Abstract
Background
Our objective was to determine the quality of literature in costing of the economic burden of patient safety.
Methods
We selected 15 types of patient safety targets for our systematic review. We searched the literature published between 2000 and 2010 using the following terms: “costs and cost analysis,” “cost-effectiveness,” “cost,” and “financial management, hospital.” We appraised the methodologic quality of potentially relevant studies using standard economic methods. We recorded results in the original currency, adjusted for inflation, and then converted to 2010 US dollars for comparative purposes (2010 US$1.00 = 2010 €0.76). The quality of each costing study per patient safety target was also evaluated.
Results
We screened 1948 abstracts, and identified 158 potentially eligible studies, of which only 61 (39%) reported any costing methodology. In these 61 studies, we found wide estimates of the attributable costs of patient safety events ranging from $2830 to $10,074. In general hospital populations, the cost per case of hospital-acquired infection ranged from $2132 to $15,018. Nosocomial bloodstream infection was associated with costs ranging from $2604 to $22,414.
Conclusion
There are wide variations in the estimates of economic burden due to differences in study methods and methodologic quality. Greater attention to methodologic standards for economic evaluations in patient safety is needed.
Introduction
Patient safety has received considerable public, professional, political, and scientific attention over the past decade. Although the human burden associated with adverse events is well established, the economic cost of patient safety has received less attention. Despite the substantial effort that has been expended to develop and implement safety improvements, there is uncertainty about both the economic impact of unsafe care and the improvement strategies that offer the best value. Significant resources have been expended across the world to reduce patient safety events through interventions, without clear improvements.Citation1,Citation2
A fuller understanding of the economic burden of patient safety may inform health policy, health services research priorities, safety improvement priorities, and patient safety priorities. High quality data on economic burden of a condition are an essential component of comparative economic analyses such as cost-effectiveness analyses.
The objective of an economic burden study is to describe the economic impact of a patient safety target. These types of studies generally examine the overall cost of the condition to an environment (eg, acute care setting, society).
Economic burden studies should be based on rigorous analytical methods, be impartial and credible in the use of data, and be transparent for and accessible by the reader.Citation3 Economic burden studies are conducted using recognized frameworks which can be modified for specific target conditions. Citation4,Citation5 Drummond and Jefferson and Drummond et al constructed a checklist of economic parameters used worldwide. Citation6,Citation7 Economic burden studies should clearly outline the resource studies, the method for attributing costs to these resources, the method for measuring the resources used, the time frame for measuring the resources, and the economic perspective (hospital, third-party payer, or society) from which the resources were measured.
Our objective was to determine the quality of literature in costing of the economic burden of patient safety targets in the acute care environment.
Methods
We developed a list of patient safety targets based on prior systematic reviews,Citation8 and existing national and international safety initiatives.Citation9,Citation10 Patient safety targets were based on three characteristics: (1) a clinical outcome (eg, hospital-acquired methicillin-resistant Staphylococcus aureus [MRSA] infection) or a surrogate with an established link to a clinical outcome (eg, MRSA colonization); (2) high specificity as a measure of patient safety, as opposed to being a naturally occurring condition; and (3) a sufficiently long history of measuring this outcome in the literature, such that some studies on the economic burden could be expected.
Patient safety targets included: adverse events, adverse drug events, ventilator-associated pneumonia, nosocomial urinary tract infection, antibiotic-resistant organism colonization, antibiotic-resistant organism infection, catheter-associated bloodstream infection, nosocomial Clostridium difficile-associated disease, surgical site infection, nosocomial pressure ulcers, wrong site surgery, retained surgical foreign bodies, contrast-induced nephropathy, nosocomial venous thromboembolism, and nosocomial fall-related injuries. We also included six improvement strategies (hand hygiene, rapid response teams, bundles, check-lists, automatic stop orders and bar coding) to ensure that we obtained all relevant economic literature that may not be captured through searches based solely on patient safety targets.
We sought burden-of-illness or cost-of-illness studies. A search was performed using the MEDLINE database for articles published between 2000 and 2010 using the following search terms for costs: “costs and cost analysis” (Medical Subject Headings [MeSH]), “cost-effectiveness” (text word), “cost” (text word), and “financial management, hospital” (MeSH). We also searched the Agency for Healthcare Research and Quality Patient Safety Network (see http://psnet.ahrq.gov) using the term “cost.”
Reviews, editorials, and articles with no costing information in the abstract were excluded. One member of the study team (MK) excluded reviews, editorials, and articles with no costing information in the abstract. Two independent members of the study team (MK and EE) reviewed the remaining abstracts and obtained the full publication of any abstract considered potentially relevant by either member. Full publications of any abstracts considered potentially relevant were retrieved. Two investigators (EE and NM) independently evaluated each publication, using adapted relevant methodologic features (n = 21) as described by Drummond and Jefferson.Citation6 Each feature was arbitrarily scored one point, for a maximum score of 21. Features from the original list were excluded if they were not applicable to economic burden studies. If the two reviewer scores were within five points of one another, the higher score was taken. Otherwise, reviewers met to discuss and resolve discrepancies.
