Abstract
Obesity increases the risk for developing type 2 diabetes mellitus (T2DM) and this in turn correlates with an elevated probability of long-term diabetes complications once diabetes is established. Interventions aimed at lowering weight via changes in diet and lifestyle have repeatedly been shown to improve glycemic control in patients with T2DM and even to reverse early disease. Weight gain, a potential side effect of treatment for patients with T2DM, is also an important concern, and it has been noted that weight increases associated with antidiabetes therapy may blunt cardiovascular risk reductions achieved by decreasing blood glucose. Among older agents, metformin and acarbose have the lowest risk for weight gain, while sulfonylureas, meglitinides, and thiazolidinediones are all associated with weight increases. Clinical trial results have also consistently demonstrated that treatment with glucagon-like peptide-1 receptor agonists and amylin lowers weight, and that dipeptidyl peptidase-4 inhibitors are weight neutral in patients with T2DM. Conventional human insulin formulations are known to increase weight in patients with T2DM. However, some insulin analogs, particularly insulin detemir, have lower liability for this adverse event. The use of both pharmacologic and surgical therapies aimed at treating obesity rather than lowering blood glucose have the potential to improve glycemic control and even resolve T2DM in some patients.
Introduction
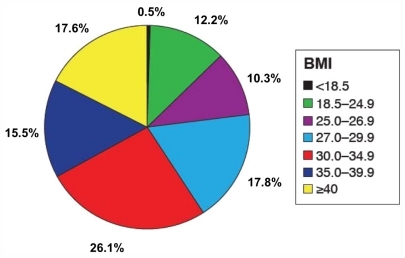
Obesity, along with other factors such as advancing age, family history of diabetes, history of gestational diabetes, impaired glucose metabolism, and physical inactivity, are associated with increased risk for type 2 diabetes (T2DM).Citation1 It has been noted that the prevalence of diagnosed diabetes among adults 18–79 years of age in the USA increased by 41% from 1997 to 2003, and this increase was greatest among obese individuals (body mass index [BMI] ≥30 kg/m2).Citation2 It is believed that obesity contributes to the development of T2DM by elevating levels of nonesterified free fatty acids, hormones, adipocytokines, and other substances that increase insulin resistance. Obesity-related elevation in proinflammatory molecules, including tumor necrosis factor-α and interleukin-6, are also believed to contribute to the development of both T2DM and metabolic syndrome.Citation3 The prevalence of overweight and obesity among patients with T2DM are both extremely high. Results from the Study to Help Improve Early Evaluation and Management of Risk Factors Leading to Diabetes, for example, indicated that 28% of individuals surveyed with diabetes were overweight (BMI 25–29.99 kg/m2) and 59% were obese (defined as above) ().Citation4
Figure 1 Distribution of body mass index (BMI) values for patients with type 1 or type 2 diabetes mellitus in the Study to Help Improve Early Evaluation and Management of Risk Factors Leading to Diabetes.
Obesity is not only associated with increased risk for the development of T2DM but also with elevated probability of long-term complications in people with this disease. The risk for these complications is also increased for obese patients in the prediabetic state.Citation5,Citation6 Patients with T2DM are at high risk for cardiovascular disease (CVD)-related events,Citation7 and overweight/obesity and T2DM are both independent risk factors for the development of CVD.Citation7,Citation8 All of these results support the view that overweight/obesity, along with hyperglycemia and other risk factors such as elevated blood pressure and abnormal lipids, act together to determine risk for all-cause and CVD mortality in patients with T2DM.Citation9
There are also strong relationships among obesity, diabetes, and cancer risk. For example, meta-analysis of epidemiological data indicated that the relative risk (RR) for postmenopausal breast cancer is ~1.5 for overweight women and >2 for obese women versus women with normal weight.Citation10 The meta-analysis also found that diabetes is associated with postmenopausal breast cancer, with summary RRs from meta-analyses of 1.15–1.20. The risk for pancreatic cancer is also significantly increased by overweight or obesity or the presence of diabetes.Citation11
Weight gain is also an important concern as a potential side effect of treatment for patients with, or at risk for, T2DM.Citation12,Citation13 Control over body weight can significantly decrease the risk for complications in patients with T2DM and should be an important aspect of management for these patients. This review considers the importance of addressing obesity across the course of disease in patients with T2DM to decrease the risk for complications and optimize long-term outcomes. It includes consideration of diet and lifestyle management, effects of antidiabetes therapy on body weight, and both pharmacologic and surgical interventions aimed at lowering weight.
