 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
The purpose of this study is to evaluate how the benefits of online continuing medical education (CME) provided to health care professionals traveled along a patient “educational chain”. In this study, the educational chain begins with the influence that CME can have on the quality of health care, with subsequent influence on patient knowledge, disease self-management, and disease biomarkers.
Methods
A total of 422 patients with at least one noncommunicable disease (NCD) treated in eight different Mexican public health clinics were followed over 3 years. All clinics were participants in the CASALUD Model, an NCD care model for primary care, where all clinic staff were offered CME. Data were collected through a questionnaire on health care, patient disease knowledge, and self-management behaviors; blood samples and anthropometric measurements were collected to measure patient disease biomarkers.
Results
Between 2013 and 2015, the indexes measuring quality of health care, patient health knowledge, and diabetes self-management activities rose moderately but significantly (from 0.54 to 0.64, 0.80 to 0.84, and 0.62 to 0.67, respectively). Performing self-care activities – including owning and using a glucometer and belonging to a disease support group – saw the highest increase (from 0.65 to 0.75). A1C levels increased between 2013 and 2015 from 7.95 to 8.41% (63–68 mmol/mol) (P<0.001), and blood pressure decreased between 2014 and 2015 from 143.7/76.8 to 137.5/74.4 (systolic/diastolic reported in mmHg) (P<0.001). The mean levels of other disease biomarkers remained statistically unchanged, despite the improvements seen in the previous “links” of the educational chain.
Conclusion
Online CME can effect certain changes in the educational chain linking quality of health care, patient knowledge, and self-management behaviors. However, in order to assure adequate NCD control, the entire health care system must be improved in tandem. Online CME programs, such as CASALUD’s, are feasible strategies for impacting changes in disease self-management at a clinic level throughout a country.
Introduction
Mexico faces a critical epidemic of noncommunicable diseases (NCDs), especially type 2 diabetes mellitus (T2DM), lipid disorders, hypertension, and obesity. Unlike many common infectious diseases that Mexico faced in the past century, NCDs can only be managed and not cured with specific medication or therapy. However, it has been estimated that 95% of this NCD managementCitation1 is performed outside of medical settings, ie, during a patient’s day-to-day life. Although certain direct-to-patient lifestyle interventions have been successful, these interventions are difficult to implement effectively in routine primary care and yield heterogeneous results.Citation2
The question becomes how primary care clinics can empower, educate, and motivate patients to take an active role in the management of their NCD(s). It is well known that diabetes knowledge and health literacy are the cornerstone for making decisions on self-management; there is a significant association between T2DM knowledge and attitudes and self-care (blood glucose monitoring and diet).Citation3 Yet, it is still unclear if improved patient knowledge in and of itself is a sufficient condition to have an impact on lifestyles, healthy behaviors, and self-management activities.Citation4 It is even less clear if these have an impact on patient health outcomes.
It is also unclear logistically how health care professionals (HCPs) can increase patient knowledge and self-management activities within the context of primary care practice given current constraints. A significant challenge to improved patient knowledge is that the Mexican medical education system does not train future HCPs on educational communication, supporting healthy behavior strategies, or building egalitarian patient–provider relationships.Citation5
One comprehensive intervention that has attempted to permeate the primary health care level and overcome this HCP-training barrier is the CASALUD Model, described in detail elsewhere.Citation6 It is a primary care model created by the “Fundación Carlos Slim” [Carlos Slim Foundation]. The CASALUD Model was designed for state clinics operating with funding from “Seguro Popular”, the universal health insurance offered to all Mexican residents not covered by other public insurance systems.
CASALUD’s capacity-building pillar is carried out through the computer-based Online Interactive Platform for Health Education (called PIEENSO for its initials in Spanish). In general, physicians have shown improved satisfaction and knowledge with online continuing medical education (CME) programs that include interactivity, practice exercises, repetition, and feedback.Citation7 PIEENSO includes all of these components and is able to function with or without an Internet connection, allowing HCP access even in rural areas.
