Abstract
Purpose
To determine the type, frequency, and factors associated with medication preparation and administration errors in adult intensive care units (ICUs) and neonatal ICUs (NICUs)/pediatric ICUs (PICUs).
Patients and methods
We conducted a prospective direct observation study in an adult ICU and NICU/PICU in a tertiary university hospital. Between June 2012 and June 2013, a clinical pharmacist and medical student observed the nursing care staff on weekdays during the preparation and administration of intravenous drugs. We analyzed the frequency and type of preparation and administration errors and factors associated with errors.
Results
Six hundred and three preparations in the adult ICU and 281 in the NICU/PICU were observed. Three hundred and eighty-five errors occurred in the adult ICU and 38 in the NICU/PICU. There were 5,040 and 2,514 error opportunities, with overall error rates of 7.6% and 1.5%, respectively. The total opportunities for error meant each single step of preparation and administration that was relevant for the drug. Most errors applied to the category “uniform mixing” (adult ICU: n=227, 59%; NICU/PICU: n=14, 37%). The multivariate logistic regression results showed a significantly different influence of the “preparation type” for the adult ICU compared with the NICU/PICU with regard to the occurrence of an error. Preparations for adult patients of the LCD type (liquid concentrate with diluent into syringe or infusion bag) were more often associated with errors than the P (powder in a glass vial that must be reconstituted and diluted if necessary), P=0.012, and LC (liquid concentrate into syringe), P=0.002 type.
Conclusion
“Uniform mixing” was the most erroneous preparation step in intravenous drug preparations in two ICUs. Improvement of nurse training and the preparation of prefilled syringes in the pharmacy might reduce errors and improve the quality and safety of drug therapy.
Introduction
Drug therapy for hospital inpatients is error prone. Errors can cause adverse events and patient harm. MEs can occur during the prescription, preparation, and administration processes.Citation1 Critically ill patients in ICUs usually need numerous intravenous medications, and the error risk is multiplied by the number of calculation and preparation steps. Therefore, the preparation and administration performed by the nursing staff in the ward are complex and time-consuming.Citation2 The administration step of a drug is the last barrier before an error could affect a patient. Error detection is less likely if the same person performs preparation and administration, which is a common practice in ICUs. This makes ICU patients especially vulnerable to preparation and administration errors for intravenous drugs.Citation3–Citation10 Studies show error rates for at least one error with preparations of intravenous drugs of 48.4%–97.7%.Citation5,Citation6,Citation9 NICU/PICU patients have an even higher risk of MEs because of the use of off-label and unlicensed drugsCitation11 and the lack of weight-adapted drug doses and strengths for use in this patient group.Citation8,Citation12 The preparation of pediatric intravenous drugs often includes dilution steps from the more concentrated original solutions that are used for adults.Citation13 Studies with pediatric inpatients alone show error rates of 8.0%–62.7% for the preparation and administration of all types of drugs.Citation8,Citation14–Citation19
Interventions such as nurse training and central preparation of drugs in the pharmacy reduce the error rates for the preparation and administration of intravenous drugs.Citation2,Citation18
First, we aimed to determine the type and frequency of MEs at the preparation and administration processes in two ICUs in our hospital. The secondary objective was to identify factors that could influence the error rate.
Patients and methods
We conducted an observational study in the NICU/PICU and one in the adult ICU at a university hospital. Both studies have been approved by the local ethics committee (EK 151/12 and EK 175/13) and by the local data protection officer of the medical faculty of RWTH Aachen University. Additionally, the director of nursing of the wards provided their informed consent. Furthermore, before conducting the study, the observer introduced herself to every nurse and asked for permission for direct observation. Only after the oral informed consent by nurse, the observer started data collection.
A clinical pharmacist and medical student directly and disguisedly observed the nursing care staff during the preparation and administration of intravenous drugs on the wards. The observation was disguised because the nursing care staff was not aware of the goal of the study. The nursing care staff was informed about an observation on the ICUs but not about the data collection form and the different steps observed in detail.