We report all cost data in 2010 United States dollars for comparative purposes between patient safety targets. The original year and currency is stated in the summary data. Each cost was first converted to US dollars of the same year as indicated in the publication using the Bank of Canada currency converter.Citation11 Then, each converted cost was inflated to 2010 US dollars using the United States Department of Labor Bureau of Labor Statistics inflation calculator.Citation12
Results
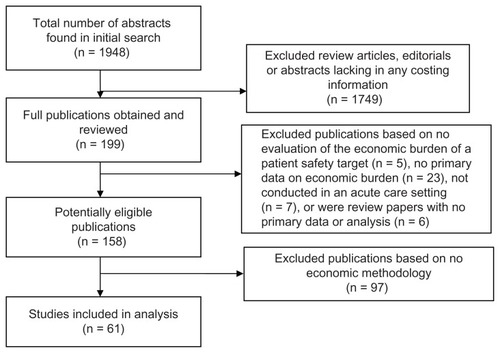
Our initial search yielded 1948 citations. We screened out 1749 abstracts that were review articles, editorials, or lacking in any costing information or results. We obtained and reviewed the remaining 199 publications. We excluded 41 publications for the following reasons: no evaluation of the economic burden of a patient safety target (n = 5), no primary data on economic burden (n = 23), not conducted in an acute care setting (n = 7) or were review papers with no primary data or analysis (n = 6). This left 158 potentially eligible publications. Ninety-seven (61%) of the 158 potentially eligible publications described no economic methodology despite reporting an estimate of economic burden and were excluded from further review ().
Methodologic quality
For the remaining 61 studies, the median methodologic feature score was 15/21 (mean 14.6 ± 21, range 9–20). All studies had essential methodologic features such as a statement of the research question, a statement of the economic importance of the research question, and a justification of the economic viewpoint. Fewer than 50% of these 61 studies reported productivity changes, discussed the relevance of productivity changes, provided details of inflation adjustments or currency conversions, or described any sensitivity analyses. Studies used different methods for identifying attributable cost, including propensity scores, case–controls, and regression analysis ( and ).
Table 1 Summary of studies of economic burden of patient safety targets in acute care (detailed summary of each study is in )
Table 2 Methodologic characteristics of studies of economic burden of patient safety events in acute care (n = 61)
Table 3 Detailed summary of systematic review
There was heterogeneity in study populations, resources incorporated, methods and results, so economic burden summary for all patient safety targets could not be calculated. We summarize the methodologic feature scores and range of results for each type of adverse event in . The maximum score was 21. We provide detailed summaries of each study organized by patient safety target ().
General studies of adverse events and adverse drug events
We identified eight studies of the economic burden of adverse events and adverse drug events published since 2000. Five of these studies used a retrospective cohort study design, and relied on regression analyses to determine the attributable costs. Of these, two articles broadly focused on any adverse event or hospital-acquired complication.Citation13,Citation14 An additional article evaluated the economic burden of a broad range of adverse events in patients with spinal cord injuries.Citation15 One article included five specific adverse events: medication errors, patient falls, urinary tract infection, pneumonia, and pressure ulcers.Citation16 Another article evaluated costs related only to surgical adverse events, but did not further define them.Citation17 The three remaining studies related to adverse events were either case seriesCitation18 or prospective cohorts with nested cases and controls.Citation19,Citation20 Two of these studies defined a case as any adverse eventsCitation19 or a case leading to a medical dispute.Citation18 One study specifically evaluated adverse drug events.Citation20
Costs attributable to adverse events were $4571Citation19 and $10,074Citation14 in two studies. In patients with spinal cord injury, the cost attributable to adverse events was $6258, but were significantly higher for specific complications; for example, procedural complications in these patients were associated with additional costs of $20,183.Citation15 The cost attributable to adverse drug events was $2830.Citation20 In another study, medication error in medical and surgical cases were associated with costs of $361 and $568, respectively.Citation16 Attributable length of stay related to adverse events ranged from 0.77 days to 32 days.Citation15,Citation19,Citation20 Three of the eight articles did not record length-of-stay data.Citation16–Citation18
Nosocomial infections (not otherwise specified)
We identified ten studies of the economic burden of general nosocomial infections not otherwise specified by type of infection. These included one prospective design, five retrospective cohort designs, three retrospective case control designs, and one decision model. Analytic methods included regression analysis, such as linear regression, multivariate regression, and ordinary least-squares regression analysis.
