Abstract
Background
The Awareness of Abdominal Adiposity as a Cardiometabolic Risk Factor Study assesses the prevalence of cardiometabolic risk factors in adults with abdominal obesity (waist circumference ≥90 cm in men and ≥80 cm in women) and evaluates how physicians manage these patients.
Methods
This is an observational cross-sectional study. Internists, cardiologists, and endocrinologists contributed patients to the study. A standardized questionnaire was completed and registered demographics, anthropometric measurements, lab results from the medical files, and any treatment utilized to manage dyslipidemia, arterial hypertension, diabetes, and cardiovascular disease.
Results
A total of 1312 patients was included. The mean age was 49.3 ± 14.6 years and 834 (63.6%) were female. The primary reason for the physician consultation was treatment of obesity (47.5%), followed by management of arterial hypertension (27.7%), diabetes (18.3%), dyslipidemia (14.2%), and cardiovascular disease (7.1%). The majority of patients identified excess body weight as a health problem (81.4%). However, patients had lost a mean of 4.3 ± 3.5 kg. Only 63.4% of patients with arterial hypertension were on drug therapy. Few of them had reached target values for diastolic (24.1%) and systolic/diastolic (13.3%) pressure. Less than half of the patients with dyslipidemia were receiving lipid-lowering medication. Only 32.2% were at their target low-density lipoprotein cholesterol levels. In patients with type 2 diabetes, mean fasting plasma glucose level (8.9 ± 3.4 mmol/L) was above the threshold recommended by current guidelines.
Conclusions
The study describes the medical care given to individuals with abdominal obesity during daily clinical practice by general practitioners, cardiologists, and endocrinologists in urban Mexico. Our data confirm that a large proportion of patients are undertreated. Only a small percentage of patients with obesity-related comorbidities reach treatment targets. Interventions proven to be effective in the prevention of chronic complications have in general not been implemented.
Introduction
The importance of abdominal adiposity as a marker for chronic nontransmissible diseases is well established.Citation1 Increased waist circumference is a component of several diagnostic criteria for the metabolic syndrome.Citation2–Citation4 This clinical parameter is considered a standard of care for the adult population.
Until recently, the evidence supporting the importance of abdominal adiposity has been derived from studies in European and North American populations.Citation5 The thresholds used in Caucasians lack sensitivity for the detection of type 2 diabetes and lipid disorders in non-Caucasian subjects.Citation6 Multiple papers in Asian, Hispanic, and other ethnic groups provide conflicting results regarding the diagnostic proficiency of waist circumference.Citation7–Citation9 Despite this, the majority accept that this variable is a useful marker for the identification of several chronic diseases.Citation10
Few papers have evaluated the pattern of care received by patients with abdominal obesity.Citation11 The aim of this study is to document the pattern of care received by subjects with abdominal adiposity under the management of cardiologists, endocrinologists, and primary care physicians.
Patients and methods
The Awareness of Abdominal Adiposity as a Cardiometabolic Risk Factor Study is a survey designed to assess the prevalence of cardiometabolic risk factors in a cohort of subjects with increased waist circumference. In addition, the study aims to evaluate how physicians manage these patients. Data were collected prospectively from adults in eight countries (Argentina, Chile, Colombia, Egypt, Lebanon, Mexico, Saudi Arabia, South Africa). Here, we report the results of the patients studied in Mexico.
The participating hospitals and clinics provided a list of the active specialists in their outpatient clinics. Internists (n = 32), cardiologists (n = 42), and endocrinologists (n = 41) were randomly selected from this list and invited to participate in the study. All physicians had previously participated in clinical trials. They were asked to invite the first patient scheduled for consultation that fulfilled the inclusion/exclusion criteria during a one-month period. Only one patient could be included per consulting day.
This is an observational study. The inclusion criteria of the study were outpatients ≥18 years old with abdominal obesity (defined by a waist circumference ≥90 cm for men and ≥80 cm for women as recommended by the International Diabetes FederationCitation4). The exclusion criteria included participation in other clinical studies, a life expectancy less than a year, conditions causing an increased abdominal circumference not related to excess adiposity (eg, ascitis, pregnancy), recent admission to a hospital, difficulty understanding the questionnaire, or unwillingness to participate.