For the protection of privacy, we did not record either patient data or the names of the nurses. We determined the average number of nurses per shift, the number of occupied beds, and the nurse–patient ratio for the observation period.
Setting
Between June and August 2012, the clinical pharmacist and medical student observed the adult ICU. The medical student was trained by the clinical pharmacist in standard practices for preparation and application of injectable drugs to ensure that both observers used the same error definition prior to the observation period. Data collection was preceded by 3 pilot-days during which the observers became familiar with the processes and medications on the ward. Between September 2012 and June 2013, the medical student observed the nursing care staff of the NICU/PICU. During this period, the clinical pharmacist supervised the medical student while being available for questions and discussions. Drug prescription in the adult ICU was done in the CPOE system Philips CS770 ICCA, Philips Medical Systems, Andover, MA, USA. After preparing the medication according to the physicians’ prescription on the ward and administering it to the patient, nurses electronically confirmed each administration of medication in the ICCA.
NICU/PICU physicians prescribed medication using the CPOE VISITE 2000, Pharma GmbH, Oberhaching, Germany. Prescriptions were printed out for the nurse to transcribe the medication in the paper-based patient record. The nurse prepared the medication in a separate room with an LAF, administered it to the patient, and confirmed the administration in the patient record.
Data collection
Data collection on both wards was performed on weekdays during the day at time periods when usually most preparations were performed. Drug rounds took place in the morning, at lunchtime, and in the evening. The observers attended at least one drug round per day. The sampling was performed by time period and not by patient. A standardized data collection form was used to evaluate the steps of the preparation and administration processes for intravenous drugs, including drug name, solvent, diluent, reconstitution, mixing, dose, labeling, time and route of administration, and administration rate. Errors were classified in one category of ME (). We chose this classification in accordance with a compilation of the American Society of Hospital Pharmacists in the guidelines on preventing MEs in hospitals with a focus on errors in different preparation steps.Citation20 Each prepared drug was assigned into the “type of preparation” () and “therapeutic drug class” that was defined by the first level of WHO ATC class. If an ME was likely to result in a serious adverse event, the observer intervened in the preparation or administration process. Otherwise, there was no intervention by the observer when an error occurred.
Table 1 Categories of MEs in the preparation and administration processes
Table 2 Type of preparation
Definitions
According to the NCC MERP, MEs are defined as “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Such events may be related to professional practice, health care products, procedures, and systems, including prescribing, order communication, product labeling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use”.Citation1 In our study, inappropriate medication use was defined as any instance in which the preparation or administration of injectable drugs varied from the physician’s prescription, the SMPC of the drug, hospital policies and procedures, national/international guidelines, internal guidelines, or the good manufacturing practice. Aspects of hygiene (hand disinfection, workplace surface disinfection, and disinfection of vial membrane) were not considered. Additionally, we did not assess the clinical appropriateness of the prescription.
Data analysis
We calculated the overall error rate as percentage (with a 95% CI) for both ICU and NICU/PICU by dividing the overall number of errors by the number of total opportunities for error for all observed preparations. The total opportunities for error meant each single step of preparation and administration that was relevant for the drug. Additionally, we calculated the error rate as a percentage (with a 95% CI) for both the ICU and NICU/PICU. The error rate in percentage was the number of preparations with at least one error, in relation to the number of all observed preparations multiplied by 100.
Furthermore, we calculated the error rate as a percentage (with a 95% CI) for every category of ME by dividing the number of errors per single category by the number of all observed preparations with relevance for the category.