This CME program offers the following two certificates: a 110-hour Online Certificate, which updates HCP knowledge on NCDs and current evidence-based NCD prevention, treatment, and management strategies (including how to deliver diabetes self-management education [DSME]) and a Competencies Certification, a 40-hour course in which physicians solve real-life cases to test their knowledge in practical settings. As of May 2016, 224 HCPs from the two studied states had participated in CASALUD’s CME program by completing the Online Certificate and/or the Competencies Certification.
The objective of this study was to track how online CME provided to HCPs at primary health care centers (PHCs) through the CASALUD Model impacted the patient–provider “educational chain”. This chain, along with other factors that influence patient health, is shown in . Detailed descriptions of the components of each link in the chain can be found in the following section.
Figure 1 Educational chain and other factors that affect patient health.
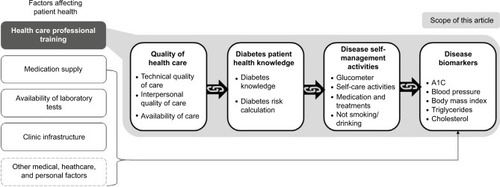
While CASALUD addresses issues with medication supply, availability of laboratory tests, clinic infrastructure, and of course HCP training, it is important to keep in mind that other medical, health care, and personal factors influence patient disease biomarkers. This article limits itself to exploring the educational chain that may theoretically connect HCP training with patient health.
The educational chain is defined as a series of conditions that begins with HCP training. This can prompt more co-responsible health care – understood as a relationship with equal responsibility between providers, patients, and the community – especially shared decision-making and DSME.Citation8 This improved health care brings about increased patient health knowledge, which is subsequently acted upon through healthier self-management activities. At the end of the educational chain, if all of the prior conditions are present, one might expect to see an improvement in patient health (measured through disease biomarkers). To test this hypothesis, patient disease biomarkers were also tracked over the course of the 3-year study in order to observe the effects that the educational chain might have had on patient health.
Methods
A total of 422 patients participated in an observational, 3-year longitudinal study. The purpose of the study was to observe the influence of the online CME delivered through the capacity-building pillar of CASALUD on the quality of health care, patient knowledge, disease self-management activities, and patient disease biomarkers. This study was not designed to be a representative sample of all CASALUD clinics in Mexico; rather, the objective was to closely follow a group of patients receiving care through the CASALUD Model in order to better understand their experiences.
The group of patients included in this study was defined in close consultation with participant PHCs: eight PHCs from two central Mexican states where the CASALUD Model had been implemented. First, the participant PHCs proposed a list of all active seekers of PHC health care services with a previous diagnosis of at least one NCD (T2DM, hypertension, or a lipid disorder). Of the patients on these lists, clinic HCPs invited all patients who were contactable to participate in this study; if a patient requested further details, he or she was contacted by study researchers. This strategy was followed until the sample size was reached. The sample size was designed to permit the detection of changes of 0.5% in glycated hemoglobin (A1C) levels at a confidence level of 95% while taking possible desertions into account.
Patients were excluded if they moved out of the study area, were no longer covered under the studied health system (Seguro Popular), withdrew consent, passed away, or were otherwise unable to attend data collection events. They were considered lost to follow-up if they were not contactable or failed to present at a PHC during data collection events, despite numerous attempts to contact.
Data collection began in April 2013, when patients signed informed consent; follow-up surveys occurred during April–May 2014 and 2015, when patients gave verbal assent. Participants were provided with the results and interpretation of all laboratory tests, as well as a complimentary breakfast on the day of data collection.
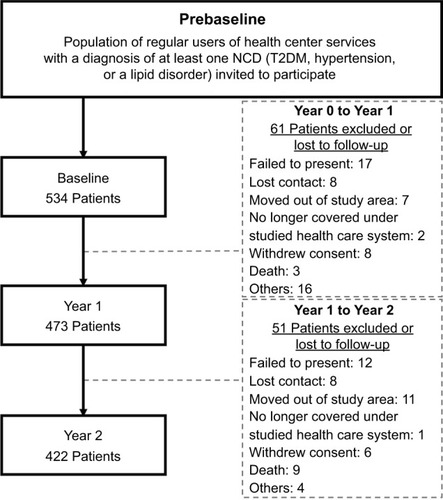
Sixty-one participants were lost to follow-up or excluded between 2013 and 2014, and 51 participants between 2014 and 2015, slightly >20% of the originally recruited participants (). Patients reporting kidney failure at any point during data collection were eliminated from the study, as national guidelines call for these patients to be referred to secondary care. As CASALUD is a general primary care model and does not contemplate patients with severe complications, these patients should not fall under the CASALUD Model.