A standardized questionnaire was completed. The questionnaire consisted of two sections: one filled in by the physician and the other answered by the patient. It included documentation of demographics, anthropometric measurements (ie, weight, height, waist, hip and neck circumference, and body mass index), lab results from the medical file, and any treatment utilized to manage dyslipidemia, arterial hypertension, diabetes, and cardiovascular diseases. In addition, concomitant medications, smoking habits, and alcohol consumption were also included. Anthropometric measurements were done using standardized procedures. Blood pressure was measured in a seated position. The mean of two readings obtained after a resting period of at least 10 minutes between measurements was used for the analyses.
High blood pressure was defined as a value ≥140/90 mmHg or use of antihypertensive medication. The diagnostic threshold was lowered to ≥130/80 in patients with type 2 diabetes. Dyslipidemia was defined as any of the following abnormalities: low-density lipoprotein cholesterol (LDL-c) ≥2.6 mmol/L, total cholesterol ≥5.2 mmol/L, triglycerides ≥1.6 mmol/L, or high-density lipoprotein cholesterol (HDL-c) ≤ 1.1 mmol/L in males and ≤1.3 mmol/L in females. Type 2 diabetes was diagnosed using the American Diabetes Association’s criteria.Citation12
The human research ethics committee of the participating institutions approved the study, and informed consent was obtained from all subjects.
Statistical analyses
The number of patients to be included in each physician group (cardiology, endocrinology, or primary care physician/internists) was 384. As a result, 1200 patients were expected to be studied in each country. Normally distributed data, determined using the Kolmogorov–Smirnov test, were expressed as means and standard deviation (±SD), whereas variables with a skewed distribution were reported as median (min–max). McNemar’s Chi Square, Student’s paired t-test or Wilcoxon’s test was used as appropriate for comparison between the basal characteristics and the information at follow-up visits. Kruskal–Wallis analysis was used to evaluate significant differences between specialties. Logistic regression analyses was used to identified independent factors associated with dyslipidemia, hypertension, fasting plasma glucose, type 2 diabetes, cardiovascular diseases, and two or more of these cardiovascular risk factors. All analyses were performed with SAS (v 8.2; SAS Institute, Inc, Cary, NC).
Results
Participating physicians
A total of 105 physicians participated in the study. They were primary care/internists (n = 32, 28.7%), cardiologists (n = 42, 36.5%), or diabetologists/endocrinologists (n = 41, 35.7%). Their mean age was 48.4 ± 8.9 years and 74% (n = 84) were male. The age (P = 0.89), time in practice (P = 0.76), the number of patients seen per month (P = 0.07), and the number of patients seen for obesity/overweight (P = 0.93) per month did not differ significantly between groups ().
Table 1 Basal characteristics of physicians evaluated in the study
Patients
A total of 1312 patients was included. The mean age was 49.3 ± 14.6 years and 834 (63.6%) were female. Of the study sample, 384 (29.3% of the study sample), 428 (32.6%), and 500 (38.1%) patients consulted the internists or primary care physicians, cardiologists, and endocrinologists/diabetologists respectively ().
Table 2 Basal characteristics of patients
The primary reason given by the patients for the physician consultation was treatment of obesity (n = 623, 47.5%), followed by management of arterial hypertension (n = 363, 27.7%), diabetes (n = 240, 18.3%), dyslipidemia (n = 186, 14.2%), and cardiovascular disease (n = 93, 7.1%). Some (n = 331, 25.4%) gave two or more reasons for consultation. The patient’s follow-up under their current physician was greater than five years in 167 (12.8%), less than five years in 653 (50.2%), and 481 (37%) were seen for the first time. Patients requiring treatment of obesity (64%) or diabetes (27%) primarily consulted endocrinologists. Those that consulted cardiologists were seeking therapy for arterial hypertension (56%), dyslipidemia (21%), or cardiovascular disease (17%). Cardiometabolic risk factors rarely occur individually. There was a significant overlap between diabetes, dyslipidemia, and arterial hypertension.
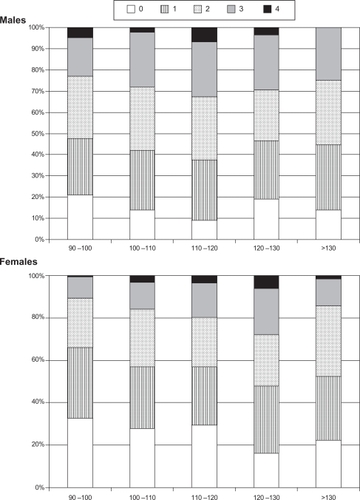
The number of cardiovascular risk factors did not increase significantly with increasing waist circumference (). However, in women, the prevalence of diabetes (13%–36%, P = 0.001) and hypertension (41.3%–62.2%, P = 0.01) was shown to increase with abdominal adiposity.