T2DM and overweight/obesity
Results from numerous large-scale long-term studies have indicated that excess weight is harmful in patients with or without T2DM. Results from the Framingham Study showed that atherosclerotic risk factor clustering is common in both men and women in the general population, worsens with weight gain, and is associated with increased risk of coronary heart disease. This prospective study of 2406 men and 2569 women aged 18–74 years at baseline indicated that a 2.25 kg increase in weight over 16 years was associated with a 20% rise in the summed severity of six CVD risk factors (high-density lipoprotein cholesterol [HDL-C], total cholesterol, BMI, systolic blood pressure, triglycerides, and plasma glucose) in men and a 37% increase in women.Citation14 The importance of obesity in increasing the risk for diabetes complications was underscored by the Heart Outcomes Prevention Evaluation study. Results from this 4.5-year study of 6620 men and 2182 women (about 32% with diabetes) showed that obesity, in particular, abdominal adiposity, leads to an increased risk for CVD, including myocardial infarction by 23% (P < 0.01), congestive heart failure by 38% (P < 0.03), and all-cause mortality by 17% (P < 0.05).Citation15
Given the highly negative effects of obesity in patients with or without T2DM, it is not surprising that several studies have demonstrated significant benefits of weight loss for improving glycemic control and reducing risk for diabetes complications and mortality. One-year results of the Look AHEAD (Action for Health in Diabetes) trial showed that clinically significant weight loss in patients with T2DM was associated with improved glycemic control and a more favorable CVD risk profile.Citation16 This study of 5145 individuals with T2DM showed that intensive lifestyle intervention, which produced a mean 8.6% reduction in body weight, was associated with a significant decrease in mean hemoglobin A1c (HbA1c) from 7.3% to 6.6% (−0.64 ± 0.02; P < 0.001), significant decreases in systolic (−6.8 ± 0.4; P < 0.001) and diastolic (−3.0 ± 0.2; P < 0.001) blood pressure and triglycerides (−30.3 ± 2.0; P < 0.001), and significant increases in HDL-C (+3.4 ± 0.2; P < 0.001).Citation16 Similarly, a 2-year study of weight reduction achieved via weight-loss diets in moderately obese individuals (14% with T2DM) showed that a low-carbohydrate diet resulted in a 20% decrease in the ratio of total cholesterol to HDL-C and a 4.7 ± 6.5 kg decrease in body weight, and that a Mediterranean diet decreased fasting glucose in patients with T2DM by 32.8 mg/dL (1.82 mmol/L) and body weight by 4.4 ± 6.0 kg.Citation17 Results obtained after 4 years of the ongoing Look AHEAD trial revealed that, among those with T2DM, intensive lifestyle intervention can provide sustained weight loss along with improvements in fitness, glycemic control, and CVD risk factors.Citation18
Results from a prospective analysis of data from 4970 over-weight individuals with diabetes enrolled in the American Cancer Society’s Cancer Prevention Study I with a 12-year mortality follow-up indicated that 34% of the study cohort reported intentional weight loss (based on reply to a questionnaire with the following as choices: “unintentional” loss or gain, “intentional” loss or gain, or “no change”). Intentional weight loss was associated with a 25% reduction in total mortality and a 28% reduction in diabetes- and CVD-related mortality.Citation19 Data from the weight loss arm of the Trials of Hypertension Prevention showed that even modest weight loss (4.4 kg at 6 months, 2.0 kg at 18 months, and 0.2 kg at 36 months) led to clinically significant long-term risk reductions for hypertension 0.58 (95% confidence interval [CI] 0.36–0.94) at 6 months, 0.78 (95% CI 0.62–1.00) at 18 months, and 0.81 (95% CI 0.70–0.95) at 36 months.Citation20
Effective intervention to decrease obesity can also lower the occurrence of diabetes in at-risk individuals. Results from the Malmo study that included 41 subjects with early T2DM and 181 with impaired glucose tolerance (IGT) indicated that an intervention focused on diet and exercise normalized glucose tolerance in >50% of subjects with IGT and reversed T2DM in >50% of those diagnosed with early disease over 6 years of follow-up.Citation21 A second small-scale study randomized (4:1) male health-screening examinees with IGT to standard treatment (n = 356) or an intensive intervention group that included detailed instructions on lifestyle that were repeated every 3–4 months during hospital visits. The cumulative 4-year incidence of diabetes was 9.3% in the control group versus 3.0% in the intervention group (P < 0.001).Citation22 The Diabetes Prevention Program included 1079 nondiabetic participants, with IGT and a mean baseline BMI of 33.9 kg/m2, who were randomized to intensive lifestyle intervention and followed for 3.2 years. Results from this group of patients showed that each 1 kg of weight loss was associated with a 16% reduction in the risk for development of T2DM.Citation23 Similarly, findings from a Cochrane meta-analysis of eight controlled trials indicated that interventions aimed at increasing exercise combined with diet modification reduced the risk of T2DM compared with standard recommendations in high-risk groups (people with IGT or metabolic syndrome) (RR 0.63; 95% CI 0.49–0.79). This intervention improved systolic (weighted mean difference −4 mmHg; 95% CI −5 to −2) and diastolic (−2 mmHg; 95% CI −3 to −1) blood pressure levels, respectively.Citation24
All of these results support the American Diabetes Association (ADA), North American Association for the Study of Obesity (now known as The Obesity Society), and American Society for Clinical Nutrition guidelines, which indicate that moderate weight loss (5% of body weight) can decrease insulin resistance, decrease fasting blood glucose, and reduce the need for antidiabetes medications.Citation25 ADA guidelines published in 2011 also recommend such weight loss, and note that 7% reduction along with regular physical activity (150 minutes/week) can reduce the risk for developing diabetes.Citation26
Selection of treatment across the spectrum of disease in T2DM
The two major US treatment algorithms for antidiabetes therapy in patients with T2DM differ substantially. The consensus statement from the ADA/European Association for the Study of Diabetes recommends a stepwise approach to treatment, with initial therapy consisting of diet and lifestyle changes plus metformin and subsequent treatment with sulfonylurea or insulin to achieve HbA1c < 7%.Citation27 In contrast, the American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel recommends more aggressive, individualized combination therapy with a wider range of agents (eg, metformin, thiazolidinediones, incretin-based treatments, insulin) as initial pharmacotherapy for patients with T2DM to achieve HbA1c < 6.5%.Citation28 Both guidelines emphasize the importance of diet and lifestyle modification as an essential part of treatment.Citation27,Citation28
Dietary intervention
The emphasis on diet and lifestyle intervention in newly diagnosed patients with T2DM is supported by results from several clinical trials. Results from the Look AHEAD study showed that 1 year of diet and exercise aimed at weight loss improved glucose disposal rate, fasting plasma glucose, free fatty acids, and adipose tissue distribution in a small cohort of 26 men (mean baseline BMI 32.4 kg/m2) and 32 women (mean baseline BMI 34.8 kg/m2) with T2DM. Results from this study also showed that changes in overall weight (adipose tissue mass) and hepatic fat were the most important determinants of metabolic improvements in these patients.Citation29
