Abstract
Background
No specific study has focused on patients with metastatic squamous cell carcinoma of the head and neck (SCCHN) at diagnosis. Due to high response rates of induction chemotherapy in chemo-naïve patients with localized disease, their prognosis should be better than patients with recurrent disease.
Methods
From January 1, 2008 to July 1, 2012, we retrospectively collected all patients’ records with SCCHN diagnosed as metastatic. Patients, disease, treatment and its results were analyzed. Survival was calculated using the Kaplan–Meier method.
Results
Of the 749 new patients treated for SCCHN in our institution, 16 (2.1%) were metastatic at diagnosis, of whom five had cytological results to prove it. Six patients died before treatment or had palliative care and ten received initial chemotherapy and then surgery and/or radiotherapy according to the primary response. Four patients treated with first-line chemotherapy with docetaxel-5FU-cisplatin (TPF) showed a complete response of metastatic lesions allowing locoregional treatment. The overall survival at 1 year and 3 years was 50% and 24%, respectively. The median survival was 7 months (1–72 months). Seven patients (43.7%) had a higher survival at 12 months, including five (31.5%) who are still alive without recurrence with a mean follow-up of 30 months. There was a significant difference in overall survival (P<0.01) between patients who had chemotherapy with TPF versus other therapeutic protocols. The median survival of patients with lung metastases only was 15 months (1–72 months), significantly higher than that of patients with liver and/or bone localizations, which was 2 months (1–9 months).
Conclusion
Patients with metastatic SCCHN treated by TPF followed by multimodal treatment could achieve long survival.
Introduction
To our knowledge, there has been no specific study on patients who present with metastatic squamous cell carcinoma of the head and neck (SCCHN), which represents between 1.5% and 16.8% of newly diagnosed cancer patients.Citation1–Citation3 These patients are typically included in studies of patients with relapse whose prognosis is poor, with a survival of 10.1 months in Phase III studies with the best results.Citation4 However, it is noteworthy that in patients receiving treatment for the first time, the response rates of SCCHN to induction chemotherapy ranges from 68% to 72%, among the highest rates for solid tumors.Citation5,Citation6 Moreover, studies have shown that for some localized tumors, chemotherapy alone resulted in a cure.Citation7,Citation8 More recently, a case report showed that it was possible to achieve long-term remission in a patient with a metastatic oropharyngeal tumor.Citation9 Together these elements lead us to believe that the initial treatment of some of these metastatic patients could be curative.
The main objective of this study was to show from the study of a registry that prolonged survival is possible with multimodal treatment combining chemotherapy, surgery, and radiotherapy in some metastatic patients.
The secondary objectives were to establish an epidemiological profile of metastatic patients and to identify indications making it possible to revise the purpose of treatment for highly selected patients.
Materials and methods
From January 1, 2008 to July 1, 2012, all new patients with SCCHN identified from the Multidisciplinary Consultation Meeting registry were sent to the Lyon Sud Hospital Center (referral center).
Patients with nasopharyngeal or sinusoidal-nasal carcinoma were excluded.
We then observed in this group all patients who were diagnosed as metastatic and treated as such.
We collected data on age, sex, performance status for general health, tobacco use, alcohol consumption, T stage, N stage, the site of metastases, diagnostic procedures, therapeutic decision and its implementation, as well as evolution of the disease in the patient. Survival was calculated using the Kaplan–Meier method.
Results
Patients
From January 1, 2008 to July 1, 2012, 888 new patients were identified from the Lyon Sud hospital center Multidisciplinary Consultation Meeting registry, including 749 with cancer of the oral cavity, oropharynx, hypopharynx or larynx. Of these patients, 16 (2.1%) were metastatic (14 men, 2 women) with a mean age of 61.7 years (48–89 years). Fourteen patients were tobacco smokers (more than 10 pack-years), and five patients also had a high daily alcoholic consumption.
The diagnosis of metastases was made using a cervico-thoracic computed tomography (CT) scan for all patients, supplemented by a positron emission tomography (PET) scan for five patients, cytology for five patients, and bone scintigraphy for one patient.
The main characteristics of patients and their tumors are listed in .
Table 1 Patients and tumor characteristics
Therapeutic strategy
Four patients were not treated: they either died before any treatment (n=2) or only supportive care was given (n=2).
