Abstract
Background
Metabolic syndrome (MetS) is an aggregation of risk factors associated with increased incidence of cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality. Information on MetS prevalence is scarce in the northeast region, Brazil. This study aims to estimate the prevalence of MetS according to different diagnostic criteria in a community sample of men during the November Blue Campaign living in the metropolitan area of Natal, Rio Grande do Norte, Brazil.
Methods
This is a cross-sectional study on 500 men aged 40 years or older invited by the Blue November Campaign of 2015, an awareness program aimed at the prevention of male diseases. The evaluation included blood pressure, anthropometric measurements (weight, height, and waist circumference), fasting blood glucose, and blood lipid profile. The diagnosis of MetS was made according to the criteria of International Diabetes Federation (IDF)/American Heart Association (AHA)/National Heart, Lung, and Blood Institute (NHLBI), IDF, and National Cholesterol Education Program’s Adult Treatment Panel III (NCEP-ATPIII).
Results
The prevalence was high by considering the following three criteria: IDF/AHA/NHLBI (66.8%), IDF (60.0%), and NCEP-ATPIII (46.4%). Concordance between diagnostic criteria measured by the kappa statistic (k) was excellent between IDF/AHA/NHLBI and IDF (k=0.85, P<0.0001) and moderate between IDF/AHA/NHLBI and NCEP-ATPIII (k=0.59) and IDF and NCEP-ATPIII (k=0.54).
Conclusion
Prevalence of MetS in the male population was high using the three diagnostic criteria. IDF/AHA/NHLBI and IDF criteria have a high level of agreement, but NCEP-ATPIII criteria identify a lower number of MetS cases.
Introduction
The metabolic syndrome (MetS) is a complex and worldwide epidemic disorder with high socioeconomic impact due to its association with increased morbidity and mortality.Citation1 The main causes are increasing urbanization, nutrition transition, and reduced physical activity.Citation1 MetS consists of a cluster of several metabolic and physiological abnormalities, including abdominal obesity, impaired glucose metabolism, hypertriglyceridemia, decreased high-density lipoprotein cholesterol (HDL-C), and arterial hypertension. It is believed that this syndrome increases the risk of type 2 diabetes mellitus (T2DM) and cardiovascular diseases (CVDs).Citation2,Citation3 People with MetS are estimated to have twice the risk of developing CVD compared to healthy individuals and a fivefold increased risk of T2DM.Citation4
The Framingham Offspring Study demonstrated that the attributable risk in the population for diabetes associated with MetS was 62% in men and 47% in women with the modified National Cholesterol Education Program (NCEP) criteria.Citation5 The MetS’s pathogenesis remains unclear, as does the establishment of diagnostic criteria. It has been demonstrated clearly that the syndrome is common and that its prevalence is rising worldwide, which is largely a consequence of increasing obesity and sedentary lifestyles. As a result, the MetS is now both a public health issue and a clinical problem.Citation3 The MetS has an estimated prevalence of 20%–25% in the general population. Its prevalence is greater for older people, reaching 42% in individuals older than 60 years.Citation6
One in approximately every four or five adults develops MetS, depending on the environmental conditions and daily lifestyle habits of the country where he/she resides. The prevalence of this syndrome has been estimated to increase with age for individuals older than 50 years,Citation7 the use of new eating patterns,Citation8 changes in the work environment,Citation9 the number of meals during the day,Citation10 and the duration of sleepCitation11–Citation14 and in low-income peopleCitation15 and smokers.Citation15 Meanwhile, the prevention and treatment of MetS are based on changes in lifestyle through a multifactor approach based on education, regular physical exercise, and a healthy diet, as well as pharmacological strategies.Citation16
In Brazil, the Ministry of Health’s Comprehensive Male Health Care Policy (PNAISH) promotes the improvement of the health conditions of the male population from 25 to 59 years, a preponderant part of the productive force, contributing to the reduction in morbidity and mortality in this population through rational coping of risk factors and facilitating access, actions, and comprehensive health care services.Citation17 The Blue November Campaign is a part of these actions and includes a set of awareness strategies on the importance of prevention and early diagnosis of diseases that affect the male population, especially the most prevalent.Citation18
Considering that MetS represents a higher risk for T2DM and CVD, combined with the scarcity of data in Brazil, this study aims at determining the prevalence of MetS in men living at the metropolitan area of Natal, Rio Grande do Norte, northeast region of Brazil. The community-based sample was taken on the Blue November Campaign of 2015 using the criteria defined by consensus among the International Diabetes Federation (IDF)/American Heart Association (AHA)/National Heart, Lung, and Blood Institute (NHLBI). The prevalence of MetS according to IDF/AHA/NHLBI was compared with the criteria set forth by the IDF and NCEP’s Adult Treatment Panel III (NCEP-ATPIII).