A meta-analysis of eleven randomized controlled trials that included 402 patients with T1DM or T2DM indicated that although each of those studies had unique criteria for identifying either low or high glycemic indexes, those considered low significantly decreased HbA1c with a weighted mean difference of −0.5% (95% CI −0.9 to −0.1; P = 0.02) versus high-glycemic-index diets. Results from this meta-analysis also showed that a low-glycemic-index diet significantly decreased episodes of hypoglycemia versus a high-glycemicindex diet in one study (difference of −0.8 episodes per patient per month; P < 0.01).Citation30
In considering these results, it is important to note that different types of diets have distinct effects on weight loss in patients with T2DM. Diets that might be considered include low fat, high protein/low carbohydrate (ketogenic and nonketogenic), low glycemic-index, and very lowcalorie regimens. A clinical comparison of low-fat, restricted-calorie; Mediterranean, restricted-calorie; and low-carbohydrate, nonrestricted-calorie diets indicated that all decreased weight (2.9 kg, 4.4 kg, and 4.7 kg, respectively) in moderately obese patients, (mean baseline BMI 31 kg/m2) but that the low-carbohydrate diet had more favorable effects on lipids and the Mediterranean diet had more favorable effects on glycemic control.Citation17 Both low-glycemic-index and low-carbohydrate ketogenic diets (<20 g carbohydrate/day) have been shown to lower both HbA1c and body weight in patients with T2DM, but the reductions with the ketogenic diet were significantly greater than those with the low-glycemic-index diet (1.5% versus 0.5%; P = 0.03 and 11.1 kg versus 6.9 kg; P = 0.008).Citation31 A low-carbohydrate nonketogenic diet (30% protein, 50% fat, and 20% carbohydrate) has also been shown to be effective for lowering fasting glucose by 40% and HbA1c by 1.7% versus a standard diet in patients with T2DM.Citation32 A very low calorie diet (450 calories/day) has also been shown to be effective in patients with T2DM. Results from one study of 18 patients who followed this diet for 30 days indicated an 11.7 kg reduction in body weight over this period, and improvements in serum lipids, blood pressure, and glycemia that were sustained over 18 months.Citation33
Conventional oral antidiabetes therapy
Conventional oral antidiabetes agents include metformin, sulfonylureas, meglitinides, alpha-glucosidase inhibitors, and thiazolidinediones ().Citation27,Citation34 One or more of these agents are generally employed, along with dietary and lifestyle intervention, as initial therapy for patients with T2DM, with varying effects on body weight and, potentially, CVD risk.Citation13,Citation27,Citation35
Table 1 Oral antihyperglycemic medications available in the USA
Metformin
The action of metformin is reduction of hepatic glucose output and reduction of fasting blood glucose levels.Citation27 Treatment with metformin results in HbA1c reductions of 1.0%–2.0%.Citation27 Metformin has a favorable profile with respect to body weight and other CVD risk factors. It does not cause weight gain and it improves both the blood lipid profile and fibrinolytic activity.Citation13 Results from one study indicated that 1 year of treatment with metformin decreased triglycerides from baseline by 26.6 mg/dL (0.3 mmol/L) and low-density lipoprotein cholesterol [LDL-C] by 4.6 mg/dL (0.12 mmol/L), and increased HDL-C by 3.1 mg/dL (0.08 mmol/L).Citation36 Weight loss in patients with T2DM taking metformin is associated with reductions in both total body fat and visceral fat in those with abdominal or visceral obesity.Citation37 Results from one study in which patients were treated with metformin (1000 mg/day) for 26 weeks indicated that mean body weight decreased by 2.0 kg (P < 0.05 versus placebo), abdominal subcutaneous fat decreased by 0.4 kg, and intraabdominal fat decreased by 0.3 kg (both P < 0.05 versus baseline).Citation38 Metformin is associated with gastrointestinal side effects and is contraindicated in patients with renal insufficiency.Citation27
Sulfonylureas
Sulfonylureas lower glycemia by enhancing insulin secretion and their use can lower HbA1c by 1.0%–2.0%.Citation27 Despite the fact that sulfonylureas are still recommended for the treatment of T2DM, the use of these agents is being called into question. Results from a study of 9876 patients with T2DM who were treated with oral glucose-lowering drugs after a myocardial infarction indicated that the risk for cardiovascular mortality was significantly increased (hazard ratio [HR] 1.28; 95% CI 1.14–1.44) versus those who received metformin. Citation39 Results from a second retrospective cohort that included 34,253 patients treated with a sulfonylurea, metformin, rosiglitazone, or pioglitazone in a single academic health care network indicated that the RR for myocardial infarction for those receiving a sulfonylurea was 2.2 (95% CI 1.6–3.1) compared with metformin.Citation40 Results from a cohort of 205 adult men with T2DM who were followed for a mean of 9.4 years indicated that those treated with a sulfonylureas alone experienced a mean weight gain of 0.42 kg/year,Citation41 and it is reasonable to suggest that increased cardiovascular risk with sulfonylureas may be related to the weight gain in patients treated with these drugs. Sulfonylureas are also associated with potentially severe hypoglycemic events.Citation27
Meglitinides
Like sulfonylureas, meglitinides bind to sulfonylurea receptors on pancreatic β-cells (although at a different receptor site) to stimulate insulin secretion. These drugs have shorter half-lives than sulfonylureas and must be administered more often, but they do result in HbA1c reductions of 0.5%–1.5%.Citation27 Meglitinides are also associated with significant weight gain (2.4 kg over 3 months; P < 0.05) versus metformin when used for the treatment of patients with T2DM;Citation42 results from a meta-analysis of 15 clinical trial results for this class indicated that weight gains as high as 3 kg may occur over 3 months.Citation43 Meglitinides have also been associated with hypoglycemia, but with a frequency lower than that for sulfonylureas.Citation27
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitors slow digestion of polysaccharides in the proximal small intestine. This results in lowering of HbA1c by 0.5%–0.8% and decreased postprandial glucose levels with low risk for hypoglycemia.Citation27 The alpha-glucosidase inhibitor acarbose decreased HbA1c by 0.8% (95% CI −0.9 to −0.7), according to a meta-analysis of 30 acarbose trials, and was not associated with weight gain in patients with T2DM.Citation44 It has been shown to decrease the risks for progression to diabetes and CVD events in patients with IGT who were treated for a mean of 3.3 years in the Study to Prevent Non-Insulin Dependent DM trial. Results from this study indicated that acarbose treatment resulted in a 25% RR reduction in the development of T2DM (95% CI 0.63–0.90; P = 0.0015), and a 49% decrease in risk for CVD events (95% CI 0.28–0.95; P = 0.03).Citation45 Miglitol, which is the other alpha-glucosidase inhibitor, has been shown to provide similar reductions in HbA1c but is associated with abdominal discomfort.Citation46,Citation47 The hypoglycemic potency of alpha-glucosidase inhibitors is less than that of either biguanides or sulfonylureas.Citation13 Unfortunately, those treatments are associated with gastrointestinal side effects that have resulted in limited use within the US.