Figure 2 Patient flow diagram.
Abbreviations: NCD, noncommunicable disease; PHC, primary health care center; T2DM, type 2 diabetes mellitus.
Although all patients were analyzed together, they were also grouped by individual disease; detailed criteria on group composition are available in Table S1.
Data for the first three links in the educational chain were collected with a questionnaire designed to capture perceptions of health care, diabetes patient health knowledge, and self-reported disease self-management activities. In the questionnaire, one group of questions corresponded to perceived quality of health care, one group of questions corresponded to patient disease knowledge, and one group of questions corresponded to chronic disease self-management activities. Each of these groups was further divided into subgroups. Perceived quality of care was divided into three subgroups: technical quality of care, interpersonal quality of care, and availability of care, while patient disease knowledge was divided into T2DM risk calculation and T2DM knowledge. The last group of T2DM self-management activities was divided into glucometer, medication and treatments, self-care activities, and no tobacco/alcohol use.
Indexes were created with the concept of unidimensional distance; values are presented on a scale ranging from 0 to 1, where 0 is the complete absence of affirmative responses to that set of questions and 1 means that all patients responded affirmatively. The questions used to define each group or subgroup, along with a more detailed description of how the indexes were constructed, can be found in Tables S2–S4.
Blood samples were collected to measure A1C, triglycerides, and cholesterol, which were all analyzed by photometry with a cobas c 111 analyzer. Blood pressure measurements were performed using an Omron Brand Automatic Blood Pressure Monitor, weight was measured using the Camry EB9015 scale, and height and waist circumference were measured using a PRETUL Tape Measurer. Blood pressure, height, and weight were measured twice, or three times in the case of discrepancy.
Results
The average age of participants at the beginning of data collection was 56.3 years. In line with gender distribution of the general patient population in Seguro Popular PHCs,Citation9 the group of participants was also predominantly female (81.8%). Descriptive (age) and frequency (gender and socioeconomic level) variables are presented in . The majority of the participants were classified as belonging to lower (D, 46.9%) or lower-middle socioeconomic levels (D+, 23.7%). Socioeconomic levels were measured with criteria defined by the Mexican Association of Marketing Research and Public Opinion Agencies (AMAI, in Spanish). The AMAI instrument uses 13 questions on educational attainment, household conditions, and ownership of certain belongings – such as a personal computer and automobile – in order to classify households into one of the five levels.
Table 1 Sociodemographic characteristics at study commencement
The vast majority of the participants (83.2%) met the International Diabetes Federation criteria for metabolic syndrome at the beginning of the study,Citation10 as shown in Table S5. This speaks to a population of complicated comorbidities. Indeed, at baseline, only 43.3% of patients with T2DM had their disease under control (A1C <7% or 53 mmol/mol). Many patients with T2DM had a long-term diagnosis, having been diagnosed either between 5 and 10 years (24.0%) or >10 years (31.8%) prior to the study.
Change in indexes was measured through a repeated measures analysis of variance (ANOVA), which tests for changes over time in a single population.Citation11 This test revealed that some indexes of each link of the educational chain remained relatively stable throughout the 3 years, while clear increases were observed in certain subgroups and groups. These changes are described below and presented visually in –, with descriptive and analytic statistical information presented in .
Table 2 Changes in Indexes 2013–2015 with repeated measures analysis of variance
Figure 3 Quality of health care.
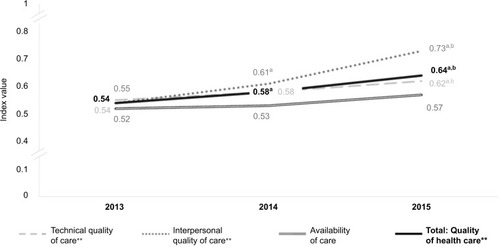
Figure 4 Diabetes patient health knowledge.

