Abstract
One-third of patients with epilepsy continue to have seizures despite current treatments, indicating the need for better antiseizure medications with novel mechanisms of action. Ezogabine (retigabine) has recently been approved for adjunctive treatment of partial-onset seizures in adult patients with epilepsy. Ezogabine utilizes a novel mechanism of action, involving activation of specific potassium channels. The most common side effects of ezogabine are shared by most antiseizure medications and primarily consist of central nervous system (CNS) symptoms, such as somnolence, dizziness, confusion, and fatigue. In addition, a small percentage of patients on ezogabine experience a unique adverse effect affecting the bladder, which results in urinary hesitancy; thus, patients on ezogabine should be monitored carefully for potential urological symptoms. Overall, ezogabine appears to be well tolerated and represents a reasonable new option for treating patients with intractable epilepsy.
Introduction
Epilepsy is a common disease with a cumulative lifetime risk of at least 3%.Citation1 It is associated with significant morbidity and mortality, as well as decreased quality of life in a variety of social, educational, and vocational measures.Citation2–Citation4 Specifically, mortality has been demonstrated to be up to threefold higher in developed countries.Citation5 Further, adults with seizures are at risk for lower levels of education, higher rates of unemployment, and psychological and physical ailments.Citation6 A number of new antiseizure medications have been developed and marketed in the last two decades. Despite these new therapies, medically intractable epilepsy, defined as persistent seizures after an adequate trial of two appropriate antiseizure medications, continues to occur in approximately one-third of cases.Citation7,Citation8 This makes the development of antiseizure medications with novel mechanisms of action an important goal to further broaden the possible success in intractable epilepsy of various etiologies. However, with novel mechanisms of action there is a risk of unique side effects.
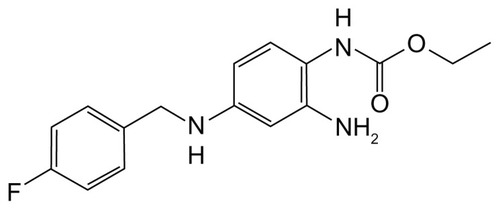
One of these new antiseizure medications with a novel mechanism of action is ezogabine (EZG). EZG is an ethyl N-(2-amino-4-{[(4-fluorophenyl)methyl]amino} phenyl) () and is known by the international nonproprietary name of “retigabine” in Europe and most of the world. This drug was recently approved by the European Medicines Agency and the US Food and Drug Administration (FDA) for adjunctive treatment of partial-onset seizures in adults. It appears to work by a unique mechanism of action compared with other currently available antiepileptic drugs. A number of other recent reviews have also highlighted different aspects of EZG,Citation9–Citation13 but this review focuses especially on the adverse effects of EZG.
Mechanism of action
First developed through the National Institutes of Health Antiepileptic Drug Development program after the identification of a structural analog’s (flupirtine) efficacy against seizures, EZG’s mechanism of action is novel among currently available antiseizure medications.Citation14 EZG exerts its effects on the Kv7 family of potassium channelsCitation15,Citation16 by binding to the cytoplasmic aspects of the S5 and S6 parts of the activation gate of these potassium channels involved in the M-current.Citation17,Citation18 In doing so, EZG increases rates of channel opening, maintains potassium channels in the open state for longer periods of time, and alters the voltage characteristics of the cell, making channel opening more likely.Citation16
The channels bound by EZG consist of the Kv7 homoand heteromeric subunits KCNQ2–5.Citation15,Citation16,Citation19 EZG’s primary site of action is the KCNQ2/3 heteromer,Citation15,Citation16 which is expressed in the nervous system and accounts for its antiseizure efficacy. There is no enhancement of the potassium currents mediated by the KCNQ1 channel subunit, which is found primarily in cardiac tissueCitation18 and also in the gastrointestinal system and brain.Citation20 However, KCNQ4 and KCNQ5 potassium channels are activated by EZG and may be found in cochlear hair cellsCitation21 or smooth muscle.Citation22 EZG causes relaxation of smooth muscle in the bladder, which probably accounts for the adverse effects of EZG on urinary function.Citation23
Metabolism–drug interactions