Thiazolidinediones
Thiazolidinediones are modulators of peroxisome proliferator-activated receptor γ modulators that increase the insulin sensitivity of muscle, fat, and liver.Citation27 These drugs lower plasma glucose by enhancing its uptake into tissues and decrease HbA1c by 0.5%–1.4%.Citation27 In adipose tissue, thiazolidinediones act as insulin sensitizers and are potent inhibitors of lipolysis, and they enable mobilization of fat from muscle and liver tissues as well as β-cells. These actions result in amelioration of lipotoxicity and improve insulin sensitivity by reducing insulin secretion, which helps to preserve β-cell function and therefore maintain glycemic control over time.Citation48 Thiazolidinediones are associated with weight gain and edema as well as increased risk for congestive heart failure.Citation27 Results from a meta-analysis of four randomized trials that included 14,291 patients (6421 receiving rosiglitazone, 7870 receiving control therapy) with follow-up of 1–4 years indicated that rosiglitazone significantly increased the risk of myocardial infarction (RR 1.42; P = 0.02) and heart failure (RR 2.09; P < 0.001), but not CVD mortality (RR 0.90; P = 0.53).Citation49 A recent study that directly compared risks for acute myocardial infarction, acute heart failure, or all-cause mortality among patients ≥18 years of age who started treatment with rosiglitazone (n = 6421) or pioglitazone (n = 7870) between January 1, 2001, and December 12, 2005 indicated that 4.16% of the patients treated with rosiglitazone experienced acute myocardial infarction, acute heart failure, or death versus 4.14% of those treated with pioglitazone (HR 1.03; 95% CI 0.91–1.15; P = 0.666) over a median follow-up period of 34 months.Citation50 In considering these results, it is worth noting that the 10-year risk for coronary heart disease in patients with T2DM is about 13%.Citation51 It has also been shown that thiazolidinediones cause bone loss and increase fracture risk in patients with T2DM.Citation52 Recent results have also indicated that long-term treatment with pioglitazone may be associated with increased risk for bladder cancer. A study that included 193,099 patients in the Kaiser Permanente Northern California diabetes registry indicated that any use of pioglitazone was not associated with elevated risk of bladder cancer (P = 0.8). However, there was an increased risk (HR 1.4; 95% CI 1.03–2.0) in patients who used pioglitazone for >24 months.Citation53
Incretin-based treatments
Incretins – glucagon-like peptide (GLP)-1 receptor agonists and dipeptidyl peptidase (DPP)-4 inhibitors ()Citation27,Citation34,Citation54 – have become increasingly accepted as treatments for patients with T2DM, and their effects on body weight differ from those of conventional oral therapies.Citation55 Several mechanisms contribute to the glucose-lowering effects of GLP-1 receptor agonists. These include glucose-dependent stimulation of insulin secretion, reduction of plasma glucagon concentrations, and delay of gastric emptying. These agents lower HbA1c by 0.5%–1.0%.Citation27 The weight loss associated with these agents is believed to result from delayed gastric emptying which maintains a feeling of fullness, thus reducing appetite and food intake as well as the signaling of satiety via direct stimulation of parts of the brain involved in regulation of appetite.Citation56 Meta-analyses of results from 21 randomized controlled trials revealed that patients who received GLP-1 receptor agonists (n = 5429) had significant reductions in BMI compared to those treated with placebo (difference −0.44 kg/m2; P = 0.012) and those who received insulin (difference −1.57 kg/m2; P < 0.001).Citation57 Meta-analyses of results from eight trials in which GLP-1 receptor agonists were compared with oral antidiabetes agents indicated significantly greater weight loss with the incretin mimetics versus comparators (weighted mean difference −2.37 kg; 95% CI −3.95 to −0.78).Citation58 Direct comparison of the two currently approved GLP-1 receptor agonists indicated that liraglutide and exenatide were associated with similar weight reductions (3.24 kg versus 2.87 kg, respectively; P = 0.2235). However, liraglutide decreased mean HbA1c to a greater extent than exenatide (1.12% versus 0.79%; P < 0.0001).Citation59 Analysis of results from studies of liraglutide have shown that the reduction in body weight in patients treated with this agent results primarily from decreases in both subcutaneous and visceral adipose tissue.Citation60 The most common adverse events associated with GLP-1 receptor agonists are gastrointestinal events. Long-term treatment of rodents with liraglutide was found to cause thyroid C-cell hyperplasia,Citation61 but clinical results have not indicated any increased risk for medullary thyroid cancer.Citation54 It has been reported that eight cases of acute pancreatitis occurred during clinical development of exenatide and there were 36 postmarketing reports of acute pancreatitis in exenatide-treated patients. Four patients developed acute or chronic pancreatitis during liraglutide clinical trials.Citation62
Table 2 Injectable diabetes medications available in the USA: (A) insulins and (B) incretin mimetics and noninsulin synthetic analogs
Systematic reviews of clinical results for DPP-4 inhibitors indicated that these agents lower HbA1c by 0.5%–0.8% and are generally weight-neutral.Citation27,Citation63,Citation64 Since these drugs act via increasing the duration of action of GLP-1, they have low risk for hypoglycemia. DPP-4 inhibitors are available as fixed-dose combinations with metformin. It has been suggested that DPP-4 inhibitors have the potential to interfere with immune function and have been associated with increased risk for upper respiratory infections.Citation27 Evaluation of clinical trial results for sitagliptin has also shown that it is not associated with an increase in risk for cardiovascular events.Citation65 A trial designed to compare the efficacy of liraglutide and sitagliptin published in 2010 reported more substantial reductions in HbA1c among patients who received 1.8 mg liraglutide (−1.50%; 95% CI −1.63 to −1.37) and 1.2 mg liraglutide (−1.24%; 95% CI −1.37 to −1.11; n = 221) than those treated with sitagliptin (−0.90%; 95% CI −1.03 to −0.77; n = 219).Citation66
Pramlintide
Pramlintide, an amylinomimetic, is approved for treatment of elevated postprandial glucose levels in T1DM and T2DM.Citation67 Combined analysis of four studies of pramlintide in patients with T2DM indicated that it significantly reduced HbA1c by 0.33% (95% CI 0.14–0.51; P = 0.004) and weight by 2.57 kg (95% CI 1.70–3.44; P < 0.00001) versus controls.Citation68 The adverse events observed most often with pramlintide are nausea and hypoglycemia.Citation69
