransmission in MDD: a critical look at the data
GABA concentrations in MDD assessed by magnetic resonance spectroscopy
Neuroscientists have been investigating the potential connection between GABA physiology and MDD for many years, beginning with the observation that GABA concentrations were reduced in the cerebrospinal fluid (CSF) of MDD patients.Citation16 More recently, with the advent of magnetic resonance spectroscopy (MRS) imaging, it has been repeatedly demonstrated that CNS GABA concentrations are reduced in some MDD patients (). These findings have been most consistent in the occipital cortex (OCC), where several reports have shown reductions compared to healthy controls.Citation17–Citation20 These observations have been replicated in brain regions such as the anterior cingulate cortexCitation18 and in some but not all prefrontal cortex (PFC) areas.Citation21 It is possible that reductions in OCC GABA concentrations are specific to a subpopulation of treatment-resistant patients, as at least one study has shown that treatment-resistant, but not non-treatment-resistant, MDD patients have reduced OCC GABA concentrations.Citation18
Table 1 The relationship between major depressive disorder and GABA concentration measured by magnetic resonance spectroscopy
If major depression is related to reduced GABA concentrations, then a corollary may be the idea that effective treatment for depression should normalize GABA. Some reports have suggested that effective treatment with antidepressantsCitation22 or electroconvulsive therapyCitation23 leads to an increase in GABA concentrations in the OCC when assessed compared to the patient’s own baseline. Additionally, some research groups have shown that there are no differences in GABA concentrations between remitted depressed patients and controls in the PFCCitation24,Citation25 and OCC.Citation25 These results alone seem to support the idea that MDD is associated with reduced GABA concentrations. However, Sanacora et al later found that effective cognitive behavioral therapy treatment led to a nonsignificant trend toward a reduction in OCC GABA concentrations,Citation26 while Bhagwagar et al showed that OCC GABA concentrations in recovered MDD patients were still reduced compared to healthy controls.Citation27,Citation28 These differing results may reflect methodological differences in the detection of GABA,Citation25 brain region-specific relationships between GABA concentrations and depression, or differences in the mechanism of antidepressant treatments.
Therefore, the overall consensus appears to be that GABA concentrations are down in the CNS of depressed patients, at least in some brain regions and in treatment-resistant or severely depressed patients. However, there are not enough data available to develop a firm consensus on whether these altered GABA concentrations represent consistent biomarkers for depression states, and in fact there is some evidence both for and against this notion. However, it should be noted that in many cases, depressed patients have cognitive dysfunction that persists even after mood symptoms have been reduced by “successful” antidepressant treatment.Citation29 It is possible that remaining GABA reductions after the retreat of depressed affect are related to a persisting syndrome of cognitive dysfunction. However, none of these studies has evaluated the cognitive state of the patients before and after antidepressant treatment, so this idea is purely speculation at this time. Furthermore, whether the observed reductions in GABA concentrations are circumscribed to specific brain regions or whether there is a broader pattern of reduced CNS GABA concentrations remains unclear. Additionally, given the fact that cellular GABA pools can be loosely separated into metabolic and neurotransmitter subcompartments, with the metabolic compartment representing the lion’s share of cellular GABA,Citation8 it is not possible based on MRS data alone to determine whether the reduced GABA concentrations observed in MDD patients are actually related to changes in GABAergic neurotransmission. These issues can only be clarified with more empirical data. Moreover, as the technology of MRS advances, it will be preferable if future studies focus more heavily on brain regions with greater theoretical relevance to depression-related changes in affect and cognitive function.
GAD expression in MDD patients
If GABA concentrations are reduced in the brain of MDD patients, then it makes sense to look for altered physiology in GAD, the enzyme that produces GABA. Several research groups to date have investigated either the expression or function of GAD in postmortem brains from MDD patients, and these data are summarized in . Unfortunately, there is some mismatch between the brain regions studied using protein- or gene-expression techniques, which have focused most heavily on the frontal cortex, compared to the MRS studies that have tended to focus on the OCC due to technological limitations. In the frontal cortex, one research group reported that medication-free MDD patients had a significant reduction in the expression of GAD67 compared to healthy control subjects,Citation30 but found that there was no difference in medicated MDD patients versus controls. These data may be in line with MRS data showing reduced GABA concentrations in the dorsal PFC in untreated but not treated depressed patients.Citation21,Citation24 An investigation of GAD67 expression in the cerebellum in a small group of MDD patients compared to controls also found a significant reduction in MDD patients.Citation31 However, other groups that have investigated GAD67 protein expression using either Western blot,Citation32 immunohistochemistry,Citation33 or gene expression using quantitative polymerase chain reaction (PCR),Citation34 have found no significant changes in GAD67 expression in the frontal cortex of MDD patients. Therefore, the evidence that GAD67 expression is altered in the brain of depressed patients is currently equivocal at best. It should be noted, however, that the majority of these studies used tissue samples from a mix of patients who were treated and untreated, and thus may be confounded by the influence of antidepressant medications.
Table 2 The relationship between major depressive disorder and glutamic acid decarboxylase expression or function
While GAD67 expression may or may not be reduced in the frontal cortex of MDD patients, research groups that have investigated the expression of GAD65 in the frontal cortex of this patient population have universally shown that there are no changes compared to healthy control patients.Citation30,Citation32,Citation34 Conversely, in the cerebellum of MDD patients, Fatemi et alCitation31 observed a significant reduction in GAD65 expression compared to controls. However, it is important to point out that the primary method of regulating GAD65’s enzymatic activity is its association with PLP, not the degree of its expression, and the vast majority of GAD65 is dissociated from PLP under normal conditions (see earlier discussion under GABA synthesis). Therefore, it is not clear that this reduction in GAD65 expression is from an active enzyme population, and the relevance of this reduction is thus questionable.
In addition to data generated on the expression of specific GAD isoforms, several research groups have investigated the relationship between undifferentiated GAD and MDD in a number of brain regions using either immunohistochemical techniques or enzyme functional assays, and in general the findings have varied by the region studied. In the PFC, the overall results have been equivocal, with one study finding increased density of GAD-immunoreactive (IR) cells,Citation35 another finding significant decreases,Citation36 and a third finding no change.Citation37 Additionally, an investigation of GAD enzymatic activity in the PFC of suicide patients compared to healthy controls found no changes in GAD function.Citation38 Similarly, results in the orbitofrontal cortex, temporal cortex, and thalamus up to this point have had mixed results.Citation35,Citation37,Citation38 However, it appears that there is some agreement that the density of GAD-IR cells is increased in the entorhinal cortexCitation36,Citation37 and hippocampus of MDD patients.Citation35–Citation37
Based on these data, it appears that GAD expression or function is not strongly regulated in either direction in the frontal cortex of depressed patients, including the dorsal PFC, orbitofrontal cortex, and anterior cingulate cortex. Moreover, the seemingly consistent increases in GAD expression observed in the entorhinal cortex and hippocampus may suggest that GABA physiology is not altered in a monolithic, pan-CNS manner, but rather is regionally specific. In any case, at this time the data on GAD expression cannot be considered generally supportive of the idea that GABA concentrations are reduced in MDD due to changes in GAD function. However, there are several significant caveats to consider when evaluating these ideas. A number of these studies were confounded due to the presence of mixed samples of treated and untreated depressed patients, making it difficult to delineate how GAD would be regulated by MDD alone. In addition, these studies have tended to use small patient samples and are probably not numerous enough to confidently make claims about the population of depressed patients. Finally, there is little agreement between the MRS and GAD-expression literature in terms of the brain areas studied. Bearing these significant caveats in mind, it is probably premature to take a firm stance on how GAD expression is regulated in depressed patients, and how this may or may not be relevant to the observed reductions in GABA concentration. Moreover, in order to move this research forward, more studies are required that carefully control for the effects of antidepressant treatments, use larger sample sizes, and study brain regions that have also been studied using MRS.
GABAergic neuron-related Ca2+-binding proteins and the neuropeptide somatostatin
Another potential way to explain the reductions in GABA concentrations seemingly observed in MDD via MRS studies is to examine the density of GABAergic interneurons. To the extent that GABA neurons selectively express GAD in the CNS, the previous section may have already suggested that there are not any consistent changes in GABA neuron density in MDD. However, GABAergic interneurons can be further subdivided based on the expression of the calcium-binding proteins calbindin, calretinin, and parvalbumin (PV),Citation39 and it is possible that changes in GABAergic physiology in MDD are specific for one or more of these cell types. To our knowledge, only a few research groups have investigated the expression of these proteins in depressed patients, and as in studies of GAD have tended to focus on the frontal cortex. Perhaps the most consistent result has suggested that the density of calbindin-IR interneurons is significantly reduced in areas, including the dorsolateral PFC (DLPFC)Citation40 and OCC,Citation41 and trends toward a reduction in the orbitofrontal cortex.Citation40 Reports on the density of calretinin-IR and parvalbumin-IR interneurons in the DLPFC and orbitofrontal cortex have generally found no significant changes.Citation40,Citation42,Citation43 Therefore, it may be the case that there is a reduction in calbindin-IR interneurons in the cortex of depressed patients. However, this observation is based on only two studies in a cumulative sample of 24 depressed patients, and needs further replication before it can be thought of as a consistent biology in MDD.Citation40,Citation41
It should also be noted that several well-controlled studies have demonstrated that the expression of the neuropeptide somatostatin, which is commonly coreleased by GABAergic interneurons, is reduced in postmortem brains of MDD patients in such regions as the amygdala and subgenual cingulate.Citation44,Citation45
A role for glial pathology in disrupted GABA concentrations
It is important to note that there are several lines of histological evidence pointing to glial pathology in the frontal cortex of MDD patients. These observations include reductions in size and density of glia,Citation46 as well as reductions in the gene or protein expression of glial-specific markers, such as glial fibrillary acidic protein, the calcium-binding protein S100B, EAAT1, EAAT2, and glutamine synthetase.Citation47,Citation48 These glial pathologies can be theoretically important for a discussion of GABA neurotransmission from the perspective that glial cells, such as astrocytes, regulate glutamate–glutamine cycling through cellular machinery that includes EAAT1/2 and glutamine synthetase (see earlier discussion on Glutamate inactivation and catabolism). This process is thought to be a major neurochemical source of GABA,Citation14 in part because experimental disruptions of glutamate–glutamine cycling under depolarizing conditions significantly attenuate neuronal GABA pools.Citation15 In fact, there have been some suggestions that glutamate–glutamine cycling is more important for maintenance of GABA neurotransmitter pools than for glutamate stores.Citation49
Current thinking on the consequences of reduced glial density on neurotransmission has imagined a complex set of effects that include not only a reduction in the pool of glutamate available for synaptic neurotransmission but also an increase in the stimulation of extrasynaptic receptors due to the reduced glial uptake, leading to an altered ratio of synaptic to extrasynaptic signaling.Citation47,Citation48 Given that GABA metabolism and inactivation is regulated via glial mechanisms that are very similar to glutamate, the same ideas could be used for GABA neurotransmission in MDD. This theory could plausibly explain the reduced concentrations of GABA observed in MRS studies of MDD, as well as the observations of reduced concentrations of GLX, a combined measure of glutamate and glutamine.Citation50
Although the idea of a compartmentalized effect of glial dysfunction on synaptic and extrasynaptic amino acid neurotransmission is certainly plausible, it is not entirely supported by the data in nonclinical model systems. The idea that reduced postsynaptic GABA neurotransmission can result from disrupted glutamate–glutamine cycling has been observed in nonclinical models.Citation51 However, Paulsen and FonnumCitation49 investigated the effects of both a selective glial lesion and pharmacological inhibition of glutamine synthetase on basal and potassium-stimulated extracellular GABA and glutamate concentrations. These authors found that within the first 2–3 hours of either treatment, extracellular concentrations of glutamate and GABA were indeed higher, but after 6–7 hours the extracellular concentrations of both amino acid transmitters fell well below those of the control condition. These data do not support the idea that glial pathology would drive compartmentalized effects on synaptic versus extrasynaptic amino acid neurotransmission over a long time frame, although it is possible that the translatability of the models used in this study may be questioned. However, glial pathology is still a plausible explanation for the reduced cortical GABA concentrations observed in MDD.
