?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
According to the International Diabetes Federation, total global health care expenditures for diabetes tripled between 2003 and 2013 because of increases in the number of people with diabetes as well as in the average expenditures per patient. This study aims to provide accurate and timely information about the economic impacts of type 2 diabetes mellitus (T2DM) in Vietnam.
Method
The cost-of-illness estimates followed a prospective, prevalence-based approach from the societal perspective of T2DM with 392 selected diabetic patients who received treatment from a public hospital in Ho Chi Minh City, Vietnam, during the 2016 fiscal year.
Results
In this study, the annual cost per patient estimate was US $246.10 (95% CI 228.3, 267.2) for 392 patients, which accounted for about 12% (95% CI 11, 13) of the gross domestic product per capita in 2017. That includes US $127.30, US $34.40 and US $84.40 for direct medical costs, direct nonmedical expenditures, and indirect costs, respectively. The cost of pharmaceuticals accounted for the bulk of total expenditures in our study (27.5% of total costs and 53.2% of direct medical costs). A bootstrap analysis showed that female patients had a higher cost of treatment than men at US $48.90 (95% CI 3.1, 95.0); those who received insulin and oral antidiabetics (OAD) also had a statistically significant higher cost of treatment compared to those receiving OAD, US $445.90 (95% CI 181.2, 690.6). The Gradient Boosting Regression (Ensemble method) and Lasso Regression (Generalized Linear Models) were determined to be the best models to predict the cost of T2DM (R 2=65.3, mean square error [MSE]=0.94; and R 2=64.75, MSE=0.96, respectively).
Conclusion
The findings of this study serve as a reference for policy decision making in diabetes management as well as adjustment of costs for patients in order to reduce the economic impact of the disease.
Introduction
Diabetes mellitus is a rapid-onset, chronic, noncommunicable disease that causes many serious complications, such as a decrease in quality of life, and is a major cause of death in most countries.Citation1,Citation2 In 1980, there were 108 million people living with diabetes, and this number had quadrupled by 2014.Citation2,Citation3 The World Health Organization estimated in 2014 that there were 422 million people over the age of 18 (8.5%) with diabetes mellitus worldwide, putting the risk of death from diabetes 3.3 times higher than human immunodeficiency virus/acquired immune deficiency syndrome and tuberculosis and 8.3 times higher than malaria.Citation1,Citation2,Citation4 In 2015, 5 million people had died of diabetes or complications from diabetes worldwide, an alarming 14% increase from just 3 years earlier.Citation1,Citation4 Based upon this rate, the International Diabetes Federation (IDF) has predicted that by 2040, one in 10 people will have diabetes, with one in 11 people contracting it during that time period.Citation1
Diabetes mellitus is a chronic disease that occurs when the body is unable to produce enough insulin or cannot use insulin.Citation5 The diagnosis of diabetes mellitus is clinical and is based on multiple measurements of blood glucose; the condition is further classified into one of the three major types of diabetes, including type 1, type 2, and gestational diabetes.Citation6,Citation7 The most common form of diabetes is type 2 diabetes mellitus (T2DM), with 91% in high-income countries being diagnosed with it.Citation8–Citation11 Although manifestations of the disease are difficult to identify in their early stages, with many cultural and social changes, the indications of the disease are more conspicuous.Citation1,Citation12–Citation14 Individuals diagnosed with diabetes mellitus suffer not only from the dangerous health-related complications but also from significant financial burdens associated with the treatment and lifelong management of the disease progression.Citation15 Based on a cost estimate from the 2015 statistics with 5 million deaths from the disease, around 673–1197 billion US dollars (USD) were spent on medical expenses from treatment of illness to death and with 827 billion USD as the annual direct medical fees.Citation1,Citation3,Citation16
According to the IDF, total global health care expenditures for diabetes have tripled between 2003 and 2013 as a result of an increase in the number of people with diabetes as well as the average health care expenditure for the treatment of diabetes.Citation17 This increase is expected to grow exponentially in the coming years, especially for those with low and middle incomes, and the cost of treatment for diabetes in low and middle countries will be more burdensome than high-income countries.Citation1 In the USA, the estimated total cost of treatment for diabetes in 2012 was $245 billion USD, including $176 billion USD for direct medical expenses and $69 billion USD for losses because of reduced productivity.Citation18 As Vietnam is a low-income developing country,Citation19 its incidence of diabetes is increasing at an alarming rate, nearly doubling in the past 10 years.Citation20 Pham estimated that at present, one in every 20 people is diagnosed with diabetes.Citation21 In addition, the number of people with prediabetes has also increased significantly to three times as many as for people with diabetes.Citation20 By the end of 2015, Vietnam had 63,021 cases of diabetes, representing 5.6% of people aged 20–79 years, of whom 53,457 died.Citation22 Pham also estimated that by 2035, the incidence of diabetes and prediabetes will increase to 7% and 15.7%, respectively.Citation21 In Vietnam, the average treatment cost per diabetic patient was $162.7 USD in 2015, which is more than the $150 USD per capita monthly average.Citation22 However, no studies on the cost of treatment of diabetes in Vietnam are available.Citation15 This study endeavors to present treatment costs from a societal perspective and also provide accurate and timely information about the economic impacts of T2DM in Vietnam.