Novel therapy
A new class of glucose-lowering agents that are of particular interest because of their favorable effects on body weight are sodium-glucose co-transporter 2 inhibitors. These agents decrease the reabsorption of glucose and thus increase renal glucose excretion.Citation70 Results from a clinical study of dapagliflozin 2.5 mg, 5 mg, or 10 mg versus placebo indicated HbA1c reductions of 0.58%, 0.63%, and 0.82% versus 0.13%, respectively. Reductions in body weight were 1.18 kg, 1.56 kg, and 2.26 kg versus 0.72 kg, respectively.Citation71 Treatment with sodium-glucose co-transporter 2 inhibitors has been shown to be associated with increased risk for urinary tract and genital infections.Citation71 Concern about the safety of dapagliflozin has been raised by results indicating that nine of 5478 patients taking dapagliflozin in clinical trials had bladder cancer, compared with one of 3156 patients in the placebo group. In addition, nine of 2223 women taking dapagliflozin had breast cancer, compared with one of 1053 women in the placebo group.Citation72,Citation73
Insulin treatment
A very large percentage of patients with T2DM ultimately require insulin therapy (see for examples)Citation34 to maintain control over blood glucose.Citation48,Citation74 Insulin remains the most potent medication currently available to achieve tight control over plasma glucose and avoid or delay long-term disease complications among nonhospitalized patients. However, insulin treatment is commonly associated with weight gain,Citation75 which varies substantially with the type of insulin employed for treatment (see below). This may be due in part to improved glycemic control resulting in decreased glycosuria, resulting in more glucose absorption and therefore more calories retained. Defensive snacking behaviors, driven by fears of hypoglycemia, can also contribute to weight gain in patients using insulin.Citation74 Insulin also has anabolic effects, and this is reflected by the fact that patients with diabetes gain lean as well as fat mass. Results from two studies indicated that 30%–37% of the weight gain associated with insulin treatment was lean mass.Citation76,Citation77
Treatment with an older and commonly used insulin preparation, neutral protamine Hagedorn (NPH) insulin, has been consistently associated with weight gain. Results from one study of insulin therapy in patients with T2DM indicated that patients gained 3.8 kg over 6 months of treatment and most of this gain was fat mass.Citation78 This complication of treatment with NPH is significantly decreased with insulin analogs. Meta-analysis of clinical trial results ()Citation79 indicated that the long-acting insulin analog detemir was associated with less weight gain than NPH insulin in patients with diabetes, although the insulin analog glargine was not (standardized mean difference detemir versus glargine −0.37 kg; P = 0.048).Citation79 Another meta-analysis of trials found more weight gain with glargine than NPH (pooled mean change −0.33 kg; 95% CI −0.61 to −0.06).Citation80
Figure 2 Differences (with 95% confidence intervals [CI]) between long-acting analogs and neutral protamine Hagedorn insulin in the effects on body mass index at endpoint in clinical trials of patients with type 1 or type 2 diabetes mellitus.
![Figure 2 Differences (with 95% confidence intervals [CI]) between long-acting analogs and neutral protamine Hagedorn insulin in the effects on body mass index at endpoint in clinical trials of patients with type 1 or type 2 diabetes mellitus.](/cms/asset/7841e8ad-48be-4a71-90ac-062ede2dbbfa/dmso_a_24022_f0002_c.jpg)
Results from several large-scale clinical trials demonstrated the significantly superior effects of insulin detemir on weight gain versus NPH insulin and insulin glargine. Results from a 24-week study in which either insulin detemir or NPH insulin was added to oral antidiabetes therapy in 476 patients with T2DM indicated a 1.2 kg weight gain with insulin detemir versus 2.8 kg with NPH insulin (P < 0.001).Citation81 Results from a 26-week, randomized, controlled trial that included 271 patients with T2DM who received either insulin detemir or NPH insulin once daily in the evening along with mealtime insulin aspart substituted for two daily doses of insulin (at least one had to be a premix) indicated that weight had increased significantly less with detemir (0.4 kg) than with NPH (1.9 kg) (P < 0.0001) at the end of the study.Citation82 Another 26-week trial compared insulin detemir and NPH insulin in 505 patients with T2DM who also received insulin aspart at mealtimes. After 26 weeks of treatment, patients receiving insulin detemir gained significantly less weight (1.0 kg) than those who were administered NPH insulin (1.8 kg) (P = 0.017).Citation83 A 26-week comparison of insulins detemir and glargine in 385 patients with T2DM who also received mealtime insulin aspart in a basal-bolus regimen showed that there was further significantly less weight gain with insulin detemir (1.2 kg) versus insulin glargine (2.7 kg) (P = 0.001).Citation84 The reason for decreased weight gain in patients treated with long-acting insulin detemir has not been elucidated, but results from several studies have suggested possible explanations. It may be that acylation and albumin binding used to extend the duration of action for insulin detemir results in a greater influence on hepatocytes than peripheral tissues. This might reduce glucose output from the liver without promoting peripheral lipogenesis.Citation85 An effect of insulin detemir in the central nervous system may also contribute to its decreased risk for weight gain versus NPH insulin and insulin glargine. A study in 15 healthy volunteers showed that a bolus injection of insulin detemir during hyperinsulinemic-euglycemic clamp produced a change in the electroencephalogram not observed after injection of regular human insulin. Results from this study also showed that insulin detemir significantly decreased subsequent food intake by 303 kcal versus regular human insulin (P < 0.04).Citation86
The pharmacokinetic/pharmacodynamic profile for insulin detemir may also contribute to the favorable effects of this agent on body weight. Insulin detemir has a flatter time-action profile versus NPH insulin, providing more consistent plasma levels.Citation87 The pharmacokinetic and pharmacodynamic within-subject variation is lower for insulin detemir versus glargine,Citation88 and this may also contribute to lower weight gain during treatment.