Cortical silent period and short-interval cortical inhibition
It can be argued that electrophysiological measures associated with transcranial magnetic stimulation, such as cortical silent period and short-interval cortical inhibition, provide evidence of disrupted GABA neurotransmission in depressed patients.Citation52 While it is true that manipulating GABAergic neurotransmission can induce changes in these measures, this can also be said of other neurotransmitter systems.Citation53 Therefore, it seems that there is a complicated physiology underlying cortical silent period and short-interval cortical inhibition that make it difficult to clearly interpret the causes of any changes observed in MDD patients. Therefore, data on these electrophysiological measures have not been considered in this review.
GABA receptors in MDD
GABAA receptors
GABAA receptors are pentameric transmembrane ion channels that have heterogeneous subunit composition and anatomical expression patterns, and are thought to mediate the majority of fast inhibitory neurotransmission in the CNS. The subunit composition of GABAA receptors determines a number of functional factors, including subcellular localization (eg, synaptic versus extrasynaptic localization), channel open probabilities, desensitization rate, and modulatory ligand affinity.
Unfortunately, although there has been evidence that central GABA physiology is altered in MDD since at least 1980, there is a relative paucity of research that has investigated whether altered composition or function of GABAA receptors is present in the brain tissue of clinical MDD populations. Recently, however, a few studies have shown changes in GABAA receptor-gene expression in depressed patients compared to controls. For example, Choudary et alCitation54 found upregulation of the genes governing several GABAA receptor subunits, including GABAAβ3, GABAAδ, and GABAAγ2, in the frontal cortex. Similarly, a larger analysis of multiple brain regions using PCR in depressed suicide victims demonstrated altered expression of numerous GABA receptor-subunit genes, most of which were related to the GABAA receptor (19 of the 27 differentially regulated GABAergic genes), and were mostly upregulated. This notably included increased expression of GABRA5 (coding for the GABAAα5 receptor subunit) and GABRG2 (GABAAγ2 receptor subunit) in the DLPFC and the inferior temporal cortex,Citation55 and reduced expression of GABRG1 in the DLPFC. However, the expression pattern was found to be region-specific. On the basis of gene-expression data alone, it is tempting to conclude that the GABAA receptor is implicated in the pathophysiology of MDD, at least in those patients who committed suicide.
Studies using protein-expression techniques have also found some evidence of changes in GABAA receptor in tissue from depressed patients. For example, Fatemi et alCitation56 found significant increases in GABAA-receptor α1, α2, α6, γ3, and ε subunits in the lateral cerebellum of depressed patients compared to controls, as well as a reduction in the β1 subunit, although significance for the α2, γ3, and β1 subunits was lost when the authors statistically controlled for the effects of antidepressant treatments. Unfortunately, at the time of writing, we were not able to identify any studies that looked at the expression of GABAA-receptor subunits in the frontal cortex, and thus it is difficult to compare these results to the gene-expression data discussed, or to arrive at a consensus on how GABAA receptors are regulated in depression.
Given that the benzodiazepine-binding site is localized between the α- and γ-receptor subunits, the altered expression of the messenger ribonucleic acid (mRNA) governing expression of these subunits may make it plausible to expect that the binding of benzodiazepine-site ligands will be different in depressed patients compared to controls. Unfortunately, there is not much literature on benzodiazepine binding in depressed patients. A recent study by Klumpers et alCitation57 found significant reductions in benzodiazepine-site binding in the parahippocampal gyrus and right lateral superior temporal gyrus of a small sample of MDD patients. Another study found no significant changes in benzodiazepine-site binding in the temporal cortex or frontal cortex in untreated depressed suicide patients, but found significant frontal cortex binding increases only in cases where patients were receiving antidepressant treatment.Citation38 Three additional studies failed to find any differences in benzodiazepine-binding sites in depressed patients in the locus coeruleus,Citation58 the OCC in patients where low GABA concentrations were found via MRS,Citation17 or in the amygdala and hippocampus of suicide victims.Citation59 Therefore, although these results are largely negative, there has been very little overlap in the brain regions studied by these binding studies, leaving open the possibility that benzodiazepine-receptor expression is regulated in a regionally specific manner in MDD. Moreover, the lack of agreement on the brain regions that have been evaluated for benzodiazepine-site binding and altered expression of the genes governing GABAA-receptor expression make it difficult to evaluate whether the altered gene-expression pattern has led to changes in the function of the GABAA receptor. Once again, this issue can only be resolved with more empirical data. To our knowledge, there have been no attempts to investigate binding at the GABAA-receptor orthosteric site in MDD patients at this time.
GABAB receptors
The role of GABAB receptors in MDD has received little attention from the research community in comparison to the GABAA receptor. Fatemi et alCitation60 investigated the expression of GABAB receptors in the lateral cerebellum of depressed patients, and found reduced expression of the GABBR1 and GABBR2 subunits in a small sample of depressed patients compared to controls. However, studies that have investigated GABAB binding in the frontal cortexCitation61,Citation62 and in the temporal cortex and hippocampusCitation62 found no evidence of altered GABAB-receptor binding, with the exception of an increased affinity in the temporal cortex of drug-free suicide victims. Of course, studies in suicide victims can be criticized from the perspective that only a small population of depressed patients actually go through with suicide, and thus it may be argued that a different set of CNS biologies are at play in these patients compared to the broader MDD population. In any case, the available data do not convincingly point to an altered GABAB-receptor biology in MDD patients.
Neurosteroids, GABA neurotransmission, and mood dysfunction
Premenstrual syndrome (PMS) and the more severe premenstrual dysphoric disorder (PMDD), which are associated with a cyclical onset and retreat of negative mood symptoms, may represent clinically relevant examples of a connection between GABA neurotransmission and mood dysfunction. Although the mechanisms underlying these symptoms are not entirely clear, there is a line of evidence implicating abnormal responses to neuroactive steroids that are metabolically derived from ovarian hormones, such as the progesterone metabolite allopregnanolone, in the etiology of these disorders. The highest probability of negative mood onset in these disorders occurs during the late luteal phase, when levels of the ovarian hormone progesterone are falling. Although it should be noted that in PMDD, symptoms can also increase in the early luteal phase when progesterone levels are rising.Citation63 Schmidt et alCitation64 demonstrated that mood symptoms associated with PMS could be blocked by pharmacological inhibition of the menstrual cycle, perhaps helping to implicate hormonal fluctuations. However, these authors found that direct administration of estradiol or progesterone in women with PMS caused increases in negative mood that did not occur in healthy women. Similarly, Smith et alCitation65 used transcranial magnetic stimulation of the motor cortex to demonstrate that women with PMS had an increase in motor-cortex excitability during the luteal versus follicular phase, when within-subject progesterone levels were relatively higher. By comparison, cortical excitability during the luteal phase of control patients was reduced, and importantly these controls did not have different plasma progesterone or estradiol concentrations compared to patients during either phase. Given that the progesterone metabolite allopregnanolone modulates GABAA-receptor function, it seems plausible that the mood dysfunction associated with these disorders is related to abnormal neurosteroid regulation of GABA neurotransmission.
The weight of the available nonclinical data suggests that acute allopregnanolone administration positively modulates most GABAA-receptor conformations, resulting in enhanced GABA-mediated inhibitory neurotransmission.Citation66 Acute allopregnanolone administration also has well-recognized behavioral effects that are consistent with a positive modulatory effect on GABA neurotransmission, including anxiolyticCitation67 and seizure-reducingCitation68 properties. However, allopregnanolone’s effects on GABA neurotransmission are complex and acute administration of this steroid can have paradoxical effects under some conditions in nonclinical model systems,Citation69,Citation70 and in the clinic,Citation64 which can include reductions in GABA-mediated inhibition and anxiogenic properties.
Recent papers suggest that in nonclinical models, these paradoxical effects can be attributed to allopregnanolone’s negative modulatory effects on GABAA receptors containing the α4 and δ subunits.Citation69 The α4 and δ subunit-containing GABAA receptors are normally expressed at low levels in most brain regions, with notable exceptions, such as the dentate gyrus and thalamus.Citation71 However, during periods of fluctuating progesterone levels, eg, in progesterone-withdrawal models, GABAA-receptor composition shifts by sharply increasing the expression of the α4 and δ subunits in the CA1 subregion of the hippocampus,Citation72,Citation73 while at the same time reducing the expression of the α1 subunit.Citation63 In addition to producing paradoxical effects of allopregnanolone, this shift in GABAA receptor-subtype expression causes a complex set of changes to basal inhibitory neurotransmission. For example, the shift from α1 subunit-containing GABAA receptors to α4 subunit-containing GABAA receptors increases the decay kinetics of GABAA receptor-mediated inhibitory currents,Citation74 leading to reduced phasic inhibitory neurotransmission.Citation75 However the increase in δ-containing GABAA receptors, which are localized extrasynaptically and have a low desensitization rate,Citation74 induces an increase in tonic inhibitory neurotransmission.Citation69,Citation76 Therefore, the effects of progesterone withdrawal in nonclinical models can be conceptualized as a shift in the balance of phasic versus tonic GABA neurotransmission.
Moreover, there is some evidence suggesting that these changes in GABAA-receptor conformation are relevant to clinical disorders, such as PMDD. The shift from α1-containing GABAA receptors to α4-containing GABAA receptors in nonclinical model systems is associated with a reduction in sensitivity to positive allosteric modulation at the benzodiazepine site,Citation72 and a similar reduction in sensitivity to benzodiazepines has been observed in human patients with PMS. Therefore, it is plausible to suggest that the mood dysfunction associated with PMS and PMDD are related to increased expression of α4- and perhaps δ-containing GABAA receptors, suggesting a dysregulation of GABAergic neurotransmission. Moreover, data showing increased motor-cortex excitability in women with PMSCitation65 may suggest that inhibitory neurotransmission is overall reduced in this disorder. However, this idea may be complicated by evidence from an MRS study of GABA concentrations, which found that women with PMDD experienced increases in cortical GABA concentrations from the follicular to the luteal phase, when negative mood symptoms increased,Citation77 while control subjects had significantly reduced GABA concentrations across these menstrual phases. Therefore, while it is clear from the accumulated evidence that PMS and PMDD are related to dysregulated GABAergic neurotransmission, the precise nature of this relationship remains unclear at this time.