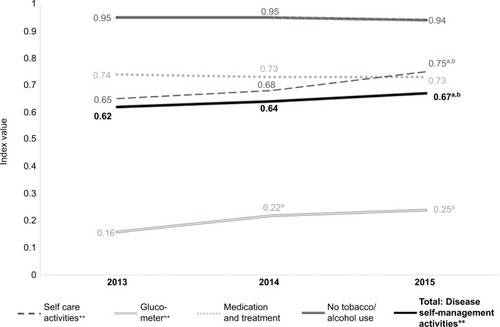
Figure 5 Disease self-management activities.
The perceived quality of health care was the group of indicators that saw the most statistically significant increases in aggregate, as well as in the majority of its subgroups (shown in ). The subgroup that saw the most improvement was interpersonal quality of care, which comprised four questions directed toward patient–provider communication and shared decision-making. During the timeframe that CASALUD’s CME program was implemented (2013–2015), this index rose from 0.54 to 0.73 (P<0.001). Technical quality of care also increased significantly during this same time period. Due to these important increases, the total group score rose significantly from 0.54 to 0.64 in the 2 years following the implementation of the CASALUD’s online CME program (P<0.001).
Improvements in indicators of quality of health care were reflected in patient health knowledge: the overall group score increased moderately but significantly from 0.80 at baseline to 0.84 at Year 2 (P<0.001). Both subgroups, T2DM knowledge and T2DM risk calculation, increased in the greatest proportion between 2013 and 2014 (). The proportion of patients correctly reporting that T2DM is a risk factor for blindness, stroke, amputation, and other common complications was high at the commencement of the study and increased further.
Moving to the next link in the chain, the overall group index of diabetes self-management activities rose from 0.62 in 2013 to 0.67 in 2015 (P<0.001), as shown in . Most important was the fact that significantly more patients reported owning and using a glucometer, as well as participating in self-care activities. The subgroup of self-care activities comprised exercising, following a healthy eating plan, checking their own bare feet, involving their family in care, and belonging to a peer support group at their PHC. Self-reported medication adherence and abstention from tobacco and alcohol were high at study commencement and remained stable throughout the study period.
The disease biomarker average, in general, remained unchanged over the course of the study. No significant changes were observed in lipid levels or in the percentage of patients with this diagnosis who had their disease under control. Although average body mass index (BMI) did not change significantly, the percentage of patients who were able to lose enough weight to fall within a normal range was important: 10.3% of participants who began with BMI >30 were able to move below that level by 2015 (P<0.001).
The mean levels of two types of disease biomarkers changed significantly: A1C levels and blood pressure. A1C levels increased between 2013 and 2015 from 7.95 to 8.41% (63–68 mmol/mol) (P<0.001), and the percentage of patients with A1C >7% (53 mmol/mol) decreased from 43.3% to 34.0% (P<0.001). As a reference, people with diabetes on constant monotherapy typically experience an increase in A1C levels of ~1% every 2 years.Citation12 Blood pressure decreased significantly between 2014 and 2015 from 143.7/76.8 to 137.5/74.4 (systolic/diastolic reported in mmHg). Detailed numbers by year are presented in , and further discussion on the significance of these findings is included in the following section.
Table 3 Patient disease biomarkers
Discussion
While other articles have explored individual connections between HCP education, quality of care, patient knowledge, disease self-management activities, and disease biomarkers, this is, to our knowledge, the first paper to present these categories as a chain. We propose this theoretical structure in order to better identify why certain studies have found connections between categories and others have not. While this chain has not yet been validated, the authors hypothesize that each link may have a significant impact on the links further down the chain (as shown in ).