Prevalence and management of cardiometabolic risk factors
Obesity
The majority of the participants were either overweight or obese. Only 3% of men and 4% of women had a body mass index (BMI) < 25 kg/m2. The mean BMI for males and females was 31.99 ± 5.01 and 32.66 ± 5.71 kg/m2, respectively. The prevalence of obesity was higher in women compared to men (65.1% vs 61.2%, P = 0.05). Ten percent of participants had a BMI ≥ 40 kg/m2. Neck circumference was recorded in 96.1% (n = 1261) of the study sample, respectively. Men had a significantly greater neck circumference compared to women (42.4 ± 3.6 cm vs 37.0 ± 3.4 cm, P < 0.001). In contrast, the waist circumference was larger in women (113.2 ± 12.3 vs 110.5 ± 11.3 cm, P < 0.001).
Excess body weight was identified as a health problem by the majority of patients (81.4%). More than half (65.2%) had sought medical attention for this problem on at least one occasion. About half (48.4%) had made significant efforts to lose weight during the previous three months. This feature was more common among patients seeing an endocrinologist (P = 0.002). No difference in weight loss occurred between specialist groups.
The majority of the patients (89%) had the intention to follow a dietary program with or without the advice of their physician. The endocrinologist asked patients to follow a dietary program more often than other specialists (79.6% vs 61.9%, P < 0.001). The endocrinologists prescribed the dietary program themselves to about half their patients and requested the participation of a nutritionist in 33.2% of cases. The other health professionals were less likely to give dietary advice or seek the advice of a nutritionist ().
Table 3 Summary of the interventions stratified by physician specialty
The majority of patients (84%) were asked to increase their level of physical activity. The physicians themselves prescribed the physical activity program in close to 40% of patients from all three physician groups. No differences were observed between groups, in the percentage of patients exercising and the duration of physical activity at baseline. Weight control drugs were used by a small percentage of the patients (12.1%); sibutramine (5.4%) was most popular, followed by orlistat (2.5%). Less than one-quarter of the patients on weight control medication had been on it for more than three months; this percentage did not vary between specialist groups.
High blood pressure
The prevalence of high blood pressure was 63.4% (n = 703). The agreement between physician-diagnosis and patients recalled for arterial hypertension was moderate (kappa = 0.62). High blood pressure was diagnosed 5.9 ± 7.2 years before inclusion into the study. Patients under the care of the cardiologists had significantly higher systolic and diastolic pressures (P < 0.001, ). Only 63.4% of patients with high blood pressure were receiving drug therapy. At the time of evaluation, few of them had reached target values for diastolic (24.1%) and systolic/diastolic (13.3%) pressure. The most frequent antihypertensive drugs were angiotensin II receptor blockers, diuretics, beta-blockers, and calcium channel blockers. Their use did not differ between specialists.
Dyslipidemia
The prevalence of dyslipidemia was 60.4% (n = 703) (). The agreement between physician-diagnosis and patients recalled for dyslipidemia was low (kappa = 0.36). Plasma lipid levels were available in 78% of the patients. The primary care physicians requested lipid measurements less often than the other two groups. Abnormal lipid concentrations were diagnosed 2.2 ± 4.1 years before inclusion into the study. Patients under the care of the cardiologists had significantly higher total cholesterol, LDL-c, and triglyceride concentrations (P < 0.001, ). The prevalence of total cholesterol levels ≥5.2 mmol/L was 44.4%; this percentage was significantly greater in patients under the care of the cardiologists (50.7%, P = 0.009). The prevalence of hypertriglyceridemia was 55.3%; this abnormality was also more frequent in patients who were being attended by the cardiologists (61.8%). Low HDL-c values were found in 55.2% of men and 67.2% of women. Less than half of the patients with dyslipidemia were receiving drug therapy. A greater percentage of the patients under cardiologist care were on lipid-lowering therapy compared to the other two groups (). Statins were the most frequently used drug (76.5%). The use of lipid-lowering medications did not differ between specialists. Only a small proportion of the patients on lipid-lowering medication were at their LDL-c targets (32.2%).