Adjunctive therapies for management of body weight in patients with T2DM
Pharmacotherapy
The close association between obesity and T2DM suggests that a more proactive approach to weight management in obese individuals without diabetes may have the potential to delay or possibly prevent the onset of T2DM. In patients who already have diabetes, better control of weight has the potential to decrease glucose levels. However, development of pharmacologic agents to manage obesity has been difficult, with many being denied approval and only a few currently in the pipeline ().Citation89
Table 3 Pharmacotherapy for obesity in the USA
Orlistat blocks absorption of ingested fat by inhibiting pancreatic lipase and it is approved for use in adults and children ≥12 years of age for up to 1 year.Citation90 Meta-analysis of results from 29 controlled clinical trials of orlistat has indicated that it produces a mean 2.75 kg weight loss over 52 weeks of treatment.Citation91 Systematic review of 28 clinical trials for orlistat has also shown that it has significant benefit in improving the lipid profile in patients with diabetes, with significant (P < 0.05) reductions versus placebo in total cholesterol (weighted mean difference −0.37 mmol/L) and LDL-C (−0.27 mmol/L).Citation92 Results from a 4-year prospective study that included 3305 patients (BMI ≥ 30 kg/m2 and normal [79%] or IGT [21%]) indicated that the cumulative incidence of diabetes was 6.2% for orlistat and 9.0% with placebo (37.3% risk reduction; P = 0.0032).Citation93 Cetilistat is a novel inhibitor of gastrointestinal and pancreatic lipases that has proceeded to Phase III development. A 14-week (12 weeks of active treatment) study included 612 overweight or obese patients (mean baseline BMI 34.3 kg/m2) with T2DM who were randomized to cetilistat (40 mg, 80 mg, or 120 mg three times daily), or orlistat (120 mg three times daily). Study results indicated similar reductions in body weight of 3.78–4.32 kg for patients treated with 80 mg or 120 mg cetilistat or 120 mg orlistat (all P ≤ 0.01 versus baseline).Citation94
Other agents currently approved for treatment of obesity (each for up to 12 weeks in adults) include phentermine, diethylpropion, and phendimetrazine.Citation90 Meta-analysis of results from nine clinical trials with phentermine indicated that it decreased mean body weight by 3.6 kg over 2–24 weeks of treatment,Citation91 but it has not been specifically evaluated in patients with T2DM in a large-scale controlled clinical trial. Meta-analysis of results from 13 clinical trials of diethylpropion indicate a mean weight reduction of 3.0 kg among obese individuals in studies of 6–52 weeks duration.Citation91 Phendimetrazine has been shown to result in weight loss of 2.5–5.5 kg over an unspecified period in overweight patients.Citation95
While other agents or combinations have been developed for the treatment of obesity, none are currently approved by the Food and Drug Administration (FDA). Sibutramine acts principally by blocking synaptic reuptake of serotonin and noradrenaline;Citation96 meta-analysis of results from eight controlled clinical trials of sibutramine in patients with T2DM indicated that decreases in body weight and waist circumference were significantly greater with this agent versus placebo, but sibutramine had minimal effects on glycemic control or lipids. This agent was recently withdrawn from the market in the US due to increased risk for myocardial infarction and stroke,Citation97 as reported in the Sibutramine Cardiovascular Outcome Trial.Citation98,Citation99 Abbott Laboratories (Abbott Park, IL), the manufacturer of sibutramine, also withdrew sibutramine from other countries and has suspended all activities related to it.Citation100
Lorcaserin is a selective serotonin receptor agonist that was also developed for the treatment of obesity.Citation100 The efficacy of lorcaserin was evaluated in a double-blind study in which 3182 obese or overweight adults (mean baseline BMI 36.2 kg/m2) received 10 mg lorcaserin twice daily or placebo for 52 weeks. At week 52, patients in the placebo group continued on this treatment, but patients in the lorcaserin group were randomly reassigned to receive either placebo or lorcaserin. At the end of the first 52 weeks, 47.5% of patients in the lorcaserin group and 20.3% in the placebo group had lost ≥5% of their body weight (P < 0.001). Among patients who received lorcaserin during year 1 and lost ≥5% of their baseline weight, the loss was maintained by 67.9% of those who continued on lorcaserin during year 2 versus 50.3% of those rerandomized to placebo.Citation101 However, administration of lorcaserin was associated with the development of neoplasms in rats and an FDA advisory panel recommended against its approval. The FDA accepted this recommendation and requested more information addressing this issue.Citation100
Tesofensine is a noradrenaline, dopamine, and serotonin reuptake inhibitor and it has been evaluated for treatment of obesity in a Phase II, randomized, double-blind, placebo-controlled trial that included 203 obese patients with mean baseline BMI of 30 to ≤40 kg/m2 who were prescribed tesofensine 0.25 mg, 0.5 mg, or 1.0 mg/day or placebo plus an energy-restricted diet for 24 weeks. After 24 weeks, diet and placebo resulted in a 2.0% weight loss versus 4.5%, 9.2%, and 10.6%, respectively for 0.25 mg, 0.5 mg, and 1.0 mg/day tesofensine (P < 0.0001).Citation102 Further development of this agent has been halted while the manufacturer, NeuroSearch (Ballerup, Denmark), seeks a partner to continue commercialization. Citation103 Development of another agent that demonstrated efficacy in Phase II trials, velneperit (S-2367), a selective neuropeptide Y Y5-receptor antagonist, has been discontinued due to anticipated difficulties in gaining approval in the US and European Union.Citation104,Citation105