Methods
Study design
In this cross-sectional study, the cost-of-illness estimates follow the sum-all cost and prevalence-based approach from a societal perspective, with selected diabetic patients who received treatment from a public hospital in Ho Chi Minh City of Vietnam in the 2016 fiscal year.Citation23,Citation24 The sum-all medical cost method involves adding all the medical costs of providing care to a patient, regardless of whether the cost was directly related to the disease or not.Citation25 Incorporation with a prevalence-based approach yields a general picture of the economic burden as well as component costs to provide better management reference for policymakers to manage the disease.Citation26
Data collection
This was a cross-sectional study of T2DM patients who had received care in a public government hospital in 2016. The data are taken from the patient’s medical records, which are located in the hospital’s electronic database along with the demographic characteristics from the face-to-face interview. From this, the necessary data are synthesized to develop a model of treatment costs. Patients with T2DM are identified using the International Classification of Diseases Revision, tenth revision (ICD-10 code) with disease diagnosis code E11. Diabetes complications and comorbidities are also identified using ICD-10.
As the hospital examination period is once a month, a simple random sampling will be performed within a month (i.e., the number of patients in the day will be randomly selected with generating random numbers following a code line in Python random.choice([0, 1]), with the output equal 1 being selected and vice versa). This study included patients who qualified for all of the following two criteria such as 1) assigned ICD-10 code of E11; 2) attended treatment for T2DM for 1 year in this facility. Patients with type1 diabetes and women with gestational diabetes were excluded.
Estimation of costs
Cost-of-illness estimates in this study were incidence-based from a societal perspective, and hence considered all costs, irrespective of who incurred them. The costs consisted of direct costs and indirect costs.Citation27
Direct costs
Direct costs include direct medical cost and direct nonmedical cost. In this study, direct medical costs are classified as medical care costs (visits and emergency care as well as procedures performed by medical personnel), diagnosis, pharmaceuticals, operation, and medical supplies. To standardize direct medical costs, the study uses reference unit costs of medical services in Vietnam from the study of Vo et al.Citation28 Because Vo et al’s investigation was conducted in 2014, all unit costs will be changed to their 2017 values .Citation29 Self-reported illness-related cost items, such as meals (special food or diabetic supplements), transportation, accommodation, and informal care costs, were collected from patients and their family members and were considered direct nonmedical costs.
Indirect costs
The indirect costs associated with diabetes include workdays missed because of health conditions (absenteeism), reduced work productivity while working because of health conditions (presenteeism), reduced workforce participation due to disability, and productivity lost because of premature mortality.Citation30–Citation32 To estimate the indirect costs, this study uses the human capital method,Citation26 as follows:
Absenteeism: the number of workdays missed because of poor health.Citation33 The study recorded the total number of days off for routine medical visits as well as days off because of sickness based upon information provided by patients.