Type 2 diabetes
The prevalence of type 2 diabetes was 22% (n = 289). The agreement between physician-diagnosis and patients recalled for diabetes was moderate (kappa = 0.87). Type 2 diabetes was diagnosed 6.4 ± 7.4 years before inclusion into the study. Patients attended by endocrinologists had the highest diabetes prevalence (31%, P < 0.001, ). The majority of patients (92.6%) were receiving drug therapy. The most frequently used drugs were metformin and sulfonylureas. Insulin was used by 14.7% of the patients with diabetes. The mean fasting plasma glucose level was 8.9 ± 3.4 mmol/L. Half of the patients with diabetes (52.2%) had an AMA = HbA1c measurement. Almost half of the diagnosed cases had an HbA1c < 7%. This percentage was higher in those under endocrinologist care (64.6%, P < 0.001). At the time of evaluation, only a few of these patients were at optimal levels of diastolic (27.4%) and systolic (43.0%) pressures. Diabetes related chronic complications were common in the study sample. The most common microvascular complications were sensitive polyneuropathy (71%) followed by retinopathy (27.5%) and nephropathy (23.2%). In addition, 19% had had a cardiovascular complication.
Cardiovascular disease
This category includes all patients who had suffered a myocardial infarction, unstable angina, transient ischemic attack, peripheral artery disease, revascularization, or any other clinical manifestation caused by coronary artery disease. The prevalence of cardiovascular disease was 14.4% (n = 184). The agreement between physician-diagnosis and patients recalled for cardiovascular disease was moderate (kappa = 0.47). Cardiovascular disease was diagnosed 8.4 ± 10.5 years before inclusion into the study. Patients under the care of cardiologists had the highest prevalence (23.6%, P < 0.001, ). The majority of patients (72.9%) treated by cardiologists were receiving medication. This was not true for the other two groups (primary care physicians 38%, endocrinologists 33.5%). Few patients were at treatment targets. Only 32.2% had an LDL cholesterol <2.6 mmol/L, 49% were at blood pressure targets, 39.4% had triglycerides <1.6 mmol/L, and 38.6% had the recommended HDL cholesterol concentrations.
The social and medical burden of abdominal obesity
The quality of life of patients was good with a mean score in the EQ-5D survey of 0.8 ± 0.2 points (n = 1070). A small percentage (6.4%) of patients referred to themselves as disabled due to illness and unable to work. No mood abnormalities were reported by 64.1% of patients. However, 38.6% (n = 413) and 4.1% (n = 44) reported moderate or extreme discomfort caused by their illness, respectively ().
Table 4 The social and medical burden of abdominal obesity
Covariates associated with obesity-related comorbidities
Logistic regression models were constructed to identify variables associated with each of the comorbidities (). Waist circumference was independently associated with high blood pressure and HbA1c in patients with diabetes. Borderline significance was found for the association of waist circumference and hypertriglyceridemia (P = 0.077) and hypoalphalipoproteinemia (P = 0.056) respectively. No association was found between waist circumference and fasting glycemia, presence of cardiovascular disease, and the occurrence of two or more cardiometabolic risk factors.
Table 5 Logistic regression analyses to evaluate the association between waist circumference, BMI, age, and gender with the risk factors studied
Discussion
Over the past 40 years, excess body weight has become a major health problem in Mexico.Citation13 However, not every case has comorbidities that affect the quality of life and life expectancy.Citation14 Health systems worldwide are not prepared to face the ongoing obesity epidemic. Many patients and physicians are not aware of the health risks associated with abdominal obesity.Citation15 It is a requirement not only to design effective obesity treatment programs but also to have an adequate description of the characteristics of the target population. This information cannot be obtained from population-based surveys or institutional databases because these sources include individuals seeking treatment for various medical conditions or those not looking for therapy at all. Our study describes the medical care given to individuals with abdominal obesity during daily clinical practice by general practitioners, cardiologists, and endocrinologists. It was designed to provide data representative of the pattern of care that patients with abdominal obesity receive in urban Mexico. Our data confirm that a large proportion of patients are undertreated. Only a small percentage of patients with obesity-related comorbidities reach treatment targets. Interventions proven to be effective in the prevention of chronic complications have in general not been implemented.
The study population is representative of patients treated by specialists who are usually involved in the management of abdominal obesity. Precautions were taken to avoid potential selection bias by the physicians. This approach allowed us to detect problems in both diagnostic and therapeutic actions. Our survey identified multiple conceptual and logistic challenges in the management of patients with abdominal obesity. Although all patients had abdominal obesity, less than half identified this as the main reason for the medical consultation. Half of the study population (48.4%) mentioned that they had made significant efforts to lose weight over the previous three months. However, the mean weight lost was moderate (4.3 ± 3.5 kg). A small proportion of physicians requested the participation of a nutritionist to provide dietary advice. In many cases, the specialist offered no dietary modification. The majority of patients (84%) were asked to increase their physical activity. However, less than half reported more than 120 minutes of physical activity per week.