A relationship between neurosteroids and mood has also been proposed in MDD. Several studies have demonstrated that antidepressant treatments, such as the SSRI fluoxetine, can enhance the production of such neurosteroids as allopregnanolone. For example, preclinical models have demonstrated that acute intraperitoneal administration of 20 mg/kg fluoxetine significantly elevates the brain concentration of allopregnanolone in adrenalectomized, castrated male rats 30 minutes after injection,Citation78 which may suggest that fluoxetine treatment can indirectly modulate GABAA receptor-mediated neurotransmission. Interestingly, the same research group later suggested that intraperitoneal administration of 1.45 μmol/kg fluoxetine (equivalent to approximately 0.45 mg/kg of the base) was able to reverse reductions in brain allopregnanolone concentrations in mice induced by social isolation at 30 minutes after injection.Citation79 Given that the fluoxetine dose required to reach 80% occupancy at the mouse 5-hydroxytryptamine (HT) transporter protein (SERT) is approximately 8 mg/kg,Citation80 these data suggest that fluoxetine may have effects on neurosteroid concentrations in extremely low dose ranges. However, these data may also lead one to question the relevance of this mechanism to treatment response, based on clinical data suggesting that approximately 80% SERT occupancy is present at minimally effective SSRI doses in MDD patients.Citation81
We have identified a small number of studies to date that have measured changes in neurosteroid levels in MDD patients in response to treatment with antidepressants. Uzunova et alCitation82 measured CSF concentrations of such neurosteroids as allopregnanolone in a small patient sample (n=15), and found that at baseline, patients had substantially lower allopregnanolone concentrations than were found in a sample of three control patients. Furthermore, Uzunova et al found that allopregnanolone levels increased significantly with successful treatment with fluoxetine or fluvoxamine over a period of about 8 weeks. These data imply that normalization of CSF neurosteroid concentrations are related to the antidepressant effects of these drugs, which could have ramifications for GABAA receptor-mediated inhibitory neurotransmission. However, there are some caveats to consider when interpreting this study. Despite the fact that the majority of the subjects in this study were women (nine of 15) and allopregnanolone concentrations are known to fluctuate with the menstrual cycle, the authors failed to account for the menstrual status of the women in this study, and in fact most of the apparent variance in treatment effects on allopregnanolone in this study were focused in the female subjects. Therefore, the primary dependent measure of this study was confounded.
However, a separate research group presented another small but better-controlled study,Citation83 which found that a small sample of treatment-naïve outpatients with MDD had altered plasma neurosteroid concentrations compared to healthy controls. Specifically, allopregnanolone and 3α,5β-tetrahydroprogesterone were significantly reduced in patients compared to healthy control subjects, while 3β,5α-tetrahydroprogesterone was significantly increased. These differences were reversed by chronic treatment with fluoxetine. In another experiment presented in the same paper, the authors found similar but much smaller responses in neurosteroid concentrations to successful antidepressant treatments in a more severely depressed sample of patients. However, these authors found no correlation between plasma neurosteroid concentrations and therapeutic response in these experiments, again making the relevance of this neurosteroid response to MDD symptoms questionable. Interestingly, a third clinical studyCitation84 found that the antidepressant mirtazapine could significantly increase plasma allopregnanolone concentrations in a small group of patients where only about 40% responded to treatment by the end of the study. However, patients receiving mirtazapine with lithium as an adjuvant had a higher response rate (approximately 75%), but had no changes in plasma allopregnanolone concentrations, thus suggesting that elevated neurosteroid concentrations are not necessary for successful antidepressant treatment. Taken together, these data do suggest that some pharmacological antidepressant treatments are able to modulate neurosteroid concentrations in clinical MDD populations; however, the evidence supporting their relevance for clinical antidepressant efficacy is currently not strong.
GABA pharmacology and depressive symptoms
GABAergic interneurons are likely to exert a powerful regulatory influence on the neural networks responsible for controlling mood and cognitive function. Therefore, it may be possible to normalize the networks responsible for these symptoms in MDD by modulating GABA neurotransmission whether or not there is a primary GABAergic dysregulation at the root of MDD. However, if reduced GABA concentrations are an etiological factor in MDD, then it is logical to expect that increasing GABA neurotransmission should relieve depression-related symptoms, while treatments that reduce GABA neurotransmission should induce depressive symptoms.
Perhaps the best-characterized set of GABA-related pharmacological treatments in MDD is the benzodiazepine class of GABAA receptor-positive allosteric modulators (PAMs). Two review papers that examined the effects of benzodiazepines generally found that classical benzodiazepines, such as chlordiazepoxide and diazepam, are not effective at treating patients with MDD.Citation85,Citation86 However, both studies concluded that treatment with the triazolobenzodiazepine alprazolam was able to reliably reduce MDD scores compared to placebo, and one found that alprazolam treatment was as effective as tricyclic antidepressant treatment,Citation85 at least in cases of mild-to-moderate depression. However, these reviews disagreed about whether these depression-score reductions were mediated by changes in “core symptoms”, such as anhedonia. One study concluded that alprazolam was able to reduce anhedonia,Citation86 while the other concluded that most of alprazolam’s effects on depression scores were due to changes in psychomotor retardation, anxiety, and sleep disturbances, and not due to changes in anhedonia or anergia.Citation85 It is important to note that the doses used for the classical benzodiazepines in these studies were at the recommended doses for treatment of anxiety, whereas alprazolam doses were generally much higher. Additionally, recent clinical data have suggested that coadministration of the benzodiazepine-site PAM eszopiclone with SSRIs can lead to significantly greater treatment response, as well as faster onset of efficacy.Citation87,Citation88 Therefore, treatment with the benzodiazepine-site PAMs, such as alprazolam or eszopiclone as an adjuvant may be effective in treating at least some aspects of MDD, although it remains unclear whether alprazolam is effective in attenuating the core mood symptoms. Additionally, it is unclear whether classical benzodiazepines would be effective if used at higher doses. However, a recent nonclinical experiment demonstrated that diazepam, zolpidem, and low-dose alprazolam induced a depression-like phenotype in rodents, while a high dose of alprazolam induced an antidepressant-like response,Citation89 suggesting that alprazolam has specialized effects in its high-dose range that do not generalize to other benzodiazepine-site PAMs. Whether these effects are due to modulation of GABAA receptors or some other off-target effect is unclear.
Another line of inquiry may be drugs that act as agonists at the GABAA-receptor orthosteric binding site. Although preclinical data suggested that the combination of gaboxadol and escitalopram had synergistic antidepressant-like effects in nonclinical models,Citation90 in a clinical trial 5 and 10 mg gaboxadol did not add any benefit over escitalopram treatment alone.Citation91 Taken together with data on benzodiazepines, it does not seem that increasing activity at GABAA receptors uniformly improves depressive phenotypes. Instead, positive modulation of GABAA-receptor function only had positive effects in the case of some drugs, which may suggest a greater understanding of GABAA-receptor subtypes and their action in MDD is needed.
Systematic studies of the utility of other GABAergic treatments in MDD have been difficult to identify. However, there is evidence tying GABAergic treatments for epilepsy to mood dysregulation. For example, a review by Lambert and RobertsonCitation92 found that depressive symptoms are more common in epilepsy patients treated with barbiturates, an idea that is echoed in a report showing that phenobarbital treatment in epileptic children was associated with as much as a 40% prevalence of MDD and a 47% prevalence of suicidal ideation.Citation93 Additionally, a number of papers have suggested that the antiepileptic drug vigabatrin, which acts to increase GABA concentrations in the brain by irreversibly inhibiting the GABA-catabolizing enzyme GABA-T, increases the risk of depressive episodes. Estimates of the rate of this adverse event ranged from 4% in one study (compared to 2.6% in placebo controls)Citation94 to 12% in another (compared to 3% in placebo controls).Citation95 An anecdotal report found that major depressive episodes presented soon after either starting vigabatrin treatment or increasing dose in a small epilepsy patient group, and in seven of ten cases the patient had a prior history of MDD.Citation96 These data are further supported by nonclinical data showing that vigabatrin induced a depression-like phenotype in rodents.Citation89
Interestingly, a recent review of nonclinical data has suggested that pharmacological blockade or genetic knockout of GABAB receptors induces antidepressant-like behavioral effects in a variety of nonclinical rodent MDD models, including chronic mild stress, learned helplessness, and forced swim, while GABAB-receptor activation either blocks the effects of known antidepressants or induces a depressive-like phenotype.Citation97 Although there are no clinical investigations of GABAB-receptor antagonists in MDD that could be identified at this time, a clinical experiment demonstrated that GABAB-receptor activation using baclofen induced symptom exacerbation in the majority of a very small MDD patient sample that reversed upon baclofen withdrawal.Citation98 It should be noted that another GABAB-receptor agonist, GHB, which has been approved for use in narcolepsy, has been suggested for use as an antidepressant, primarily based on its beneficial effects on sleep quality,Citation99 although to our knowledge, there are no clinical data on GHB’s effects in MDD patients.
Taken together, these data suggest that increased activity at GABAergic receptors is beneficial in a few cases, eg, with alprazolam as a standalone treatment and eszopiclone as an adjuvant. However, increased neurotransmission at GABAA and GABAB receptors does not generally have positive effects on MDD symptoms, and in some cases can lead to an exacerbation of symptoms. In fact, it may be beneficial in some cases to reduce rather than increase GABA neurotransmission, particularly at GABAB receptors. These observations are not altogether supportive of the idea that reduced GABA neurotransmission drives MDD symptoms, but instead suggest that if GABA dysregulation is an etiological cause of MDD, then it is more complex than a simple reduction in function. In any case, our understanding of GABA’s role in MDD is still in its infancy, and more investigation is required to clarify whether GABAergic mechanisms can be effectively leveraged to treat MDD-related symptoms.
Serotonin–GABA interactions
It is important to note that although in many cases GABA receptors are sparsely expressed in subcortical brain structures, GABAergic interneurons are nearly ubiquitous, and tend to have broadly branching networks that powerfully modulate the activation state of many CNS circuits. Therefore, treatment strategies that feature direct modulation of GABAergic neurotransmission may open up for broad-ranging side effects that can include cognitive impairmentCitation100,Citation101 and abuse liability, as well as tolerance and withdrawal syndromes,Citation100 although it must be noted that some GABAergic treatments, eg, eszopiclone, are not associated with tolerance/withdrawal issues, and are considered relatively benign from a safety and tolerability perspective.
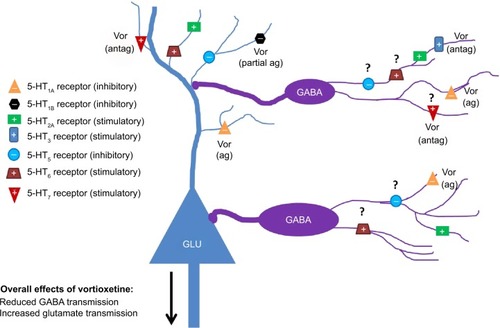
An alternative strategy may be to indirectly modulate GABA neurotransmission using targeted pharmacological actions on serotonergic receptors. Serotonin receptors are known to exist as heteroreceptors on GABAergic interneurons, where they can act to excite or inhibit interneuron function. Additionally, serotonin receptor-expression patterns are relatively circumscribed, and are often present in limbic brain regions that are relevant for the mood and cognitive symptoms associated with MDD. An in-depth discussion of the ways that serotonin signaling can modulate GABAergic neurotransmission is beyond the scope of this review. However, given the ascendant position serotonin modulation has in pharmacotherapeutic strategies for MDD, and the evidence that GABA pharmacology can influence mood and cognitive function, it seems important to highlight some of the mechanisms by which serotonin-receptor modulation can influence GABA neurotransmission. We begin with a review of the well-known serotonergic heteroreceptors that influence GABA neurotransmission, and this will be followed by a discussion of receptors for which there are fewer accumulated data. depicts the relationships between serotonergic heteroreceptors and limbic system GABA and glutamate cells.