A generalized linear mixed model with a binary distribution (PROC GLIMMIX) was used to investigate the possible influence of “ward” adjusted for “preparation type” and “therapeutic drug class” for the primary outcome to make an error within a drug preparation. The intercept was assumed to be random. We assessed a 5% significance level for each model and adjusted CIs and P-values for multiple testing by the Scheffé method.Citation21 Significant interaction effects were included in the model. Statistical analyses were performed using SAS (version 9.4; SAS Institute Inc., Cary, NC, USA) and R (version 3.3.0).Citation22
Results
The pharmacist and medical student observed 884 preparations: 603 preparations in the adult ICU and 281 preparations in the NICU/PICU (). In two cases in the adult ICU, the observer intervened in the preparation process because of a wrong dose. The first error was related to a tenfold insulin dose and the second one to a tenfold penicillin dose. In the NICU/PICU, there was no intervention. On the adult ICU, 340 preparations had at least one error (error rate 56%, 95% CI: 52–60). There were 385 errors out of 5,040 error opportunities, with an overall error rate of 7.6% (95% CI: 6.9–8.4). In the NICU/PICU, 36 preparations had at least one error (error rate 13%, 95% CI: 8.9–17). There were 38 out of 2,514 error opportunities, with an overall error rate of 1.5% (95% CI: 1.0–2.0). We assigned each preparation into a type of preparation and a therapeutic drug class ().
Figure 1 Results of observation studies in the adult ICU and NICU/PICU.
Abbreviations: C, cardiovascular system; CI, confidence interval; ICU, intensive care unit; J, anti-infectives for systemic use; LC, liquid concentrate into syringe; LCD, liquid concentrate with diluent into syringe or infusion bag; N, nervous system; NICU, neonatal intensive care unit; P, powder in a glass vial that must be reconstituted and diluted if necessary; PICU, pediatric intensive care unit.
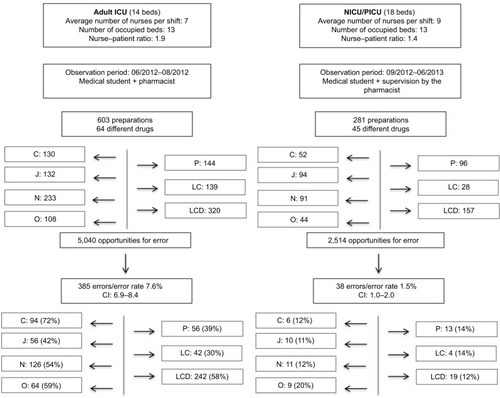
Most errors in the adult ICU occurred in the categories “uniform mixing” (n=227 in 351 preparations, 65% error rate; 95% CI: 60–70) and “labeling” (n=109 in 603 preparations, 18% error rate; 95% CI: 15–21). In the NICU/PICU, most errors were related to uniform mixing (n=14 in 226 preparations, 6.2% error rate; 95% CI: 3.1–9.3) and the infusion rate (n=9 in 281 preparations, 3.2% error rate; 95% CI: 1.1–5.3) (). Results of the multivariate generalized linear mixed model showed a significant interaction between the “preparation type” and “ward” on the occurrence of an error (P=0.0456). The “preparation types” differed significantly for the adult ICU, but not for the NICU/PICU, whereas the therapeutic drug class had no influence on the occurrence of an error in the multivariate model (P=0.149). Preparations for adult patients of the LCD type were more often associated with errors than the P (OR =2.7, 95% CI: 1.2–6.1, P=0.012) and LC (OR =1.8, 95% CI: 1.2–2.7, P=0.002) type (). The results for the NICU/PICU did not show a significant influence of the “preparation type” () on the occurrence of an error.
Figure 2 Comparison of the preparation types (P, LC, and LCD) with regard to the occurrence of an error in the adult ICU and NICU/PICU.
Abbreviations: CI, confidence interval; ICU, intensive care unit; LC, liquid concentrate into syringe; LCD, liquid concentrate with diluent into syringe or infusion bag; NICU, neonatal intensive care unit; P, powder in a glass vial that must be reconstituted and diluted if necessary; PICU, pediatric intensive care unit.
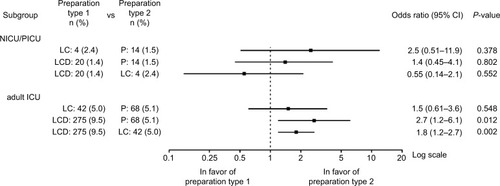
Table 3 Frequencies of error categories
Discussion
The error rates in our studies for the preparation and administration of intravenous drugs for an adult ICU and NICU/PICU were 7.6% and 1.5%. It is difficult to compare our results with other studies because they were performed in different settings (medical discipline and type of ward) with differences in the methods and definitions.