EZG is absorbed rapidly after oral administration, with a peak plasma concentration at 1.5 hours after ingestion.Citation24 EZG is metabolized primarily by acetylation and glucuronidation in the liver and is subsequently eliminated by renal excretion.Citation25,Citation26 Due to this dual metabolism, it is recommended that individuals with low creatinine clearance (<50 mL/min), undergoing hemodialysis, or with moderate to severe hepatic impairment start at a lower starting dose (50 mg/d) and titrate to a lower maximum dose (600 mg/d for renal failure or severe hepatic impairment; 750 mg/d for moderate hepatic impairment). In patients 66–81 years of age, it has been noted that EZG clearance was diminished compared with younger study participants (18–40 years of age) and the authors attributed this to the normal decrease in creatinine clearance that occurs with age. No side effects from this difference were noted.Citation27
As in vitro studies have demonstrated little or no potential for EZG to inhibit or induce the major cytochrome,Citation28 P450 isoenzymes, minimal drug interactions of clinical significance have been reported. EZG does not interact with oral contraceptive agents.Citation29 Moreover, it seems to be well tolerated in individuals taking other antiseizure medications as well, with minimal direct interactions. While EZG and lamotrigine had reciprocal effects on renal clearance, both drugs were tolerated equally well alone and in combination, thus these interactions were not thought clinically significant.Citation30 No clinically significant interactions have been found between EZG and propofol, valproate, or imipramineCitation26 and an in vivo study has demonstrated lack of interaction between phenobarbitone and EZG.Citation31 In clinical studies, no significant pharmacokinetic effect has been seen on phenytoin, carbamazepine, valproic acid or topiramate.Citation32 Overall, EZG has few clinically significant interactions with other pharmaceutical agents.
Efficacy
Three double-blind placebo-controlled multicenter trials have taken place investigating the efficacy of EZB in adults with medically intractable partial-onset epilepsy as add-on therapy in combination with other antiepileptic medications.Citation33–Citation35 A recent paper has reported an integrated analysis of these three controlled trials.Citation36 After pooling data from the three studies, 1240 patients were included, with 813 patients randomized to EZG and 427 to placebo. In all trials, after an initial 8-week baseline phase, patients were randomized to placebo or EZB (titrated to 600, 900, or 1200 mg/day, depending on the trial), followed by an 8–12-week maintenance phase. Two primary efficacy measures were used: (1) responder rate, defined as the percentage of patients experiencing a ≥50% reduction in seizure frequency compared with the baseline phase; and (2) the percent change in partial seizure frequency. A number of secondary efficacy endpoints were also assessed, including more specific categorization of seizure frequency reduction rates and the proportion of seizure-free days and seizure-free patients.
Analysis of the integrated data found statistically significant effects of EZB on both primary efficacy measures.Citation36 Responder rates (≥50% reduction in seizure frequency) were 35% and 45% for EZG at 600 and 900 mg/day, respectively, compared with 21% for placebo (P < 0.001) and 50% for EZG at 1200 mg/day, compared with 24% for placebo (P < 0.001). Average reduction in seizure frequency was 26%, 37%, and 39% for 600, 900, and 1200 mg/d EZG, respectively, all of which were statistically significantly greater than placebo (15%). Similar differences were observed in various secondary endpoints. For example, the proportion of patients experiencing a 50%–75% or ≥75% reduction in seizures showed a dose-dependent increase with EZG compared with placebo. At all doses, there was a significant increase in seizure-free days with EZG compared with placebo, although the effect was modest (81%–84% for EZG vs 78% for placebo). In addition, while in the individual trials there had been no statistically significant effect of EZG on the percentage of seizure-free patients, in the pooled analysis of EZG at 1200 mg/d, but not at 600 or 900 mg/d, there was a statistically significant increase in the proportion of seizure-free patients during the maintenance phase (15% with 1200 mg/d EZG vs 5% with placebo).