Figure 2 Serotonergic influence on GABAergic neurotransmission in limbic system brain regions. Serotonergic heteroreceptors expressed on GABAergic interneurons and glutamatergic principal cells can modulate the excitatory state of neural networks associated with the control of cognitive function and mood. Vortioxetine may be an example of a drug that inhibits GABA neurotransmission via serotonergic mechanisms. Question marks denote receptors where expression on GABAergic interneurons has been indirectly suggested but no immunohistochemical verification exists for limbic brain regions.
Well-known relationships between serotonergic targets and GABA neurotransmission
5-HT1A receptors
As heteroreceptors, 5-HT1A receptors are G-protein-coupled receptors whose activation leads to hyperpolarization of neuronal membranes via the actions of inwardly rectifying potassium channels.Citation102 In rodents, 5-HT1A receptors are expressed in MDD-relevant regions, such as the medial frontal cortex, the anterior cingulate cortex, septum, and hippocampus, and are thought to be present on calbindin- and PV-IR GABAergic interneurons.Citation103 Therefore, treatments that increase activity at 5-HT1A heteroreceptors expressed on GABA cells should lead to a reduction in GABAergic tone, and a disinhibition of downstream circuits. Electrophysiological studies do lend some support to this idea. 5-HT1A-receptor activation causes an increase in cortical pyramidal neuron firing that is thought to be driven by reduced GABAergic inhibitory tone.Citation104–Citation106 However, it should be noted that 5-HT1A receptors are also thought to be expressed on pyramidal neurons, which may be responsible for the fact that in most pyramidal neurons recorded in one study, increased firing was followed by inhibition.Citation106
5-HT2A receptors
5-HT2A receptors are G-protein-coupled receptors that serve to depolarize neuronal membranes via the stimulation of Gq/11 and the resulting increases in intracellular inositol phosphate and Ca2+ concentrations.Citation107 This receptor is thought to be expressed as a postsynaptic receptor, and is strongly localized in MDD-relevant regions, including the frontal cortex, the medial septum, the hippocampus, and the amygdala complex.Citation108 Studies in rodents have found that 5-HT2A heteroreceptors are expressed on GABAergic interneurons, as well as glutamatergic principal cells in numerous brain regions.Citation107,Citation109,Citation110 The degree of expression of the 5-HT2A receptor on inhibitory and principal cells appears to vary by brain region. For example, in the rodent prelimbic cortex, approximately 50% of pyramidal cells express mRNA for the 5-HT2A receptor, while about 30% of GABA cells express the 5-HT2A receptor mRNA. In the infralimbic cortex, only 10% of pyramidal cells and 25% of GABA cells express 5-HT2A receptors.Citation109 However, in the medial septum, hippocampus, and amygdala, nearly all principal excitatory cells and the vast majority of GABAergic interneurons express this receptor.Citation107,Citation110 Therefore, 5-HT2A-receptor activation should have a stimulatory influence on GABAergic interneurons; however, its stimulatory effects on principal cells will again lead to complex actions on local circuits that will likely differ in each brain area.
In general, our understanding of the actions of 5-HT2A receptors in vivo is somewhat limited by the availability of centrally active, selective agonists. In vivo extracellular recordings of neuronal firing have found that activation of 5-HT2A/2C receptors using the nonselective agonist 2,5-dimethoxy-4-iodoamphetamine (DOI) both increased and decreased activity in subsets of normal spiking cells,Citation111,Citation112 which could conceivably include both principal excitatory cells, such as pyramidal neurons, and regular spiking interneurons, such as those expressing the Ca2+-binding proteins calbindin and calretinin. However, the overall effect on population spiking seems to differ based on the region from which the recordings were taken. Puig et alCitation111 found that DOI administration led to an overall 2.4-fold increase in spiking activity in deep layers of the medial frontal cortex, while recordings from the orbitofrontal cortex and anterior cingulate cortex showed that DOI reduced population activity.Citation112,Citation113 Moreover, given the multiplicity of 5-HT2A receptor-expressing GABAergic interneurons on principal cells, eg, in the amygdala and hippocampus,Citation107 it seems likely that the effects of pharmacological treatments that either activate or inhibit 5-HT2A receptors are overwhelmingly mediated by downstream effects of GABA neurotransmission. This may explain evidence that 5-HT2A-receptor antagonism using M100907 leads to seemingly paradoxical increases in excitatory postsynaptic currents and enhancements in hippocampal long-term potentiation (LTP).Citation114
5-HT3 receptors
The 5-HT3 receptor is unique among the 14 known serotonergic receptors, in that it is the only stimulatory ligand-gated ion channel. It is expressed in MDD-relevant brain regions, such as the frontal cortex, anterior cingulate cortex, hippocampus, and related cortical regions, such as the entorhinal and perirhinal cortices and the amygdala complex.Citation115 The 5-HT3 receptor is also seemingly unique in that its expression, at least in the rodent brain, is largely circumscribed to GABAergic interneurons,Citation116,Citation117 where it is thought to provide a serotonin-mediated fast excitatory drive. More specifically, cortical interneurons expressing 5-HT3 receptor mRNA are at their highest density in the shallow cortical layers, and are thought to express the calcium-binding proteins calbindin and calretinin, but not parvalbumin.Citation116,Citation117 Consistent with this idea, 5-HT3-receptor agonists suppress the firing of medial prefrontal cortical pyramidal neurons in rodents, while 5-HT3-receptor antagonists suppress the firing of GABAergic interneurons and concomitantly increase the firing rate of cortical pyramidal cells.Citation117–Citation119 Additionally, 5-HT3-receptor antagonists increase measures of synaptic potentiation, such as theta-burst LTP and drive increases in cortical theta oscillatory rhythms.Citation120
Less well-known relationships between serotonergic targets and GABA neurotransmission
5-HT4 receptors
5-HT4 receptors are G-protein-coupled receptors that are associated with Gs, and thus act to depolarize cellular membranes by stimulation of adenylyl cyclase and the resulting increase in cyclic adenosine monophosphate (cAMP) production.Citation121 Based on autoradiographic mapping, these receptors are thought to be expressed in limbic regions, such as the olfactory tubercle, islands of Calleja, septum, hippocampus, and amygdala;Citation122 however, at this time we have not been able to identify any studies that have investigated the cell types that express this receptor using histological techniques.
Based on evidence from electrophysiological recordings, it is likely that 5-HT4 receptors are expressed on pyramidal neurons in the CA1 region of the hippocampus, given that at least one group has found a 5-HT4 receptor-mediated depolarizing current in these cells.Citation121 However, evidence tying 5-HT4 receptors to GABAergic interneurons is relatively sparse. There is some electrophysiological and neurochemical evidence that stimulation of 5-HT4 receptors can have an effect on GABA-mediated neurotransmission; however, it is not clear that these effects are mediated via direct effects of 5-HT4 receptors on GABAergic cells. For example, Bianchi et alCitation123 found that 5-HT4-receptor stimulation using the selective agonist BIMU-8 in hippocampal slices from guinea pigs had no effect on GABA outflow under basal conditions, but during electrical stimulation low BIMU-8 concentrations elicited GABA release, while higher concentrations inhibited GABA release. These effects could be blocked by a selective 5-HT4-receptor antagonist, or by antagonists selective for muscarinic receptors, making it possible that these effects are mediated indirectly via cholinergic transmission rather than by direct effects on GABAergic interneurons. Similarly, Cai et alCitation124 found that GABAA receptor-mediated currents measured from cortical pyramidal neurons could be either increased or decreased by 5-HT4-receptor stimulation, depending on the activation state of protein kinase A. However, these data only demonstrate that 5-HT4 receptors can modulate GABAA receptor-mediated currents, and do not necessarily suggest that these effects are mediated by direct effects of 5-HT4 receptors on GABAergic cells. Moreover, without histological data on the presence or absence of 5-HT4 receptors on GABAergic interneurons, it is probably premature to draw conclusions on the nature of the relationship between 5-HT4 receptors and GABAergic neurotransmission.
5-HT5 receptors
Studies of the 5-HT5 receptor in stably transfected cell lines have suggested that this receptor is coupled to Gi/Go and is thus negatively coupled to adenylyl cyclase.Citation125 Additionally, there is some evidence suggesting that 5-HT5 receptors can be coupled to inwardly rectifying K+ channels in the rodent PFC.Citation126 Immunohistochemical evidence demonstrates that the 5-HT5 receptor is expressed throughout the CNS in rodents, with its most intense immunoreactivity being noted in the suprachiasmatic nucleus and hypothalamic regions.Citation127 In addition to these regions, 5-HT5 receptors were also observed at weak or moderately weak levels of immunoreactivity in cognition- and mood-relevant regions, such as the frontal cortex, anterior cingulate, and hippocampus.Citation127 Moreover, the evidence linking 5-HT5 receptors to GABAergic interneurons or principal excitatory cells is relatively sparse at this time. Oliver et alCitation127 observed relatively weak 5-HT5-receptor immunoreactivity in striatal medium spiny neurons, and thus the presence of 5-HT5 receptors on GABAergic neurons has been confirmed in at least one brain region. This group also observed 5-HT5-receptor immunoreactivity on principal cells in some regions, including hippocampal pyramidal neurons in regions CA1–3, as well as granule cells in the dentate gyrus. Finally, it is likely that 5-HT5 receptors are also expressed on cortical pyramidal neurons, given evidence of a 5-HT5-mediated inhibitory current in layer V cortical pyramidal neurons.Citation126 Again, based on this sparse evidence, we believe it is premature to make any firm conclusions on the relationship between 5-HT5 receptors and GABAergic neurotransmission at this time.
5-HT6 receptors
5-HT6 receptors are G-protein-coupled receptors that are positively linked to adenylyl cyclase activity when transiently expressed in cell lines via Gs.Citation128 Investigation of the anatomical pattern of 5-HT6-receptor expression found the highest expression in the striatum, olfactory tubercle, hippocampus, and frontal cortex, while more moderate expression was found in the thalamus and substantia nigra, among other regions.Citation128,Citation129
The expression pattern is relatively similar when investigated via in situ hybridizationCitation128 or immunohistochemical techniques,Citation129 which may suggest that 5-HT6 receptors tend to have a somatodendritic localization.
Once again, evidence tying 5-HT6 receptors to GABAergic neurotransmission is relatively sparse at this time, and theories about a connection between the two are largely driven by indirect evidence from electrophysiological or neurochemical studies. One notable electrophysiological study by West et alCitation130 found that despite being coupled to Gs, stimulation of 5-HT6 receptors using the 5-HT6-preferring agonist WAY-181187 attenuates theta-burst stimulation-induced LTP in hippocampal slice recordings. Additionally, West et al found that WAY-181187 increased the frequency of inhibitory postsynaptic currents (IPSCs) recorded from pyramidal neurons. Both of these effects were blocked by the selective 5-HT6-receptor antagonist SB-399885. Another studyCitation131 found that WAY-181187 significantly increased the concentration of extracellular GABA in the PFC, striatum, and dorsal hippocampus when evaluated in vivo, and further that this effect was blocked by the 5-HT6-receptor antagonist SB-217046. The authors also demonstrated that potassium-stimulated glutamate release in the slice was attenuated by WAY-181187 at 30 and 100 μM concentrations, but not at 10 μM. However, given that this agonist only has about a 60-fold selectivity for the 5-HT6 receptor over the 5-HT2C receptor (ie, 2 nM versus 120 nM, respectively), and is not active at the 10 μM concentration, it is not entirely clear that it is the 5-HT6-receptor mechanism that is driving this effect on glutamate release, particularly given that no attempt was made to antagonize this effect with SB-217046.
