Abstract
Background
Medication-related hospital admission (MRHA) is hospitalization due to drug-related problems. MRHAs have been reported to be on the rise in recent decades.
Objective
This study was aimed at determining the prevalence, patterns, and predictors of MRHA among patients visiting the emergency ward of the University of Gondar comprehensive specialized hospital, Ethiopia.
Methods
A cross-sectional study was conducted from June 1, 2022, to August 30, 2022 G.C. in the emergency ward at the University of Gondar Comprehensive Specialized Hospital. The AT-HARM 10 tool was used to collect data from participants who fulfilled the inclusion criteria. Data was entered into EpiData Manager 4.6.0.0 and was exported to Statistical Package for Social Sciences (SPSS) version 24 for analysis. Descriptive statistics were presented using frequency and percentage. Binary logistic regression was applied to identify factors associated with MRHAs with a 95% confidence level, and significance was declared at a p-value <0.05.
Results
The prevalence of MRHAs was 30.5% (95% CI = 27.7–36.4%). More than half (64.52%) of MRHAs were definitely preventable. The majority of MRHAs (48.39%) were severe. Non-compliance (41.12%), followed by untreated indication (26.61%) and adverse drug reaction (12.09%) were the most frequent causes of MRHAs. Renal impairment (AOR = 2.703, 95% CI: 1.29 to 5.663), chronic disease (AOR = 10.95, 95% CI: 4.691 to 25.559), history of traditional medication use (AOR = 2.089, 95% CI: 1.162 to 3.755), and history of hospitalization (AOR = 4.001, 95% CI: 1.98 to 8.089) were significantly associated with MRHAs.
Conclusion
MRHAs were substantially prevalent. Most of the MRHAs were definitely preventable. Renal impairment, chronic disease, history of traditional medication use, and history of hospitalization were predictors of MRHAs. At the university hospital, health care providers should strive to prevent and manage MRHAs appropriately.
Keywords:
Background
Patients have been admitted to hospitals due to medication-related problems over the past few decades. Most of the admissions resulted from either preventable or potentially preventable drug-related problems (DRP).Citation1
A drug-related problem (DRP) is defined as an event or circumstance that involves a patient’s drug treatment that actually, or potentially, interferes with the achievement of an optimal outcome.Citation2
Some of the DRPs responsible for medication-related hospital admissions (MRHA) might be adverse drug reactions, inappropriate drug selection, noncompliance, untreated indications, and drug interaction.Citation3
A recent systematic review revealed that the most common cause of DRPs was “drug selection” (80.38%) in the primary domain, with the common subdomains “inappropriate drug according to guidelines/formulary” (54.63%), “no or incomplete drug treatment in spite of existing indication” (8.73%), “no indication for drug” (7.55%) and “too many different drugs/active ingredients prescribed for indication” (6.67%). Secondly, the cause of DRPs was reported in the primary domain “dose selection”, accounting for 10.52% with the common subdomains “drug dose too low” (4.54%) and “drug dose too high” (4.06%).Citation4 A systematic review and meta-analysis done in Ethiopia showed that the “need for additional drugs” was the most frequently reported type of DRP, (33%), followed by “noncompliance”, 21%.Citation5 Different studies have identified many factors for MRHA. As an example, old age,Citation1 female gender,Citation6 polypharmacy,Citation7 and the presence of comorbiditiesCitation6,Citation8 are related.
A systematic review found that around 5–10% of hospital admissions were due to DRPs.Citation1 Another systematic review stated that the prevalence of drug-related hospital admissions varies from 1.3% to 41.3%. Among patients hospitalized related to medications, 2.7% died due to DRPs.Citation2
In a study conducted in the Netherlands, among general and academic hospitals the total costs of medication-related hospital admissions in one year were €81 million and €14 million, respectively.Citation9 A study in Brazilian hospitals revealed that the mean per hospital visit treatment costs of emergency department visit rates due to drug-related morbidity were US $900 ± $1569 (range US $18–$10,847).Citation10 The annual estimated cost of MRHA in an Australian study was 1.4 billion Australian dollars.Citation11 In Africa, a study conducted in Nigeria stated that annually a total of 1.83 million naira (USD 15,466.60) was used up to manage patients admitted due to ADRs.Citation12
According to a systematic review and meta-analysis done in Ethiopia, a high prevalence of drug-related problems occur at different stages of medication use process.Citation13 Low-income countries such as Ethiopia could experience various draw backs related to MRHA. Medication-related hospital admissions contribute to increased health-care costs, loss of productivity, lower patient satisfaction, low quality of life, and increased mortality.Citation2,Citation14 Determining the prevalence, preventability, severity, and associated factors of medication-related hospital admissions might aid in minimizing adverse health outcomes.