The results of studies in adult patients for all types of medication showed error rates for preparations with at least one error ranging from 3.3% to 44.6%.Citation3,Citation4,Citation23–Citation25 Within these studies, intravenous medication often has much higher error rates than other types of medications. Nguyen et al reported an error rate of 72.2% in intravenous vs 11.8% in oral preparations.Citation3 Studies regarding the preparation and administration of intravenous drugs alone showed error rates as high as 48%–97%.Citation5,Citation6,Citation9 Our results for the error rate in the adult ICU (56%) for preparations with at least one error divided by the total number of preparations fall well within the lower range.
For the pediatric patient group, we found no studies on intravenous drug preparations alone. The studies by Chedoe et al and Chua et al on all types of medication showed that the intravenous route contributed significantly to the rate of drug administration errors.Citation18,Citation19 Compared with studies in children, which include the preparation and administration of all types of medications, our error rate of 13% is still in the lower range of 8%–62.7%.Citation8,Citation14–Citation19
Most errors in our study in the adult ICU and NICU/PICU occurred in the category “uniform mixing” (59% and 37%). “Insufficient mixing of two solution” means an ME. Relating to our local hospital guidelines, the sufficient mixing is defined as shaking at least three times. Sufficient mixing is necessary for a homogeneous distribution of the drug in the diluent and consequently for a uniform dosing. This is particularly important for continuous infusions with an infusion pump. It is difficult to compare this result with those in previous studies because different definitions for preparation errors were used. “Uniform mixing” is often part of the category “incorrect drug preparation” without differentiating between the individual preparation steps.Citation6,Citation8 Cousins et al reported a 79% error rate for preparations that were not mixed properly in a German hospital.Citation7 In a study by Chedoe et al, “not mixed” was the third most frequent error category in the pre- and postintervention period.
The second error group for adult patients was “labeling” (18%). To increase the safety in the administration process, national and international organizations and institutions recommended standardized colored syringe drug labeling according to the International Organization for Standardization standard 26825.Citation26,Citation27 These labels were already used in the two ICUs before conducting the study. Nevertheless, there is still a lack of some preprinted labels, especially for anti-infectives. In a study by Cousins et al, the name of the drug was missing in 19% of preparations, and the dose was missing in 29% of preparations.Citation7 Despite available standardized drug labels, nearly one-third of labeling errors in our study (29%) concerned the drug propofol. We assume that the nurses may have omitted the labels with the thought that the characteristic lipid emulsion of propofol could make labeling redundant.
The second most frequent error category in the NICU/PICU was the “infusion rate”. All nine errors concerned a lower infusion rate with >5% deviation from the SMPC. This is explained by the fact that most intravenous infusions in our NICU/PICU are given short infusions of either 30 or 60 minutes. Analgesics are usually given faster, especially in cases of acute pain, to achieve a faster onset of action. The incidents were classified as errors because they meet the error criteria defined in this study. However, it is debatable whether they constitute an error in a wider medical sense. Other studies also reported administration errors that were characterized by rapidly administered bolus doses.Citation7,Citation28
Multivariate analysis showed that the type of preparation had a significant influence on the occurrence of an error in the adult ICU. The preparation type “liquid concentrate with diluent into syringe or infusion bag” was more often associated with an error than the other types of preparations (“powder in a glass vial that must be reconstituted and diluted if necessary” and “liquid concentrate into syringe”). One reason could be the twofold dilution in this type of preparation. The therapeutic drug class had no influence on the occurrence of an error in both ICUs.