Methods
Study population
The research was carried out according to the Norms and Ethical Guidelines of the National Health Council Resolution 510/2016 of the Brazilian Ministry of Health and approved by the Research Ethics Committee of the University Hospital Onofre Lopes, Federal University of Rio Grande do Norte, in 2014. The study was a cross-sectional survey based on an urban community sample of men 40 years or older in Natal, Rio Grande do Norte, with the Certificate of Presentation for Ethical Appreciation (CAAE) 25997913.1.0000.5292. The participants were invited between November 2015 and April 2016 through television advertisements, seeking volunteers to take part in the Blue November Campaign of 2015, which is the prevention of male diseases’ awareness program, promoted by the University Hospital Onofre Lopes.
A total of 500 men who agreed to participate in the study signed the informed consent form. Then, they were included in the survey, all were submitted to anamnesis, clinical, and laboratorial evaluation, and data were collected on the individual components of the MetS (blood pressure, waist circumference [WC], fasting glucose [FG], HDL-C, triglycerides [TG], and medication history). Also, we measured total cholesterol, low-density lipoprotein cholesterol (LDL-C) and body mass index (BMI).
Measurements
The blood pressure was measured with a mercury sphygmomanometer applied to the left arm, with the subject in the sitting position. The BMI was calculated by dividing the subject’s weight in kilograms by the square of height in meters (kg/m2) using an automatic anthropometric scale (Filizola, São Paulo, Brazil) calibrated by INMETRO. WC was measured using an inelastic measuring tape at the midpoint between the iliac crest and the lowest rib, with the patient in the standing position.
Blood samples were drawn from overnight fasting and using automated methods and commercially available assays at the Laboratory of Clinical Analysis of the University Hospital Onofre Lopes. We measured FG by the enzymatic test kit AA and lipid profile (including TG by the enzymatic test kit GOP/PAP AA, total cholesterol by the enzymatic test kit AA, and HDL-C by colorimetric test kit monofase AA plus) with an automated CMD 800 iX1 equipment (Wiener Lab, Rosario, Argentina).
The diagnosis of MetS was established according to the IDF/AHA/NHLBI criteria and compared with the IDF and NCEP-ATPIII criteria. The cutoff used for WC in IDF/AHA/NHLBI and IDF criteria was that of European ethnicity, according to .
Table 1 Definitions and diagnostic criteria for MetS
Statistical analysis
Prevalence rates are presented with binomial 95% CIs. The kappa statistic was used to analyze concordance between diagnostic criteria. The Chi-square test was used to compare proportions. Significance level was set at P<0.05. Stata 11 (Stata Corp., College Station, TX, USA) was used for statistical calculations.
Results
The present study assessed, on a community-based sample of the male population living in the metropolitan area of Natal, the prevalence of MetS and the agreement between diagnostic criteria, according to the latest criteria, IDF/AHA/NHLBI, compared with the IDF and NCEP-ATP III criteria. During a 6-month period, 500 men aged 43–83 years who participated in a voluntary health examination were assessed. The clinical and demographic characteristics of the study population are presented in , which showed a mean age of 57.3 years, the WC of 100.4 cm, the serum TG of 189.5 mg/dL, and the FG of 123.2 mg/dL.
Table 2 Characteristics of the study population in Natal, Rio Grande do Norte, at 2015
The prevalence rates among age groups (40–49, 50–59, 60–69, and ≥70 years) according to the three diagnostic criteria did not find a statistically significant difference, as shown in . The group of 60–69 years presented the highest prevalence in all criteria, such as IDF/AHA/NHLBI, IDF, and NCEP-ATPIII.
Figure 1 Prevalence of metabolic syndrome by age range according to different diagnostic criteria in the male population older than 40 years in Natal, Rio Grande do Norte.