Presenteeism: reduced productivity while at work,Citation33 which is generally measured through worker responses to surveys. However, their responses are not entirely accurate because workers, especially laborers, depend on daily productivity for their income. Consequently, the productivity loss associated with diabetes-attributed presenteeism was determined using an estimate (14 days per worker with diabetes per year).Citation34
Unemployment: reduced productivity for those not in the workforce, which was defined as the reduction in people not in the workforce in personal activities, includes time spent providing child care, household activities, and other tasks, such as volunteering in the community.Citation33 This population includes all adults under 65 years of age who are not employed. The earnings of patients were multiplied by a factor of 75% to account for those not in the workforce.Citation34
Data analyses and statistical methods
Cost data are typically highly skewed because a few patients incur particularly high costs.Citation35,Citation36 Such problems were handled using the nonparametric double bootstrap-t method to calculate the 95% CIs as well as the significant differences between means (with a 95% significance level).Citation37,Citation38 Consequently, cost data are represented as an arithmetic mean (bootstrap 95% CI) cost to make that information available for decision makers.Citation36,Citation39 All costs were measured in terms of Vietnamese currency (dong [₫]) and converted to USD using the exchange rate of $1 USD=₫22,708.6.Citation29
Microvascular complications include diabetic retinopathy, diabetic nephropathy, and diabetic neuropathy, while macrovascular complications include cardiovascular and coronary artery diseases.Citation40 The study excluded comorbidities with a prevalence of <5%. The Chi-square test was performed to compare statistically significant differences in the prevalence of complications and comorbidities among men and women. Statistically significant correlations between the prevalence of comorbidities and complications associated with patient age were assessed with the Spearman’s rank correlation coefficient (ρ). Descriptive statistics (frequency, percentage, mean, median, 25th–75th interquartile) were used to summarize demographic information, clinical status, and component expenditures of the data.
A two-way sensitivity analysis was conducted to find the variance of total treatment costs when the two hypothetical values (cost lost because of “Presenteeism” and “Unemployment”) changed (“Presenteeism” is between 5.5 and 33.5 days,Citation41 and the “Unemployment” rate of the average earnings is 65%–85%).
This study applied machine learning algorithms to determine the fittest model for prediction and also to identify the factors affecting the direct medical costs of T2DM. Those algorithms compared the precision using the R 2-score and the mean square error (MSE). Direct medical costs and continuous value features (age, blood glucose level, number of comorbidities, body mass index [BMI], and disease duration), which did not have a Gaussian distribution, were transformed using the Box–Cox method,Citation42,Citation43 and then all continuous value features were scaled with a standardization method to convert the data from differences in measured units to the scaling factor (z-score).Citation44,Citation45 This study labeled the category variables (gender, health insurance status, marriage status, education, occupation, monthly income, drinking, smoking, exercising, relatives’ T2DM history, treatment, and type of complications) with a value between 0 and n-1 (Supplementary material).
All statistical analyses were performed using Python version 3.5 (Anaconda platform 4.4.0).Citation46,Citation47
Ethical consideration
Written informed consent was obtained from adult participants and their caregivers who were involved in the study, before the specimen collection and the questionnaire survey began. The research protocol was approved by the Biomedical Research Ethics Council at the District 9 Hospital in Ho Chi Minh City, Vietnam, and also the University of Medicine and Pharmacy in Ho Chi Minh City, Vietnam (IORG0007145).
Results
Patient characteristics
Data collected from 392 patients with T2DM were statistically analyzed according to the most common characteristic. The mean (SD) age of the patients was 65.14 (13.45) years, and participants were divided into six groups according to age. Those from 60 to 69 years of age made up the largest group, accounting for 30.4% of the sample. In addition, female patients were nearly twice as likely as males (66.6% and 33.4%, respectively) to have T2DM. Most patients reported having been diagnosed with T2DM for at least 6–10 years (36.7%); the rate of patients with disease duration from 1–5 years or ≥21 years is very low (2.6% and 2.0%, respectively).
The proportion of patients with blood glucose levels 131–179 mg/dL was the highest at 42.9%. Moreover, 69.6% of participants reported having diabetes complications, while those with comorbidities accounted for 97.4% of the total number of patients included in the survey. The vast majority of inpatients (88.0%) had different levels of health insurance coverage; the most common (80.4% of participants) had 80% health insurance coverage. A middle-school education level was most prevalent (60.2%), as was a monthly income of $200 USD (53%) ().