Method
Study Design, Area, and Period
A cross-sectional study was conducted from June 1, 2022, to August 30, 2022 G.C in the emergency ward at the UoGCSH, located in Gondar town, northwest Ethiopia. The calculated flying distance from Addis Ababa, the capital city of Ethiopia, to Gondar, is equal to 262 miles, which is equal to 421 km, and the driving distance between Addis Ababa and Gondar is 727.22 km.Citation15 The University of Gondar Comprehensive Specialized Hospital is a tertiary care facility with different wards, including emergency, ambulatory, pediatrics, oncology, gynecology, and surgery wards. According to the UoGCSH’s 2022 G.C. annual report, around 280,000 patients visited the hospital and 12,000 are admitted to the emergency ward.
Population, Inclusion, and Exclusion Criteria
Patients aged ≥ 18 years admitted to the emergency ward at UoGCSH were the source population. However, those adult patients admitted to the emergency ward at UoGCSH during the study period were the study population. All adult patients admitted to the emergency ward with complete medical history data were included in the study. Patients with intentional medication poisoning, intoxication with chemicals and/or presented with trauma and injuries associated with accidents were excluded.
Sample Size Determination and sampling Procedure
The sample size was determined using a single population proportion formula with the assumption of a 95% confidence level, 5% margin of error, and 60% population proportion was used. This was obtained from a recent study conducted at the emergency ward.Citation16
n= (1.96)2(0.6×0.4)/ (0.05)2=368.79
By adding a 10% non-response rate (368.79*10% = 36.87) to the calculated sample size, 406 patients were estimated for the study. Where n = sample size, p = sample proportion/population proportion, z = confidence level/Z- score, and = margin of error.
Patients who fulfilled the inclusion criteria were subjected to a systematic random sampling technique. During the four-month data collection period, 4000 patients were estimated to be admitted to the emergency ward. The formula “k=N/n” was used to obtain the “k” value. The “k” value became “10”, and then a lottery method was used by rolling a piece of paper one through ten and randomly selecting one of the rolled papers to choose the first study participant. Then every tenth patient admitted to the ward was taken as a sample.
Variables of the Study
The dependent variable was medication-related emergency ward admission. The independent variables include age, marital status, patients with uncorrected/uncorrectable visual impairment, patients with uncorrected/uncorrectable renal impairment, patients that had chronic illness, patients with a history of traditional medication use, patients that had a history of hospitalization, number of medication the patient was using before admission, and duration of treatment for medication used before admission.
Operational Definitions
MRHA: If patient’s medical record at admission was stated as medication-related or if the patient is admitted due to one or more DRPs including (non-compliance, untreated indications, improper drug selection, subtherapeutic dosage, failure to receive drugs, overdosage, ADRs, drug interactions, and drug use without indication.Citation17,Citation18 Non-MRHA: If the admission was caused by
an infection or a previously undiagnosed disease, progression of a previously diagnosed disease that is not medication-related, physical trauma, substance intoxication and social circumstances or allergies that are not medication-related.Citation19
Definitely preventable: If the patient avoids taking a drug that is recognized to reduce or avert the symptoms according to the prescriber supervision, had a known allergy to the medication, had a disease for which the drug was contraindicated, and took unindicated mediation.
Potentially preventable: where sufficient monitoring within a given time preludes DRPs.
Not preventable: If the mediation-related event could not have been avoided by any reasonable means, or it was an uncertain occurrence in the course of treatment fully in congruence with good medication utilization.Citation18,Citation20
Severity was considered “mild”: if a laboratory abnormality or the symptom did not require medication intervention.
Severity was considered “moderate”: if a laboratory abnormality or symptom that required medication intervention at the emergency ward.
Severity was considered “severe”: if the symptom required hospital admission and was life-threatening (difficult to gain a rapid intervention using medication).Citation6,Citation14
Data Collection Instrument, Procedure, and quality Control
To collect the data, two pharmacists were trained on the data collection tool. Patients who fulfill the inclusion criteria and were willing to participate were assessed based on the tool when they are admitted to the emergency ward. Socio-demographic data were obtained based on previous similar studies. A tool that was developed at Uppsala University Hospital, Sweden, was used to identify medication-related admissions and related variables. AT-HARM10 tool consisting of ten closed questions was used to distinguish between admissions that are unlikely to be and those that are possibly medication-related.Citation19 Preventability of MRHA was assessed according to the modified version of G. T. Schumock and J. P. Thornton's preventability criteria.Citation21
Part of the questionnaire that needed the response of patients (the socio-demographic data, patient’s interview questions regarding drug therapy use) was translated into the local language (Amharic), and then they were interviewed. Then it was back translated into the English version to confirm translation consistency. Clinical information was gathered from patient medical records (procedure notes, physician orders, prescription papers, medication administration records, physician progress notes, pertinent laboratory reports, and nursing progress notes). Estimated glomerular filtration rate (eGFR) of patients was calculated using the Cockcroft-Gault equation.Citation22 For patients with renal impairment, “Drug Prescribing in Renal Failure” was used as a guide to determine the appropriateness of the drug dose prescribed.Citation23
After the questionnaire was pre-tested on 5% (20 individuals) of the study population, some rearrangements were made to the tool for appropriate data collection. The data collectors were trained for two days on the study objectives and how to use the questionnaire properly. Data collectors were supervised while collecting data. The data was checked for its completeness and consistency on a daily basis.