Ten patients were treated with initial chemotherapy. Among these patients, the treatment program was carried out fully in 70% of cases (n=7), one patient died after the first course from evolution of the disease; and poor tolerance did not allow continuation of treatment for two others.
Four patients treated with first-line chemotherapy with docetaxel-5FU-cisplatin (TPF) showed a complete response of metastatic lesions allowing locoregional treatment with surgery and/or radiotherapy in the head and neck region. Two patients had maintenance treatment with cetuximab after radiotherapy.
One patient had tumor surgery with neck dissection; and resection of two lung metastases followed by cervical radiotherapy.
One patient first had tumor surgery and neck dissection followed by cervical radiotherapy plus cetuximab.
The sequence of initial treatment for the 16 patients included is summarized in .
Table 2 Results
Survival
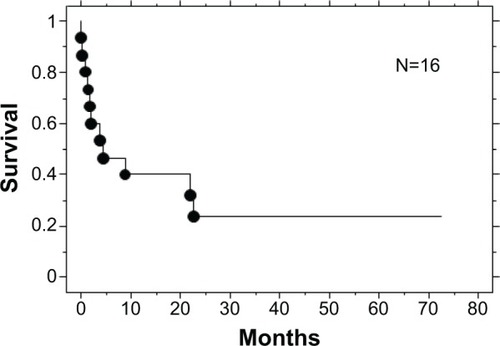
The overall survival at 1 year and 3 years was 50% and 24%, respectively. The median survival was 7 months (1–72 months) ().
Five patients are alive, including four with no evidence of disease at 14, 20, 52, and 72 months after diagnosis, respectively.
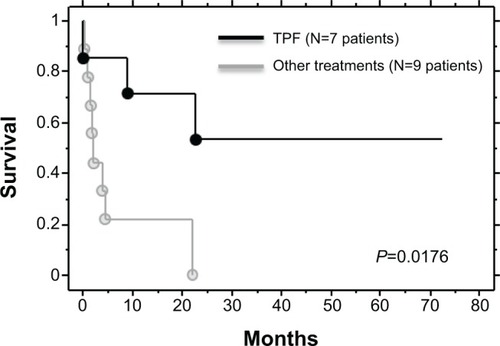
There was a significant difference in overall survival (P<0.01) between patients who had chemotherapy with TPF versus other therapeutic protocols (). Seven patients (43.7%) had a higher survival at 12 months, including five who are still alive without recurrence with a mean follow-up of 30 months. All these patients received multimodal treatment.
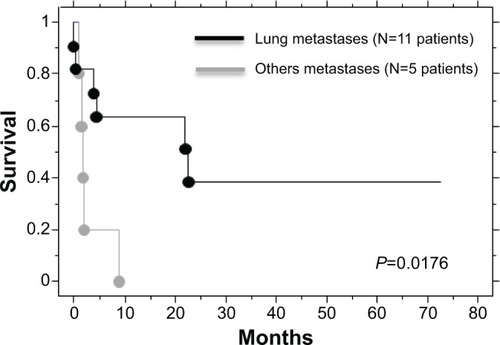
The median survival of patients with lung metastases only was 15 months (1–72 months), significantly higher than that of patients with liver and/or bone localizations, which was 2 months (1–9 months) ().
The results for each patient are summarized in .
Discussion
The treatment of patients with metastatic SCCHN is poorly documented. Studies found in the literature focus mainly on the treatment of secondary metastases, the incidence of which varies from 9.2% to 38%, depending on the study.Citation10,Citation11 When diagnosing SCCHN, the percentage of metastatic patients is lower, ranging from 1.5% to 16.8%.Citation2,Citation3 In the largest published series we found on 73,247 new patients, 2.82% had immediate metastases,Citation1 this percentage is close to our study (2.13%). These figures are dependent on diagnostic tools used to investigate possible secondary localizations. Modern imaging, in particular CT and PET-CT, increases the sensitivity of detection but the false positive rate is about 5%.Citation12
Diagnostic confirmation of secondary lesions should be based on histological evidence, evidence that in practice is not always easy to obtain and often cannot differentiate a primary from a secondary lesion for pulmonary localizations. Because of these constraints, we only have five patients in our study with a histological diagnosis of metastases; for the other patients the initial diagnosis was based on imaging parameters (CT/PET), and for four patients evolution of the tumor confirmed the secondary lesions a posteriori.