Table 1 Socio-demographic and clinical characteristics of patients with diabetes mellitus in Vietnam (2016, n=392)
Prevalence of complications and comorbidities
The proportion of types of complications and number of comorbidities included were significantly different between men and women with T2DM (p=0.002; p=0.006, respectively). Similarly, the majority of comorbidities were statistically significantly different between males and females with T2DM, with a higher proportion of females reporting comorbidities than males, except for those with hypertension (p=0.434), liver diseases (p=0.058), or spondylitis (p=0.057).
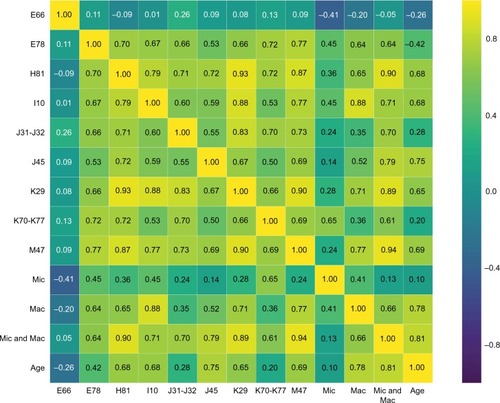
Furthermore, in terms of the correlation between the prevalence of complications, with the exception of microvascular ones, patients with other complications had statistically significant correlations with patient age, such as I10-hypertension and J45-asthma (ρ=0.68, p=0.029; ρ=0.75, p=0.013; respectively) ().
Table 2 Prevalence of complications and comorbidities among patients with T2DM in Vietnam (2016, n=392)
Spearman’s analysis also indicates that the association between comorbidities and complications is associated with hypertension and vestibular disorders with increasing age (ρ=0.79). The same relationship was observed between vestibular disorders and gastritis/duodenitis (ρ=0.93) and hypertension and macrovascular complications (ρ=0.88) (). shows the correlation coefficient matrix of the Spearman test between the prevalence of complications and comorbidities associated with patient age.
Annual treatment costs associated with sociodemographic characteristics, complications, and comorbidities
The proportion of cost components varies depending on groups of each characteristic. However, it can be seen that direct costs (including direct medical costs and direct nonmedical costs) is almost higher compared to indirect costs. Moreover, in most cases, the direct medical cost is about three to four times higher than direct nonmedical cost. Intuitively, the direct medical cost of patients with treatment of oral antidiabetics (OAD) is US $ 117.4 (95% CI 102.1, 135.7), while the latter is US $42.7 (95% CI 20.7, 88.3). Direct medical costs of macrovascular complications have the smallest arithmetic mean at US $ 81.8 (95% CI 50.9, 131.1), while the largest arithmetic mean is M47-spondylosis at US $ 240.2 (95% CI 199.1, 292.5). Direct nonmedical costs have an arithmetic mean ranging from 31.0 to 36.0. The indirect cost for treating macrovascular disease has the smallest arithmetic mean US $ 80.3 (95% CI 67.1, 95.1). Indirect costs for patients with liver diseases have the largest arithmetic mean value (US $91.0, bootstrap 95% CI 80.5, 105.4) ().
Table 3 Details of total cost per annum in USD for management of diabetes in Vietnam (2016, USD)
The bootstrap analysis was conducted to identify statistically significant differences in treatment costs associated with the characteristics of patients. Of all the characteristics described, only BMI and lifestyle had no difference in total cost between each group. For age group, the average cost difference was statistically significant; specifically, the average cost of patients aged 60–69 years was higher than the 40–49 years group, the 50–59 years group, and the ≥80 years group. The average cost of the 40–49-year-old age group was higher than that of the 70–79 age group at US $94.1 (95% CI 19.8–165.9). Female patients had a higher cost of treatment than men with $48.9 USD (3.1, 95.0). Patients with a T2DM duration of ≥21 years had significantly higher treatment costs than those who had a T2DM duration between 6 and 10 years and 11–15 years, which were US $81.0 (95% CI 24.2, 135.3) and US $78.9 (95% CI 23.3, 140.3), respectively. When classified according to blood glucose level, the treatment cost of the 70–130 mg/dL group was lower than the other two groups and is statistically significant. Patients who used insulin and OAD had a statistically significant higher cost of treatment compared to those receiving OAD at US $445.9 (95% CI 181.2, 690.6) ().