Analysis of Data
After data was entered, cleared, and checked with EpiData Manager 4.6.0.0, it was exported to Statistical Package for Social Sciences (SPSS) version 24 for analysis. The normality of the different variables included in the analysis was checked using histograms and the Shapiro–Wilk test. Descriptive statistics were used to characterize dependent and independent variables. The frequency and percentage of socio-demographic characteristics, clinical characteristics, and variables that measure MRHA were analyzed. Categorical variables were described as frequency and percentages, and continuous variables as the median and interquartile range (IQR). Tables and figures were used to summarize and describe the results.
To test the strength of association between dependent and independent variables, variables having a p-value <0.2 in bivariable binary logistic regression analysis were entered into multivariable binary logistic regression. The Hosmer–Lemeshow goodness of fit test was used to check model fitness. Chi-square test was used to see the association between two variables. All variables obeying the assumption of independence were analyzed later by multivariable binary logistic regression. Multicollinearity was assessed before the analysis and variables with the variance inflation factor (VIF) ranging from 1–1.8 were included.Citation24 In addition, the presence of outliers was checked using the interquartile range method (Q1-1.5*IQR and Q3+1.5*IQR).Citation25 There were no outliers in the data. Furthermore, the strength of association was measured using an odds ratio (OR). A p-value of < 0.05 was considered statistically significant with a 95% level of confidence.
Result
Socio-Demographic Data
From a total of 406 study participants, the median age of study participants was 40 years (IQR: 28–55). More than half (54.4%) of participants were female. Most of the patients (52%) were married. Beyond two-third (72.7%) of participants were rural residents. Regarding educational level, more than half (56.9%) of patients could not read or write. Majority (82.5%) of patients live with their families. A scanty number of patients (3.4%) had a smoking habit and less than half (45.6%) of patients had a drinking habit ().
Table 1 The Socio-Demographic Data of Patients Admitted to the Emergency Ward at UoGCSH, from June 1, 2022, to August 30, 2022 G.C
Patients’ Clinical and Medication Related Data
Patients were assessed at admission of which 11.6% had visual impairment and 16% had renal insufficiency. More than one-third (36.7%) of participants had chronic disease that were diagnosed before admission to the emergency ward of UoGCSH.
Around one-third (32.5%) of patients had a history of traditional medication use. Less than half (46.1%) of study participants had a history of hospital admission, and more than two third (63.1%) of them were hospitalized within 3 up to 6 months ().
Table 2 The Clinical Data of Patients Admitted to the Emergency Ward at UoGCSH from June 1, 2022, to August 30, 2022 G.C
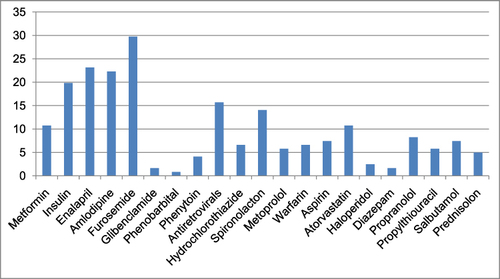
Hypertension (14.28%) followed by diabetes mellitus (10.59%) were the most common history of diagnoses for patients who were admitted to the emergency ward ().
Figure 1 Patient’s history of diagnosis before they were admitted to the emergency ward at UoGCSH, from June 1, 2022 to August 30, 2022G.C.
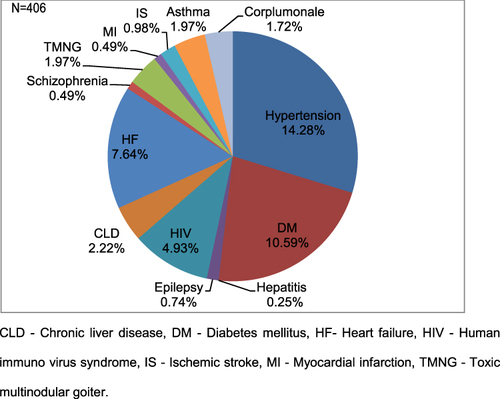
The median number of medications used before admission was 2 (IQR: 1–3). The median duration of treatment before admission was 36 months (IQR: 5–133 months). Among 121 patients who had used medication before admission, nearly one-third (29.75%) of patients used Furosemide ().
Prevalence and Patterns of Medication Related Hospital Admission
From a total of 406 admitted patients, MRHA was identified in 124 (30.5%) of study participants of which more than half (64.52%) were definitely preventable Regarding the severity, most (81.45%) of MRHAs were severe ().
