Abstract
Background
Distal and lateral onychomycoses are the most frequent forms of onychomycosis, causing subungual hyperkeratosis that usually limits local penetration of antimycotic drugs. Tazarotene exerts anti-inflammatory and immune-modulating activities toward both infective agents and damaged keratinocytes. Given the well-documented efficacy of tazarotene on hyperkeratotic nail psoriasis, we investigated its therapeutic use in onychomycosis.
Patients and methods
We designed a preliminary open clinical trial in patients affected by distal and lateral subungual onychomycosis of the toenails and verified the fungistatic activity of tazarotene in vitro. Fifteen patients were treated with topical tazarotene 0.1% gel once per day for 12 weeks. Mycological cultures and potassium hydroxide stains of nail samples were performed at the beginning and at the end of the study. Treatment was considered effective when clinical healing and negative mycological culture were obtained. Onycholysis, nail bed discoloration, and subungual hyperkeratosis were measured using standardized methodologies and analyzed by means of Mann–Whitney test and analysis of variance. Fungistatic activity of tazarotene was evaluated by disk diffusion assay.
Results
Six patients (40%) reached a mycological cure on target nail samples already after 4 weeks of treatment. Complete clinical healing and negative cultures were reached in all patients at week 12, with a significant improvement of all clinical parameters of the infected nails. Disk diffusion assay after 48 hours of incubation with tazarotene solution showed a central area of inhibition in all examined fungal cultures.
Conclusion
Our results documented a good clinical outcome using topical tazarotene 0.1% gel in distal and lateral subungual onychomycosis and its fungistatic activity of tazarotene in vitro. The majority of patients appeared cured at a 6-month follow-up. The efficacy and safety of tazarotene must be confirmed on a larger number of patients, although already documented in nail psoriasis patients often affected by onychomycosis.
Introduction
Onychomycosis is a chronic fungal infection of the nail, characterized by nail discoloration, thickening, and defect. The involved pathogens are dermatophytes, yeasts (Candida), and nondermatophytes.Citation1 Dermatophytes such as Trichophyton rubrum and Trichophyton mentagrophytes are the most common agents of onychomycosis, accounting for 50%–90% of cases, with prevalence of the infection higher in toenails than in fingernails.Citation2 Candida and nondermatophytic molds are frequent in countries with hot and humid climate.Citation3 If untreated, nail fungal infections can extend to other nails and potentially cause further complications, especially in at-risk patients. Aging and reduced peripheral circulation are among the major risk factors for onychomycosis; diabetes weakens the immune function, favoring slow nail growth, thickening, and susceptibility to infections and nail injury.Citation4–Citation7 Onychomycosis sometimes is associated with nail psoriasis, favored by abnormal capillary units and onychodystrophy.Citation8 Differential diagnoses of onychomycosis include chronic nail eczema, bacterial infections, traumatic onychodystrophies, pachyonychia congenita, nail bed tumors, yellow nail syndrome, and idiopathic onycholysis.Citation9 The treatment of onychomycosis is sometimes difficult because the predisposing factors are not influenced by therapy.Citation10,Citation11 Onychomycosis is usually treated with topical or systemic antifungals.Citation12,Citation13 Local treatment requires strong patient adherence because the treatment time is generally long; moreover, onychomycosis-related subungueal hyperkeratosis is generally thick and this limits the penetration of the antimycotic drug. Consequently, long-term treatments can discourage or induce stopping of the therapy before healing is achieved. The Cochrane meta-analysis of Crawford et alCitation14 reports limited success in the treatment of onychomycosis with topical agents. Although many therapeutic options are available, new drugs with a greater safety and relatively rapid efficacy are required. One of the most used topical drug for nail psoriasis is tazarotene.Citation15,Citation16 Its efficacy is classically related to its immunomodulating properties and anti-inflammatory activity, with consequent inhibition of the infective process.Citation17 Tazarotene is also successfully used for acne treatment, given its anti-inflammatory and immune-modulating effectiveness that protect keratinocytes from infection by Propionibacterium acnes.Citation17 Epidermal penetration of tazarotene depends on its ability to reduce hyperkeratinization, favoring keratinocyte differentiation, as also documented by the reduction of expression of hyperproliferation-associated keratins 6 and 16.Citation18 The latter appear dysregulated in genetic diseases, such as pachyonychia congenita and focal palmoplantar keratoderma.Citation18 As a matter of fact, fungal infections could exacerbate or predispose an individual to pachyonychia congenita.Citation19,Citation20 In light of our previous studies reporting the clinical efficacy and the simplicity of the use of tazarotene in the nails of psoriatic patients,Citation15,Citation16 we investigated its effect on distal and lateral subungual onychomycosis in an open preliminary study of immunocompetent patients and its fungistatic activity in vitro.