Apart from the preparation type, the nurse–patient ratio, the number of different drugs, and the place of drug preparation may influence the error rate. In our adult ICU, the number of patients per nurse was on average higher than in the NICU/PICU (1.9 vs 1.4 patients per nurse). Studies showed that the occurrence of MEs was associated with the number of patients per nurse.Citation10,Citation24 Additionally, the number of different drugs in the observation period was much higher in the adult ICU than in the NICU/PICU (64 vs 45 drugs). These factors may explain the lower error rate in our pediatric patient group. Nevertheless, the preparation of intravenous drugs for pediatric patients typically requires more calculation and dilution steps, which increases the risk of error. In addition to human and organizational factors, the environment has a fundamental role in the management of drug therapy. Environmental factors include noises, interruptions, and disorder.Citation29 Drug preparation in the adult ICU was performed on a dedicated bedside table on the ward, while the preparation in the NICU/PICU was performed in a separate room with an LAF. Both settings were affected by interruptions and the lack of preparation space. Strategies to reduce interruptions and distractions are needed.
The results of our studies allow for the development of interventions to improve our preparation and administration process. Taxis and Barber showed that one cause of MEs is lack of knowledge of preparation and administration procedures.Citation28 Studies demonstrated that nurse education is one type of intervention to reduce MEs.Citation18,Citation30,Citation31 Providing nurse training and information about the most frequent errors, “uniform mixing”, “labeling”, and “infusion rate”, in our study may help to reduce these error types. In a study by Chua et al, an intervention between two observation periods showed a reduction in the administration errors from 44.3% to 28.6%.Citation19 The intervention involved a presentation for the nursing staff that involved sharing the error results of the first observation period. The intervention increased awareness of preparation and administration errors.
Another possible strategy is the preparation of ready-to-use syringes in the pharmacy. De Giorgi et al showed that ready-to-use syringes have a good cost–efficacy ratio as a safety tool for the preparation and administration processes.Citation32 Another study found that prefilled syringes are more expensive than ampules, but prefilled syringes could reduce MEs.Citation2,Citation33
Limitations
Within the last years, a CIRS was introduced in both wards. Errors associated with the preparation and administration of drugs were not recorded during our study period. In the time period after our study until 2016, recorded errors in the CIRS resulted in an implementation of the four-eyes principle during the preparation of drugs by two nurses in all neonatal and pediatric wards. Incident report review like CIRS is another type of method to detect medications errors. However, its detection rate is lower than that of observational studies.Citation34 Nevertheless, these implemented measures could have influenced the error rate within the last 5 years. Presenting of CIRS reports could increase the awareness of preparation and administration errors in both wards and therefore reducing the error rate. Additionally, the four-eyes principle could decrease the error rate in the NICU/PICU. Regardless of the implemented measures within the last 5 years, the resulting error rates of our study revealed the processes that are most error prone during the preparation and administration of intravenous drugs in our study. These results allow developing interventions to improve these error prone processes.
The two ICUs in which the studies were conducted are difficult to compare. Both wards differ regarding the patient characteristics, sample size, medication, and structural and organizational setting.
We only analyzed the preparation and administration process of intravenous drugs. Further studies are needed to evaluate the preparation and administration of other types of medication as well as the prescribing, transcribing, and dispensing process with the aim to improve medication safety.
We did not judge the clinical relevance of each error. Most errors likely will not cause severe patient harm. To assess the severity of each error, an independent expert panel of physicians, pharmacists, and nurses is needed.Citation3
We chose the disguised observation technique in our study. This method gives more reliable and objective results than spontaneous reporting or chart review, but it is time-consuming.Citation34 One disadvantage of this method is the influence on the nurses’ behavior (Hawthorne effect).Citation35 The error rate could increase if the observer caused nervousness among the nurses or the error rate could decrease if nurses were more watchful during the observation. Additionally, the observers’ behavior could influence the nurses too. A discrete and nonjudgmental behavior has less influence on the nurses. This would play an important role, if the observer decided to intervene to avoid an error, which could result into a serious adverse event. Although there might be a small effect on the nurses’ behavior, studies have shown that the observer does not have a significant influence on the error rate.Citation34–Citation36
The two observers could not be on the wards at all times and could not observe two preparations at the same time; therefore, some preparations were likely missed. Furthermore, we observed the wards during time periods when most medications were prepared, including the time periods with the highest workload for the nurses, which could increase the error rate. Both observers had the same standardized data collection form to ensure that the same error definition was applied. They conducted a pilot study to achieve familiarity with the preparation and administration processes. This approach resulted in a high accordance in the judgment of errors between these two observers. Nevertheless, there might be interobserver variability but the influence on the error rate is rather low.