These data make it tempting to conclude that 5-HT6 receptors are expressed on GABAergic interneurons and act to increase their activity in such regions as the hippocampus. There is some evidence to support the idea of 5-HT6-receptor colocalization with GABAergic cells; however, it is relatively thin at this time. One study found that 5-HT6 receptors were expressed on nigrostriatal neurons that are known to coexpress GABA, dynorphin, and substance P.Citation129 In another paper, double immunofluorescence was used to demonstrate in an example cell that 5-HT6-IR processes were closely apposed to a GAD67-IR cell.Citation132 Finally, a study in postmortem human striatal tissue found that 5-HT6 immunoreactivity was present in PV-IR cells.Citation133
However, the most comprehensive anatomical study of 5-HT6 receptors to date found substantial heterogeneity in the types of cells that express 5-HT6 receptors in human limbic brain regions, such as the frontal cortex and hippocampus. Marazziti et alCitation134 demonstrated that the highest density of 5-HT6 receptor-IR cells in the frontal cortex was present in layer I, and that those cells were astrocytes rather than neurons. These authors also found that 5-HT6 receptor-IR cells were present in deeper cortical layers, and that those cells had a pyramidal morphology and were positive for the neuronal nuclear label NeuN. Finally, Marazziti et al showed that 5-HT6 receptor-IR cells in human hippocampal regions CA1–4 were pyramidal cells, and did not report colocalization with GABAergic cells in this region. Therefore, while it seems clear from the rodent electrophysiology and neurochemistry data that 5-HT6-receptor activation can modulate GABAergic neurotransmission, it is not clear that this modulation is due to direct effects of 5-HT6 receptors on GABAergic cells.
5-HT7 receptors
The 5-HT7 receptor is a relatively novel G-protein-coupled receptor that is expressed in several MDD-relevant brain regions, such as the frontal cortex, septum, thalamus, hippocampus, and amygdala.Citation135,Citation136 It is coupled to Gs, and thus 5-HT7-receptor stimulation can be expected to increase adenylyl cyclase activity and intracellular cAMP, leading to depolarization of neuronal membranes. The availability of data on the cellular localization of 5-HT7 heteroreceptors is still somewhat limited; however, at this time 5-HT7-receptor expression has been confirmed on some types of GABAergic neurons, eg, on cerebellar Purkinje cells,Citation137 and the presence of 5-HT7 receptors on GABAergic interneurons in other regions has been inferred based on electrophysiology data showing that 5-HT7-receptor stimulation increases the frequency of spontaneous IPSCs.Citation138 Therefore, as with the 5-HT2A and 5-HT3 receptors, stimulation of the 5-HT7 receptor is thought to have an excitatory effect on GABAergic neurotransmission.
However, 5-HT7 receptors are also thought to be expressed on pyramidal cells in the frontal cortex and hippocampus on the basis of immunohistochemicalCitation136 and electrophysiological evidence.Citation138–Citation140 Therefore, stimulation of 5-HT7 receptors is likely to have mixed effects on the overall excitatory state of the circuits in which it is present, although on average it seems to lead to an overall excitation of firing.Citation140 This idea is overall supported by observations that repeated administration of the 5-HT7 receptor-selective antagonist SB269970 reduces the frequency and amplitude of spontaneous excitatory postsynaptic potentials from cortical pyramidal neurons.Citation138
In summary, when the direct effects of these serotonergic heteroreceptors on GABAergic cells are considered, it appears that serotonin signaling has generally excitatory effects on GABAergic neurotransmission that are mediated through 5-HT2A, 5-HT3, and perhaps 5-HT7 receptors, although it should be noted that 5-HT1A receptors appear to be a 5-HT-mediated mechanism for GABA inhibition. The direct effects of 5-HT4–7 receptors on GABAergic interneurons are unclear at this time. Importantly, the overall effect of 5-HT stimulation on GABA neurotransmission in vivo will likely vary by region on the basis of which heteroreceptors are expressed locally.
Examples of serotonergic antidepressants modulating GABAergic neurotransmission
Fluoxetine
Fluoxetine is an SSRI that was approved in the US in the late 1980s, and has become a standard treatment for patients with MDD. Its action is characterized in vivo by a combination of its own inhibitory effects at the SERT (Dissociation constant [Ki] =0.9 nM)Citation141 and the SERT-inhibitory effects of its long-acting metabolite norfluoxetine (Ki =2.3 nM),Citation141 and thus fluoxetine is thought to bring about its antidepressant actions by elevating extracellular 5-HT concentrations. Based on the conclusion that serotonin heteroreceptors have a generally excitatory effect on GABAergic neurotransmission, it can be expected that the increases in 5-HT tone induced by fluoxetine treatment will lead to overall increases in GABAergic neurotransmission.
Although in general there is not a great deal of information available on the actions of serotonergic antidepressants on GABA neurotransmission, there is a fair amount of data available on fluoxetine’s effects. Studies of fluoxetine’s effects on interneuron firing using electrophysiological recordings in the slice suggest that bath application of fluoxetine in the range of 10–100 μM leads to significant increases in PFC fast-spiking (FS) interneuron-firing rates, curiously without significantly affecting pyramidal neuron firing.Citation142 A separate research group using slice electrophysiology demonstrated that application of fluoxetine at 10–30 μM concentrations led to significant increases in the frequency but not amplitude of spontaneous IPSCs.Citation143 In addition, recordings from brain slices taken from animals treated with a dose of 10 mg/kg/day fluoxetine for 21 days demonstrated that the intrinsic excitability of FS interneurons (measured as the number of spikes elicited by increasing current injections) was enhanced compared to FS cells recorded from vehicle-treated slices.Citation142 Finally, Gören et alCitation144 found that acute or repeated fluoxetine administration at 5 mg/kg/day significantly increased CSF GABA concentrations in rodents. Each of these observations suggests that fluoxetine administration can induce significant increases in GABA neurotransmission, consistent with the idea that serotonin neurotransmission has a generally excitatory action on GABA.
In addition to these observations, there are several studies using high concentrations of fluoxetine that may suggest it can potentiate GABA neurotransmission independently of its serotonergic mechanisms. For example, Robinson et alCitation145 used human cell lines expressing recombinant GABAA receptors to show that fluoxetine has a positive allosteric modulatory effect on GABAA-receptor responses in the range of 130 μM concentrations, while the active metabolite norfluoxetine had a similar effect in the range of 600 nM concentrations. This effect was found for GABA receptors expressing all α subunits except α5, and was later replicated in a separate set of experiments using a 300 μM fluoxetine concentration.Citation146 Furthermore, a point mutation in the α5 subunit conferred sensitivity to this allosteric modulatory effect, while a separate point mutation in the α1 subunit reduced the sensitivity of GABAA receptors to fluoxetine.Citation146 A separate group using electrophysiological recordings in cultured hippocampal neurons from rodents found that fluoxetine (at concentrations of 10–30 μM) was able to increase the frequency and amplitude of spontaneous IPSCs in a manner that was insensitive to ritanserin or tetrodotoxin, suggesting a postsynaptic action that is at least independent of 5-HT2-receptor actions.Citation147 Therefore, it is possible that fluoxetine has the ability to positively modulate GABA neurotransmission independently of serotonergic signaling. However, it should be pointed out that the clinical relevance of these observations can be questioned from the perspective that they represent very high biophase concentrations of fluoxetine.
Clinical observations of whole-brain exposure suggest that fluoxetine can reach concentrations in the tens of micromoles during treatment for MDD,Citation148 which by itself may suggest that allosteric modulatory effects beginning in the hundreds of micromoles are probably irrelevant in MDD patients. However, it should be noted that whole-brain exposure is not necessarily the best exposure measurement to predict a drug’s CNS actions, as it represents the free brain drug concentration plus drug that is bound to lipids and proteins, and is thus not free to interact with neurotransmitter receptors. Fortunately, for drugs like fluoxetine, the CSF concentration can be a good heuristic of the brain free concentration.Citation149 Measurements of CSF concentrations in humans after 6 weeks of clinically relevant dosing have found that fluoxetine concentrations are at approximately 25 nmol/L, while norfluoxetine concentrations are at about 17 nmol/L.Citation150 Based on this observation, concentrations of 10–30 μM fluoxetine in cultured neurons are probably also at an irrelevantly high concentration, given that cultured neurons are thought to be much more available for drug interactions compared to neurons in brain-slice preparations due to the relative absence of glial cells. Based on this line of evidence, it is possible, although unlikely, that fluoxetine has direct positive allosteric modulatory effects on GABA neurotransmission in the clinic.
It is important to note, however, that fluoxetine does not appear to have universally GABA neurotransmission-enhancing effects. For example, Méndez et alCitation143 demonstrated that 10–20 μM fluoxetine in hippocampal brain slices significantly decreased IPSC amplitudes, and further that this effect was likely due to a change in feed-forward inhibition originating from perisomatic FS interneurons. These authors went on to show that for chronic fluoxetine administration at 20 mg/kg/day, which is a dose that is well above the clinically relevant range,Citation80 the strength of the electrical stimulus required to elicit firing was significantly higher than in slices from saline-treated animals, and further that those IPSCs were smaller than in control slices. However, it is important to note that this group did not observe changes in basal firing frequency, resting membrane potentials, or membrane resistances. Another group used slice electrophysiological recordings from rats chronically treated with the more reasonable dose of 10 mg/kg/day to show that 5-HT2 receptor-mediated IPSCs desensitize faster than in control conditions,Citation151 and further that chronic fluoxetine treatment led to a significant decrease in the effects of 5-HT application on FS interneuron-firing rates.Citation142 Therefore, at the very least, long-term fluoxetine treatment can lead to a desensitization of 5-HT2 receptor-mediated effects on GABA neurotransmission, and may also decrease the excitability of FS interneurons in some hippocampal circuits.
Given that fluoxetine requires chronic administration in the clinic in order to effectively treat MDD, it is reasonable to assume that changes in GABA neurotransmission resulting from chronic fluoxetine treatment are more relevant to fluoxetine’s antidepressant efficacy. However, given that chronic fluoxetine use can increase intrinsic excitability in some interneuronsCitation142 and increase CSF GABA concentrations,Citation144 while at the same time reducing serotonin’s effect on phasic GABA activation,Citation142,Citation151 it is unclear whether fluoxetine’s GABA-enhancing effects are beneficial for mood. However, behavioral data from nonclinical model systems have suggested that pharmacological antagonism of GABAA receptors using bicuculline can partially block fluoxetine’s antidepressant-like effects,Citation152 and thus it is at least plausible that fluoxetine’s antidepressant effects are partially mediated by enhancing GABA neurotransmission.