Table 4 Mean cost statistically significantly difference between groups in Vietnam (2016, USD)
Annual costs of diabetes
Direct medical costs accounted for the highest proportion of total costs at 51.7%, while direct nonmedical costs made up only 14.0%; indirect costs accounted for 34.3% of the total. Of all the costs of direct medical costs, the cost of pharmaceuticals accounted for the highest proportion (27.5%), the cost of operation was lower (12.5%), and medical care and diagnoses and medical supplies (4.6%, 4.9%, and 2%, respectively) comprised a very low proportion. Similarly, in indirect cost categories, “Absenteeism” costs accounted for the highest rate of 20.9%, while “Presenteeism” cost and “Unemployment” costs were low (8.7% and 4.7%, respectively). In general, the average annual cost of treatment for a person with T2DM is US $246.1 (228.3, 267.2), while average annual direct medical costs total US $127.3 (111.3, 147.1); expenditures are US $34.4 (30.9, 8.3) for average annual direct nonmedical costs and US $84.4 (78.8, 91.1) for indirect costs ().
Sensitivity analysis
The results of the two-way sensitivity analysis revealed that the total indirect costs ranged from US $27,388.80 (−17.3%) to US $45,407.20 (+37.2%). In addition, when the average indirect costs varied from US $69.90 to US $115.80, the average total cost of treatment ranged from US $231.60 to US $277.50. Thus, the change in the average total cost of treatment when the two variables of indirect cost estimates fluctuated remained within the 95% CI of the mean total cost of treatment estimated by the study.
Machine learning algorithms to predict T2DM treatment costs
The Gradient Boosting Regression and the Lasso Regression are the two best machine learning regression algorithms for predicting annual direct medical costs (R 2=65.42, MSE=0.938; and R 2=64.32, MSE=0.968, respectively) with a Box–Cox transformation and the total direct medical costs (with lambda=0.024) (). The optimal model (Gradient Boosting Regression) identified seven factors that contribute to the cost of diabetes: number of comorbidities (0.42), age (0.23), health insurance status (0.1), duration of illness (0.09), type of treatment (0.07), blood glucose level (0.07), and type of complication (0.02).
Discussion
This prevalence-based cost-of-illness study involved a targeted-group population that was generated from cost and administrative data retrieved from the Government Public Hospital on patients with T2DM in Vietnam. The annual cost per patient estimate in this study was US $246.10 (95% CI 228.3, 267.2), which accounted for about 12% (95% CI 11, 13) of the gross domestic product (GDP) per capita in 2017. Of this cost per patient, US $127.30, US $34.40, and US $84.40 were spent on direct medical costs, direct nonmedical costs, and indirect costs, respectively. These expenses seem lower than those reported in other Asian and Southeast Asian countries. According to a 2008 study in Thailand, the average cost treating a diabetes patient was estimated at US $881.47 (20% of the GDP per capita in 2008),Citation48 while a study of the economic costs of diabetes in Iran reported a cost of US $544.00 (accounting for 17% of the GDP per capita in 2005).Citation49 A Chinese study reported costs of US $1,707.80 (45% of the GDP per capita in 2009) to manage each patient with T2DM.Citation50 It is notable that the direct medical costs reported by high-income countries, such as Singapore or nations in the Americas and Europe, are much higher.Citation33,Citation35,Citation51,Citation52 In addition, the indirect cost in this study was recorded as US $84.40 (78.80, 91.10); absenteeism costs accounted for 60.9% of this cost. This finding indicated that the correlation between the number of workdays missed significantly influences the indirect costs; one possible explanation for this is that the indirect costs in the study were lower than those reported by other studiesCitation15 because the GDP per capita in Vietnam is lower than that of most other countries.