Subgroup analyses did not demonstrate any differences in the magnitude of the effect of EZG based on age (18–44 years vs >44 years), sex, race (white vs nonwhite), region (US vs non-US), number of baseline antiseizure medications, and seizure subtypes (simple partial, complex partial, secondary generalized). Overall, these randomized placebo-controlled trials demonstrated that EZG is effective as add-on therapy for adults with intractable partial-onset epilepsy. The magnitude of the effects of EZG on seizures is similar to most other new antiseizure medications used as adjunctive therapy for intractable epilepsy and only a small percentage of patients become seizure-free on EZG.
Adverse events
Over the course of the three major placebo-controlled trials,Citation33–Citation35 EZG was generally quite well tolerated. Based on the pooled analysis, adverse events that were considered severe were similar in the placebo (10%), EZG 600 mg/d (10%), and EZG 900 mg/d (12%) groups but were higher in the EZG 1200 mg/d group (20%).Citation36 All other adverse events were noted by investigators to be mild to moderate. Three deaths (0.7%) related to sudden death in epilepsy, injury, and respiratory failure occurred in the 427 patients on placebo, whereas only two deaths (0.2%) in the cumulative EZG groups due to sudden death in epilepsy and diabetic ketoacidosis occurred in the 813 patients. Discontinuation of the study due to adverse events occurred in 10%, 15%, 24%, and 28% of patients in the placebo, 600 mg/d, 900 mg/d, and 1200 mg/d groups, respectively.Citation36
Reasons for discontinuation of the study and the overall most common adverse events were generally central nervous system (CNS) related (). These adverse events occurred with increasing frequency as the dose of EZG was increased. The most common side effects included dizziness and somnolence and, to a lesser extent, confusion, fatigue, and asthenia.Citation33–Citation35 Porter et alCitation33 noted speech difficulties in no patients in the placebo arms and five (5%), twelve (12.6%), and 17 (16%) patients in the 600 mg/d, 900 mg/d, and 1200 mg/d arms, respectively.
Table 1 Adverse effects of ezogabine reported in at least 5% of patients with intractable partial seizures in placebo-controlled add-on clinical trials
EZG has been noted to decrease gastrointestinal smooth muscle contractility.Citation37,Citation38 Constipation was not mentioned in two studiesCitation33,Citation35 but occurred in three (2%) patients in the placebo arm and nine (5.9%) patients in the 1200 mg/d group French et al’s study.Citation34 Alterations in liver enzyme levels were noted rarely but were transient and did not require discontinuation from the studies.Citation33–Citation35 No changes in electrocardiography have been reported. Adverse events related to cardiac abnormalities were similar in the placebo (4%) and EZG (5%) groups.
While most of the reported side effects of EZG are similar to many other antiseizure medications in that they most commonly affect the CNS, EZG has one relatively unique and specific adverse effect, which is related to urinary function.Citation37 EZG had initially been noted to relax rat bladdersCitation39 as well as decrease bladder tension and contraction amplitude.Citation40 As a result of this basic science data, urinary adverse events were recorded during the placebo-controlled trials. In Brodie et al’s trial,Citation35 three patients were discharged from these trials for urinary symptoms, although the groups to which these patients were assigned were not delineated: one for nephritis and two for urinary hesitation. French et alCitation34 reported nine (5.9%) patients in the 1200 mg/d arm and one (0.7%) in the placebo arm with urinary hesitation and eight (5.2%) patients in the 1200 mg/d arm and two (1.3%) in the placebo arm with dysuria. In the pooled analysis, urinary or renal symptoms were reported in the EZG 1200 mg/d group (25%) almost twice as frequently as in the placebo (13%) group, although similar rates as in the placebo group were reported with 600 mg/d (14%) and 900 mg/d (13%).Citation35,Citation36 Other urinary symptoms and signs reported included urinary tract infections, polyuria, hematuria, proteinuria, and chromaturia. These adverse events were noted to diminish with time on the medication and were noted to be mild to moderate. Very few cases led to discontinuation (1% for both EZG and placebo). Due to the urinary symptoms, the FDA has required post-marketing analysis and recording of urinary symptoms.