Vortioxetine
Vortioxetine is a multimodal-acting antidepressant that was recently approved in North America and Europe for the treatment of MDD. Vortioxetine is an inhibitor at the SERT (Ki =1.6 nM in human receptors), an antagonist at 5-HT1D (Ki =54 nM), 5-HT3 (Ki =3.7 nM), and 5-HT7 receptors (Ki =19 nM), an agonist at 5-HT1A receptors (Ki =15 nM), and a partial agonist at 5-HT1B receptors (Ki =33 nM).Citation153,Citation154 Based on the earlier discussion, it is expected that vortioxetine’s direct pharmacological effects on GABAergic neurotransmission will be inhibitory overall, based on 5-HT1A-receptor activation, antagonism of 5-HT3, and perhaps also 5-HT7 receptors. Vortioxetine may have some indirect excitatory effects on GABA neurotransmission mediated via increased activation of 5-HT2A receptors due to 5-HT-reuptake inhibition. However, we have hypothesized that on average, vortioxetine will inhibit GABAergic neurotransmission.
Slice electrophysiological recordings have demonstrated that vortioxetine blocks 5-HT-induced increases in spontaneous inhibitory postsynaptic potentials recorded from hippocampal pyramidal neurons and increases hippocampal theta-burst LTP.Citation155 In vivo recordings of putative frontal cortical pyramidal cells also found that acute vortioxetine significantly increased firing rates.Citation156 In each case, the hypothesized mechanism involved 5-HT3-receptor antagonism. Additionally, in vivo electroencephalography has demonstrated that vortioxetine increases frontocortical theta and gamma power during active awake periods.Citation155,Citation157 By comparison, the SSRI escitalopram had no effects on 5-HT-induced spontaneous inhibitory postsynaptic potentials, theta-burst LTP, frontal cortex pyramidal firing, or theta/gamma oscillatory power.Citation155–Citation157 These data fit with the hypothesis that vortioxetine indirectly reduces GABAergic neurotransmission via its serotonergic pharmacological actions. However, more studies are required to further substantiate vortioxetine’s effects on GABA neurotransmission, to understand the mechanisms underlying these effects, and to demonstrate that vortioxetine’s effects on GABA neurotransmission translate into clinical MDD populations.
Importantly, there is a large set of accumulated clinical data demonstrating that vortioxetine is an effective antidepressant.Citation158 Therefore, despite the fact that vortioxetine and fluoxetine have apparently opposing effects on GABAergic neurotransmission, both are effective antidepressants. Moreover, this idea may further call into question the hypothesis that a simple reduction in GABA neurotransmission is at the etiological root of MDD.
Conclusion
In summary, there has been evidence of reduced CNS GABA concentrations in MDD going back to at least 1980, and more recent MRS data have generally supported this idea. However, it is not clear based on current clinical data whether these reductions are circumscribed to certain brain regions, whether the reduced GABA concentrations are from an intracellular pool that is used for neurotransmission, or whether the reduced GABA concentrations are a consistent biomarker for depression. Moreover, the MDD-related reductions in GABA are probably not related to impaired function in GABA synthesis via GAD, but instead it is more likely that these changes in GABA concentrations are related to pathology in calbindin-IR interneurons or in glia, although more data are required to confirm these ideas. Gene-expression data suggest that GABAA-receptor physiology may be altered in MDD, but a relative paucity of receptor-binding, protein-expression, and functional assay data has made it difficult to assess whether these changes have translated into altered receptor function, or what the consequences of these changes might be for GABA neurotransmission. There are GABA pharmacology data that could support the reduced GABA neurotransmission hypothesis in MDD. However, there are also data suggesting that increasing GABA neurotransmission actually induces negative mood (eg, mood dysfunction induced by vigabatrin, barbiturates, or baclofen). Nonclinical data have suggested that reducing some aspects of GABA neurotransmission is actually beneficial for mood, eg, in the case of direct GABAB-receptor antagonists. Finally, two serotonergic antidepressants – fluoxetine and vortioxetine – have apparently opposing effects on GABA neurotransmission, despite both being effective antidepressants. Moreover, it may be important to consider the idea that treatments capable of reducing some aspects of GABA neurotransmission may be more in line with theories claiming that synaptic potentiation is important for the fast onset of antidepressant efficacy seen in ketamine.Citation7 Taken together, these data suggest that the notion that MDD is related to simple reductions in GABAergic neurotransmission must be reevaluated and discarded in favor of a more nuanced and complex model.
Disclosure
Alan L Pehrson and Connie Sanchez are employees of Lundbeck Research USA. The authors report no other conflicts of interest in this work.
References
- World Health OrganizationDepression2012 Available from: http://www.who.int/mediacentre/factsheets/fs369/enAccessed September 11, 2014
- McIntyreRSChaDSSoczynskaJKCognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventionsDepress Anxiety201330651552723468126
- BirnbaumHGKesslerRCKelleyDBen-HamadiRJoishVNGreenbergPEEmployer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performanceDepress Anxiety2010271788919569060
- JaegerJBernsSUzelacSDavis-ConwaySNeurocognitive deficits and disability in major depressive disorderPsychiatry Res20061451394817045658
- CharneyDSMonoamine dysfunction and the pathophysiology and treatment of depressionJ Clin Psychiatry199859Suppl 1411149818625
- CarotenutoMEspositoMParisiLDepressive symptoms and childhood sleep apnea syndromeNeuropsychiatric Dis Treat20128369373
- ZarateCDumanRSLiuGSartoriSQuirozJMurckHNew paradigms for treatment-resistant depressionAnn N Y Acad Sci20131292213123876043
- MartinDLRimvallKRegulation of gamma-aminobutyric acid synthesis in the brainJ Neurochem19936023954078419527
- SoghomonianJJMartinDLTwo isoforms of glutamate decarboxylase: why?Trends Pharmacol Sci199819125005059871412
- PinalCSTobinAJUniqueness and redundancy in GABA productionPerspect Dev Neurobiol199852–31091189777629
- MartinDLBarkeKEAre GAD65 and GAD67 associated with specific pools of GABA in brain?Perspect Dev Neurobiol199852–31191299777630
- RowleyNMMadsenKKSchousboeAWhiteHSGlutamate and GABA synthesis, release, transport and metabolism as targets for seizure controlNeurochem Int201261454655822365921
- KogaMSerritellaAVMessmerMMGlutathione is a physiologic reservoir of neuronal glutamateBiochem Biophys Res Commun2011409459660221539809
- BeharKLRothmanDLIn vivo nuclear magnetic resonance studies of glutamate-gamma-aminobutyric acid-glutamine cycling in rodent and human cortex: the central role of glutamineJ Nutr20011319 Suppl2498S2504S discussion 2523S–2524S11533301
- RaeCHareNBubbWAInhibition of glutamine transport depletes glutamate and GABA neurotransmitter pools: further evidence for metabolic compartmentationJ Neurochem200385250351412675927
- GoldBIBowersMBJrRothRHSweeneyDWGABA levels in CSF of patients with psychiatric disordersAm J Psychiatry198013733623647356067
- KugayaASanacoraGVerhoeffNPCerebral benzodiazepine receptors in depressed patients measured with [123I]iomazenil SPECTBiol Psychiatry200354879279914550678
- PriceRBShunguDCMaoXAmino acid neurotransmitters assessed by proton magnetic resonance spectroscopy: relationship to treatment resistance in major depressive disorderBiol Psychiatry200965979280019058788
- SanacoraGGueorguievaREppersonCNSubtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depressionArch Gen Psychiatry200461770571315237082
- SanacoraGMasonGFRothmanDLReduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopyArch Gen Psychiatry199956111043104710565505
- HaslerGvan der VeenJWTumonisTMeyersNShenJDrevetsWCReduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopyArch Gen Psychiatry200764219320017283286
- SanacoraGMasonGFRothmanDLKrystalJHIncreased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitorsAm J Psychiatry2002159466366511925309
- SanacoraGMasonGFRothmanDLIncreased cortical GABA concentrations in depressed patients receiving ECTAm J Psychiatry2003160357757912611844
- HaslerGNeumeisterAvan der VeenJWNormal prefrontal gamma-aminobutyric acid levels in remitted depressed subjects determined by proton magnetic resonance spectroscopyBiol Psychiatry2005581296997316043137
- ShawABrealyJRichardsonHMarked reductions in visual evoked responses but not gamma-aminobutyric acid concentrations or gamma-band measures in remitted depressionBiol Psychiatry201373769169823200528
- SanacoraGFentonLRFasulaMKCortical gamma-aminobutyric acid concentrations in depressed patients receiving cognitive behavioral therapyBiol Psychiatry200659328428616139814
- BhagwagarZWylezinskaMJezzardPReduction in occipital cortex gamma-aminobutyric acid concentrations in medication-free recovered unipolar depressed and bipolar subjectsBiol Psychiatry200761680681217210135
- BhagwagarZWylezinskaMJezzardPLow GABA concentrations in occipital cortex and anterior cingulate cortex in medication-free, recovered depressed patientsInt J Neuropsychopharmacol200811225526017625025
- Herrera-GuzmánIGudayol-FerréEHerrera-GuzmánDGuàrdia-OlmosJHinojosa-CalvoEHerrera-AbarcaJEEffects of selective serotonin reuptake and dual serotonergic-noradrenergic reuptake treatments on memory and mental processing speed in patients with major depressive disorderJ Psychiatr Res200943985586319128810
- KarolewiczBMaciagDO’DwyerGStockmeierCAFeyissaAMRajkowskaGReduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depressionInt J Neuropsychopharmacol201013441142020236554
- FatemiSHStaryJMEarleJAAraghi-NiknamMEaganEGABAergic dysfunction in schizophrenia and mood disorders as reflected by decreased levels of glutamic acid decarboxylase 65 and 67 kDa and Reelin proteins in cerebellumSchizophr Res2005722–310912215560956
- GuidottiAAutaJDavisJMDecrease in reelin and glutamic acid decarboxylase67 (GAD67) expression in schizophrenia and bipolar disorder: a postmortem brain studyArch Gen Psychiatry200057111061106911074872
- Gilabert-JuanJVareaEGuiradoRBlasco-IbáñezJMCrespoCNácherJAlterations in the expression of PSA-NCAM and synaptic proteins in the dorsolateral prefrontal cortex of psychiatric disorder patientsNeurosci Lett201253019710223022470
- SibilleEMorrisHMKotaRSLewisDAGABA-related transcripts in the dorsolateral prefrontal cortex in mood disordersInt J Neuropsychopharmacol201114672173421226980