The presence of distant metastases is involved in the therapeutic decision, and the proposed treatment is based on generally palliative chemotherapy. The prognosis is poor with a median survival of 1–12 months and 88% of patients die in the year following diagnosis.Citation12 The type of chemotherapy in these patients is not codified as efficacy studies are carried out on patients with metachronous metastases, who are rarely chemotherapy-naïve. Presumably these two patient populations are different. Indeed, when we compare the response rate obtained by first line palliative chemotherapy (10%–53%)Citation4,Citation13–Citation15 with those obtained with induction chemotherapy (68%–72%)Citation5,Citation6 the difference is significant, which means that treatment-naïve SCCHN tumors are very chemo-sensitive tumors. In addition, studies have shown that it is possible to obtain cures with chemotherapy alone in patients with locally advanced non-metastatic SCCHN.Citation7,Citation8 It therefore does not seem illogical to propose a curative treatment in some metastatic patients.
In our study, patients who were in good general condition were treated according to the standard induction protocol with TPF to allow the best possible locoregional control. As expected,Citation16 this chemotherapy is relatively toxic with two patients who had to stop due to side effects. After chemotherapy, local surgery was performed followed by radiation for patients with complete response on metastase and for who it remains only a locally advanced disease. Indeed, even if the disease is incurable, it is important in terms of quality of life to avoid locoregional evolution at all costs. When this was possible, surgery of metastases was performed. Our seven patients treated with this multidisciplinary approach had a longer than 12 months survival, with a median of 30.8 months and four treated patients remain disease-free at 14, 20, 52, and 72 months.
The role of surgery in metastatic patients remains controversial. It can be used on tumor, lymph node, or metastases. It generally allows a better quality of survival, better control of symptoms, and prevents rupture of big vessels and the need for tracheotomy.Citation17 Metastatic surgery mainly addresses secondary pulmonary lesions, but may be indicated for certain liver lesions.Citation9 In the literature, pulmonary metastasectomy is associated with improved survival, these data concern limited retrospective studies that do not relate specifically to immediate metastases.Citation18–Citation20
The role of radiotherapy is also debatable. In the literature, a single-center, retrospective study by Ampil et al including seven metastatic patients found a prolonged survival of 14 months for four irradiated patients versus 5.5 months for three non-irradiated patients.Citation21
The type of chemotherapy as potentiation of the radiotherapy is a function of the chemotherapy initially administered. We know that after four or more courses of TPF, tolerance is better if radiotherapy is potentiated with cetuximab than with cisplatin.Citation22,Citation23 Continuation of cetuximab as maintenance is based on data from Vermorken et al’s study.Citation4 Since the prognosis of human papillomavirus (HPV) positive tumors has clearly been demonstrated to be better, it should be interesting to have the HPV status. Unfortunately it was not possible because it was not routine practice. Today it is done only for clinical trials. But in our study, only two out of seven patients with a survival longer than 15 months have cancer of the oropharynx that is known to be the major site for HPV positive tumors.
Conclusion
For patients with immediate metastases, our study suggests that when the patient’s general condition allows it, treatment by chemotherapy induction with TPF type has a good outcome, particularly on metastases. Optimal locoregional treatment with surgery and/or radiotherapy may be proposed to ensure local control. Resection of residual metastases seems beneficial. This multidisciplinary approach results in a large number of long-term survivors without evidence of recurrence (four out of seven patients eligible for this approach).
Disclosure
Philippe Céruse is a member of the board of Merck Serono. The other authors have no conflicts of interest to disclose.