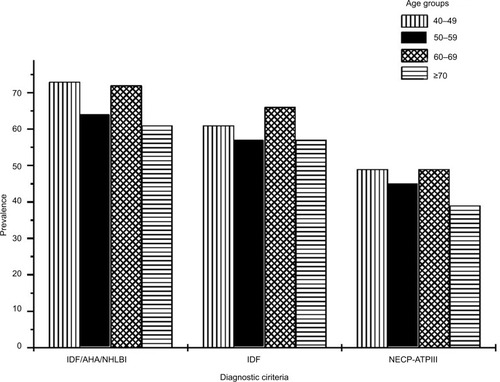
The percentage prevalence of MetS found for the three criteria studied is shown in . In this study, it was higher using the IDF/AHA/NHLBI criteria (66.8%) followed by the IDF criteria and the NCEP-ATPIII criteria. Concordance analysis of the three diagnostic criteria used for the definition of MetS was analyzed by determining the kappa statistic. The concordance showed excellent agreement between IDF/AHA/NHLBI and IDF criteria (kappa statistic 0.85, P<0.0001) but a moderate agreement between either of those criteria and NCEP-ATPIII criteria (kappa statistic 0.59 and 0.54, respectively).
Table 3 Prevalence of MetS according to different diagnostic criteria in the male population older than 40 years in Natal, Rio Grande do Norte
Discussion
MetS and age
The literature shows great variability in the prevalence of MetS among the elderly, which depends greatly on the criteria used for the diagnosis and also the ethnic and regional characteristics of the study population.Citation19 Park et al,Citation15 in the United States, showed that the prevalence of MetS increases with advancing age, peak at the sixth decade of life for men and the eighth decade of life for women. The emerging prevalence data suggest that MetS is quite prevalent especially among older people. This effect can be explained largely by age-related rises in blood pressure and glucose.Citation20
In Brazil, Nakazone et al,Citation21 in a follow-up of 200 gender-matched cardiology patients aged 31–50 years in Ribeirão Preto, São Paulo, Brazil, showed the prevalence of MetS as 35.5% by the NCEP-ATPIII criteria and 46% by the IDF criteria. Rigo et al,Citation22 in a study at Novo Hamburgo, Rio Grande do Sul, Brazil, with 378 elderly individuals aged >60 years, estimated the prevalence of MetS as 56.9, 53.4, and 50.3%, by the IDF, NCEP-ATPIII reviewed by AHA/NHLBI, and NCEP-ATPIII criteria, respectively. In a study, conducted by Saad et al,Citation19 of elderly population treated at the Outpatient Clinic of Internal Medicine and Geriatrics of Fundação Municipal de Saúde de Niterói, Rio de Janeiro, Brazil, the prevalence of MetS in males was 69.8, 60.3, 58.7, and 44.4% according to the Joint Interim Statement (JIS), IDF, World Health Organization (WHO), and NCEP-ATPIII criteria, respectively.
Kelliny et alCitation23 surveyed a sample representative of the general population aged 25–64 years in Seychelles, Africa, and found the prevalence of MetS in men to be 33.5% by the IDF criteria, 33.4% by the WHO criteria, and 31.9% by the NCEP-ATPIII criteria.