Conclusion
We found that the type of preparation had a significant influence on the occurrence of an error in the adult ICU. Preparations with more than one dilution step were more often associated with errors than other types of preparations. In both wards, the most erroneous ME category was “uniform mixing”. Nurse training may be a feasible intervention to reduce errors. Additionally, the preparation of prefilled syringes in the pharmacy and improvements in the nurse– patient ratio and preparation location might reduce the error rate and thus improve the quality and safety of drug therapy.
Author contributions
TH designed and conducted the analysis. She analyzed and interpreted the data and drafted the first manuscript. EvdL conducted the analysis. She interpreted parts of the data and reviewed the manuscript. MS assisted with the analysis and interpretation of the data and revised the manuscript. CF interpreted the data while conducting the statistical tests and reviewed the manuscript. TO contributed to the conception of the analysis and reviewed the manuscript. GM contributed to the conception of the analysis and reviewed the manuscript. AE contributed to the conception and interpretation of the analysis and reviewed the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Abbreviations
| ATC | = | Anatomical Therapeutic Chemical |
| CI | = | confidence interval |
| CIRS | = | critical incidence reporting system |
| CPOE | = | computerized physician order entry |
| ICCA | = | IntelliSpace Critical Care and Anesthesia |
| ICU | = | intensive care unit |
| LAF | = | laminar air flow |
| LC | = | liquid concentrate into syringe |
| LCD | = | liquid concentrate with diluent into syringe or infusion bag |
| ME | = | medication error |
| NCC MERP | = | National Coordinating Council for Medication Error Reporting and Prevention |
| NICU | = | neonatal intensive care unit |
| P | = | powder in a glass vial that must be reconstituted and diluted if necessary |
| PICU | = | pediatric intensive care unit |
| SMPC | = | summary of product characteristics |
Acknowledgments
We thank Julia Amkreutz for thorough proofreading.
Disclosure
No benefits in the form of an honorarium, grant, or other form of payment contributed to the manuscript. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest and report no conflicts of interest in this work.
References
- National Coordinating Council for Medication Error Reporting and PreventionAbout medication errors Available from: http://www.nccmerp.org/about-medication-errorsAccessed August 19, 2018
- AdapaRMManiVMurrayLJErrors during the preparation of drug infusions: a randomized controlled trialBr J Anaesth2012109572973422850220
- NguyenHTNguyenTDvan den HeuvelERHaaijer-RuskampFMTaxisKMedication errors in Vietnamese hospitals: prevalence, potential outcome and associated factorsPLoS One2015109e013828426383873
- ChuaSSTeaMHRahmanMHAn observational study of drug administration errors in a Malaysian Hospital (study of drug administration errors)J Clin Pharm Ther200934221522319250142
- TaxisKBarberNIncidence and severity of intravenous drug errors in a German hospitalEur J Clin Pharmacol2004591181581714586530
- OngWMSubasyiniSMedication errors in intravenous drug preparation and administrationMed J Malaysia2013681525723466768
- CousinsDHSabatierBBegueDSchmittCHoppe-TichyTMedication errors in intravenous drug preparation and administration: a multicentre audit in the UK, Germany and FranceQual Saf Health Care200514319019515933316
- ChuaSSChuaHMOmarADrug administration errors in paediatric wards: a direct observation approachEur J Pediatr2010169560361119823870
- WestbrookJIRobMIWoodsAParryDErrors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experienceBMJ Qual Saf2011201210271034
- ValentinACapuzzoMGuidetBSentinel Events Evaluation (SEE) Study InvestigatorsErrors in administration of parenteral drugs in intensive care units: multinational prospective studyBMJ2009338b81419282436
- ConroySAssociation between licence status and medication errorsArch Dis Child201196330530621131639