In general hospital populations, the cost per case of hospital-acquired infection ranged from $2132 to $15,018.Citation21–Citation27 Hospital-acquired infections cost $2910 in gastrectomy patientsCitation28 and $21,856Citation29 in neonates. The estimated costs of hospital-acquired infections over one fiscal year in New Zealand in medical patients were US$5,626,640 and surgical patients were US$4,803,046.Citation30
Surgical site infections
We found eight studies of the economic burden of surgical site infections. Study designs included prospective cohort (n = 1), retrospective cohorts (n = 3), retrospective case control (n = 2), and two nested case control designs. The average cost per case of surgical site infection in a general patient population was reported to be $1105,Citation22 $2604,Citation31 and $14,422Citation32 in three studies. In orthopedic patients, the median attributable cost of surgical site infection was $24,058.Citation33 Surgical site infection in patients after colorectal procedures was $14,868,Citation34 head-and-neck cancer-related surgery was $22,234,Citation35 coronary artery bypass graft procedures were $10,245,Citation36 and low transverse cesarean delivery were $2888 to $3574Citation37 per case. The latter study found similar attributable costs for surgical site infections using two different statistical methods for attributing costs (attributable cost for surgical site infection was $3529 by regression and $2852 by propensity score).Citation37
Nosocomial bloodstream infections
We found ten studies of the economic burden of nosocomial blood stream infections (one prospective, three retrospective cohorts, five retrospective case controls, and one case series).
In general European patient populations, nosocomial bloodstream infection was associated with costs ranging from $2604 to $22,414.Citation22,Citation31,Citation38–Citation41 One American study reported average incremental costs of $21,013.Citation42 In a pediatric intensive care unit (ICU), nosocomial bloodstream infection was estimated to cost $49,663.Citation43 Very-low-birth-weight infants with nosocomial bloodstream infection incurred average total costs $71,384 higher than those without the infection.Citation44 S. aureus bacteremia in patients with prosthetic implants was associated with $81,743 in costs per nosocomial case in one prospective case series.Citation45
Nosocomial sepsis
We found two studies of the economic burden of nosocomial sepsis. In one retrospective cohort study, nosocomial sepsis was associated with mean additional costs of $33,872Citation46 per case. In one prospective cohort, ICU-acquired sepsis was associated with a mean increase of $44,178 in total costs per case.Citation47
Nosocomial rotavirus infection
We reviewed three studies of nosocomial rotavirus infection. One prospective cohort study estimated the costs associated with nosocomial rotavirus infection in children under 30 months of age, but did not provide a per-case result; this study estimated that the national cost of all cases in 1 year in Italy is $11,952,319.Citation48 Rotavirus in children under 48 months of age was associated with $3591 in costs per case in one prospective case series.Citation49 One prospective study with a nested case control reported $2210 in mean excess costs per case.Citation50
Nosocomial urinary tract infection
We found four studies of the economic burden of nosocomial urinary tract infections. These included one prospective, two retrospective cohorts, and one retrospective case control study. The average costs attributable to urinary tract infection ranged from $788 to $18,717.Citation22,Citation31,Citation51,Citation52
Nosocomial pneumonia
We found four studies of the economic burden of nosocomial pneumonia. Two studies were prospective cohort studies and found that nosocomial pneumonia was associated with average additional costs of $856Citation53 and $23,624.Citation35 One German article detailed both a prospective case control and a retrospective case control, reporting average excess costs of $10,387 and $21,057, respectively.Citation54 In one study, the average cost attributable to ventilator-associated pneumonia in a pediatric ICU was $55,333.Citation55
Nosocomial respiratory tract infection
We included three studies on the economic burden of nosocomial respiratory tract infections: one retrospective cohort, one retrospective case control, and one case control study.