MetS and criteria
MetS is a widely prevalent and multifactorial disorder and has been given several names such as insulin resistance (IR) syndrome, plurimetabolic syndrome, Reaven’s syndrome, syndrome X, and the deadly quartet.Citation7 There are various MetS definitions. The first formal definition of the MetS was proposed in 1998, by a consultation group for the definition of diabetes on behalf of the WHO.Citation3 A different criterion was proposed by the NCEP-ATPIII in 2001 establishing that, for the diagnosis of MetS, an individual must have at least three of the following five criteria: central obesity measured by WC (>102 cm), hypertriglyceridemia, low HDL-C, hypertension (≥130/85 mmHg), and fasting hyperglycemia (≥110 mg/dL).Citation16
In 2005, the IDF produced another set of criteria for use both in epidemiology and in clinical practice worldwide, with the aims of identifying people with MetS, to clarify the nature of the syndrome and to focus on therapeutic strategies to reduce the long-term risk of CVD. The IDF established that, for the diagnosis of MetS, an individual must have central obesity, measured by the WC, with ethnicity-specific values as one required component and two other components (hypertriglyceridemia or low HDL-C or hypertension or fasting hyperglycemia) (≥100 mg/dL).Citation24
In 2009, both the IDF and AHA/NHLBI agreed that abdominal obesity should not be a prerequisite for diagnosis but that it should be one of the five criteria, so that the presence of any three of the following five risk factors constitutes a diagnosis of MetS: increased WC with ethnicity-specific reference values (eg, WC men ≥94 cm and women ≥80 cm in Caucasians), elevated TG (≥150 mg/dL or 1.7 mmol/L) or drug treatment for elevated TG, decreased HDL-C (<40 mg/dL or 1.03 mmol/L in males; <50 mg/dL or 1.29 mmol/L in females) or drug treatment for reduced HDL-C, elevated FG (≥100 mg/dL or 5.6 mmol/L) or drug treatment for elevated glucose, and elevated blood pressure (≥130/85 mm Hg) or use of antihypertensive drugs in a patient with a history of hypertension.Citation3 In this study, the higher prevalence by the IDF/AHA/NHLBI and IDF criteria was probably due to the lower cutoff of WC and fasting glycemia established by them.Citation3
In the United States, Ford et alCitation26 showed the prevalence of MetS in participants of the National Health and Nutrition Examination Survey, according to the JIS definition, to be higher with the JIS-94 definition (60.1%) than with the JIS-102 definition (59.3%) in men aged between 60 and 69 years. Alkerwi et alCitation25 found a prevalence of MetS in Luxembourg, according to the JIS definition, estimated from the ORISCAV-LUX study, also higher with the JIS-94 definition (68.3%) than with the JIS-102 definition (60.4%) in men aged between 60 and 69 years.The use of lower cutoff points of WCs is beneficial, as it raises the risk level for cardiometabolic disease among those identified as having the MetSCitation27 and then indicates the need for early cardiovascular risk reduction. This approach implies a large impact on preventive strategies and health care resources.
The different prevalence values for MetS found in these studies indicate the need to strongly consider the population ethnic aspects and regional habits. The findings demonstrate the difficulty in having a diagnostic criterion that is accurate, sensitive, and specific and that can be useful for assessing the general population, overcoming the limitations of regional specificities. Oliveira et alCitation28 showed the prevalence of MetS in the population with rheumatoid arthritis treated at the Rheumatology Outpatient Clinic of Hospital Universitário Walter Cantídio of Universidade Federal do Ceará, Ceará, Brazil, to be 53.4% by the IDF criteria and 50% by the NCEP-ATPIII criteria. Xi et alCitation29 used data from the China Health and Nutrition Surveys in 2009 to describe the prevalence of MetS in China and showed that the prevalence in men according to revised NCEP-ATPIII criteria for Asians was 20.9%, according to IDF criteria was 16.2%, and according to the Chinese Diabetes Society criteria was 12.2%.
MetS in Brazil
Similar to what has been found in Western countries, the prevalence of MetS is rapidly increasing in developing countries. In Brazil, studies estimating the prevalence of MetS for urban regions in the southeast reported 29.8% in 2007Citation30 and 25.4% in 2008Citation31 by the NCEP-ATPIII criteria, 35.5 and 46.0% in 2007Citation21 by the NCEP-ATPIII and IDF criteria respectively, 34.0% in 2011Citation32 by IDF criteria, 35.9 and 43.2% in 2011Citation33 by the NCEP-ATPIII and IDF criteria, respectively, and 45.2, 64.1, 69.1, and 51.9% in 2014Citation19 by the NCEP-ATPIII, IDF, Joint Interim Statement (JIS), and WHO criteria, respectively. According to the Brazilian region, the prevalences have been estimated as follows: in the Northeast, 50% by the NCEP-ATPIII criteria and 53.4% by the IDF criteria in 2016;Citation28 in the South, 50.3% by the ATPIII criteria, 53.4% by ATPIII reviewed by the AHA/NHLBI criteria, and 56.9% by the IDF criteria in 2009;Citation22 and in the Midwest region, 32.0% by the harmonized MetS criteriaCitation3 in 2012.Citation34 In a rural population of southeastern Brazil, the MetS was found in 21.6% in 2007Citation35 and 14.9% in 2011Citation36 by the NCEP-ATPIII criteria, and in the northeastern region, the MetS was found in 24.8% by the NCEP-ATPIII criteria in 2006.Citation37 Among the indigenous population in the north, the MetS was found 34% by the NCEP-ATPIII and 43% by the IDF criteria in 2009,Citation38 and in the midwest region, the MetS was found 66.1% by the IDF/AHA/NHLBI criteria in 2015.Citation39