Our observations confirm that the treatment of abdominal obesity is complex and unsatisfactory.Citation16 Modification of lifestyle is a remarkable challenge for adults. Physicians should be highly motivated to create awareness of the disease in patients and their relatives. In addition, they should educate and train patients to modify their dietary habits and to increase physical activity on a long-term basis. Health systems around the world should change their procedures and priorities to effectively face the epidemic in abdominal obesity.Citation17,Citation18
Increased waist circumference is a predictor for the presence of obesity-related comorbidities. As a consequence, the treatment of abdominal obesity should not be limited to inducing weight loss. The adequate management of comorbidities is a prime component of therapy. Each of these interventions is effective in reducing the risk of long-term obesity related complications.Citation19–Citation21 Despite this, current treatment targets are achieved in only a small proportion of cases (). Our results are similar to others reported worldwide.Citation22 Clinical inertia, lack of awareness in patients and physicians, and limited resources are some of the reasons for this finding.Citation23 Structured programs designed to improve the quality of care of patients with diabetes and cardiometabolic risks are urgently needed.
Scant information exists regarding the social burden caused by abdominal obesity.Citation24 The quality of life of patients was good, with a mean score in the EQ-5D survey of 0.8 ± 0.2 points. Despite this, 38.6% and the 4.1% referred to moderate or extreme discomfort caused by their illness, respectively. Thus, abdominal obesity should not be considered as only a medical problem. Social, economic, and psychological phenomena are the underlying factors. Medical personnel should be prepared to help patients overcome the environmental barriers that preclude them from having a healthy lifestyle.
The cross-sectional design and the lack of a control group without abdominal obesity are the main limitations of this report. Both defects limit our ability to confirm the known linear association that exists between waist circumference and the number and severity of each one of the cardiometabolic risks. Also, the approach used to assess dietary habits and physical activity may have a low sensitivity and significant variability.Citation25 In addition, information on other features of the metabolic syndrome (eg, fatty liver, chronic kidney disease, polycystic ovarian disease, hyperuricemia, and obstructive sleep apnea) was not registered. Finally, we concentrated on the management of abdominal obesity and its complications. We did not place emphasis on the diabetes-related microvascular complications because abdominal obesity is not a major risk factor for these outcomes.
Acknowledgments
We would like to thank each of the physicians who par ticipated in this survey as follows: Acosta R, Aguilar R, Aldrete J, Alonso E, Alvarez A, Arellano A, Arteaga H, Autrey A, Baeza R, Bailon E, Bancalari C, Becerra I, Becerril C, Benitez C, Bonfil M, Briseño H, Cabrera R, Campos E, Cejudo E, Cervantes A, Chavira I, Cobo C, Colinabarranco M, Cortes R, De La Cruz A, De La Peña J, Delgadillo S, Dies H, Escalante JM, Escudero X, Espinoza B, Fabian MG, Fanghänel G, Figueras R, Fletes V, Fremont LE, Garcia J, Garcia RE, Garza A, Garza F, Garza AF, Godinez S, Gomez GA, Gonzalez M, Gonzalez M, Granados C, Gutierrez CM, Gutierrez I, Hernandez A, Hernandez HR, Herrera A, Hubbard AM, Ibarra MA, Jalon A, Jimenez M, Juarez HJ, Lopez H, Lucano A, Lugo P, Marquez E, Martinez E, Martinez P, Mateos N, Medina SH, Mendoza RG, Montemayor D, Moreno JI, Muñoz M, Muñoz A, Nuñez JJ, Ochoa C, Ortiz A, Palomar A, Ponce C, Portocarrero L, Posadas C, Rajme V, Ramirez D, Ramirez HA, Rios MA, Rios EP, Rivero CA, Robles JA, Robles FJ, Rodriguez GA, Rodriguez F, Ruiz E, Saenz de Miera A, Salazar M, Sanchez AR, Sanchez H, Siordia JJ, Sosa A, Tamez HE, Valencia HP, Vazquez I, Vergara A, Vidrio M, Villa VF, Zanoniani C, Zuñiga-Guajardo S.