Some data from the open-label extension trial have now been published in a recent review.Citation37 There continues to be no evidence of direct renal adverse events, although one participant did have reversible renal failure related to obstructive uropathy.Citation37 Of note, four participants have now been reported with nephrolithiasis in the 1200 mg/d group.Citation37 However, based on the overall incidence of nephrolithiasis in the USA and EZG’s mechanism of action, it is not felt that ezogabine is an independent risk factor for nephrolithiasis at this time. Urinary crystals with an appearance similar to bilirubin have been reported in some participants.Citation37 This could result in an abnormal urinalysis result but does not appear to be related to a risk for nephrolithiasis. Overall, it would seem prudent to monitor any patients on EZG for urologic symptoms and be cautious with those with risk factors for urinary obstruction.
No data are available on the safety of EZG use during pregnancy. As such, EZG is a pregnancy class C drug. In addition, there is a lack of established safety data on infants of breastfeeding mothers on EZG.
Other clinical applications
A variety of additional clinical applications beyond epilepsy have been proposed for EZG. These include in neuromyotonia,Citation41 neuropathic pain,Citation42,Citation43 mania, and addiction to psychostimulants.Citation44 Other rodent models have demonstrated a possible anti-dystonic effect.Citation45 An in vitro study has demonstrated a possible anxiolytic effect of EZG.Citation46 However, these other applications are still under investigation.
Discussion and conclusion
Epilepsy, despite several new medications that have been developed in the last few decades, continues to be refractory to medications in one-third of patients and can be a significant cause of morbidity and mortality. EZG is a new antiseizure drug with a novel mechanism of action. It is a potassium-channel activator primarily active in the CNS, with alternate sites of action in the urinary bladder, gastrointestinal smooth muscle, and vascular smooth muscle.Citation47,Citation48
EZG has proven efficacy and is approved both in the USA and Europe for treatment of adults with intractable partial-onset epilepsy. Given its novel mechanism of action, there is hope that EZG may be more effective for some patients with intractable epilepsy than other available antiseizure medications, although, overall, the efficacy data are fairly comparable to studies of other drugs in intractable patients. Early data demonstrate minimal interaction with medications other than lamotrigine and those interactions were deemed to be clinically insignificant.Citation30
EZG is generally well tolerated and is rarely discontinued due to adverse events. The number of reported adverse events is also likely to be influenced by the forced fast titration schedule deemed necessary by the authors of the placebo-controlled trials. Most of these adverse events were CNS related, such as somnolence and fatigue.
However, EZG has a novel adverse effect on the urinary tract – specifically, on the urinary bladder – both in animal models and in human trials. Urinary or secondary renal adverse effects are collectively relatively common, occurring in about 25% of patients in the highest-dose EZG group.Citation36,Citation37 Symptoms from urinary adverse events were usually noted to be minor or moderate, sometimes only involving laboratory abnormalities on urinalysis and rarely leading to discontinuation from the trial. However, urinary hesitancy and retention can be clinically significant problems. Thus, due to this novel side effect and the lack of a significant quantity of long-term data as to the severity and prevalence of urinary adverse events, the FDA has recommended a risk evaluation and mitigation strategy to further track the use of EZG in this regard. Overall, no long-term data currently exist as to the safety of EZG.
Disclosure
The authors declare no conflicts of interest in this work.