Table 3 Patterns of MRHAs Among Patients Admitted to the Emergency Ward at UoGCSH, from June 1, 2022, to August 30, 2022 G.C
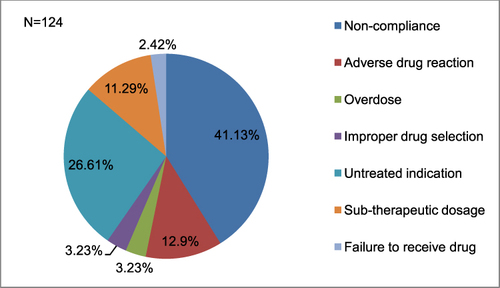
Out of 124 MRHAs, most (41.12%) of them were due to non-compliance, followed by untreated indication (26.61%) and adverse drug reaction (12.09%) ().
Figure 3 The DRP categories among patients with MRHA admitted to the emergency ward of UoGCSH from June 1, 2022 to August 30, 2022G.C.
Among patients admitted due to medication, ninety-nine of them were on drug therapy. Of which more than three-fourth (79.79%) of them had regular follow-up at health care facilities. And more than half (60.6%) of patients get their medications paid. More than one-third (35.35%) of participants had a problem of remembering their medication regimen. Three-fourth (75.75%) of patients does not have medications other than prescribed medications. More than half (53.54%) of participants had discontinued their medication without telling their doctors. The most common reason for patients to discontinue their medications was “feeling well” (35.85%) followed by ADR (24.53%) ().
Table 4 Medication-Related Information of Patients Who Have Been on Drug Therapy Before Admission to the Emergency Ward at UoGCSH from June 1, 2022, to August 30, 2022 G.C
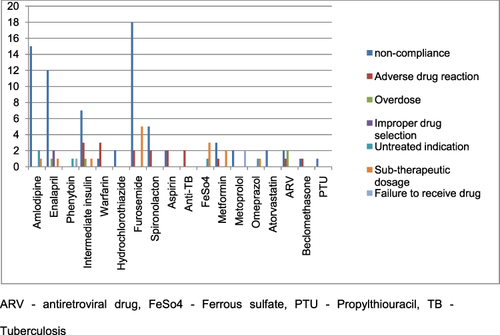
Furosemide was the most commonCitation16 medication associated with the DRP category non-compliance, followed by AmlodipineCitation2 and EnalaprilCitation11 ().
Figure 4 Lists of medications that patients were taking associated with DRP categories at the emergency ward of UoGCSH from June 1, 2022 to August 30, 2022G.C.
According to the multivariate logistic regression analysis, the variables renal impairment, chronic disease, history of traditional mediation use and history of hospitalization were significantly associated with the occurrence of MRHA.
Patients with renal impairment (AOR = 2.703, 95% CI: 1.29–5.663), patients with chronic disease (AOR = 10.95, 95% CI: 4.691–25.559), patients with a history of traditional mediation use (AOR = 2.089, 95% CI: 1.162–3.755), and patients with a history of hospitalization (AOR = 4.001, 95% CI: 1.98–8.089) were predictors of MRHA ().
Table 5 Factors Associated with MRHA in the Emergency Ward at UoGCSH from June 1, 2022, to August 30, 2022 G.C
Discussion
The findings of this scientific evidence would help to allay MRHAs not only at UGCSH but also in similar settings throughout the nation.
This study revealed a high prevalence of MRHA that was 30.5% (95% CI = 26.1–35). The result is consistent with a study done in EthiopiaCitation18 and Spain.Citation26 A much higher prevalence was observed in a study done in Ethiopia (57.9%)Citation16 and Sweden (41.3%).Citation6 The prevalence in the present study is lower than the study done in Ethiopia stated previously. This might be due to the current study was not a multicentre study design resulting in a lower percentage of prevalence. The present study does not assess the elderly population alone unlike the Swedish study. Drug-related problems are more predominantly experienced by the elderly population resulting in MRHA. Age-related physiologic changes associated pharmacokinetic and pharmacodynamics alterations, multi-morbidity and polypharmacy are more common in these population.Citation27
Patients with chronic illness should be alert about the appropriateness of their mediation use. If not used properly it might lead them to be hospitalized frequently. This could give them a devastating economic consequence and a compromised quality of life.Citation28
The current study revealed 64.52% (95% CI = 56.5–73.4) of MRHAs were definitely preventable. Similarly a study in EthiopiaCitation18 revealed the majority of MRHAs were definitely preventable. By contrast a study done in the Czech Republic,Citation29 Australia,Citation11 and CanadaCitation30 showed the majority of MRHS were potentially preventable According to the present study finding, patients usually refuse to take medications as prescribed by physicians and patients do not seek therapy even if they have a condition that requires drug therapy. These reasons would result in definitely preventable MRHA. Compliance with mediation is mandatory for a patient to achieve desired treatment outcome.Citation31 In addition ignorance or some disease by itself might not allow a patient to receive treatment despite being necessary.Citation32 Medical teams should create awareness about the benefits of being compliant and taking the required treatment to patients on a regular during their arrival of taking medications (Mediation refill). Patients should take responsibility to improve their health condition by visiting health facilities if necessary and be adhered to medication.