Patients and methods
We report an observational open clinical trial in 15 patients affected by onychomycosis of the toenail treated with topical tazarotene (Zorac/Tazorac®; Allergan Inc, Irvine, CA, USA) 0.1% gel in an off-label use. The enrolled patients were of both sexes and aged between 14 years and 70 years (). Patients eligible were those affected by distal and lateral subungual onychomycosis without associated skin or systemic diseases, naïve or in washout for other treatments. Exclusion criteria were immunosuppression, treatment for other systemic diseases, and the presence of other diseases causing nail dystrophy such as psoriasis, eczema, and lichen planus. Every patient or parent gave informed signed consent. The study was approved by our local Ethics Committee. The drug was applied once a day on the affected nail plates and nail folds for 12 weeks (end point). Patients were visited every 4 weeks. We evaluated onycholysis, nail bed discoloration, and subungueal hyperkeratosis (thickening of the subungueal region) at baseline and end point, assigning the following semiquantitative scores for onycholysis and discoloration: absence (0), 0%–25% (1), 25%–50% (2), and >50% (3).Citation14 For subungual hyperkeratosis, the scores were as follows: absent (0), 1 mm (1), 2 mm (2), and >3 mm (3).Citation21
Table 1 Clinical characteristics of patients
We also evaluated changes of the affected area comparing baseline and end point appearance of the affected target areas, as reported.Citation22 Briefly, the response rate was assessed by the analysis of digital photographs of the affected nails taken at the baseline and at the end of the study.Citation23 Data were analyzed by means of analysis of variance and Student’s t-test for continuous data and by Mann–Whitney test for ordinal data; P-values <0.05 were considered statistically significant. Mycological cultures and potassium hydroxide stains were also performed on nail samples taken by scraping, clipping, or curetting the affected nail site and subungual region at the baseline and at the end point. Staining of fungi was performed with lactophenol cotton blue solution (Sigma-Aldrich, St Louis, MO, USA).
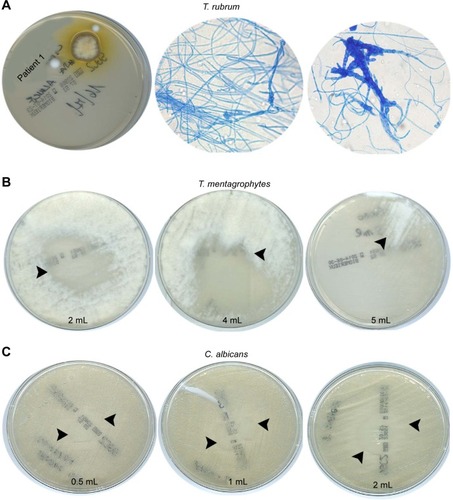
Fungistatic activity of tazarotene in vitro was investigated by disk diffusion assay (Kirby–Bauer method).Citation24 Briefly, 1 g of 0.1% tazarotene gel was dissolved in 3 mL of physiological solution in a sterile tube. To test the effect, a concentration of 0.5 McFarland standard was used for each fungus. For the assays, we used 0.5–5 mL of tazarotene solutions, respectively. The fungi analyzed were Candida albicans, C. glabrata, T. mentagrophytes, and T. verrucosum. Plates were then incubated at 28°C–30°C for 24 hours and 48 hours. The sensitivity was evaluated by measuring the inhibition zone diameter. All statistical analysis was performed using the statistical package SPSS16.0 (SPSS Inc, Chicago, IL, USA).