- BielauHSteinerJMawrinCDysregulation of GABAergic neurotransmission in mood disorders: a postmortem studyAnn N Y Acad Sci2007109615716917405927
- GosTGüntherKBielauHSuicide and depression in the quantitative analysis of glutamic acid decarboxylase-immunoreactive neuropilJ Affect Disord20091131–2455518538859
- GosTSteinerJBielauHDifferences between unipolar and bipolar I depression in the quantitative analysis of glutamic acid decarboxylase-immunoreactive neuropilEur Arch Psychiatry Clin Neurosci2012262864765522526728
- CheethamSCCromptonMRKatonaCLParkerSJHortonRWBrain GABAA/benzodiazepine binding sites and glutamic acid decarboxylase activity in depressed suicide victimsBrain Res198846011141232851368
- LundJSLewisDALocal circuit neurons of developing and mature macaque prefrontal cortex: Golgi and immunocytochemical characteristicsJ Comp Neurol199332822823127678612
- RajkowskaGO’DwyerGTelekiZStockmeierCAMiguel-HidalgoJJGABAergic neurons immunoreactive for calcium binding proteins are reduced in the prefrontal cortex in major depressionNeuropsychopharmacology200732247148217063153
- MaciagDHughesJO’DwyerGReduced density of calbindin immunoreactive GABAergic neurons in the occipital cortex in major depression: relevance to neuroimaging studiesBiol Psychiatry201067546547020004363
- BeasleyCLZhangZJPattenIReynoldsGPSelective deficits in prefrontal cortical GABAergic neurons in schizophrenia defined by the presence of calcium-binding proteinsBiol Psychiatry200252770871512372661
- ReynoldsGPBeasleyCLZhangZJUnderstanding the neurotransmitter pathology of schizophrenia: selective deficits of subtypes of cortical GABAergic neuronsJ Neural Transm20021095–688188912111475
- GuillouxJPDouillard-GuillouxGKotaRMolecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depressionMol Psychiatry201217111130114221912391
- TrippAKotaRSLewisDASibilleEReduced somatostatin in subgenual anterior cingulate cortex in major depressionNeurobiol Dis201142111612421232602
- RajkowskaGMiguel-HidalgoJJWeiJMorphometric evidence for neuronal and glial prefrontal cell pathology in major depressionBiol Psychiatry19994591085109810331101
- RajkowskaGStockmeierCAAstrocyte pathology in major depressive disorder: insights from human postmortem brain tissueCurr Drug Targets201314111225123623469922
- SanacoraGBanasrMFrom pathophysiology to novel antidepressant drugs: glial contributions to the pathology and treatment of mood disordersBiol Psychiatry201373121172117923726152
- PaulsenREFonnumFRole of glial cells for the basal and Ca2+-dependent K+-evoked release of transmitter amino acids investigated by microdialysisJ Neurochem1989526182318292566651
- YükselCÖngürDMagnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disordersBiol Psychiatry201068978579420728076
- LiangSLCarlsonGCCoulterDADynamic regulation of synaptic GABA release by the glutamate-glutamine cycle in hippocampal area CA1J Neurosci200626338537854816914680
- LevinsonAJFitzgeraldPBFavalliGBlumbergerDMDaigleMDaskalakisZJEvidence of cortical inhibitory deficits in major depressive disorderBiol Psychiatry201067545846419922906
- PaulusWClassenJCohenLGState of the art: pharmacologic effects on cortical excitability measures tested by transcranial magnetic stimulationBrain Stimul20081315116320633382
- ChoudaryPVMolnarMEvansSJAltered cortical glutamatergic and GABAergic signal transmission with glial involvement in depressionProc Natl Acad Sci U S A200510243156531565816230605
- SequeiraAMamdaniFErnstCGlobal brain gene expression analysis links glutamatergic and GABAergic alterations to suicide and major depressionPloS One200948e658519668376
- FatemiSHFolsomTDRooneyRJThurasPDExpression of GABAA α2-, β1- and ε-receptors are altered significantly in the lateral cerebellum of subjects with schizophrenia, major depression and bipolar disorderTransl Psychiatry20133e30324022508
- KlumpersUMVeltmanDJDrentMLReduced parahippocampal and lateral temporal GABAA-[11C]flumazenil binding in major depression: preliminary resultsEur J Nucl Med Mol Imaging201037356557419890631
- ZhuHKarolewiczBNailEStockmeierCASzebeniKOrdwayGANormal [3H]flunitrazepam binding to GABAA receptors in the locus coeruleus in major depression and suicideBrain Res20061125113814617118347
- StocksGMCheethamSCCromptonMRKatonaCLHortonRWBenzodiazepine binding sites in amygdala and hippocampus of depressed suicide victimsJ Affect Disord199018111152153156
- FatemiSHFolsomTDThurasPDDeficits in GABA(B) receptor system in schizophrenia and mood disorders: a postmortem studySchizophr Res20111281–3374321303731
- ArranzBCowburnRErikssonAVestlingMMarcussonJGamma-aminobutyric acid-B (GABAB) binding sites in postmortem suicide brainsNeuropsychobiology1992261–233361335560
- CrossJACheethamSCCromptonMRKatonaCLHortonRWBrain GABAB binding sites in depressed suicide victimsPsychiatry Res19882621191292853398
- SmithSSShenHGongQHZhouXNeurosteroid regulation of GABA(A) receptors: focus on the α4 and δ subunitsPharmacol Ther20071161587617512983
- SchmidtPJNiemanLKDanaceauMAAdamsLFRubinowDRDifferential behavioral effects of gonadal steroids in women with and in those without premenstrual syndromeN Engl J Med199833842092169435325
- SmithMJAdamsLFSchmidtPJRubinowDRWassermannEMAbnormal luteal phase excitability of the motor cortex in women with premenstrual syndromeBiol Psychiatry200354775776214512217
- MajewskaMDHarrisonNLSchwartzRDBarkerJLPaulSMSteroid hormone metabolites are barbiturate-like modulators of the GABA receptorScience19862324753100410072422758
- CarboniEWielandSLanNCGeeKWAnxiolytic properties of endogenously occurring pregnanediols in two rodent models of anxietyPsychopharmacology199612621731788856837
- DevaudLLPurdyRHMorrowALThe neurosteroid, 3α-hydroxy-5α-pregnan-20-one, protects against bicuculline-induced seizures during ethanol withdrawal in ratsAlcohol Clin Exp Res19951923503557625568
- ShenHGongQHAokiCReversal of neurosteroid effects at α4β2δ GABAA receptors triggers anxiety at pubertyNat Neurosci200710446947717351635
- SmithSSRudermanYFryeCHomanicsGYuanMSteroid withdrawal in the mouse results in anxiogenic effects of 3α,5β-THP: a possible model of premenstrual dysphoric disorderPsychopharmacology2006186332333316193334
- WisdenWLaurieDJMonyerHSeeburgPHThe distribution of 13 GABAA receptor subunit mRNAs in the rat brain. I. Telencephalon, diencephalon, mesencephalonJ Neurosci1992123104010621312131
- GulinelloMGongQHLiXSmithSSShort-term exposure to a neuroactive steroid increases α4 GABA(A) receptor subunit levels in association with increased anxiety in the female ratBrain Res20019101–2556611489254
- Sundstrom-PoromaaISmithDHGongQHHormonally regulated α(4)β(2)δ GABA(A) receptors are a target for alcoholNat Neurosci20025872172212118257
- SmithSSGongQHNeurosteroid administration and withdrawal alter GABAA receptor kinetics in CA1 hippocampus of female ratsJ Physiol2005564Pt 242143615705652
- SmithSSGongQHLiXWithdrawal from 3α-OH-5α-pregnan-20-one using a pseudopregnancy model alters the kinetics of hippocampal GABAA-gated current and increases the GABAA receptor α4 subunit in association with increased anxietyJ Neurosci19981814527552849651210
- MaguireJLStellBMRafizadehMModyIOvarian cycle-linked changes in GABA(A) receptors mediating tonic inhibition alter seizure susceptibility and anxietyNat Neurosci20058679780415895085
- EppersonCNHagaKMasonGFCortical gamma-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder: a proton magnetic resonance spectroscopy studyArch Gen Psychiatry200259985185812215085
- UzunovDPCooperTBCostaEGuidottiAFluoxetine-elicited changes in brain neurosteroid content measured by negative ion mass fragmentographyProc Natl Acad Sci U S A1996932212599126048901628
- MatsumotoKUzunovaVPinnaGPermissive role of brain allopregnanolone content in the regulation of pentobarbital-induced righting reflex lossNeuropharmacology199938795596310428414
- PehrsonALLeiserSCGulinelloMTreatment of cognitive dysfunction in major depressive disorder – a review of the preclinical evidence for efficacy of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors and the multimodal-acting antidepressant vortioxetineEur J Pharmacol Epub201485
- MeyerJHWilsonAASagratiSSerotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography studyAm J Psychiatry2004161582683515121647
- UzunovaVShelineYDavisJMIncrease in the cerebrospinal fluid content of neurosteroids in patients with unipolar major depression who are receiving fluoxetine or fluvoxamineProc Natl Acad Sci U S A1998956323932449501247
- RomeoEStröhleASpallettaGEffects of antidepressant treatment on neuroactive steroids in major depressionAm J Psychiatry199815579109139659856
- SchuleCBaghaiTCEserDMirtazapine monotherapy versus combination therapy with mirtazapine and aripiprazole in depressed patients without psychotic features: a 4-week open-label parallel-group studyWorld J Biol Psychiatry20078211212217455104
- BirkenhägerTKMolemanPNolenWABenzodiazepines for depression? A review of the literatureInt Clin Psychopharmacol19951031811958675972
- PettyFTrivediMHFultonMRushAJBenzodiazepines as antidepressants: does GABA play a role in depression?Biol Psychiatry19953895785918573660
- FavaMMcCallWVKrystalAEszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorderBiol Psychiatry200659111052106016581036
- FavaMSchaeferKHuangHA post hoc analysis of the effect of nightly administration of eszopiclone and a selective serotonin reuptake inhibitor in patients with insomnia and anxious depressionJ Clin Psychiatry201172447347921208574
- El ZahafNASalem ElhwuegiAThe effect of GABAmimetics on the duration of immobility in the forced swim test in albino miceLibyan J Med201492348024560379
- ChristensenTBétryCMnie-FilaliOSynergistic antidepressant-like action of gaboxadol and escitalopramEur Neuropsychopharmacol2012221075176022406239
- KasperSEbertBLarsenKTonnoirBCombining escitalopram with gaboxadol provides no additional benefit in the treatment of patients with severe major depressive disorderInt J Neuropsychopharmacol201215671572522008735
- LambertMVRobertsonMMDepression in epilepsy: etiology, phenomenology, and treatmentEpilepsia199940Suppl 10S21S4710609603
- BrentDACrumrinePKVarmaRRAllanMAllmanCPhenobarbital treatment and major depressive disorder in children with epilepsyPediatrics19878069099173684404
- MumfordJPDamMMeta-analysis of European placebo controlled studies of vigabatrin in drug resistant epilepsyBr J Clin Pharmacol198927Suppl 1101S107S2667602
- LevinsonDFDevinskyOPsychiatric adverse events during vigabatrin therapyNeurology19995371503151110534259
- RingHACrellinRKirkerSReynoldsEHVigabatrin and depressionJ Neurol Neurosurg Psychiatry19935689259288350115