Figure 6 Hypothesized linkages between health care, health knowledge, self-management activities, and disease biomarkers (with observed statistically significant changes)

The strongest increases in indicators were seen in the quality of health care (technical quality of care and interpersonal quality of care). This is not surprising, as CASALUD’s capacity-building pillar focuses on aligning the care provided in Seguro Popular clinics with Mexican federal government standards of care and clinical practice guidelines. This pillar is also heavily concentrated on instilling the importance of patient-centered care and patient co-responsibility. While there is no clear definition of interpersonal quality of care in the literature yet,Citation13 it is clear that communication and shared decision-making have an important impact on patient treatment adherence and therapeutic behavior changes.Citation14
Levels of knowledge regarding T2DM care (such as target A1C levels) were low at baseline, and rose significantly by Year 2. Improvements in quality of health care – including DSME, provider communication, and shared decision-making – may have led to this significant increase in T2DM knowledge. The PIEENSO courses specifically train HCPs on how to deliver DSME to their patients, and the authors propose that DSME was an important intermediate link between quality of health care and diabetes patient health knowledge.
Patient health knowledge was acted on, as seen in the significant improvements in the overall group of disease self-management activities. The most important increases were seen in owning and using a glucometer and participating in self-care activities. Perceived and objective quality of care can have an important impact on patients’ self-management abilities. In this case, increased medical quality, specifically DSME and joint patient–provider decision-making, may prompt patients to take a greater role in their own disease management. Indeed, regular intervention built on existing, longstanding primary care relationships may have a significant impact on patientsCitation15 and patient–provider relationships have been shown to have a direct impact on T2DM management attitudes and adherence to diet and exercise plans.Citation16
While positive results were seen in the first three links of the chain, this was not reflected in significant changes in biomarkers across all variables. This is in line with other studies that have attempted to train primary care providers in delivering DSME and lifestyle interventions. While these studies typically find great improvements in provider satisfaction, knowledge, and practice change, there is little existing evidence on how online HCP CME can affect patient outcomes.Citation7 Indeed, a systematic review found that the strength of evidence between care quality, patient health literacy, and self-management was insufficient for glycemic control and low for hypertension.Citation4 Significantly, 83% of our study population had metabolic syndrome, only 44% of patients with T2DM had their disease under control, and 56% had been diagnosed with T2DM over 5 years prior to the study. Patients with longstanding chronic diseases tend to respond less (in terms of biomarkers) to lifestyle interventions.Citation17
Improvements in blood pressure drew our attention, and other Mexican authors studying NCDs in Seguro Popular clinics have noted a similar phenomenon: control of blood pressure is more common than control of diabetes.Citation18 Anecdotal reports from HCPs suggest that blood pressure drugs are better stocked in the PHC pharmacies and of higher quality than available glucose-lowering medications. Hypertension can also be more sensitive to diet and physical activity: the ENCORE study saw improvements of 16.1 mmHg in systolic blood pressure with diet alone.Citation19
The lack of statistically significant positive improvements in other disease biomarkers, especially A1C, has been observed in multidisciplinary interventions. The impact of long-term patient education (>6 months) delivered by HCPs in a primary care setting on NCD disease outcomes is still not completely understood.Citation13,Citation20 Training nurses, and even specialized therapists and multidisciplinary teams, on broad educational interventions is generally not able to sustain improvements in biomarkers between treatment and control groups of diabetes patients.Citation21 This is because, in order to see results in a specific educational chain, educational programs should be targeted and disease specific instead of more generalized “lifestyle” educational programs. This was demonstrated by the recent CASCADE and DEPICTED studies, which tested group education programs for physicians and pediatric clinics to improve long-term glycemic control in their patients, without observing significant differences.Citation22,Citation23 Most importantly, it has been shown that HCPs require continual feedback and technical support to maintain the skills learned through training sessions.Citation24 Online CME linked to DSME may be the best option to train HCPs on disease-specific education and training, so that persons with diabetes can maintain the benefits of this training in the long term.