Respiratory tract infections were associated with additional mean costs of $3476Citation31 and $4509Citation22 in two studies, respectively. In one additional study, a case was defined as an infection of nosocomial respiratory syncytial virus; this infection was associated with mean costs of $13,083 per case.Citation56
Miscellaneous nosocomial infections
We included 12 studies that described the economic burden of miscellaneous nosocomial infections. During a Pseudomonas aeruginosa outbreak, it was retrospectively estimated that infected patients who had been on mechanical ventilation incurred excess costs of $26,522.Citation57 Another retrospective case series investigated the economic impact of a norovirus outbreak that affected patients and staff, and did not provide a per-case cost estimate; dividing the total outbreak costs by the given number of case infections yielded a crude estimate of $1282 per case;Citation58 another similar study yielded an estimate of $2972 per case of outbreak-related norovirus.Citation59 In one drug-resistant Salmonella typhimurium outbreak in a Turkish neonatal ICU, cases incurred charges $1208 higher than controls.Citation60 A pertussis outbreak incurred total hospital costs of $34,956 and $50,668 in two hospitals.Citation61 The attributable costs during a Salmonella outbreak in one Australian tertiary care complex were reported in total costs rather than per case, and dividing by the number of cases yields an estimate of $2552 per case.Citation62 One retrospective case control study defined a case as a multidrug-resistant infection of Acinetobacter baumannii in burn patients, and reported a mean additional cost per case of $121,371.Citation63 In one Irish hospital, postoperative MRSA infection incurred additional costs of $13,651.Citation64 Another retrospective case series reported the attributable cost of MRSA to be $123,367 and vancomycin-resistant Enterococcus (VRE) to be $128,690.Citation65 One prospective study with a nested case control reported a median incremental cost of $9708 per case of Clostridium difficile-associated disease (CDAD).Citation66 One case control study reported the attributable costs of VRE in the medical ICU and in hospital to be $9543 and $14,532, respectively.Citation67 One retrospective cohort study examined the cost associated with potentially preventable complications and found it to be $634,432,559.Citation68
Nosocomial venous thromboembolism (VTE)
We identified two burden studies published since 2000. One study focused on nosocomial deep vein thrombosis after hip replacement surgery.Citation69 The cost of deep vein thrombosis was modeled in patients undergoing total hip replacement surgery, with Markov decision and univariate analyses. The article reported the annual per-patient cost of deep vein thrombosis to be $4676. Also provided are the discounted lifetime costs of $3779, as well as costs specific to deep vein thrombosis-related complications, namely post-thrombotic syndrome with ulcer ($4700) and pulmonary embolism ($8131). A retrospective US study of deep vein thrombosis (n = 15,679), pulmonary embolism (n = 7653) and post-thrombotic syndrome (n = 624) found annual attributable direct medical costs of $19,430 for deep vein thrombosis, $21,033 for pulmonary embolism, $28,713 for combined deep vein thrombosis, and pulmonary embolism, and $5455 for patient safety target. This study did not explicitly distinguish cases of nosocomial deep vein thrombosis, but 78% of the study cohort had abdominal or orthopedic surgery prior to the index venous thrombosis event.Citation70
Nosocomial falls
We reviewed three burden-of-illness studies related to nosocomial falls. Two studies were case series.Citation71,Citation72 The third study had a prospective cohort design.Citation73 One studyCitation73 identified cases only in patients aged over 60 years. One study focused on legal compensation rather than hospital-related costs,Citation72 and neither of the other two articlesCitation71,Citation73 clearly stated what methods were used for determining attributable costs. There was one additional case control study reported attributable length of stay, but not costs.Citation74
Oliver found that 60.5% of legal claims related to in-hospital falls resulted in payment of costs or damages, with mean payment of $25,793.Citation72 Nurmi provided the cost per treating an in-hospital fall, estimated at $1359.Citation73 The third study did not describe costs per case or per fall, but did provide the total estimated attributable cost of all cases included in the study; dividing by the provided number of cases yields a crude estimate of $3230 per case.Citation71
We did not find any eligible studies for the following target conditions: nosocomial pressure ulcers, wrong site surgery, retained surgical foreign bodies, contrast inducted nephropathy.
Discussion
We found that 61% of published studies on the economic burden of patient safety targets in acute care describe or report no clear costing methodology. Among the remaining 61 studies (39%), which did report costing methodology, there were wide variations in methodologic features and methods for attributing costs. These studies report wide estimates of the economic burden of patient safety in acute care. For example, the attributable costs of patient safety targets ranged from $2000 to $200,000. In general hospital populations, the cost per case of hospital-acquired infection ranged from $2132 to $15,018. Nosocomial bloodstream infections were associated with costs ranging from $2604 to $22,414. We also found no adequate economic burden data for important patient safety, such as wrong site surgery, retained surgical foreign bodies, contrast-induced nephropathy, and acute care-acquired pressure ulcers.