- CryanJFSlatteryDAGABAB receptors and depression. Current statusAdv Pharmacol20105842745120655491
- PostRMKetterTAJoffeRTKramlingerKLLack of beneficial effects of l-baclofen in affective disorderInt Clin Psychopharmacol1991641972071816278
- MamelakMNarcolepsy and depression and the neurobiology of gammahydroxybutyrateProg Neurobiol200989219321919654034
- ChouinardGIssues in the clinical use of benzodiazepines: potency, withdrawal, and reboundJ Clin Psychiatry200465Suppl 571215078112
- PietrzakRHScottJCHarelBTLimYYSnyderPJMaruffPA process-based approach to characterizing the effect of acute alprazolam challenge on visual paired associate learning and memory in healthy older adultsHum Psychopharmacol201227654955823027677
- LüscherCJanLYStoffelMMalenkaRCNicollRAG protein-coupled inwardly rectifying K+ channels (GIRKs) mediate postsynaptic but not presynaptic transmitter actions in hippocampal neuronsNeuron19971936876959331358
- AznarSQianZShahRRahbekBKnudsenGMThe 5-HT1A serotonin receptor is located on calbindin- and parvalbumin-containing neurons in the rat brainBrain Res20039591586712480158
- LevkovitzYSegalMSerotonin 5-HT1A receptors modulate hippocampal reactivity to afferent stimulationJ Neurosci19971714559155989204940
- Lladó-PelfortLAssiéMBNewman-TancrediAArtigasFCeladaPIn vivo electrophysiological and neurochemical effects of the selective 5-HT1A receptor agonist, F13640, at pre- and postsynaptic 5-HT1A receptors in the ratPsychopharmacology2012221226127222147258
- Lladó-PelfortLSantanaNGhisiVArtigasFCeladaP5-HT1A receptor agonists enhance pyramidal cell firing in prefrontal cortex through a preferential action on GABA interneuronsCereb Cortex20122271487149721893679
- BombardiCDi GiovanniGFunctional anatomy of 5-HT2A receptors in the amygdala and hippocampal complex: relevance to memory functionsExp Brain Res2013230442743923591691
- López-GiménezJFVilaróMTPalaciosJMMengodGMapping of 5-HT2A receptors and their mRNA in monkey brain: [3H] MDL100,907 autoradiography and in situ hybridization studiesJ Comp Neurol2001429457158911135236
- CeladaPPuigMVArtigasFSerotonin modulation of cortical neurons and networksFront Integr Neurosci201372523626526
- LüttgenMOve OgrenSMeisterBChemical identity of 5-HT2A receptor immunoreactive neurons of the rat septal complex and dorsal hippocampusBrain Res200410101–215616515126129
- PuigMVCeladaPDiaz-MataixLArtigasFIn vivo modulation of the activity of pyramidal neurons in the rat medial prefrontal cortex by 5-HT2A receptors: relationship to thalamocortical afferentsCereb Cortex200313887088212853374
- WoodJKimYMoghaddamBDisruption of prefrontal cortex large scale neuronal activity by different classes of psychotomimetic drugsJ Neurosci20123293022303122378875
- AshbyCRJrJiangLHKasserRJWangRYElectrophysiological characterization of 5-hydroxytryptamine2 receptors in the rat medial prefrontal cortexJ Pharmacol Exp Ther199025211711782137174
- WangRYArvanovVLM100907, a highly selective 5-HT2A receptor antagonist and a potential atypical antipsychotic drug, facilitates induction of long-term potentiation in area CA1 of the rat hippocampal sliceBrain Res19987791–23093139473706
- BloomFEMoralesMThe central 5-HT3 receptor in CNS disordersNeurochem Res19982356536599566603
- MoralesMBloomFEThe 5-HT3 receptor is present in different subpopulations of GABAergic neurons in the rat telencephalonJ Neurosci1997179315731679096150
- PuigMVSantanaNCeladaPMengodGArtigasFIn vivo excitation of GABA interneurons in the medial prefrontal cortex through 5-HT3 receptorsCereb Cortex200414121365137515166106
- AshbyCRJrMinabeYEdwardsEWangRY5-HT3-like receptors in the rat medial prefrontal cortex: an electrophysiological studyBrain Res199155021811911679370
- ReznicJStaubliUEffects of 5-HT3 receptor antagonism on hippocampal cellular activity in the freely moving ratJ Neurophysiol19977715175219120594
- StäubliUXuFBEffects of 5-HT3 receptor antagonism on hippocampal theta rhythm, memory, and LTP induction in the freely moving ratJ Neurosci1995153 Pt 2244524527891179
- ChapinEMHaj-DahmaneSTorresGAndradeRThe 5-HT(4) receptor-induced depolarization in rat hippocampal neurons is mediated by cAMP but is independent of I(h)Neurosci Lett200232411411983280
- WaeberCSebbenMNieoullonABockaertJDumuisARegional distribution and ontogeny of 5-HT4 binding sites in rodent brainNeuropharmacology1994333–45275417984292
- BianchiCRodiDMarinoSBeaniLSiniscalchiADual effects of 5-HT4 receptor activation on GABA release from guinea pig hippocampal slicesNeuroreport200213172177218012488792
- CaiXFlores-HernandezJFengJYanZActivity-dependent bidirectional regulation of GABA(A) receptor channels by the 5-HT(4) receptor-mediated signalling in rat prefrontal cortical pyramidal neuronsJ Physiol2002540Pt 374375911986365
- FranckenBJJurzakMVanhauweJFLuytenWHLeysenJEThe human 5-HT5A receptor couples to Gi/Go proteins and inhibits adenylate cyclase in HEK 293 cellsEur J Pharmacol19983612–32993099865521
- GoodfellowNMBaileyCDLambeEKThe native serotonin 5-HT(5A) receptor: electrophysiological characterization in rodent cortex and 5-HT(1A)-mediated compensatory plasticity in the knockout mouseJ Neurosci201232175804580922539842
- OliverKRKinseyAMWainwrightASirinathsinghjiDJLocalization of 5-HT(5A) receptor-like immunoreactivity in the rat brainBrain Res20008671–213114210837806
- RuatMTraiffortEArrangJMA novel rat serotonin (5-HT6) receptor: molecular cloning, localization and stimulation of cAMP accumulationBiochem Biophys Res Commun199319312682768389146
- GerardCMartresMPLefevreKImmuno-localization of serotonin 5-HT6 receptor-like material in the rat central nervous systemBrain Res19977461–22072199037500
- WestPJMarcyVRMarinoMJSchaffhauserHActivation of the 5-HT(6) receptor attenuates long-term potentiation and facilitates GABAergic neurotransmission in rat hippocampusNeuroscience2009164269270119660530
- SchechterLELinQSmithDLNeuropharmacological profile of novel and selective 5-HT6 receptor agonists: WAY-181187 and WAY-208466Neuropsychopharmacology20083361323133517625499
- WoolleyMLMarsdenCAFoneKC5-HT6 receptorsCurr Drug Targets CNS Neurol Disord200431597914965245
- MarazzitiDBaroniSPironeADistribution of serotonin receptor of type 6 (5-HT(6)) in human brain post-mortem. A pharmacology, autoradiography and immunohistochemistry studyNeurochem Res201237592092722278721
- MarazzitiDBaroniSPironeASerotonin receptor of type 6 (5-HT6) in human prefrontal cortex and hippocampus post-mortem: an immunohistochemical and immunofluorescence studyNeurochem Int201362218218823219521
- HedlundPBSutcliffeJGFunctional, molecular and pharmacological advances in 5-HT7 receptor researchTrends Pharmacol Sci200425948148615559250
- NeumaierJFSextonTJYrachetaJDiazAMBrownfieldMLocalization of 5-HT(7) receptors in rat brain by immunocytochemistry, in situ hybridization, and agonist stimulated cFos expressionJ Chem Neuroanat2001211637311173221
- GeurtsFJDe SchutterETimmermansJPLocalization of 5-HT2A, 5-HT3, 5-HT5A and 5-HT7 receptor-like immunoreactivity in the rat cerebellumJ Chem Neuroanat2002241657412084412
- TokarskiKKusekMHessG5-HT7 receptors modulate GABAergic transmission in rat hippocampal CA1 areaJ Physiol Pharmacol201162553554022204801
- BaconWLBeckSG5-Hydroxytryptamine(7) receptor activation decreases slow afterhyperpolarization amplitude in CA3 hippocampal pyramidal cellsJ Pharmacol Exp Ther2000294267267910900247
- FanLLZhangQJLiuJIn vivo effect of 5-HT(7) receptor agonist on pyramidal neurons in medial frontal cortex of normal and 6-hydroxydopamine-lesioned rats: an electrophysiological studyNeuroscience201119032833821684321
- OwensMJMorganWNPlottSJNemeroffCBNeurotransmitter receptor and transporter binding profile of antidepressants and their metabolitesJ Pharmacol Exp Ther19972833130513229400006
- ZhongPYanZDifferential regulation of the excitability of prefrontal cortical fast-spiking interneurons and pyramidal neurons by serotonin and fluoxetinePloS One201162e1697021383986
- MéndezPPazientiASzabóGBacciADirect alteration of a specific inhibitory circuit of the hippocampus by antidepressantsJ Neurosci20123247166161662823175817
- GörenMZKüçükibrahimogluEBerkmanKTerziogluBFluoxetine partly exerts its actions through GABA: a neurochemical evidenceNeurochem Res20073291559156517486443
- RobinsonRTDraftsBCFisherJLFluoxetine increases GABA(A) receptor activity through a novel modulatory siteJ Pharmacol Exp Ther2003304397898412604672
- DerryJMPaulsenIMDaviesMDunnSMA single point mutation of the GABA(A) receptor α5-subunit confers fluoxetine sensitivityNeuropharmacology200752249750517045313
- YeZYZhouKQXuTLZhouJNFluoxetine potentiates GABAergic IPSCs in rat hippocampal neuronsNeurosci Lett20084421242918606211
- HenryMESchmidtMEHennenJA comparison of brain and serum pharmacokinetics of R-fluoxetine and racemic fluoxetine: a 19-F MRS studyNeuropsychopharmacology20053081576158315886723
- LiuXSmithBJChenCEvaluation of cerebrospinal fluid concentration and plasma free concentration as a surrogate measurement for brain free concentrationDrug Metab Dispos20063491443144716760229
- MårtenssonBNybergSToressonGBrodinEBertilssonLFluoxetine treatment of depression. Clinical effects, drug concentrations and monoamine metabolites and N-terminally extended substance P in cerebrospinal fluidActa Psychiatr Scand19897965865962475012
- ZhongPYanZChronic antidepressant treatment alters serotonergic regulation of GABA transmission in prefrontal cortical pyramidal neuronsNeuroscience20041291657315489029
- KhistiRTChopdeCTJainSPAntidepressant-like effect of the neurosteroid 3α-hydroxy-5α-pregnan-20-one in mice forced swim testPharmacol Biochem Behav200067113714311113493
- PehrsonALSanchezCSerotonergic modulation of glutamate neurotransmission as a strategy for treating depression and cognitive dysfunctionCNS Spectr201419212113323903233
- WestrichLPehrsonAZhongHIn vitro and in vivo effects of the multimodal antidepressant vortioxetine (Lu AA21004) at human and rat targetsInt J Psychiatry Clin Pract201216Suppl 147
- DaleEZhangHLeiserSCVortioxetine disinhibits pyramidal cell function and enhances synaptic plasticity in the rat hippocampusJ Psychopharmacol2014281089190225122043
- RigaMSCeladaPSanchezCArtigasFRole of 5-HT3 receptors in the mechanism of action of the investigational antidepressant vortioxetineEur Neuropsychopharmacol201323Suppl 2S393S394
- LeiserSCPehrsonALRobichaudPJSanchezCThe multimodal antidepressant vortioxetine increases frontal cortical oscillations unlike escitalopram and duloxetine – a quantitative electroencephalographic study in the ratBr J Pharmacol Epub2014521
- AlvarezEPerezVArtigasFPharmacology and clinical potential of vortioxetine in the treatment of major depressive disorderNeuropsychiatric Dis Treat20141012971307