MetS and lifestyle
Kesse-Guyot et alCitation8 showed that the increased prevalence of MetS worldwide had been attributed to changes in lifestyle, particularly regarding new eating patterns and sedentarism. The study by Straif et alCitation9 found the growth in MetS prevalence due to the working hours that once occurred during daytime being extended in the last decades for a large number of services and production areas. Knutson et alCitation10 reported that meals more often breakfast, lunch, and dinner and snacks in the intervals lead to better appetite control, greater effect of postprandial thermogenesis, largest mobilization of lipids due to repeated stimulation of the sympathetic nervous system, lower elevation in plasma glucose, and less variation in insulin levels and C-peptide, therefore maintaining the control of MetS. Wu et alCitation11 demonstrated that reduced sleep time (<6 h/day) was positively associated with MetS, while Gangwisch et al,Citation12 Meier-Ewert et al,Citation13 and Stamatakis and PunjabiCitation14 observed that decreased sleep duration has been linked to several metabolic disorders, such as glucose intolerance, IR, dyslipidemia, hypertension, and systemic inflammatory processes. Park et alCitation15 showed that the prevalence is higher in low-income people (mainly women), smokers, and sedentary men. The scientific literature supports the beneficial effects of low-calorie diet associated with physical exercise, reinforcing the importance of changing lifestyle in the management of MetS.Citation40
MetS and concordance analysis
Similar results of this study, about concordance analysis, were also observed in Brazil, where Saad et alCitation19 found a very good concordance between IDF and JIS (k=0.89) and moderate concordance between IDF and NCEP-ATPIII (k=0.55), NCEP-ATPIII and JIS (k=0.53), WHO and NCEP-ATPIII (k=0.51), WHO and IDF (k=0.47), and WHO and JIS (k=0.45). Alkerwi et alCitation25 in Luxembourg showed excellent concordance between JIS-94/80 and IDF (k=0.93), between JIS-94/80 and NCEP-ATPIII (k=0.91), and between IDF and NCEP-ATPIII (k=0.84) criteria, but in the United States, the agreement was k=0.92 between the NCEP-ATPIII and IDF criteria in postmenopausal women,Citation26 and in 2008, Kelliny et alCitation23 in Africa found excellent agreement between NCEP-ATPIII and IDF (k=0.82) and moderate agreement between WHO and IDF (k=0.61) and between WHO and NCEP-ATPIII (k=0.59).
The difference in concordance between the MetS diagnostic criteria in different populations is probably due to ethnic characteristics, dietary habits, and lifestyle, thus making it difficult to use a single diagnostic criterion for all populations. Substantial socioeconomic and demographic changes that have occurred in the Brazilian population over the past decades have been associated with a deterioration of the metabolic profile because of adverse changes in lifestyle habits. Although the MetS has been a feature of urban westernized lifestyle, risk factors for CVD are now emerging as a major public health problem in the urban population of developing countries. The main focus of treating MetS is managing the risk factors with lifestyle changes that include losing weight, following a heart-healthy diet, reducing one’s blood pressure, improving one’s cholesterol and blood sugar levels, getting more regular physical activity, and quitting smoking. Maintaining a healthy lifestyle is a lifelong commitment. Successfully controlling MetS takes a long-term effort and teamwork with health care providers. At the same time, early diagnosis, prevention, and management of MetS are considered the key approaches to reduce the risk of progression of atherosclerosis and the development of CVD.Citation7
Conclusion
We observed that the prevalence of MetS in the male population was high using the three diagnostic criteria and that IDF/AHA/NHLBI and IDF criteria have a high level of agreement. However, NCEP-ATPIII criteria identify a lower number of MetS cases. It is essential to evaluate the occurrence of MetS and its associated factors in order to contribute to the elaboration of health promotion public policies that have a significant impact on the prevention and treatment of T2DM and CVD.