Our results are consistent with the few prior reviews of the economic burden of patient safety in the acute care setting. A 2005 review identified 165 articles that included an economic analysis as an objective, but 35% of these articles provided no economic analysis, and 25% provided no primary economic data. The remaining studies had significant gaps in their costing methodology, and only 16% conducted sensitivity analyses that could address these limitations.Citation75 Another review of comparative economic evaluations of patient safety programs identified 40 studies published between 2001 and 2004, none of which provided sufficient information about both the cost of the prevention program and the cost of the patient safety being targeted.Citation76 A 1999 study estimated the economic burden of patient safety in Utah and Colorado at $1,442,024 per event (1996 US dollars). This early estimate is much higher than estimates in our systematic review, because the 1999 study evaluated not just direct acute care costs, but also outpatient direct health care costs after the event, as well as indirect (societal) costs such as lost workforce productivity up to age 75 years. None of the adverse event studies in our review considered this broad range of costs for a prolonged time horizon.Citation77
Our findings, in conjunction with these prior reviews, indicate that greater attention is needed to the methodologic standards for evaluating the economic burden of patient safety in the acute care setting. Better knowledge of the economic burden of patient safety will inform decisions about health policy, patient safety research programs, and improvement priorities. High quality economic burden studies are an essential component of comparative economic analyses, such as cost effectiveness studies. Most of the studies we identified considered only the acute care hospital economic perspective, but the economic perspective should extend beyond the acute care hospital, as it has been estimated that 22%–66% of the economic burden of patient safety in acute care are borne by the hospital.Citation78,Citation79 Economic burden studies for patient safety should explicitly consider cost categories, legal, marketing and operational perspectives (direct or indirect), and time frames (including short- and long-term effects). There are also important methodologic considerations when attributing costs to patient safety, rather than the patient’s underlying condition. These considerations include the reliability of data sources used to identify patient safety, the adequacy of methods to control for confounding factors such as comorbidity and severity of illness, and the appropriateness of estimation methods including the incorporation of adverse event timing, matching methods, and regression modeling.Citation80 Differential timing of the occurrence of patient safety can lead to wide estimates of attributable costs.Citation81–Citation83
Our review has several important limitations. First, we focused on studies published between 2000 and 2010 and indexed in MEDLINE. Studies outside of our search strategy may contain potentially useful data. For example, we did not include a 2010 study by the Society of American Actuaries because it was not indexed in MEDLINE.Citation84 However, our finding that 61% of studies provide no or limited costing methodology would be unchanged by the inclusion of a few additional studies. Second, we focused only on patient safety targets in the acute care setting. We did not include studies of patient safety targets from other settings, such as community or chronic care. Third, we did not evaluate the interrater reliability of our methodologic reviews. Our review method was designed to yield higher methodologic ratings, as we always took the higher rating of the two reviewers, yet we still identified a significant lack of methodologic features. Fourth, we arbitrarily assigned one point for each methodologic feature, so that we could report a simple summary measure of methodologic features. However, we recognize that methodologic features are not necessarily equally weighted. Finally, there was heterogeneity in study methods. Variability in costing and methodologic features made it impossible to generate summary estimates of economic burden for all patient safety targets.
In summary, the burden of patient safety targets ranged from as little as $2000 to $200,000 in hospitalized individuals to $600 million at a population level. These results are dependent on the resources and costs included in the analysis. We found that the majority of published studies on the economic burden of patient safety targets in acute care described no costing methodology. The methodologic quality of the remaining studies was moderate, but there were wide variations in methodologic quality and methods for attributing costs. Greater attention is needed to the methodologic standards for evaluation of economic burden. This study highlights the limitations in the methods required to conduct economic evaluations in patient safety. Such limitations make decision-making regarding the adoption of patient safety initiatives difficult. The identification of limitations will allow for focused work on their improvement and will allow for the development of guidelines for future economic evaluation in patient safety.
Contributions
Dr Nicole Mittmann, Ms Marika Koo, Dr Nick Daneman, Dr Andrew McDonald, Dr Michael Baker, Dr Anne Matlow, Dr Murray Krahn, Dr Kaveh Shojania, and Dr Edward Etchells all had substantial contributions to the concept and design, acquisition of data, or analysis and interpretation of data. All authors contributed to the draft or revision of the article in a critical manner and they all gave final approval of the version being submitted.
Acknowledgments
The authors acknowledge Ms Peggy Kee and Ms Evelyn Worthington for their administrative and data analysis, and Dr William Geerts, Dr Damon Scales, and Dr Andrew Simor for their assistance in the study design. This work was funded by an unrestricted grant from the Canadian Patient Safety Institute.
Disclosure
The authors report no conflicts of interest in this work.