Results
Mycological cure in target nails (ie, those with mycological confirmation of onychomycosis at baseline) was observed in subungual samples collected at the first follow-up visit (4 weeks) in 40% of patients, and complete cure with complete clinical healing in all patients was observed at the end point (12 weeks). Direct microscopy and in vitro laboratory culture of the sampled material collected after 12 weeks were negative for infections. Representative clinical images of four patients at baseline and end point after tazarotene treatment are reported in . Therapeutic results were good, with no side effects except for mild erythema on the perionychia in two patients; nail growth and tropism were also restored. As shown in , all examined clinical parameters markedly decreased at the end point. The percentage of affected area and the proportion of affected patients decreased (P<0.001; ). Onycholysis, subungual hyperkeratosis, and discoloration completely disappeared in all patients at the end point (P<0.04; ). The nails were completely healed at the follow-up visits up to 6 months.
Figure 1 Representative clinical images of four patients at baseline and end point (12 weeks, topical tazarotene 0.1% gel therapy).

Figure 2 Semiquantitative evaluation of the clinical effect of topical treatment of tazarotene 0.1% gel.
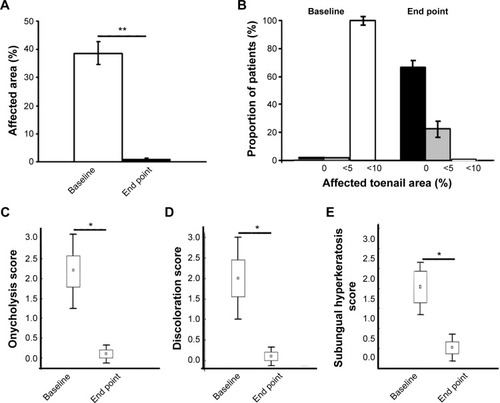
Patients’ fungal culture testCitation11 was performed at baseline (); 66.7% of patients were positive for T. rubrum (), 13.3% for T. mentagrophytes, 13.3% for E. floccosum, and 6.7% for T. tonsurans. Disk diffusion assay () document the inhibition of T. mentagrophytes growth, starting with 2 mL of tazarotene solution, which became almost complete with 5 mL (), as well as the reduced growth of C. albicans () starting with 1 mL of tazarotene solution. Similar results were observed with plates with C. glabrata and T. verrucosum, with greater prominence in the presence of 4 mL and 5 mL of the solution (not shown).
Figure 3 Patients’ fungal culture test.
Discussion
In this study, we have reported the therapeutic efficacy of tazarotene 0.1% gel for the topical treatment of distal and lateral subungual onychomycosis. T. rubrum, T. mentagrophytes, and E. floccosum are the most common agents implicated in onychomycosis.Citation12 These dermatophytes are hyaline-septated molds, whose growing fungal hyphae penetrate into the stratum corneum of the skin and nails. The fungal infection produces keratinolytic proteases, creating a gap in the living cells.Citation25 Some fungi have developed the ability to digest keratinous debris in soil and the faculty of parasitizing keratinous tissues in animals.Citation25 Compared to the normal skin, the nail apparatus has a different immunological profile, a strong innate immunity, and an increased expression of antimicrobial peptides.Citation26 On the other hand, the nail apparatus has a lower level of major histocompatibility complex class-1a antigen expression, production of immunosuppressive agents, anomalies of antigen-presenting cells, and inhibition of natural killer cell activity,Citation27 all aspects that favor onychomycosis.