Time plays an important role in disease biomarkers, and it is possible that 2 years was too short of a time period to begin to see significant changes.Citation25 While a systematic review on multifactorial lifestyle interventions found no consistent effects on disease biomarkers in the short term, they did find differences in longer term outcomes, such as cardiac events and mortality.Citation2 Interestingly, the lack of significant differences in disease biomarkers may be losing importance in the current discourse. A new wave of authors is starting to question the value of solely focusing on disease biomarkers, especially A1C, as this can cause overmedication and poly-pharmacy, with associated side effects.Citation26,Citation27 Even if complications are reduced through tight A1C control, they may not be clinically significant (as in the case of retinopathy).Citation28 Rather, newer interventions should focus on improving quality of life and reducing complications as well as overall costs to health care systems.Citation21
The principal limitation of this study is the uneven implementation of the CASALUD Model. For example, not all medical providers took the Online Certificate at the same time – 79% signed up in 2013 and the rest in 2014 and 2015. Another important limitation was the lack of a control group and the fact that those participants who were lost to follow-up were not included in this study. Significant differences (P<0.001) were found between “completers” and “deserters”, with geographical differences and more men in the deserter group (the completer group was 81.8% female while the deserter group was 64.3% female). However, no differences were found in their responses to the questionnaire or biomarkers, which leads us to conclude that the results presented here were not swayed by their withdrawal from the study. Additionally, the authors recognize a possible source of bias in how the first three links in the chain were tracked: as this was a general study of CASALUD and patients’ time was limited, more extensive monitoring of diet, physical activity, and drug adherence (eg, with specialized instruments) was not possible. The first three links in the chain were therefore monitored with self-reports, which means that these data could contain a degree of response bias, specifically social desirability bias. In the same vein, it was not possible to measure how HCPs educated individual patients or which treatment guidelines they used to treat individual patients. This includes prescribing behavior or NCD management strategies, including what criteria physicians used to prescribe glucose-lowering drugs/insulin, statins, and blood pressure-lowering medication to their patients.
Implications
This study has shown the feasibility of using an online CME program, such as the CASALUD Model’s PIEENSO platform, to deliver HCP education at a clinic level throughout a country. This is of great significance, as CME that trains on comprehensive educational and patient-focused interventions may be one of the most viable options to address NCDs and other lifestyle diseases at the primary care level. Other authors have shown that the quality of online CME is non-inferior to in-person CME and is a viable option, especially for lesser-developed regions where traveling to live CME events may be complicated.Citation29 CME programs’ relative low cost, ability to be completed at HCPs’ convenience, and accessibility make them even more attractive.
Online CME programs are also more easily converted into ongoing training programs, which are crucial to maintaining consistently high-quality NCD management. Due to high HCP turnover and a need for continuous feedback, one-time training programs on general lifestyle interventions should be converted into continual training programs. Online programs such as the capacity-building pillar of CASALUD could be integrated into ongoing PHC human resources training to assure full coverage and better serve the clinical environment.
This study shows that online CME for HCPs can effect specific changes in the educational chain linking quality of health care, patient knowledge, and self-management behaviors. This is the first study to present the impact of online CME on the entire educational chain, as well as on disease biomarkers. Importantly, this article puts forth the theory that the impact of educational chains on patient disease biomarkers is multidimensional: factors unrelated to CME can also affect or even confound the results of educational interventions.
Supplementary materials
Index construction with three evaluated groups and their nine subgroups
Variables were dichotomous dummy variables; the aggregated sum was obtained for each of the three groups and the corresponding nine subgroups using the following formula:
Table S1 Criteria to define diagnosis of NCD
Table S2 Patient health knowledge
Table S3 Disease self-management activities
Table S4 Perception of quality of medical care
Table S5 The IDF consensus worldwide definition of the metabolic syndrome
Author contributions
RT-C and RM-R designed the CASALUD Model and its innovations, conceived the study, and helped to draft the manuscript. HG-R designed the CASALUD Model and its innovations, conceived the study, participated in its design and coordination, and helped to draft the manuscript. RS-M designed the CASALUD Model and its innovations, conceived the study, participated in its design and coordination, and drafted the manuscript. EL and AI performed critical revision of the manuscript and provided valuable feedback during the study design. PK-M supervised the study execution and provided administrative and technical support. BT-B helped to design the study, designed the logistics for data acquisition, provided supervision, and helped to draft the manuscript. UQ-G helped to design the study, designed the logistics for data acquisition, coordinated the study, designed the statistical analysis plan, and helped to draft the manuscript. ERA helped to design the study, participated in the analysis and interpretation of data, and drafted the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
At the national level, Jesús Felipe González-Roldán, General Director at CENAPRECE, and Gabriela Ortíz, Director at CENAPRECE, were key allies in supporting the implementation and evaluation of CASALUD. And, although we cannot enlist everyone by name here, we appreciate the support shown by the Mexican public health system staff along the way. At the state level, Martina Pérez, Director of Health Services, Jorge Octavio García, Director of Health Policy and Quality, and Jurisdiction Program Directors Ma. de la Paz Herrera and Violeta Nidia Acosta proved invaluable in coordinating with clinics and local authorities. Implementation of the CASALUD Model at health care clinics was made possible with the support of their directors, Carlos Castellanos, Miguel Ramírez, Alma Martell, María González, Tania Alomia del Río, Juana Martínez, Juan Saldaña, Georgina Sánchez, and Gloria Vázquez. We are indebted to the patients and health care workers who so graciously participated in tracing studies and interviews at their health care clinics. We would like to acknowledge the significant contribution of Vicente Sotelo and Micaela Mussini to the analysis of the data used in this study and Craig Waugh for his valuable comments on this document. Finally, many thanks go out to our field research team, Christian García, Rayénari Gurrola, Ana Laura Islas, América Ruiz, and Víctor Nolasco, whose tireless data collection efforts made this study possible. The research on the CASALUD Model reported in this publication was supported by the NCD Partnership of Eli Lilly.