References
- LandriganCPParryGJBonesCBHackbarthADGoldmannDASharekPJTemporal trends in rates of patient harm resulting from medical careN Engl J Med2010363222124213421105794
- ClassenDCResarRGriffinF“Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measuredHealth Aff (Millwood)201130658158921471476
- Canadian Agency for Drugs and Technologies in HealthGuidelines for the economic evaluation of health technologies: Canada [Internet]20063rd edOttawa, ONCanadian Agency for Drugs and Technologies in Healthvii46A17 [cited Oct 20]. Available from: http://www.cadth.ca/media/pdf/186_EconomicGuidelines_e.pdfAccessed September 30, 2011
- MittmannNEvansWKRocchiAAddendum to CADTH’s guidelines for the economic evaluation of health technologies: specific guidance for oncology productsOttawaCanadian Agency for Drugs and Technologies in Health2009
- GabrielSDrummondMMaetzelAOMERACT 6 Economics working group report: a proposal for a reference case for economic evaluation in rheumatoid arthritisJ Rheumatol200330488689012672223
- DrummondMFJeffersonTOGuidelines for authors and peer reviewers of economic submissions to the BMJBMJ19963132752838704542
- DrummondMFO’BrienBStoddartGLMethods for the Economic Evaluation of Health Care Programmes2nd edOxford UKOxford Medical Publications1997
- ShojaniaKGDuncanBWMcDonaldKMWachterRMMaking health practices safer: a critical analysis of patient safety practices2001Report No: Evidence Report/Technology Assessment No 43
- National Surgical Quality Improvement ProgramProgram Specifics: Data Analysis and Reporting2006 Available from: http://www.acsnsqip.org/main/programspecs/program_reportingjspAccessed September 30, 2011
- World Health OrganizationPatient Safety: Implementing Change2011 Available from: http://www.who.int/patientsafety/implementation/en/Accessed September 30, 2011
- Bank of CanadaDaily currency converter2011 Available from: http://www.bankofcanada.ca/rates/exchange/daily-converter/Accessed September 30, 2011
- United States Department of Labor BoLSCPI Inflation Calculator2011 Available from: http://www.bls.gov/data/inflation_calculator.htmAccessed September 30, 2011
- HoonhoutLHde BruijneMCWagnerCDirect medical costs of adverse events in Dutch hospitalsBMC Health Serv Res20099273719203365
- EhsaniJPJacksonTDuckettSJThe incidence and cost of adverse events in Victorian hospitals 2003–2004Med J Aust20061841155155516768660
- NewPWJacksonTThe costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, AustraliaSpine201035779680220228702
- PappasSHThe cost of nurse-sensitive adverse eventsJ Nurs Adm200838523023618469616
- MorrisJACarrilloYJenkinsJMSurgical adverse events, risk management, and malpractice outcome: Morbidity and mortality review in not enoughAnn Surg2003237684485212796581
- AokiNUdaKOhtaSKiuchiTFukuiTImpact of miscommunication in medical dispute cases in JapanInt J Qual Health Care200820535836218635588
- KaushalRBatesDWFranzCSoukupJRRothschildJMCosts of adverse events in intensive care unitsCrit Care Med200735112479248317828035
- SenstBLAchusimLEGenestRPPractical approach to determining costs and frequency of adverse drug events in a health care networkAm J Health-Syst Pharm200158121126113211449856
- ChenYYChouYCChouPImpact of nosocomial infection on cost of illness and length of stay in intensive care unitsInfect Control Hosp Epidemiol200526328128715796281
- ChenYYWangFDLiuCYChouPIncidence rate and variable cost of nosocomial infections in different types of intensive care unitsInfect Control Hosp Epidemiol2009301394619046058
- RobertsRRScottDCordellRThe use of economic modeling to determine the hospital costs associated with nosocomial infectionsClin Infect Dis200336111424143212766838
- KilgoreMLGhoshKBeaversMWongDYHymelPABrossetteSEThe costs of nosocomial infectionsMed Care200846110110418162862
- EsatogluAEAgirbasIOnderORCelikYAdditional cost of hospital-acquired infection to the patient: a case study in TurkeyHealth Serv Manage Res200619313714316848954
- ShengWHWangJTLuDCTChieWCChenYCChangSCComparative impact of hospital-acquired infections on medical costs, length of hospital stay and outcome between community hospitals and medical centresJ Hosp Infect200559320521415694977
- PlowmanRGravesNGriffinMASThe rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a distract general hosptial in England and the national burden imposedJ Hosp Infect200147198209
- LeeJImanakaYSekimotoMRisk-adjusted increases in medical resource utilization associated with health care-associated infections in gastrectomy patientsJ Eval Clin Pract20101610010620367820
- MahieuLMBuitenwegNBeutelsPDe DooyJJAdditional hospital stay and charges due to hospital-acquired infections in a neonatal intensive care unitJ Hosp Infect200147322322911247683