In terms of cost components, pharmaceuticals accounted for the bulk of the total expenditures in our study (27.5% of the total costs and 53.2% of the direct medical costs), which suggests that patients with T2DM are aware of the importance of treating the disease, as demonstrated by their compliance with prescribed prescription medications. In contrast with the findings of other studies, the second most expensive component of our total costs was medications.Citation33,Citation35,Citation49,Citation52 The present study also found that patients in the insulin and OAD group had higher treatment costs; some other studies also reported similar results.
Patients with poor glycemic control and associated diseases (hypertension, hyperlipidemia, and obesity) had higher treatment costs than those in the other groups, which was in agreement with the findings of another study.Citation48 In addition, more highly educated people have lower treatment costs, which may be because more educated people are likely to maintain a healthy lifestyle while monitoring and treating their disease from its onset, while the average and less educated people are often uninterested in the disease until the onset of complications, so that the cost of treatment for severe illness is high.
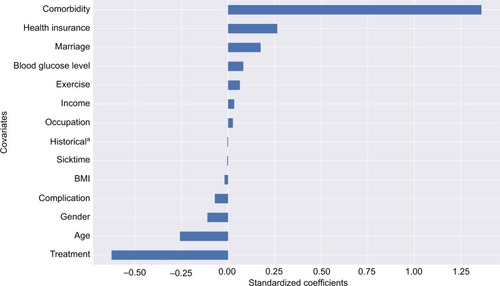
Machine learning algorithms generally provide almost the same results in predicting the cost of treatment, but only two algorithms can eliminate factors that do not directly affect the cost of treatment, namely the Gradient Boost Regression and the Lasso Regression. The former algorithm yields the highest accuracy and identifies important features in estimating the costs, such as the number of comorbidities (0.42), age (0.23), health insurance status (0.1), the duration of illness (0.09), type of treatment (0.07), blood glucose level (0.07), and type of complications (0.02) (). However, this algorithm is difficult to explain and is complex for nonexperts.Citation53 Therefore, the Lasso Regression algorithm is a better choice when presenting at nonprofessional seminars. It selects 15 of 17 features to estimate the annual direct medical cost; the regression is shown in with the significant factors that influence the costs, and the regression formula is shown below:
Figure 2 The percentage of covariances that contribute to the cost of treatment. aHistory of Type 2 diabetes of relative.
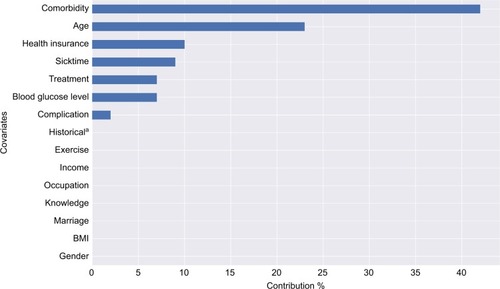
Figure 3 Standardized coefficient of Lasso Regression covariates
Abbreviation: BMI, body mass index.
As a prevalence-based cost-of-illness study from a social perspective, the strength of this study was to estimate the average annual T2DM treatment cost per case, as well as the cost of treatment for specific disease groups, especially those with different comorbidities. Moreover, the study used a variety of machine learning algorithms for a more in-depth and accurate analysis, especially in the era of technological development science, which many developing countries are using step by step to apply management data to electronics. The application of machine learning algorithms and data science knowledge to large data sources will help decision makers adopt more appropriate and effective policies for the management of diabetes. Nevertheless, this research study has several limitations that must be pointed out. First, the direct nonmedical costs and indirect costs were estimated using the subjective opinion of the patient. For this reason, they may have been inaccurate. Second, the direct medical costs were estimated using a source of unit cost reference that led to bias. Finally, the sample was small and, therefore, cannot represent the entire population of Vietnam. Future research on public health facilities will help to minimize these shortcomings.
Conclusion
This is the first study to provide a comprehensive cost analysis of the cost of treating diabetes in Vietnam. The results indicate that the numbers of comorbidities and also the selected treatment type significantly affect the cost of treatment. With the increase in the incidence of diabetes along with obesity, diabetes will continue to be a burden on health budgets. In addition, new technology has simplified data management and analysis, and the application of data analysis techniques will make disease research more effective and accurate. Research is, therefore, an important step for other studies in Vietnam to help policymakers better manage diabetes as well as adjust the costs of the disease to reduce the long-term economic burden of the increasing pandemic.