References
- HesdorfferDCLogroscinoGBennEKKatriNCascinoGHauserWAEstimating risk for developing epilepsy: a population-based study in Rochester, MinnesotaNeurology2011761232721205691
- NadkarniJJainADwivediRQuality of life in children with epilepsyAnn Indian Acad Neurol201114427928222346017
- BacaCBVickreyBGVassarSDBergATSeizure recency and quality of life in adolescents with childhood-onset epilepsyEpilepsy Behav2012231475122134098
- SillanpääMShinnarSLong-term mortality in childhood-onset epilepsyN Engl J Med2010363262522252921175314
- ForsgrenLHauserWAOlafssonESanderJWSilanpääMTomsonTMortality of epilepsy in developed countries: a reviewEpilepsia200546Suppl 11182716393174
- StrineTWKobauRChapmanDPThurmanDJPricePBalluzLSPsychological distress, comorbidities, and health behaviors among US adults with seizures: results from the 2002 National Health Interview SurveyEpilepsia20054671133113916026567
- ElgerCESchmidtDModern management of epilepsy: a practical approachEpilepsy Behav200812450153918314396
- KwanPBrodieMJEarly identification of refractory epilepsyN Engl J Med2000342531431910660394
- RheimsSRyvlinPRetigabine for partial onset seizuresExpert Rev Neurother201212550951722550979
- LargeCHSokaiDMNehligAThe spectrum of anticonvulsant efficacy of retigabine (ezogabine) in animal models: implications for clinical useEpilepsia201253342543622221318
- RejdakKLuszczkiJJBłaszczykBChwedorowiczRCzuczwarSJClinical utility of adjunctive retigabine in partial onset seizure in adultsTher Clin Risk Manag2012871422298949
- StafstromCEGripponSKirkpatrickPEzogabine (retigabine)Nat Rev Drug Discov2011101072973021959281
- WeisenbergJLWongMProfile of ezogabine (retigabine) and its potential as an adjunctive treatment for patients with partial-onset seizuresNeuropsychiatr Dis Treat2011740941421792307
- RostockAToberCRundfeldtCD-23129: a new anticonvulsant with a broad spectrum activity in animal models of epileptic seizuresEpilepsy Res19962332112238739124
- WickendenADYuWZouAJeglaTWagonerPKRetigabine, a novel anticonvulsant, enhances activation of KCNQ2/Q3 potassium channelsMol Pharmacol200058359160010953053
- MainMJCryanJEDupereJRCoxBClareJJBurbidgeSAModulation of KCNQ2/3 potassium channels by the novel anticonvulsant retigabineMol Pharmacol200058225326210908292
- WuttkeTVSeebohmGBailSMaljevicSLercheHThe new anticonvulsant retigabine favors voltage-dependent opening of the Kv7.2 (KCNQ2) channel by binding to its activation gateMol Pharmacol20056741009101715662042
- RundfeldtCNetzerRThe novel anticonvulsant retigabine activates M-currents in Chinese hamster ovary-cells tranfected with human KCNQ2/3 subunitsNeurosci Lett2000282102737610713399
- TatulianLDelmasPAbogadieFCBrownDAActivation of expressed KCNQ potassium currents and native neuronal M-type potassium currents by the anti-convulsant drug retigabineJ Neurosci200121155535554511466425
- JentschTJNeuronal KCNQ potassium channels: physiology and role in diseaseNat Rev Neurosci200011213011252765
- KharkovetsTDedekKMaierHMice with altered KCNQ4 K+ channels implicate sensory outer hair cells in human progressive deafnessEMBO J200625364265216437162
- GreenwoodIAOhyaSNew tricks for old dogs: KCNQ expression and role in smooth muscleBr J Pharmacol200915681196120319751313
- JeppsTAGreenwoodIAMoffattJDSandersKMOhyaSMolecular and functional characterization of Kv7 K+ channel in murine gastrointestinal smooth musclesAm J Physiol Gastrointest Liver Physiol20092971G107G11519389803
- FerronGMPaulJFruncilloRMultiple-dose, linear, dose-proportional pharmacokinetics of retigabine in healthy volunteersJ Clin Pharmacol200242217518211831540
- McNeillyRJTorchinCDAndersonLWKapetanovicIMKupferbergHJStrongJMIn vitro glucuronidation of D-23129, a novel anticonvulsant, by human liver microsomes and liver slicesXenobiotica19972754314419179986
- BorlakJGasparicALocherMSchupkeHHermannRN-Glucuronidation of the antiepileptic drug retigabine: results from studies with human volunteers, heterologously expressed human UGTs, human liver, kidney, and liver microsomal membranes of Crigler-Najjar type IIMetabolism20065671172116713428