In the present study the most common category of DRP that result in MRHA was noncompliance, 41.4% (95% CI = 33.1–50). This result is similar with studies done in Ethiopia,Citation16,Citation18 India,Citation33 and Saudi-Arabia.Citation34 In this study most patients discontinued their mediation when they were “feeling well” 35.85%. The clinical data showed that the majority of patients have a chronic disease that needs life-long treatmentCitation35 despite feeling well. Patients with chronic diseases need frequent medical monitoring and counseling with their prescribers not to discontinue their mediation.Citation36 The second most common reason for discontinuation of treatment was due to ADRs. Patients discontinue their medication when noxious drug reactions are experienced. To minimize drug discontinuation patients need to be reassured about possible ADRs before they take their medications.Citation37 Clinical pharmacists could review patients’ medical charts, interview patients about their medication use practice, ask if they need any clarity about how to use their medications and, identify as well as monitor ADRs in hospital wards. By doing so, clinical pharmacists would have a role in early detection, reporting, and prevention of drug-related problems.Citation38
The current study found that renal impairment was significantly associated with MRHA. Patients with renal impairment experienced nearly 3 times more MRHA than patients without renal insufficiency [AOR: 2.703, 95% CI: (1.29 −5.663), p = 0.008]. This is consistent with the studies done in NorwayCitation39 and Australia.Citation40 Inappropriate drug dose adjustment and medication choice might lead renal impaired patients to frequent admission to hospitals.Citation41 ADRs resulting from inappropriate medication use are common in patients with renal insufficiency and older population as their organ functions are compromised, which could result in hospitalization.Citation42 Close monitoring of renal function, appropriate dose adjustment and drug selection are required in patients with renal insufficient to minimize the frequency of hospitalization and improve quality of life in those patients.
The present study revealed that patients with chronic disease experienced about 11 times more MRHA than patients without chronic [AOR: 10.95, 95% CI: (4.691–25.559), p < 0.001]. Similarly studies conducted in Ethiopia,Citation18 Spain,Citation43 and NorwayCitation20 found that patients with chronic disease are at higher risk of MRHA. Patients with chronic disease could take multiple medications for a long period of time to control their disease progression.Citation44 Patient with chronic disease might not be compliant to medications and could experience ADR that result in MRHAs. Attention should be given to patients with chronic disease that have multiple medications to avoid drug interactions and subsequent ADRs.Citation45 Patients with polypharmacy might also forget taking their medication regimen that could be difficult to manage with their chronic health condition. Patient education and good professional interaction would be beneficial to increase medication adherence. Health care professionals should optimize benefits and decrease harms during medication use process in chronic disease patients. To achieve treatment goals, patient preference and individualized management should also be considered.Citation46
In addition, this study also found that patients with a history of traditional medication use experienced 2 times more MRHA than patients with no history of traditional mediation use [AOR:2.089,95% CI: (1.162 −3.755), p = 0.014].
Traditional medications are not well studied and have not passed through different clinical trials to be used widely to treat disease.Citation47 Using these medications could put patients in the position of “untreated indication” that the patient might have a disease not treated properly. It also has an effect on compliance since patients might hold or substitute their drug therapy thinking that the traditional medications would cure them.Citation48 In addition, traditional medications do not have scientifically known dose range, intervals, contraindications, and interactions. Therefore, during treatment of certain disease patients consume them inappropriately that could result in adverse events.Citation49 Patient education is important to avoid or minimize the use of traditional medications. As they are not well studied, patients might end up in complications as their conditions are not treated well. Patients who used such medication should undergo organ function tests and blood monitoring to prevent and treat any intoxication.Citation50
Furthermore, the current study showed that patients with a history of hospitalization experienced 4 times greater MRHA than patients without a hospitalization history [AOR: 4.001, 95% CI: (1.98–8.089), p < 0.001].
During hospitalization patients receive prescription medications according to their disease conditions. After an improvement, patients will be discharged from a hospital with their medications that are continued to be taken at home.Citation51 Having those medications, patients with a history of hospitalization could experience ADRs that might lead patients to be readmitted to hospitals.Citation52 In the present study most patients were noncompliant with their prescription drugs. These could result in poor disease prognosis causing the patients to be admitted to hospitals repeatedly.Citation53 Health care professionals should advise patients with a history of hospitalization to be adherent to their medication. Especially for patients with chronic disease conditions that discontinue medication upon feeling well. Patients should be reassured about possible ADRs to prevent drug discontinuation.Citation54 They should also be informed to seek medical advice and treatment for any of their health conditions.