Acknowledgments
The authors would like to show their appreciation to Ms Nguyen Thi Thu Ha for her kind help in this study. Additionally, we would like to thank the board of directors and the hospital staff of the Public Government Hospital for offering the great opportunity for us to conduct our research at their sites.
Disclosure
The authors report no conflicts of interest in this work.
References
- International Diabetes Federation IDF diabetes atlas 2015
- World Health Organization Global report on diabetes 2016
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants Lancet 2016 387 10027 1513 1530 27061677
- World Health Organization Global Health Observatory data repository 2015 Available from: http://apps.who.int/gho/data/node.main Accessed February 2, 2017
- Alberti KGMM DeFronzo RA Zimmet P International text-book of diabetes mellitus New York, NY J. Wiley 1997
- American Diabetes Association Standards of medical care in diabetes 39 Diabetes Care 2016 Available from: http://care.diabetes-journals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf
- World Health Organization Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia 2006 Available from: http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf
- Bruno Graziella RC Cavallo-Perin P Merletti F Incidence of type 1 and type 2 diabetes in adults aged 30–49 years Diabetes Care 2005 28 11 2613 2619 16249528
- Evans JM Newton RW Ruta DA MacDonald TM Morris AD Socio-economic status, obesity and prevalence of Type 1 and Type 2 diabetes mellitus Diabet Med 2000 17 6 478 480 10975218
- Holman N Young B Gadsby R Current prevalence of Type 1 and Type 2 diabetes in adults and children in the UK Diabet Med 2015 32 9 1119 1120 25962518
- Boyle JP Thompson TJ Goldschmid MG Estimating prevalence of type 1 and type 2 diabetes in a population of African Americans with diabetes mellitus Am J Epidemiol 1999 149 1 55 63 9883794
- World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013–2020 2013 Available from: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf
- World Health Organization Global status report on noncommunicable diseases 2015 2015 Available from: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf
- Srinivasan B Taub N Khunti K Davies M Diabetes: glycaemic control in type 2 BMJ Clin Evid 2008 6 09
- Seuring Till AO Suhrcke M The economic costs of type 2 diabetes: a global systematic review Pharmacoeconomics 2015 33 8 811 831 25787932
- Evelyn Wong Backholer K Gearon E Harding J Freak-Poli R Stevenson C Peeters A Diabetes and risk of physical disability in adults: a systematic review and meta-analysis Lancet Diabetes Endocrinol 2013 1 2 106 114 24622316
- Florencia A Alex B Nam HC IDF diabetes atlas Leonor G Tim N Jessica B Ute L Olivier J Basel, Switzerland International Diabetes Federation 2013
- American Diabetes Association Economic costs of diabetes in the US in 2012 Diabetes Care 2013 36 4 1033 1046 23468086
- The World Bank Vietnam Data Available from: http://www.worldbank.org/vi/country/vietnam Accessed February 12, 2017
- World Health Organization/Western Pacific Region The growing burden of diabetes in Viet Nam 2016 Available from: http://www.wpro.who.int/vietnam/mediacentre/features/feature_world_health_day_2016_vietnam/en/ Accessed February 12, 2017
- Pham NM Prevalence and determinants of diabetes and prediabetes among Vietnamese adults Diabetes Res Clin Pract 2016 113 116 124 26795973
- International Diabetes Federation Western Pacific Diabetes in Vietnam 2015 2015 Available from: http://www.idf.org/membership/wp/vietnam
- World Health Organization WHO guide to identifying the economic consequences of disease and injury 2009 Available from: http://www.who.int/choice/publications/d_economic_impact_guide.pdf
- Tarricone R Cost-of-illness analysis: what room in health economics? Health Policy 2006 77 1 51 63 16139925