- GravesNNichollsTMMorrisAJModeling the costs of hospital-acquired infections in New ZealandInfect Control Hosp Epidemiol200324321422312683515
- DefezCFabbro-PerayPCazabanMBoudemagheTSottoADauresJPAdditional direct medical costs of nosocomial infections: an estimation from a cohort of patients in a French university hospitalJ Hosp Infect200868213013618201796
- WeberWPZwahlenMReckSFeder-MengusCWidmerAFMartiWREconomic burden of surgical site infections at a European university hospitalInfect Control Hosp Epidemiol200829762362918564917
- WhitehouseJDFriedmanDKirklandKBRichardsonWJSextonDJThe impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra costInfect Control Hosp Epidemiol200223418318912002232
- MahmoudNNTurpinRSYangGSaundersWBImpact of surgical site infections on length of stay and costs in selected colorectal proceduresSurg Infect2009106539544
- PenelNLefebvreJLCazinJLAdditional direct medical costs associated with mosocomial infections after head and neck cancer surgery: a hosptial-perspective analysisInt J Oral Maxillofac Surg20083713513918022348
- JenneyAWHarringtonGARussoPLSpelmanDWCost of surgical site infections following coronary artery bypass surgeryANZ J Surg2001711166266411736828
- OlsenMAButlerAMWillersDMGrossGAHamiltonBHFraserVJAttributable costs of surgical site infection and endometritis after low transverse cesarean deliveryInfect Control Hosp Epidemiol201031327628220102279
- BlotSIDepuydtPAnnemansLClinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infectionsClin Infect Dis200541111591159816267731
- OrsiBGDi StefanoLNoahNHospital-acquired, laboratory-confirmed bloodstream infection: Increased hospital stay and direct costsInfect Control Hosp Epidemiol200223419019712002233
- PirsonMDramaixMStruelensMRileyTVLeclercqPCosts associated with hospital-acquired bacteraemia in a Belgian hospitalJ Hosp Infect2005591334015571851
- PirsonMLeclercqPJacksonTLeclercqMGarrinoMSionCFinancial consequences of hospital-acquired bacteraemia in three Belgian hospitals in 2003 and 2004J Hosp Infect200868191618055065
- KilgoreMBrossetteSECost of bloodstream infectionsAm J Infect Control200836S172. e1S172. e319084149
- ElwardAMHollenbeakCSWarrenDKFraserVJAttributable cost of nosocomial primary bloodstream infection in pediatric intensive care unit patientsPediatrics2005115486887215805357
- PayneNRCarpenterJHBadgerGJHorbarJDRogowskiJMarginal increase in cost and excess length of stay associated with nosocomial bloodstream infections in surviving very low birth weight infantsPediatrics2004114234835515286215
- ChuVHCrosslinDRFriedmanJYStaphylococcus aureus bateremia in patients with prosthetic devices: costs and outcomesAm J Med20051181416. e191416. e2416378797
- AdrieCAlbertiCChaix-CouturierCEpidemiology and economic evaluation of severe sepsis in France: age, severity, infection site, and palce of acquisition (community, hospital, or intensive care unit) as determinants of workload and costJ Crit Care2005201465816015516
- Brun-BuissonCRoudot-ThoravalFGirouEGrenier-SennelierCDurand-ZaleskiIThe costs of septic syndromes in the intensive care unit and influence of hospital-acquired sepsisIntensive Care Med20032991464147112856120
- FestiniFCocchiPMambrettiDNosocomial rotavirus gastroenteritis in pediatric patients: a multi-centre prospective cohort studyBMC Infect Dis20101023524220696065
- FruhwirthMBergerKEhlkenBMoll-SchulerIBroslSMutzIEconomic impact of community- and nosocomially acquired rotavirus gastroenteritis in AustriaPediatr Infect Dis J200120218418811224839
- PiednoirEBessaciKBureau-ChalotFEconomic impact of healthcare-associated rotavirus infection in a paediatric hospitalJ Hosp Infect200355319019514572486
- TambyahPAKnasinskiVMakiDGThe direct costs of nosocomial catheter-associated urinary tract infection in the era of managed careInfect Control Hosp Epidemiol2002231273111868889
- MorseBCBolandBNBlackhurstDWRoettgerRHAnalysis of centers for medicaid and medicare services ‘Never events’ in elderly patients undergoing bowel operationsAm Surg201076884184520726414
- RosenthalVDBuzmanSMigoneOSafdarNThe attributable cost and length of hospital stay because of nosocomial pneumonia in intensive care units in 3 hospitals in Argentina: A prospective matched analysisAm J Infect Control200533315716115798670
- DietrichESDemmlerMSchulgenGNosocomial pneumonia: a cost-of-illness analysisInfection2002302616712018471
- BrilliRJSparlingKWLakeMRThe business case for preventing ventilator-associated pneumonia in pediatric intensive care unit patientsJt Comm J Qual Saf20083411629638
- MacartneyKKGorelickMHManningMLHodinkaRLBellLMNosocomial respiratory syncytial virus infections: the cost-effectiveness and cost-benefit of infection controlPediatrics2000106352052610969097