Strength and Limitations of the Study
Efforts were made to assess the prevalence, patterns, and associated factors of MRHAs with quality data collection. Due to the fact that adults as well as African populations were assessed, the study population has heterogeneity concerns, which could affect generalizability. In addition, the submission of the work was late due to political instability that caused a loss of internet connection at the time of manuscript writing in the northern part of Ethiopia.
Conclusions
Medication-related hospital admission had a meaningful prevalence at the emergency ward of UoGcSH. Most MRHAs were identified to be definitely preventable noncompliance to prescribed medication followed by untreated indication and ADRs were the most common reason for MRHA. Renal impairment, chronic disease, history of traditional medication use and history of hospitalization were predictors of MRHA. The high prevalence could affect the quality of life of patients and the economic wellbeing of the health care setting.
Recommendations
To reduce MRHAs the hospital should give caution to health care professionals to provide patients appropriate mediation therapy. Rapid intervention should be given to patients who are admitted to the hospital due to medication-related problem. An emphasis should be given to pharmaceutical care as it would help in answering patients’ questions regarding drug-related needs. Incorporation of clinical pharmacists in hospital settings helps in prevention and identification of drug-related problems and minimize the number of patients that are admitted to hospitals related to medications. Health care professionals should educate patients about the importance of seeking medical treatment if there is an indication and mediation compliance. Health care providers should identify patient groups who are likely susceptible t to ADRs to adjust treatment choice accordingly. Patients need to be reassured about ADR of their prescribed medication. Health care providers should give a close follow-up to patients with renal impairment, chronic disease, a history of traditional medication use, and a history of hospitalization.
Abbreviation
ADRs, Adverse drug reactions; AOR, Adjusted odds ratio; DRPs, Drug-related problems; eGFR, Estimated glomerular filtration rate; MRHA, Medication-related hospital admissions; UoGcSH, University of Gondar comprehensive and specialized hospital; VIF, Variance inflation factor.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors would like to acknowledge the University of Gondar Comprehensive Specialized Hospital. The authors are also grateful to the data collectors, supervisors, and study participants for their contributions.
Data Sharing Statement
All relevant data are in the manuscript. Extra data which form the basis for this study are accessed upon reasonable request from the corresponding author.
References
- Nivya K, Kiran VSS, Ragoo N, Jayaprakash B, Sekhar MS. Systemic review on drug related hospital admissions–A PubMed based search. Saudi Pharm J. 2015;23(1):1–8. doi:10.1016/j.jsps.2013.05.006
- Ayalew MB, Tegegn HG, Abdela OA. Drug Related Hospital Admissions; A Systematic Review of the Recent Literatures. Bull Emerg Trauma. 2019;7(4):339–346. doi:10.29252/beat-070401
- Singh H, Kumar BN, Sinha T, Dulhani N. The incidence and nature of drug-related hospital admission: a 6-month observational study in a tertiary health care hospital. J Pharmacol Pharmacotherapeutics. 2011;2(1):17–20. doi:10.4103/0976-500X.77095
- Ni X-F, Yang C-S, Bai Y-M, Hu Z-X, Zhang -L-L. Drug-related problems of patients in primary health care institutions: a systematic review. Front Pharmacol. 2021;12:698907. doi:10.3389/fphar.2021.698907
- Ayele Y, Tesfaye ZT. Drug-related problems in Ethiopian public healthcare settings: systematic review and meta-analysis. SAGE Open Medicine. 2021;9:20503121211009728. doi:10.1177/20503121211009728
- Gustafsson M, Sjölander M, Pfister B, Jonsson J, Schneede J, Lövheim H. Drug-related hospital admissions among old people with dementia. Eur J Clin Pharmacol. 2016;72(9):1143–1153. doi:10.1007/s00228-016-2084-3
- Wu C, Bell CM, Wodchis WP. Incidence and economic burden of adverse drug reactions among elderly patients in Ontario emergency departments: a retrospective study. Drug Safety. 2012;35(9):769–781. doi:10.1007/BF03261973
- Repp KL, Hayes IIIC, Woods TM, Allen KB, Kennedy K, Borkon MA. Drug-related problems and hospital admissions in cardiac transplant recipients. Ann Pharmacother. 2012;46(10):1299–1307. doi:10.1345/aph.1R094
- Leendertse AJ, Van Den Bemt PM, Poolman JB, Stoker LJ, Egberts AC, Postma MJ. Preventable hospital admissions related to medication (HARM): cost analysis of the HARM study. Value Health. 2011;14(1):34–40. doi:10.1016/j.jval.2010.10.024
- Freitas G, Tramontina MY, Balbinotto G, Hughes DA, Heineck I. Economic impact of emergency visits due to drug-related morbidity on a Brazilian hospital. Value Health Reg Issues. 2017;14:1–8. doi:10.1016/j.vhri.2017.03.003
- Lim R, Ellett LMK, Semple S, Roughead EE. The extent of medication-related hospital admissions in Australia: a review from 1988 to 2021. Drug Safety. 2022;45(3):249–257. doi:10.1007/s40264-021-01144-1
- Oshikoya KA, Chukwura H, Njokanma OF, Senbanjo IO, Ojo I. Incidence and cost estimate of treating pediatric adverse drug reactions in Lagos, Nigeria. Sao Paulo Med J. 2011;129(3):153–164. doi:10.1590/S1516-31802011000300006
- Adem F, Abdela J, Edessa D, Hagos B, Nigussie A, Mohammed MA. Drug-related problems and associated factors in Ethiopia: a systematic review and meta-analysis. J Pharm Policy Pract. 2021;14(1):36. doi:10.1186/s40545-021-00312-z
- Jatau AI, Aung MMT, Kamauzaman THT, Rahman AFA. Prevalence of drug-related emergency department visits at a teaching hospital in Malaysia. Drugs. 2015;2(4):387–395. doi:10.1007/s40801-015-0045-2
- Distance from addis ababa to Gondar [Internet]. 2015–2022. Available from: https://www.distancecalculator.net/from-addis-ababa-to-gondar. Accessed July 1, 2024.