Limitations of this study can be explained in part by the sample selection criterion, which comprised all the demand served in the Blue November Campaign. The Campaign may contribute to explain the gaps in men’s health, addressing the risk factors of men aging in urban settings, poor eating habits, and sedentary lifestyle. While different regions may require further regional studies due to the characteristics of its populations to better assess their prevalence of MetS, main risk factors associated with men aging in urban settings are known and can be identified and intervened. The positive aspect was to note the importance of the Blue November Campaign as an opportunity to propose interventions for men’s health care.
Acknowledgments
This research received funding from the Federal University of Rio Grande do Norte/PROAD/PPg UFRN.
Disclosure
The authors report no conflicts of interest in this work.
References
- Misra A Khurana L Obesity and the metabolic syndrome in developing countries J Clin Endocrinol Metab 2008 93 suppl 1 S9 S30 18987276
- Corona G Rastrelli G Morelli A Vignozzi L Mannucci E Maggi M Hypogonadism and metabolic syndrome J Endocrinol Invest 2011 34 7 557 567 21720206
- Alberti KG Eckel RH Grundy SM Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity Circulation 2009 120 16 1640 1645 19805654
- Grundy SM Metabolic syndrome pandemic Arterioscler Thromb Vasc Biol 2008 28 4 629 636 18174459
- Wilson PW D’Agostino RJr Parise H Sullivan L Meigs JB Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus Circulation 2005 112 20 3066 3072 16275870
- Santos HCM Orange LG Lima CR Azevedo MMS Dourado KF Andrade SP Metabolic syndrome and other risk factors for cardiovascular disease in an obese population Rev Bras Cardiol 2013 26 6 442 449
- Gupta A Gupta V Metabolic syndrome: what are the risks for humans? Biosci Trends 2010 4 5 204 212 21068471
- Kesse-Guyot E Ahluwalia N Lassale C Hercberg S Fezeu L Lairon D Adherence to Mediterranean diet reduces the risk of metabolic syndrome: a 6-year prospective study Nutr Metab Cardiovasc Dis 2013 23 7 677 683 22633793
- Straif K Baan R Grosse Y Carcinogenicity of shift-work, painting, and fire-fighting Lancet Oncol 2007 8 12 1065 1066 19271347
- Knutson KL Spiegel K Penev P Van Cauter E The metabolic consequences of sleep deprivation Sleep Med Rev 2007 11 3 163 178 17442599
- Wu MC Yang YC Wu JS Wang RH Lu FH Chang CJ Short sleep duration associated with a higher prevalence of metabolic syndrome in an apparently healthy population Prev Med 2012 55 5 305 309 22846501
- Gangwisch JE Heymsfield SB Boden-Albala B Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey Hypertension 2006 47 5 833 839 16585410
- Meier-Ewert HK Ridker PM Rifai N Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk J Am Coll Cardiol 2004 43 4 678 683 14975482
- Stamatakis KA Punjabi NM Effects of sleep fragmentation on glucose metabolism in normal subjects Chest 2010 137 1 95 101 19542260
- Park YW Zhu S Palaniappan L Heshka S Carnethon MR Heyms-field SB The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994 Arch Intern Med 2003 163 4 427 423 12588201
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA 2001 285 19 2486 2497 11368702
- Brasil Ministério da Saúde Política de Atenção Integral à Saúde do Homem Brasília Brasil Ministério da Saúde 2008 40
- Instituto Nacional do Câncer Coordenação-Geral de Atenção às Pessoas com Doenças Crônicas. Posicionamento do Ministério da Saúde acerca da integralidade da saúde do homem no contexto do Novembro Azul Rio de Janeiro INCA 2015 Nota técnica conjunta N°001/2015. Available from: u.saude.gov.br/images/pdf/2015/novembro/09/Integralidade-sa-de-homens.pdf Accessed March 02, 2018
- Saad MA Cardoso GP Martins WA Velarde LG Cruz Filho RA Prevalence of metabolic syndrome in elderly and agreement among four diagnostic criteria Arq Bras Cardiol 2014 102 3 263 269 24676226