- WongICWongLYCranswickNEMinimising medication errors in childrenArch Dis Child200994216116418829622
- ParshuramCSToTSetoWTropeAKorenGLaupacisASystematic evaluation of errors occurring during the preparation of intravenous medicationCMAJ20081781424818166730
- ProtSFontanJEAlbertiCDrug administration errors and their determinants in pediatric in-patientsInt J Qual Health Care200517538138916115809
- OzkanSKocamanGOzturkCSerenSFrequency of pediatric medication administration errors and contributing factorsJ Nurs Care Qual201126213614321135709
- RishoejRMAlmarsdóttirABThybo ChristesenHHallasJJuel KjeldsenLIdentifying and assessing potential harm of medication errors and potentially unsafe medication practices in paediatric hospital settings: a field studyTher Adv Drug Saf20189950952230181859
- BarakiZAbayMTsegayLGerenseaHKebedeATeklayHMedication administration error and contributing factors among pediatric inpatient in public hospitals of Tigray, Northern EthiopiaBMC Pediatr201818132130305080
- ChedoeIMolendijkHHospesWVan den HeuvelERTaxisKThe effect of a multifaceted educational intervention on medication preparation and administration errors in neonatal intensive careArch Dis Child Fetal Neonatal Ed2012976F449F45522491014
- ChuaSSChooSMSulaimanCZOmarAThongMKEffects of sharing information on drug administration errors in pediatric wards: a pre-post intervention studyTher Clin Risk Manag20171334535328356748
- American Society of Hospital PharmacistsASHP guidelines on preventing medication errors in hospitalsAm J Hosp Pharm19935023053148480790
- ScheffeHA method for judging all contrasts in the analysis of varianceBiometrika1953401–287104
- R: Development Core Team A Language and Environment for Statistical Computing [computer program]Vienna, AustriaR Foundation for Statistical Computing2008
- CalabreseADErstadBLBrandlKBarlettaJFKaneSLShermanDSMedication administration errors in adult patients in the ICUIntensive Care Med200127101592159811685299
- BerdotSSabatierBGillaizeauFCarubaTPrognonPDurieuxPEvaluation of drug administration errors in a teaching hospitalBMC Health Serv Res2012126022409837
- van den BemtPMFijnRvan der VoortPHGossenAAEgbertsTCBrouwersJRFrequency and determinants of drug administration errors in the intensive care unitCrit Care Med200230484685011940757
- KaufmannJWolfARBeckeKLaschatMWapplerFEngelhardtTDrug safety in paediatric anaesthesiaBr J Anaesth2017118567067928510742
- MerryAFShippDHLowingerJSThe contribution of labelling to safe medication administration in anaesthetic practiceBest Pract Res Clin Anaesthesiol201125214515921550540
- TaxisKBarberNCauses of intravenous medication errors: an ethnographic studyQual Saf Health Care200312534334714532365
- Di SimoneETartagliniDFioriniSPetriglieriSPloccoCdi MuzioMMedication errors in intensive care units: nurses’ training needsEmerg Nurse2016244242927384804
- NguyenHTPhamHTVoDKThe effect of a clinical pharmacist-led training programme on intravenous medication errors: a controlled before and after studyBMJ Qual Saf2014234319324
- AbbasinazariMZareh-ToranposhtiSHassaniASistanizadMAzizianHPanahiYThe effect of information provision on reduction of errors in intravenous drug preparation and administration by nurses in ICU and surgical wardsActa Med Iran2012501177177723292630
- De GiorgiIFonzo-ChristeCCingriaLRisk and pharmacoeconomic analyses of the injectable medication process in the paediatric and neonatal intensive care unitsInt J Qual Health Care201022317017820382659
- BenhamouDPiriouVDe VaumasCReady-to-use pre-filled syringes of atropine for anaesthesia care in French hospitals-a budget impact analysisAnaesth Crit Care Pain Med201736211512127481691
- AllanELBarkerKNFundamentals of medication error researchAm J Hosp Pharm19904735555712180287
- DeanBBarberNValidity and reliability of observational methods for studying medication administration errorsAm J Health Syst Pharm2001581545911194136
- FlynnEABarkerKNPepperGABatesDWMikealRLComparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilitiesAm J Health Syst Pharm200259543644611887410