- BouRLorenteLAguilarAHospital economic impact of an outbreak of Pseudomonas aeruginosa infectionsJ Hosp Infect200971213814218799237
- FretzRSchmidDJelovcanSAn outbreak of norovirus gastroenteritis in an Austrian hospital, winter 2006–2007Wien Klin Wochenschr20091213–413714319280140
- ZinggWColomboCJuckerTBossartWRuefCImpact of an outbreak of norovirus infection on hospital resourcesInfect Control Hosp Epidemiol200526326326715796278
- AnilMHelvaciMOzkalayNSalmonella typhimurium outbreak in a neonatal unit in TurkeyIndian J Pediatr200976662963319418032
- BaggettHCDuchinJSSheltonWTwo nosocomial pertussis outbreaks and their associated costs – King County, Washington, 2004Infect Control Hosp Epidemiol200728553754317464912
- SpearingNMJensenAMcCallBJNeillASMcCormackJGDirect costs associated with a nosocomial outbreak of Salmonella infection: An ounce of prevention is worth a pound of cureAm J Infect Control2000281545710679138
- WilsonSJKnipeCJZiegerMJDirect costs of multidrug-resistance acinetobater baumannii in the burn unit of a public teaching hospitalAm J Infect Control20043234234415454892
- WattersKO’DwyerTPRowleyHCost and morbidity of the MRSA in head and neck cancer patients: what are the consequences?J Laryngol Otol2004118969469915509366
- MauldinPDSalgadoCDDurkalskiVLNosocomial infections due to mechicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus: relationships with antibiotic use and cost driversAnn Pharmacother200842331732618285560
- VonbergRPReichardtCBehnkeMSchwabFZindlerSGastmeierPCost of nosocomial Clostridium difficile-associated diarrhoeaJ Hosp Infect2008701152018602185
- PuzniakLAGillespieKNLeetTKollefMMundyLMA cost-benefit analysis of gown use in controlling vancomycin-resistant enterococcus transmission: Is it worth the price?Infect Control Hosp Epidemiol200425541842415188849
- FullerRLMcCulloughECBaoMZAverillRFEstimating the costs of potentially preventable hospital acquired complicationsHealth Care Financ Rev2009304173219719030
- CapriniJABottemanMFStephensJMEconomic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United StatesValue Health200361597412535239
- MacDougallDAFeliuALBoccuzziSJLinJEconomic burden of deep-vein thrombosis, pulmonary embolism, and post-thombotic syndromeAm J Health-Syst Pharm200663Suppl 6S5S1517032933
- NadkarniJBIyengarKPDussaCWatveSVishwanathKOrthopaedic injuries foloowing falls by hospital in-patientsGerontology20055132933316110235
- OliverDKillickSEvenTWillmottMDo falls and falls-injuries in hospital indicate negligent care – and how big is the risk? A retrospective analysis of hte NHS litigation authority database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006Qual Saf Health Care20081743143619064658
- NurmiILuthjePIncidence and costs of falls and fall injuries among elderly in institutional careScand J Prim Health Care200220211812212184711
- HillKDVuMWalshWFalls in the acute hospital setting – impact on resource utilisationAus Health Rev2007313471477
- SchmidekJMWeeksWBWhat do we know about financial returns on investments in patient safety? A literature reviewJt Comm J Qual Patient Saf2005311269069916430022
- FukudaHImanakaYAssessment of transparency of cost estimates in economic evaluations of patient safety programmesJ Eval Clin Pract200915345145919366392
- ThomasEJStuddertDMNewhouseJPCost of medical injuries in Utah and ColoradoInquiry199936325526410570659
- ZhanCFriedmanBMossoAPronovostPMedicare payment for selected adverse events: building the business case for investing in patient safetyHealth Aff (Millwood)20062551386139316966737
- MelloMMStuddertDMThomasEJYoonCSBrennanTAWho pays for medical errors? An analysis of adverse events costs, the medical liabililty system, and incentives for patient safety improvementJ Empir Leg Stud201144835860
- GravesNHarbarthSBeyersmannJBarnettAHaltonKCopperBEstimating the cost of health care-associated infecitons: mind your p’s and q’sClin Infect Dis20105071017102120178419
- BarnettAGBatraRGravesNEdgeworthJRobothamJCooperBUsing a longitudinal model to estimate the effect of methicillin-resistant Staphylococcus aureus infection on length of stay in an intensive care unitAm J Epidemiol200917091186119419762373
- GravesNWeinholdDRobertsJACorrecting for bias when estimating the cost of hospital-acquired infection: an analysis of lower repiratory tract infections in non-surgical patientsHealth Econ200514775576115678521
- BeyersmannJKneibTSchumacherMGastmeierPNosocomial infection, length of stay, and time-dependent biasInfect Control Hosp Epidemiol200930327327619193018
- ShreveJVan Den BosJGrayTHalfordMRustagiKZiemkiewiczEThe economic measurement of medical errors2010 Available from: http://www.soa.org/files/pdf/research-econ-measurement.pdfAccessed September 30, 2011