- Demessie MB, Berha AB. Prevalence and predictors of drug-related hospitalisation among patients visiting emergency departments of Addis Ababa city hospitals in Ethiopia: a multicentre prospective observational study. BMJ open. 2022;12(3):e054778. doi:10.1136/bmjopen-2021-054778
- Hallas J, Harvald B, Gram L, et al. Drug related hospital admissions: the role of definitions and intensity of data collection, and the possibility of prevention. J Internal Med. 1990;228(2):83–90. doi:10.1111/j.1365-2796.1990.tb00199.x
- Kemal LK, Shewaga TG. Drug-related hospital admissions and associated factors among adults admitted to felege hiwot comprehensive and specialized hospital. North West Ethiopia. 2022;2022:6767488.
- Kempen TG, Hedström M, Olsson H, et al. Assessment tool for hospital admissions related to medications: development and validation in older patients. Int J Clin Pharm. 2019;41(1):198–206. doi:10.1007/s11096-018-0768-8
- Lea M, Mowe M, Mathiesen L, Kvernrød K, Skovlund E, Molden E. Prevalence and risk factors of drug-related hospitalizations in multimorbid patients admitted to an internal medicine ward. PLoS One. 2019;14(7):e0220071. doi:10.1371/journal.pone.0220071
- Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hosp Pharm. 1992;27(6):538.
- Cockcroft DW, Gault H. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi:10.1159/000180580
- Aronoff GR. Dose adjustment in renal impairment: response from drug prescribing in renal failure. BMJ. 2005;331(7511):293–294. doi:10.1136/bmj.331.7511.293-a
- Daoud JI, editor Multicollinearity and regression analysis. In Journal of Physics: Conference Series; 2017: IOP Publishing.
- Vinutha H, Poornima B, Sagar B, editors. Detection of outliers using interquartile range technique from intrusion dataset. In Information and Decision Sciences: Proceedings of the 6th International Conference on FICTA; 2018: Springer.
- Castro I, Guardiola JM, Tuneu L, Sala ML, Faus MJ, Mangues MA. Drug-related visits to the emergency department in a Spanish University hospital. Int J Clin Pharm. 2013;35(5):727–735. doi:10.1007/s11096-013-9795-7
- Hailu BY, Berhe DF, Gudina EK, Gidey K, Getachew M. Drug related problems in admitted geriatric patients: the impact of clinical pharmacist interventions. BMC Geriatr. 2020;20(1):13. doi:10.1186/s12877-020-1413-7
- Linkens A, Milosevic V, Van Der Kuy P, Damen-Hendriks V, Mestres Gonzalvo C, Hurkens K. Medication-related hospital admissions and readmissions in older patients: an overview of literature. Int J Clin Pharm. 2020;42(5):1243–1251. doi:10.1007/s11096-020-01040-1
- Očovská Z, Maříková M, Kočí J, Vlček J. Drug-related hospital admissions via the department of emergency medicine: a cross-sectional study from the Czech Republic. Front Pharmacol. 2022;13:899151. doi:10.3389/fphar.2022.899151
- de Lemos J, Loewen P, Nagle C, et al. Preventable adverse drug events causing hospitalisation: identifying root causes and developing a surveillance and learning system at an urban community hospital, a cross-sectional observational study. BMJ Open Qual. 2021;10(1):e001161. doi:10.1136/bmjoq-2020-001161
- Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–286. doi:10.2147/TCRM.S1458
- Jayatilleke N, Hayes RD, Chang C-K, Stewart R. Acute general hospital admissions in people with serious mental illness. Psychological Medicine. 2018;48(16):2676–2683. doi:10.1017/S0033291718000284
- Dammalapati SG, Challa SR, Challa P, et al. Incidence and factors associated with drug related hospital admissions in a South Indian tertiary care hospital. Indian J Pharm Pract. 2018;11(1):37–43. doi:10.5530/ijopp.11.1.7
- Alghamdy MS, Randhawa MA, Al-Wahhas MH, Al-Jumaan MA. Admissions for drug-related problems at the emergency department of a university hospital in the Kingdom of Saudi Arabia. J Fam Med. 2015;22(1):44. doi:10.4103/2230-8229.149590
- Battineni G, Sagaro GG, Chinatalapudi N, Amenta F. Applications of machine learning predictive models in the chronic disease diagnosis. J Pers Med. 2020;10(2):21. doi:10.3390/jpm10020021
- McCorkle R, Ercolano E, Lazenby M, et al. Self‐management: enabling and empowering patients living with cancer as a chronic illness. Ca a Cancer J Clinicians. 2011;61(1):50–62. doi:10.3322/caac.20093
- Schatz S, Weber RJ. Adverse drug reactions. Pharm Pract. 2015;1(1):16.