- HermannRFerronGMErbKEffects of age and sex on the disposition of retigabineClin Pharmacol Ther2003731617012545144
- HempelRSchupkeHMcNeillyPJMetabolism of retigabine (D-23129), a novel anticonvulsantDrug Metab Dispos199927561362210220491
- FerronGMPaulJRichardsLGetsyJTroySRetigabine does not alter the pharmacokinetics of a low dose oral contraceptive in womenNeurology200156Suppl 3A335A336
- HermannRKnebelNGNiebchGRichardsLBorlakJLocherMPharmacokinetic interaction between retigabine and lamotrigine in healthy subjectsEur J Clin Pharmacol2003581279580212698305
- FerronGMPatatAParksVRolanPTroySMLack of pharmacokinetic interaction between retigabine and phenobarbitone at steady-state in healthy subjectsBr J Clin Pharmacol2003561394512848774
- BialerMJohannessenSILevyRHPeruccaETomsonTWhiteHSProgress report on new antiepileptic drugs: a summary of the Ninth Eilat Conference (EILAT IX)Epilepsy Res200983114319008076
- PorterRJPartiotASachdeoRNohriaVAlvesWMRandomized, multicenter, dose-ranging trial of retigabine for partial-onset seizuresNeurology200768151197120417420403
- FrenchJAAbou-KhalilBWLeroyRFRESTORE 1/Study 301 InvestigatorsRandomized double-blind, placebo-controlled trial of ezogabine (retigabine) in partial epilepsyNeurology201176181555156321451152
- BrodieMJLercheHGil-NagelARESTORE 2 Study GroupEfficacy and safety of adjunctive ezogabine (retigabine) in refractory partial epilepsyNeurology201075201817182420944074
- PorterRJBurdetteDEGil-NagelARetigabine as adjunctive therapy in adults with partial-onset seizures: integrated analysis of three pivotal controlled trialsEpilepsy Res Epub April 16, 2012
- BrickelNGandhiPVanlandinghamKHammondJDerossettSThe urinary safety profile and secondary renal effects of retigabine (ezogabine): a first-in-class antiepileptic drug that targets KCNQ (K(v) 7) potassium channelsEpilepsia201253460661222428574
- IpavecaVMartireaMBarresebVTaglialatelaMCurròDKV7 channels regulate muscle tone and nonadrenergic noncholinergic relaxation of the rat gastric fundusPharmacol Res201164439740921740972
- StrengTChristophTAnderssonKEUrodynamic effects of the K+ channel (KCNQ) opener retigabine in freely moving, conscious ratsJ Urol20041725 Pt 12054205815540788
- RodeFSvaløJSheykhzadeMChristianLRønnLCFunctional effects of the KCNQ modulators retigabine and XE991 in the rat urinary bladderEur J Pharmacol20106381–312112720385123
- ShillitoPMolenaarPCVincentAAcquired neuromyotonia: evidence for autoantibodies directed against K+ channels of peripheral nervesAnn Neurol19953857147227486862
- Blackburn-MunroGJensenBSThe anticonvulsant retigabine attenuates nociceptive behaviors in rat models of persistent and neuropathic painEur J Pharmacol20034602–310911612559370
- MunroGErichsenHKMirzaNRPharmacological comparison of anticonvulsant drugs in animal models of persistent pain and anxietyNeuropharmacology200753560961817714743
- HansenHHAndreasenJTWeikopPMirzaMScheel-KrügerJMikkelsenJDThe neuronal KCNQ channel opener retigabine inhibits locomotor activity and reduces forebrain excitatory responses to the psychostimulants cocaine, methylphenidate and phencyclidineEur J Pharmacol20075701–3778817628530
- RichterASanderSERundfeltCAntidystonic effects of Kv7 (KCNQ) channel openers in the dtsz mutant, an animal model of primary paroxysmal dystoniaBr J Pharmacol2006149674775317016514
- KorsgaardMPHartzBPBrownWDAhringPKStrøbaekDMirzaNRAnxiolytic effects of Maxipost (BMS-204352) and retigabine via activation of neuronal Kv7 channelsJ Pharmacol Exp Ther2005314128229215814569
- NgFLDavisAJJeppsTAExpression and function of the K+ channel KCNQ genes in human arteriesBr J Pharmacol20111621425320840535
- JoshiSSedivyVHodycDHergetJGurneyAMKCNQ modulators reveal a key role for KCNQ potassium channels in regulating the tone of rat pulmonary artery smooth muscleJ Pharmacol Exp Ther2009329136837619151245