The combinations of bupropion plus naltrexone, bupropion plus zonisamide, and topiramate plus phentermine have all been assessed for treatment of obesity, but none have been approved by the FDA. The combination of bupropion, which is approved for depression and smoking cessation, and naltrexone, an opioid receptor antagonist approved for opioid and alcohol addiction, was assessed for the treatment of obesity.Citation106 When added to diet and exercise this combination has been shown to result in a loss of 9.3% of body weight (versus 5.1% among patients who received placebo, diet, and exercise; P < 0.001) over 56 weeks among obese patients.Citation107 In February 2011, however, the FDA issued a letter noting concern about the cardiovascular safety profile of naltrexone/bupropion when used long-term in a population of overweight and obese subjects, and requested a preapproval safety study.Citation108 The combination of bupropion with the antiepileptic drug zonisamide has demonstrated efficacy for decreasing body weight in Phase II trials, but it has not yet progressed to Phase III studies.Citation109 Phentermine has been studied in combination with low-dose topiramate, an antiepileptic agent that is also used as a preventive treatment for migraines. Clinical trials with the phentermine/topiramate combination have demonstrated up to an 11% decrease in body weight when administered to obese patients.Citation110 In October 2010, however, the FDA rejected the combination and required the manufacturer, VIVUS, Inc, (Mountain View, CA) to provide more evidence regarding the elevation of heart rate associated with phentermine, including the likelihood that it increases the risk for major adverse cardiovascular events, as well as mandating a comprehensive assessment of the product’s potential to cause birth defects associated with topiramate.Citation111 A study published in 2008 reported that although the number of adverse outcomes was low among pregnant individuals exposed to topiramate, the overall rate of oral clefts in newborns was eleven times the background rate, raising concerns about congenital malformation among those receiving topiramate polytherapy.Citation112 In March 2011, the FDA informed the public that new data revealed an increased risk for development of cleft lip and/or cleft palate (oral clefts) among infants born to women who were treated with topiramate.Citation113
Neurohormonal approaches have demonstrated efficacy in the treatment of obesity and may have less risk for significant toxicity than agents aimed primarily at the central nervous system. Leptin is a neurohormone secreted by adipocytes, and leptin-deficient humans exhibit severe hyperphagia and profound obesity. Amylin is another peptide hormone that is secreted with insulin from pancreatic β-cells and the amylin analog pramlintide increases satiation and reduces food intake.Citation114 The combination of pramlintide and metreleptin is being developed as a treatment for obesity. A 24-week, randomized, double-blind trial included 177 obese or overweight subjects (mean baseline BMI 32.0 kg/m2) who received pramlintide (180 μg twice daily for 2 weeks, and 360 μg twice daily thereafter) and diet (40% calorie deficit) for 4 weeks. Those who achieved 2%–8% weight loss over 4 weeks were randomized to 20 weeks of treatment with metreleptin (5 mg twice daily), pramlintide (360 μg twice daily), or combination of the two agents at the stated doses. Weight reductions with the three treatments were −8.2%, −8.4%, and −12.7%, respectively. Combination treatment was significantly more effective than either metreleptin (P < 0.01) or pramlintide (P < 0.001) monotherapy.Citation114
The beneficial effects of liraglutide on body weight (see incretin-based treatments section) have prompted its development for the treatment of obesity. A double-blind, placebo-controlled 20-week trial included 564 obese individuals (mean baseline BMI 30–40 kg/m2) who were randomized to liraglutide doses of 1.2 mg, 1.8 mg, 2.4 mg, or 3.0 mg/day, placebo, or orlistat (120 mg/day). All subjects also had an energy-deficit diet and increased their physical activity. Mean weight losses with liraglutide 1.2 mg, 1.8 mg, 2.4 mg, and 3.0 mg were 4.8 kg, 5.5 kg, 6.3 kg, and 7.2 kg, respectively compared to 2.8 kg with placebo and 4.1 kg with orlistat.Citation115
Bariatric surgery
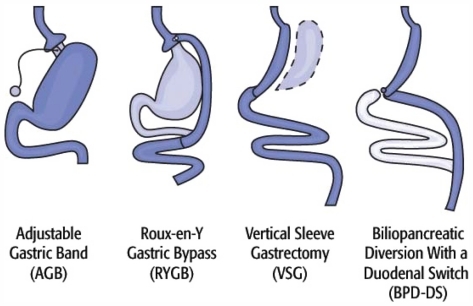
Four types of bariatric surgery are used most often in the US. These include adjustable gastric band, Roux-en-Y gastric bypass (RYGB), biliopancreatic diversion with a duodenal switch, and vertical sleeve gastrectomy ().Citation116 The adjustable gastric band limits food intake by placing a small band around the top of the stomach to produce a small pouch. The outlet size is controlled by a circular balloon inside the band that can be inflated or deflated with saline solution. The RYGB restricts food intake and also reduces absorption. Food intake is limited by a small pouch and absorption of food is reduced by routing food directly from the pouch into the small intestine and thus bypassing most of the stomach, duodenum, and upper intestine. The biliopancreatic diversion with a duodenal switch removes a large portion of the stomach to promote smaller meal sizes and decreases absorption by rerouting food away from much of the small intestine and by rerouting bile and other digestive juices. The vertical sleeve gastrectomy involves removing a large portion of the stomach to create a gastric sleeve that remains connected to a very short segment of the duodenum, which is then directly connected to a lower part of the small intestine. This operation makes the distance between the stomach and colon much shorter after this operation, thus promoting malabsorption.Citation116
Figure 3 Commonly used bariatric surgery procedures.