References
- Kuperman DI Auethavekiat V Adkins DR Squamous cell cancer of the head and neck with distant metastasis at presentation Head Neck 2011 33 5 714 718 20872838
- Jackel MC Rausch H Distant metastasis of squamous epithelial carcinomas of the upper aerodigestive tract. The effect of clinical tumor parameters and course of illness HNO 1999 47 1 38 44 German 10093788
- de Bree R Deurloo EE Snow GB Leemans CR Screening for distant metastases in patients with head and neck cancer Laryngoscope 2000 110 3 Pt 1 397 401 10718426
- Vermorken JB Mesia R Rivera F Platinum-based chemotherapy plus cetuximab in head and neck cancer N Engl J Med 2008 359 11 1116 1127 18784101
- Posner MR Hershock DM Blajman CR Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer N Engl J Med 2007 357 17 1705 1715 17960013
- Vermorken JB Remenar E van Herpen C Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer N Engl J Med 2007 357 17 1695 1704 17960012
- Laccourreye O Veivers D Hans S Menard M Brasnu D Laccourreye H Chemotherapy alone with curative intent in patients with invasive squamous cell carcinoma of the pharyngolarynx classified as T1-T4N0M0 complete clinical responders Cancer 2001 92 6 1504 1511 11745228
- Holsinger FC Lin HY Bassot V Laccourreye O Platin-based exclusive chemotherapy for selected patients with squamous cell carcinoma of the larynx and pharynx Cancer 2009 115 17 3909 3918 19551883
- Chowdhry VK Hsu J Lemke S Kittur D Hahn SS Long-term survival in a patient with metastatic oropharynx squamous cell carcinoma to liver J Cancer Res Ther 2012 8 1 138 141 22531535
- Garavello W Ciardo A Spreafico R Gaini RM Risk factors for distant metastases in head and neck squamous cell carcinoma Arch Otolaryngol Head Neck Surg 2006 132 7 762 766 16847186
- Alvi A Johnson JT Development of distant metastasis after treatment of advanced-stage head and neck cancer Head Neck 1997 19 6 500 505 9278758
- de BR Haigentz MJr Silver CE Distant metastases from head and neck squamous cell carcinoma. Part II. Diagnosis Oral Oncol 2012 48 9 780 786 22520053
- Forastiere AA Metch B Schuller DE Randomized comparison of cisplatin plus fluorouracil and carboplatin plus fluorouracil versus methotrexate in advanced squamous-cell carcinoma of the head and neck: a Southwest Oncology Group study J Clin Oncol 1992 10 8 1245 1251 1634913
- Glisson BS Murphy BA Frenette G Khuri FR Forastiere AA Phase II Trial of docetaxel and cisplatin combination chemotherapy in patients with squamous cell carcinoma of the head and neck J Clin Oncol 2002 20 6 1593 1599 11896109
- Schoffski P Catimel G Planting AS Docetaxel and cisplatin: an active regimen in patients with locally advanced, recurrent or metastatic squamous cell carcinoma of the head and neck. Results of a phase II study of the EORTC Early Clinical Studies Group Ann Oncol 1999 10 1 119 122 10076732
- Fayette J Bonnin N Ferlay C Neoadjuvant TPF in locally advanced head and neck cancer can be followed by radiotherapy combined with cisplatin or cetuximab: a study of 157 patients Anticancer Drugs 2013 24 6 623 629 23542750
- Haigentz MJr Hartl DM Silver CE Distant metastases from head and neck squamous cell carcinoma. Part III. Treatment Oral Oncol 2012 48 9 787 793 22516376
- Wedman J Balm AJ Hart AA Value of resection of pulmonary metastases in head and neck cancer patients Head Neck 1996 18 4 311 316 8780941
- Winter H Meimarakis G Hoffmann G Does surgical resection of pulmonary metastases of head and neck cancer improve survival? Ann Surg Oncol 2008 15 10 2915 2926 18648883
- Shiono S Kawamura M Sato T Pulmonary metastasectomy for pulmonary metastases of head and neck squamous cell carcinomas Ann Thorac Surg 2009 88 3 856 860 19699911
- Ampil FL Kim DD Ghali GE Baluna RG How intensive should radiotherapy for head and neck cancer with synchronous distant metastases be? Review of cases J Oral Maxillofac Surg 2012 70 3 730 733 21783296
- Buiret G Combe C Favrel V A retrospective, multicenter study of the tolerance of induction chemotherapy with docetaxel, Cisplatin, and 5-Fluorouracil followed by radiotherapy with concomitant cetuximab in 46 cases of squamous cell carcinoma of the head and neck Int J Radiat Oncol Biol Phys 2010 77 2 430 437 19775831
- Lefebvre JL Pointreau Y Rolland F Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy for larynx preservation: the TREMPLIN randomized phase II study J Clin Oncol 2013 31 7 853 859 23341517