Disclosure
The survey was organized and implemented by the sponsor (sanofi-aventis). The manuscript was prepared by the authors. The sponsor has no role in the analysis or interpretation of the results. The authors have no conflicts of interest to disclose in connection to this manuscript.
References
- Villalpando S Shamah-Levy T Rojas R Aguilar-Salinas CA Trends for Type 2 diabetes and other cardiovascular risk factors in Mexico from 1993–2006 Salud Pública Méx 2010 52 Suppl 1 S72 S79
- World Health Organization Definition, diagnosis and classification of diabetes mellitus and its complications Part 1: diagnosis and classification of diabetes mellitus Geneva, Switzerland Department of Noncommunicable Disease Surveillance 1999
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA 2001 285 19 2486 2497 11368702
- Alberti KG Eckel RH Grundy SM Harmonizing the metabolic syndrome. A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute, American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity Circulation 2009 120 16 1640 1645 19805654
- Després JP Lemieux I Bergeron J Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk Arteroscler Thromb Vasc Biol 2008 28 6 1039 1049
- Deurenberg P Yap M van Staveren WA Body mass index and percent body fat: a meta analysis among different ethnic groups Int J Obes Relat Metab Disord 1998 22 12 1164 1171 9877251
- Deurenberg P Yap M Deurenberg P Is a re-evaluation of WHO body mass index cut-off values needed? The case of Asian in Singapore Nutr Rev 2003 61 5 Pt 2 S80 S87 12828197
- Yusuf S Hawken S Ounpuu S Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case control study Lancet 2004 364 9438 937 952 15364185
- Sanchez-Castillo CP Velazquez-Monroy O Berber A Anthropometric cutoff points for predicting chronic diseases in the Mexican National Health Survey 2000 Obes Res 2003 11 3 442 451 12634443
- Grundy SM Cleeman JI Daniels SR Diagnosis and management of the metabolic syndrome: and American Heart Association/National Heart, Lung and Blood Institute Scientific Statement Circulation 2005 112 17 2735 2752 16157765
- Després JP Lemieux I Prud’homme D Treatment of obesity: need to focus on high risk abdominally obese patients BMJ 2001 322 7288 716 720 11264213
- American Diabetes Association Diagnosis criteria for diabetes mellitus. Diagnosis and classification of diabetes mellitus Diabetes Care 2010 33 Suppl 1 S62 S69 20042775
- Barquera S Campos-Nonato I Hernández-Barrera L Obesidad y adiposidad central en adultos mexicanos: resultados de la Encuesta Nacional de Salud y Nutrición 2006 Salud Publica Mex 2009 51 Suppl 4 S595 S603 20464235
- Karelis AD Brochu M Rabasa-Lhoret R Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab 2004 30 5 569 572 15671927
- Bodenheimer T Wagner E Grumbach K Improving primary care for patients with chronic illness JAMA 2002 288 14 1775 1779 12365965
- Lau D Douketis JD Morrison K Hramiak I Sharma A Ur E for members of the Obesity Canada Clinical Practice Guidelines Expert Panel 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary] CMAJ 2007 176 8 Suppl S1 S13 17420481
- World Health Organization Preventing chronic diseases: WHO global report First edition Geneva, Switzerland 2005
- Córdova-Villalobos JA Barriguete-Meléndez JA Lara-Esqueda A Chronic non-communicable diseases in Mexico: epidemiologic synopsis and integral prevention Salud Publica Mex 2008 50 5 419 427 18852939
- Heart Protection Study Collaborative Group MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomized placebo controlled trial Lancet 2002 360 9326 7 22 12114036
- Heart Outcomes Prevention Evaluation Study Investigators Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy Lancet 2000 355 9232 253 259 10675071
- The CDC Diabetes Cost-effectiveness Group Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol reduction for type 2 diabetes JAMA 2002 287 19 2542 2551 12020335
- Pan American Health Organization Regional strategy and plan of action on an integrated approach to the prevention and control of chronic diseases, including diet, physical activity and health Washington, DC Pan American Health Organization 2006
- Saydah S Fradkin J Cowie C Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes JAMA 2004 291 3 335 342 14734596
- Williams J Wake M Hesketh K Maher E Waters E Health-related quality of life of overweight and obese children JAMA 2005 293 1 70 76 15632338
- Ferrari P Friedenreich C Matthews CE The role of measurement error in estimating levels of physical activity Am J Epidemiol 2007 166 8 832 840 17670910