Disclosure
RT-C, HG-R, RS-M, and RM-R are employed full time by the Fundación Carlos Slim. PK-M currently serves as Deputy Secretary for Prevention and Health Promotion at the Mexi-can Ministry of Health. EL and AI are employed full time by the Lilly Global Health, of Eli Lilly and Company. BT-B, UQ-G, and ERA are employed full time by C230 Consultores. The authors report no other conflicts of interest in this work.
References
- Funnell M Helping patients take charge of their chronic illnesses Fam Pract Manag 2000 7 3 47 51 10947289
- Angermayr L Dieter M Klaus L Multifactorial lifestyle interventions in the primary and secondary prevention of cardiovascular disease and type 2 diabetes mellitus – a systematic review of randomized controlled trials Ann Behav Med 2010 40 1 49 64 20652464
- Kueh YC Morris T Borkoles E Shee H Modelling of diabetes knowledge, attitudes, self-management, and quality of life: a cross-sectional study with an Australian sample Health Qual Life Outcomes 2015 13 1 1 11 25608461
- Al Sayah F Majumdar S Williams B Robertson S Johnson J Health literacy and health outcomes in diabetes: a systematic review J Gen Intern Med 2013 28 3 444 452 23065575
- Tapia-Conyer R Gallardo-Rincón H Saucedo-Martínez R Innovaciones para la transformación de los sistemas de salud. [Casalud: innovations for the transformation of health systems] Gac Méd Méx 2012 148 567 571 Spanish 23254716
- Tapia-Conyer R Gallardo-Rincón H Saucedo-Martinez R CASALUD: an innovative health-care system to control and prevent non-communicable diseases in Mexico Perspect Public Health 2015 135 4 180 190 24285554
- Thepwongsa I Kirby CN Schattner P Piterman L Online continuing medical education (CME) for GPs: does it work? A systematic review Immunology 2014 43 10 717 721
- Taskforce to Strengthen Co-Responsibility among Primary Healthcare Users and Provider A Call for Co-Responsibility: Shifting the Healthcare Paradigm for Diabetes Management Mexico City Fundación Carlos Slim, The Lilly NCD Partnership, Fundació IDEA 2015 12 Available from: http://fundacionidea.org/assets/files/Call_forCo-responsibility.pdf Accessed June 22, 2016
- Ortiz Espinosa RM Muñoz Juárez S Martín del Campo DL Torres Car-reño E Consulta externa en instituciones de salud de Hidalgo, México, según la opinión de los usuarios. [The quality of outpatient services in health facilities in Hidalgo, Mexico, from the users’ perspective] Rev Panam Salud Pública 2003 13 229 238 Spanish 12804152
- International Diabetes Federation The IDF Consensus Worldwide Definition of the Metabolic Syndrome Brussels, Belgium International Diabetes Federation 2006 10 Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome Accessed July 15, 2017
- Kim H-Y Statistical notes for clinical researchers: a one-way repeated measures ANOVA for data with repeated observations Restor Dent Endod 2015 40 1 91 95 25671219
- Fonseca VA Defining and characterizing the progression of type 2 diabetes Diabetes Care 2009 32 suppl 2 S151 19875543
- Cramm JM Nieboer AP Chronically ill patients’ self-management abilities to maintain overall well-being: what is needed to take the next step in the primary care setting? BMC Fam Pract 2015 16 1 1 8 25608667
- Travaline JM Ruchinskas R D’Alonzo GEJr Patient-physician communication: why and how J Am Osteopath Assoc 2005 105 1 13 18 15710660