- Khalili H, Farsaei S, Rezaee H, Dashti-Khavidaki S. Role of clinical pharmacists’ interventions in detection and prevention of medication errors in a medical ward. Int J Clin Pharm. 2011;33(2):281–284. doi:10.1007/s11096-011-9494-1
- Holm H, Bjerke K, Holst L, Mathiesen L. Use of renal risk drugs in patients with renal impairment. Int J Clin Pharm. 2015;37(6):1136–1142. doi:10.1007/s11096-015-0175-3
- Tesfaye WH, Wimmer BC, Peterson GM, et al. The effect of hospitalization on potentially inappropriate medication use in older adults with chronic kidney disease. Curr Med Res Opin. 2019;35(6):1119–1126. doi:10.1080/03007995.2018.1560193
- Dörks M, Allers K, Schmiemann G, Herget‐Rosenthal S, Hoffmann F. Inappropriate medication in non‐hospitalized patients with renal insufficiency: a systematic review. J Am Geriatr Soc. 2017;65(4):853–862. doi:10.1111/jgs.14809
- Alruqayb WS, Price MJ, Paudyal V, Cox AR. Drug-related problems in Hospitalised patients with chronic kidney disease: a systematic review. Drug Safety. 2021;1–18.
- Sevilla-Sanchez D, Molist-Brunet N, Amblàs-Novellas J, Roura-Poch P, Espaulella-Panicot J, Codina-Jané C. Adverse drug events in patients with advanced chronic conditions who have a prognosis of limited life expectancy at hospital admission. Eur J Clin Pharmacol. 2017;73(1):79–89. doi:10.1007/s00228-016-2136-8
- Williams A, Manias E, Walker R. Interventions to improve medication adherence in people with multiple chronic conditions: a systematic review. J Adv Nurs. 2008;63(2):132–143. doi:10.1111/j.1365-2648.2008.04656.x
- De Paepe P, Petrovic M, Outtier L, Van Maele G, Buylaert W. Drug interactions and adverse drug reactions in the older patients admitted to the emergency department. Acta Clinica Belgica. 2013;68(1):15–21. doi:10.2143/ACB.68.1.2062714
- Talebreza S, McPherson ML. Recognizing and managing polypharmacy in advanced illness. Med Clinics. 2020;104(3):405–413. doi:10.1016/j.mcna.2019.12.003
- Izzo AA, Hoon‐Kim S, Radhakrishnan R, Williamson EM. A critical approach to evaluating clinical efficacy, adverse events and drug interactions of herbal remedies. Phytother Res. 2016;30(5):691–700. doi:10.1002/ptr.5591
- Tulunay M, Aypak C, Yikilkan H, Gorpelioglu S. Herbal medicine use among patients with chronic diseases. J Intercultural Ethnopharmacol. 2015;4(3):217. doi:10.5455/jice.20150623090040
- Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;4:177. doi:10.3389/fphar.2013.00177
- Ifeoma O, Oluwakanyinsola S. Screening of herbal medicines for potential toxicities. New Insights Toxicity Drug Testing. 2013;244:63–88.
- Alper E, O’Malley TA, Greenwald J, Aronson M, Park L Hospital discharge and readmission. UpToDate Waltham: upToDate; 2017.
- Pedrós C, Quintana B, Rebolledo M, Porta N, Vallano A, Arnau JM. Prevalence, risk factors and main features of adverse drug reactions leading to hospital admission. Eur J Clin Pharmacol. 2014;70(3):361–367. doi:10.1007/s00228-013-1630-5
- Štrauch B, Petrák O, Zelinka T, et al. Precise assessment of noncompliance with the antihypertensive therapy in patients with resistant hypertension using toxicological serum analysis. J Hypertens. 2013;31(12):2455–2461. doi:10.1097/HJH.0b013e3283652c61
- Hughes L, Whittlesea C, Luscombe D. Patients’ knowledge and perceptions of the side‐effects of OTC medication. J Clin Pharm Therapeutics. 2002;27(4):243–248. doi:10.1046/j.1365-2710.2002.00416.x