- Onukwugha E McRae J Kravetz A Varga S Khairnar R Mullins CD Cost-of-illness studies: an updated review of current methods Pharmacoeconomics 2016 34 1 43 58 26385101
- Changik J Cost-of-illness studies: concepts, scopes, and methods Clin Mol Hepatol 2014 20 4 327 337 25548737
- Kobelt G Health economics, economic evaluation, and glaucoma J Glaucoma 2002 11 6 531 539 12483101
- Trung QV Huong TN Riewpaiboon A Hospital service cost analysis in developing countries: a method comparison in Vietnam In press 2016
- Bank TW Vietnam 2017 Available from: http://data.worldbank.org/country/vietnam Accessed June 27, 2017
- Cawley J Rizzo JA Haas K The association of diabetes with job absenteeism costs among obese and morbidly obese workers J Occup Environ Med 2008 50 5 527 534 18469621
- Fu AZ Qiu Y Radican L Wells BJ Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions Diabetes Care 2009 32 12 2187 2192 19729528
- Lee LJ Yu AP Cahill KE Direct and indirect costs among employees with diabetic retinopathy in the United States Curr Med Res Opin 2008 24 5 1549 1559 18416887
- American Diabetes Association Economic costs of diabetes in the US in 2012 Diabetes Care 2013 36 4 1033 1046 23468086
- American Diabetes Association Economic costs of diabetes in the US in 2007 Diabetes Care 2008 31 3 596 615 18308683
- Ng CS Toh MPHS Ko Y Joyce YCL Direct medical cost of type 2 diabetes in Singapore PLoS One 2015 10 3 e0122795 25816299
- Barber JA Analysis and interpretation of cost data in randomised controlled trials: review of published studies BMJ 1998 317 7167 1195 1200 9794854
- Desgagne A Castilloux AM Angers JF LeLorier J The use of the bootstrap statistical method for the pharmacoeconomic cost analysis of skewed data Pharmacoeconomics 1998 13 5 487 497 10180748
- Efron B Tibshirani RJ An introduction to the bootstrap USA CRC Press 1994
- Thompson SG How should cost data in pragmatic randomised trials be analysed? BMJ 2000 320 7243 1197 10784550
- Fowler MJ Microvascular and macrovascular complications of diabetes Clin Diabetes 2008 26 2 77 82
- Png ME Yoong J Phan TP Wee HL Current and future economic burden of diabetes among working-age adults in Asia: conservative estimates for Singapore from 2010–2050 BMC Public Health 2016 16 1 153 26880337
- Chaze JP Assessing household health expenditure with Box–Cox censoring models Health econ 2005 14 9 893 907 16127678
- Gregori D Petrinco M Bo S Desideri A Merletti F Pagano E Regression models for analyzing costs and their determinants in health care: an introductory review Int J Qual Health Care 2011 23 3 331 341 21504959
- Edward JJ A user’s guide to principal components 587 USA John Wiley & Sons 2005
- Mohamad IB Usman D Standardization and its effects on K-means clustering algorithm Res J Appl Sci Engineer Technol 2013 6 17 3299 3303
- Pedregosa F Varoquaux G Gramfort A Scikit-learn: machine learning in Python J Mach Learn Res 2011 12 2825 2830
- Van Rossum G Drake FLJr Python tutorial Centrum voor Wiskunde en Informatica Amsterdam The Netherlands 1995
- Susmita C Arthorn R Piyanuch P Cost of diabetes and its complications in Thailand: a complete picture of economic burden Health Soc Care Community 2011 19 3 289 298 21276105
- Esteghamati A Khalilzadeh O Anvari M The economic costs of diabetes: a population-based study in Tehran, Iran Diabetologia 2009 52 8 1520 1527 19475364
- Wang W McGreevey WP Fu C Type 2 diabetes mellitus in China: a preventable economic burden Am J Manag Care 2009 15 9 593 601 19747024
- Leśniowska J Schubert A Wojna M Skrzekowska-Baran I Fedyna M Costs of diabetes and its complications in Poland Eur J Health Econ 2014 15 6 653 660 23820625
- Ingrid K Eduard H Hans H Ingrid S Direct costs of diabetes mellitus in Germany–CoDiM 2000–2007 Exp Clin Endocrinol Diabetes 2011 119 06 377 385 21264804
- Guido S Muller AC Introduction to machine learning with Python: a guide for data scientists USA O’Reilly Media 2017