- Alexander CM Landsman PB Grundy SM The influence of age and body mass índex on the metabolic syndrome and its components Diabetes Obes Metab 2008 10 3 246 250 18269640
- Nakazone MA Pinheiro A Braile MC Prevalence of metabolic syndrome using NCEP-ATPIII and IDF definitions in Brazilian individuals Rev Assoc Med Bras 2007 53 5 407 413 17952349
- Rigo JC Vieira JL Dalacorte RR Reichert CL Prevalência de síndrome metabólica em idosos de uma comunidade: comparação entre três métodos diagnósticos Arq Bras Cardiol 2009 93 2 85 91 19838483
- Kelliny C William J Riesen W Paccaud F Bovet P Metabolic syndrome according to different definitions in a rapidly developing country of the African region Cardiovasc Diabetol 2008 7 27 37 18801172
- Alberti KG Zimmet P Shaw J Metabolic syndrome – a new worldwide definition. A Consensus Statement from the International Diabetes Federation Diabet Med 2006 23 5 460 480 16681554
- Alkerwi A Donneau AF Sauvageot N Prevalence of the metabolic syndrome in Luxembourg according to the Joint Interim Statement definition estimated from the ORISCAV-LUX study BMC Public Health 2011 11 1 4 21205296
- Ford ES Li C Zhao G Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US J Diabetes 2010 2 3 180 193 20923483
- Katzmarzyk PT Janssen I Ross R Church TS Blair SN The importance of waist circumference in the definition of metabolic syndrome: prospective analyses of mortality in men Diabetes Care 2006 29 2 404 409 16443895
- Oliveira BMGB Medeiros MMC Cerqueira JVM Souza Quixadá RT Oliveira IMAX Síndrome metabólica em pacientes com diagnóstico de artrite reumatoide acompanhados em um Hospital Universitário do Nordeste brasileiro Rev Bras Reumatol 2016 56 2 117 125
- Xi B He D Hu Y Zhou D Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: the China Health and Nutrition Survey in 2009 Prev Med 2013 57 6 867 871 24103567
- Salaroli LB Barbosa GC Mill JG Molina MC Prevalência de síndrome metabólica em estudo de base populacional, Vitória, ES–Brasil Arq Bras Endocrinol Metabol 2007 51 7 1143 1152 18157391
- Marquezine GF Oliveira CM Pereira AC Krieger JE Mill JG Metabolic syndrome determinants in an urban population from Brazil: social class and gender-specific interaction Int J Cardiol 2008 129 2 259 265 18036678
- Silva EC Martins IS de Araújo EA Síndrome metabólica e baixa estatura em adultos da região metropolitana de São Paulo (SP, Brasil) Cien Saude Colet 2011 16 2 663 668 21340342
- Gronner MF Bosi PL Carvalho AM Prevalence of metabolic syndrome and its association with educational inequalities among Brazilian adults: a population-based study Braz J Med Biol Res 2011 44 7 713 719 21755260
- Dutra ES de Carvalho KM Miyazaki E Hamann EM Ito MK Metabolic syndrome in central Brazil: prevalence and correlates in the adult population Diabetol Metab Syndr 2012 4 1 20 22583910
- Velásquez-Meléndez G Gazzinelli A Côrrea-Oliveira R Pimenta AM Kac G Prevalence of metabolic syndrome in a rural area of Brazil Sao Paulo Med J 2007 125 3 155 162 17923940
- Pimenta AM Gazzinelli A Velásquez-Meléndez G Prevalência da síndrome metabólica e seus fatores associados em área rural de Minas Gerais (MG, Brasil) Cien Saude Colet 2011 16 7 3297 3306 21808917
- Oliveira EP Souza ML de Lima MD Prevalência de síndrome metabólica em uma área rural do semi-árido baiano Arq Bras Endocrinol Metabol 2006 50 3 456 465 16936986
- Medeiros CL Síndrome metabólica em idosos quilombolas e não quilombolas no Estado do Amapá dissertação Brasília Universidade Católica de Brasília 2009
- Soares LP Fabbro AL Silva AS Prevalence of metabolic syndrome in the Brazilian Xavante indigenous population Diabetol Metab Syndr 2015 7 105 26594249
- Leão LS de Moraes MM de Carvalho GX Koifman RJ Nutritional interventions in metabolic syndrome: a systematic review Arq Bras Cardiol 2011 97 3 260 265 22030698