Successful topical treatment of nail onychomycosis is fraught with difficulty due to several factors, including slow nail growth, the physical presence of nail plate interfering with nail bed access, and the difficulty in finding compounds with adequate pharmacologic profile for nail penetration.Citation28 These difficulties are reflected in the high incidence of recurrence after topical therapeutic clearance.Citation29 At present, the most frequently used topical therapies for onychomycosis are amorolfine 5%, ciclopirox 8% nail lacquer, and tioconazole 28% solution, which need to be applied for prolonged periods and require strong adherence by the patients.Citation13 Amorolfine 5% nail lacquer is effective as monotherapy for the treatment of onychomycosis, but with limited efficacy when distal nail involvement is greater than 50%.Citation30 Up to June 2014, ciclopirox was the only topical treatment approved by the US Food and Drug Administration for onychomycosis in the US.Citation28 The action of ciclopirox differs from that of other topical antifungal drugs, which generally act through ergosterol inhibition. The high affinity of ciclopirox for trivalent metal cations results in the inhibition of the metal-dependent enzymes responsible for the degradation of peroxides within the fungal cell.Citation31 Efficacy of ciclopirox 8% as a topical monotherapy (ranged from 20% to 36%) has been disappointing and limited to the mildest cases of toenail onychomycosis.Citation28 For the remaining cases, a combined therapy with a systemic antifungal is recommended.Citation28 Nevertheless, oral antifungals have general adverse effects, including intestinal and respiratory complaints.Citation32 Tioconazole is an imidazole antifungal agent recommended for local infections caused by CandidaCitation28 and can be used for the topical treatment of pachyonychia. Efinaconazole 10% and tavaborole 5% solutions are new topical antifungals specifically developed for the treatment of dermatophytic onychomycosis. In Phase III clinical trials, both newer agents were applied once daily for 48 weeks without concomitant nail debridement. Reported mycologic cure rates with efinaconazole are superior to that achieved with ciclopirox 8% nail lacquer.Citation33 In our study, complete healing after topical treatment with tazarotene was obtained at the first follow-up visit after 4 weeks in 40% of patients and complete healing in all patients after 12 weeks, with a rapid and progressive amelioration of all evaluated clinical parameters. The cure was confirmed by negative mycological culture and KOH stains. Sometimes, the ineffectiveness of topical treatment is due to the subungual strong hyperkeratosis, which prevents drug penetration.Citation34 Hyperkeratosis also represents one of the most frequent features of nail psoriasis, and nail psoriatic patients also suffer from onychomycosis.Citation35 In our patients, tazarotene has proven quite effective in reducing hyperkeratinization in fungus-infected nails. Concerning the therapeutic effects of tazarotene, our results in vitro document a direct fungistatic activity. Tazarotene is a synthetic third-generation retinoid derived from vitamin A, which has proved to be beneficial in modulating keratinocyte proliferation and in reducing inflammation. Tazarotene is used for the treatment of acne, nonmelanoma skin tumors, and inflammatory skin diseases such as psoriasis.Citation36–Citation38 In particular, tazarotene’s effect is mediated by the intracellular upregulation of cellular retinoic acid-binding protein-II expression,Citation39 which transactivates nuclear retinoic acid receptors (RARs), in particular RAR and RARγ, by binding to specific DNA sequences on their promoter gene regions, leading to reduced proliferation of normal and neoplastic cells and favoring differentiation and apoptosis.Citation36–Citation38,Citation40 The reduction in the excessive V-Akt murine thymoma viral oncogene homolog 1 activation supporting cell growthCitation41 may also explain the beneficial effects of tazarotene on ungual hyperkeratosis. Moreover, tazarotene can exert a protective action on the microvascular bed against fungal infection, similarly to that reported for psoriasis patients.Citation16 Finally, the activity of tazarotene against inflammation through immunomodulation may induce the blocking of fungal keratinolytic proteases, thus contributing to its efficacy. A limitation of our preliminary study results is the absence of a randomized placebo control group. Nevertheless, a recent analysis published in 2014 reveals that in 21 randomized controlled trials of dermatophytic nail onychomycosis, present in the PubMed database, placebo cure varied from 8.7% to 1.2%, documenting that the pooled placebo cure mean rate is very low.Citation42
Conclusion
Our preliminary results documented the safety and rapid efficacy of topical treatment with tazarotene on distal and lateral subungual onychomycosis, thus representing an alternative new promising therapeutic approach. Treated and cured patients were followed every 4 weeks, with no evidence of recurrence after 6 months. We also documented the fungistatic activity of tazarotene in T. mentagrophytes, T. verrucosum, C. albicans, and C. glabrata, supporting the theoretical assumption about its direct action on fungus replication. Our clinical evidence of efficacy suggests that tazarotene could be useful in those patients with treatment-resistant forms of onychomycosis or in those with evident enhanced nail thickening, wherein the therapeutic reducing action of the retinoid can be providential. Further studies concerning the specific effects of tazarotene and in a larger cohort of patients with a longer follow-up are needed to confirm the efficacy in terms of relapse and reinfection.