- Peckham S Falconer J Gillam S webpage on the Internet Evidence on effectiveness of health improvement activities undertaken in general practice and primary care The Organisation and Delivery of Health Improvement in General Practice and Primary Care: A Scoping Study 29 Chap. 6 Southhampton, UK NIHR Journals Library, Health Services and Delivery Research 2015 Available from: http://www.ncbi.nlm.nih.gov/books/NBK299616/ Accessed July 15, 2017
- Maddigan SL Majumdar SR Johnson JA Understanding the complex associations between patient-provider relationships, self-care behaviours, and health-related quality of life in type 2 diabetes: a structural equation modeling approach Qual Life Res 2005 14 6 1489 1500 16110929
- Ewenighi CO Uchechukwu D Adejumo BI Responses to glycemic control therapy according to age, gender, level of adiposity, and duration of diabetes in type 2 diabetic patients Indian J Med Sci 2013 67 3 and 4 61 69 Available from: http://imsear.li.mahidol.ac.th/bitstream/123456789/149553/1/ijms2013v67n3p61.pdf Accessed July 15, 2017 24231394
- Ortiz-Domínguez ME Garrido-Latorre F Orozco R Pineda-Pérez D Rodríguez-Salgado M Sistema de Protección Social en Salud y calidad de la atención de hipertensión arterial y diabetes mellitus en centros de salud. [Quality of health care for diabetic and hypertensive patients in primary care settings servicing Mexican Seguro Popular] Salud Pública Méx 2011 53 436 444 Spanish 22282206
- Hinderliter AL Sherwood A Craighead LW The long-term effects of lifestyle change on blood pressure: one-year follow-up of the ENCORE study Am J Hypertens 2014 27 5 734 741 24084586
- Cooper H Booth K Fear S Gill G Chronic disease patient education: lessons from meta-analyses Patient Educ Couns 2001 44 2 107 117 11479051
- Harvey J Psychosocial interventions for the diabetic patient Diabetes Metab Syndr Obes 2015 8 29 43 25657590
- Robling M McNamara R Bennert K webpage on the Internet The effect of the talking diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study) BMJ 2012 344 e2359 Available from: http://www.bmj.com/content/344/bmj.e2359.abstract Accessed July 15, 2017 22539173
- Christie D Thompson R Sawtell M Structured, intensive education maximising engagement, motivation and long-term change for children and young people with diabetes: a cluster randomised controlled trial with integral process and economic evaluation – the CASCADE study Health Technol Assess 2014 18 20 1 202
- Jansink R Braspenning J Keizer E van der Weijden T Elwyn G Grol R No identifiable Hb1Ac or lifestyle change after a comprehensive diabetes programme including motivational interviewing: a cluster randomised trial Scand J Prim Health Care 2013 31 2 119 127 23659710
- Holman RR Paul SK Bethel MA Matthews DR Neil HAW 10-year follow-up of intensive glucose control in type 2 diabetes N Engl J Med 2008 359 15 1577 1589 18784090
- King P Peacock I Donnelly R The UK prospective diabetes study (UKPDS): clinical and therapeutic implications for type 2 diabetes Br J Clin Pharmacol 1999 48 5 643 648 10594464
- Curtiss FR Looking for the outcomes we love in all the wrong places: the questionable value of biomarkers and investments in chronic care disease management interventions J Manag Care Pharm 2008 14 6 563 570 18693781
- Nathan DM DCCT/EDIC Research Group The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview Diabetes Care 2014 37 1 9 16 24356592
- Lockyer J Sargeant J Curran V Fleet L The transition from face-to-face to online CME facilitation Med Teach 2006 28 7 625 630 17594554