Acknowledgments
The authors wish to thank Denis Mariano for editing assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
- WesterbergDPVoyackMJOnychomycosis. Current trends in diagnosis and treatmentAm Fam Physician2013881176277024364524
- KaurRKashyapBBhallaPOnychomycosis – epidemiology, diagnosis and managementIndian J Med Microbiol200826210811618445944
- ChiCCWangSHChouMCThe causative pathogens of onychomycosis in southern TaiwanMycoses200548641342016262878
- DrakeLADinehartSMFarmerERGuidelines of care for superficial mycotic infections of the skin: tinea corporis, tinea cruris, tinea faciei, tinea manuum, and tinea pedis. Guidelines/outcomes committee. American academy of dermatologyJ Am Acad Dermatol1996342 pt 12822868642094
- ScherRKDiseases of the nailsConnHCurrent TherapyPhiladelphia, PAThe W. B. Saunders Co1990736742
- TostiAHayRArenas-GuzmanRPatients at risk of onychomycosis – risk factor identification and active preventionJ Eur Acad Dermatol Venereol200519suppl 1131616120200
- DiasNSantosCPortelaMLimaNToenail onychomycosis in a Portuguese geriatric populationMycopathologia20111721556121365319
- LeiboviciVHershkoKIngberAWestermanMLeviatan-StraussNHochbergMIncreased prevalence of onychomycosis among psoriatic patients in IsraelActa Derm Venereol2008881313318176747
- ScherRKTavakkolASigurgeirssonBOnychomycosis: diagnosis and definition of cureJ Am Acad Dermatol200756693994417307276
- DrakeLADinehartSMFarmerERGuidelines of care for superficial mycotic infections of the skin: pityriasis (tinea) versicolor. Guidelines/outcomes committee. American academy of dermatologyJ Am Acad Dermatol1996342 pt 12872898642095
- ScherRKOnychomycosis: a significant medical disorderJ Am Acad Dermatol1996353 pt 2S2S58784302
- ElewskiBEOnychomycosis: pathogenesis, diagnosis, and managementClin Microbiol Rev19981134154299665975
- PiracciniBMGianniCUpdate on the management of onychomycosisG Ital Dermatol Venereol2013148663363824442043
- CrawfordFHollisSTopical treatments for fungal infections of the skin and nails of the footCochrane Database Syst Rev2007183CD00143417636672
- DiluvioLCampioneEPaternoEJMordentiCEl HachemMChimentiSChildhood nail psoriasis: a useful treatment with tazarotene 0.05%Pediatr Dermatol200724333233317542899
- BianchiLSodaRDiluvioLChimentiSTazarotene 0.1% gel for psoriasis of the fingernails and toenails: an open, prospective studyBr J Dermatol2003149120720912890227
- EpsteinELStein GoldLSafety and efficacy of tazarotene foam for the treatment of acne vulgarisClin Cosmet Investig Dermatol20136123125
- GregoriouSKritsotakiEKatoulisARigopoulosDUse of tazarotene foam for the treatment of acne vulgarisClin Cosmet Investig Dermatol20147165170
- IraciSBianchiLGattiSCarrozzoAMBettiniDNiniGPachyonychia congenita with late onset of nail dystrophy – a new clinical entity?Clin Exp Dermatol19931854784808252777
- HarrisKHullPRHansenCDTransgrediens pachyonychia congenita (PC): case series of a nonclassical PC presentationBr J Dermatol2012166112412821790523
- KlaassenKMvan de KerkhofPCBastiaensMTPlusjeLGBaranRLPaschMCScoring nail psoriasisJ Am Acad Dermatol20147061061106624698704
- ElewskiBERichPPollakREfinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studiesJ Am Acad Dermatol201368460060823177180
- SipponenPSipponenALohiJSoiniMTapanainenRJokinenJJNatural coniferous resin lacquer in treatment of toenail onychomycosis: an observational studyMycoses201356328929623131104
- KnowlesRCMooreTDQuality control of agar diffusion susceptibility tests. Data from the quality assurance service microbiology program of the college of American pathologistsAm J Clin Pathol1980744 suppl5815856776805
- HayRJFungal skin infectionsArch Dis Child1992679106510671417045
- DorschnerRALopez-GarciaBMassieJKimCGalloRLInnate immune defense of the nail unit by antimicrobial peptidesJ Am Acad Dermatol200450334334814988673
- ItoTMeyerKCItoNPausRImmune privilege and the skinCurr Dir Autoimmun200810275218460879
- Del RossoJQThe role of topical antifungal therapy for onychomycosis and the emergence of newer agentsJ Clin Aesthet Dermatol201477101825053979
- De CuyperCHindryckxPHLong-term outcomes in the treatment of toenail onychomycosisBr J Dermatol1999141suppl 56152010730909
- ChangCHYoung-XuYKurthTOravJEChanAKThe safety of oral antifungal treatments for superficial dermatophytosis and onychomycosis: a meta-analysisAm J Med2007120979179817765049
- SubissiAMontiDTogniGMaillandFCiclopirox: recent nonclinical and clinical data relevant to its use as a topical antimycotic agentDrugs201070162133215220964457
- EpsteinEHow often does oral treatment of toenail onychomycosis produce a disease-free nail? An analysis of published dataArch Dermatol199813412155115549875192
- GuptaAKPaquetMEfinaconazole 10% nail solution: a new topical treatment with broad antifungal activity for onychomycosis monotherapyJ Cutan Med Surg201418315115524800702
- DiasMFQuaresma-SantosMVBernardes-FilhoFAmorimAGSchechtmanRCAzulayDRUpdate on therapy for superficial mycoses: review article part IAn Bras Dermatol201388576477424173183
- KlaassenKMDulakMGvan de KerkhofPCPaschMCThe prevalence of onychomycosis in psoriatic patients: a systematic reviewJ Eur Acad Dermatol Venereol201428553354124033871
- BianchiLOrlandiACampioneETopical treatment of basal cell carcinoma with tazarotene: a clinicopathological study on a large series of casesBr J Dermatol2004151114815615270884
- ThacherSMVasudevanJChandraratnaRATherapeutic applications for ligands of retinoid receptorsCurr Pharma Des2000612558
- OrlandiABianchiLCostanzoACampioneEGiusto SpagnoliLChimentiSEvidence of increased apoptosis and reduced proliferation in basal cell carcinomas treated with tazaroteneJ Invest Dermatol200412241037104115102095
- BushueNWanYJRetinoid pathway and cancer therapeuticsAdv Drug Deliv Rev201062131285129820654663
- LotanRRetinoids in cancer chemopreventionFASEB J1996109103110398801164
- CervelliVScioliMGGentilePPlatelet-rich plasma greatly potentiates insulin-induced adipogenic differentiation of human adipose-derived stem cells through a serine/threonine kinase Akt-dependent mechanism and promotes clinical fat graft maintenanceStem Cells Transl Med20121320622023197780
- GuptaAKDaigleDPaquetMTherapies for onychomycosis: a systematic review and network meta-analysis of mycological cureJ Am Podiatr Medl Assoc Epub2014717