Eight clinical trials of patients who have undergone gastric bypass surgery have shown that this intervention is associated with a 99% to 100% prevention of diabetes in individuals with IGT and an 80% to 90% clinical resolution of diagnosed T2DM.Citation117 A systematic review and meta-analysis summarizing 136 studies published in English between 1990 and 2003 that included >22,000 patients who underwent bariatric surgery (73% women; mean BMI 47 kg/m2) indicated complete resolution of T2DM (defined as discontinuation of all diabetes-related medications and blood glucose levels within the normal range) in 77% of cases. An average weight loss of 41 kg (approximately 65% of the excess weight) was recorded among patients with resolution of diabetes.Citation118 The effectiveness of bariatric surgery in decreasing body weight and returning patients to euglycemia and normal insulin levels has prompted the suggestion that the small bowel may play a key role in the pathophysiology of T2DM.Citation119
The ADA 2011 Standards of Medical Care in Diabetes support gastric reduction surgery, stating that it can be effective for inducing weight loss among individuals with severe obesity.Citation26 A Diabetes Surgery Summit Position Statement likewise recognizes the legitimacy of surgical procedures such as gastric bypass for treatment of diabetes among certain patients, and notes that clinical trials aimed at determining the role of surgery for those with less severe obesity and diabetes should be a priority.Citation120
Several new devices have been developed (and adapted) to facilitate the endoluminal approach to bariatric procedures. An endoluminal bariatric sleeve that is open at both ends and is intended to mimic the duodenal and proximal jejunal bypass impact of an RYGB produced an average weight loss of 23.6% in a group of 10 patients followed for 12 weeks.Citation121 In December 2010 the FDA approved a gastric band (LAP-BAND® Adjustable Gastric Banding System; BioEnterics Corporation, Carpinteria, CA; initially approved in 2001) for weight reduction in obese patients with a BMI ≥ 35 kg/m2 and in those with BMI > 30 kg/m2 who have one or more comorbid conditions, finding that benefits of such procedures outweigh the risks.Citation122 The effectiveness of the LAP-BAND® in patients with T2DM is supported by results from 413 patients who were followed for ≥1 year postsurgery. Resolution of diabetes was observed in 66% at 1-year and 80% at 2-year follow-up. The mean HbA1c value declined from 7.25% preoperatively to 5.58% at 2 years after surgery. The reduction in excess weight was 39.2% at 1 year and 52.6% at 2 years.Citation123
Results from the Swedish Obese Subjects study of 4047 obese patients has provided insight into the long-term effects of bariatric surgery. Ten-year follow-up of these patients showed weight losses from baseline of 25%, 16%, and 14%, respectively for patients treated with gastric bypass, vertical-banded gastroplasty (stapling), and banding. Study results also indicated significantly decreased mortality risk for patients who underwent surgery versus controls (HR 0.76; P = 0.04).Citation124
The benefits of bariatric surgery on glycemic control may result, at least in part, from their effects on the incretin system. Results from a study of 41 obese patients with T2DM under-going either bypass, banding, or very-low-calorie diet who were followed for up to 42 days indicated that patients who underwent bypass surgery had increased GLP-1 responses to meals (P < 0.05).Citation125 Similarly, a study of 16 obese patients with T2DM who received either RYGB or gastric-restrictive surgery (laparoscopic adjustable gastric band or laparoscopic sleeve gastrectomy) indicated that those treated with RYGB had significant increases in insulin secretion, GLP-1 levels, and β-cell sensitivity to glucose (P < 0.05).Citation126 It has been suggested that RYGB and other malabsorptive procedures, such as biliopancreatic diversion, improve glucose homeostasis by increasing delivery of unabsorbed nutrients to the distal gut and thus increasing secretion of GLP-1.Citation127 Further support for the view that hormonal effects, independent of weight loss, may underlie improvements in glycemic control in patients undergoing bariatric surgery is that this effect is observed in days to weeks after surgery, prior to the occurrence of significant weight loss.Citation128 The suggestion that hormonal effects associated with nutrient delivery to the distal gut and elevated GLP-1 secretion contributes to improved glycemic control is supported by results of studies which have shown that RYGB improved glucose control versus restrictive procedures despite equivalent weight loss. Results from a comparison of RYGB versus adjustable gastric banding indicated better higher postmeal GLP-1 and glucose control with the former procedure despite equivalent postsurgical BMI in the two groups of patients.Citation129 Other gastrointestinal hormones may also play a role in the weight loss associated with bariatric surgery. Peptide YYCitation3–Citation36 is involved in food intake and clinical trial results have indicated that gastric bypass surgery, but not gastric banding, increases levels of this peptide.Citation130 It has also been shown that gastric bypass surgery, but not diet-induced weight loss, increases levels of oxyntomodulin, and it has been suggested that elevation of this hormone may be necessary for the improved glucose control associated with bariatric surgery.Citation131
Economic considerations
Use of nonpharmacologic interventions and newer therapies (eg, incretin-based treatments, insulin detemir) and surgical intervention in an effort to lower body weight or prevent weight gain in patients with diabetes has the potential to increase the cost of care, although results from pharmacoeconomic studies have indicated long-term economic benefit of these approaches. It has been noted that dietary programs aimed at decreasing obesity, such as the Dietary Approaches to Stop Hypertension program, are effective for lowering weight and improving other cardiovascular risk factors and have low cost.Citation132 Projection of long-term treatment outcomes supports the cost-effectiveness of both liraglutide and exenatide for the treatment of T2DM.Citation133,Citation134 Pharmacoeconomic analysis has also indicated that treatment of patients with T2DM using insulin detemir is cost-effective versus NPH insulin.Citation135 Bariatric surgery has been reported to be cost-effective versus nonsurgical interventions in severely obese patients.Citation136
Conclusion
Overweight and obesity are common in the US population. Obesity increases the risk for T2DM as well as that for complications in people with the disease. Close attention to diet and lifestyle can significantly decrease the frequency of T2DM in high-risk patients and help control blood glucose in patients with the disease. These interventions have also been shown to be effective for reversing T2DM in patients diagnosed with this disease. Treatment for diabetes evolves with disease progression, and clinicians must consider effects on weight when selecting medications. Among older agents, metformin and acarbose have the lowest risk for weight gain. Clinical trial results have also consistently demonstrated that treatment with GLP-1 receptor agonists lowers weight, and DPP-4 inhibitors are weight-neutral in patients with T2DM. Most patients with T2DM ultimately require insulin treatment, and insulin analogs have lower liability for weight gain than human insulin. This benefit has been demonstrated most consistently for insulin detemir and is less clear for insulin glargine and the rapid-acting insulin analogs. Surgical therapies aimed at treating obesity can improve metabolic control and can even prevent T2DM in some individuals. Bariatric surgery remains the most effective treatment for obesity, and research is elucidating its unique effectiveness and it can also reverse diabetes in patients with T2DM. The factors responsible for this resolution before actual weight loss may lie in the secretion of incretin hormones. Overall, results summarized in this review underscore the point that changes in lifestyle and diet are highly effective for controlling body weight and reversing T2DM and should be emphasized as first steps in patient management. For patients who cannot achieve significant and sustained weight loss with these approaches, careful selection of antidiabetes therapy and additional surgical intervention, if necessary, can assist in the control of body weight.
Acknowledgments
The author thanks Robert W Rhoades, PhD and Aric Fader, PhD of MedVal Scientific Information Services, LLC for providing writing and editorial assistance. This manuscript was prepared according to the International Society for Medical Publication Professionals’ Good Publication Practice for Communicating Company-Sponsored Medical Research: the GPP2 Guidelines. Funding to support the preparation of this manuscript was provided by Novo Nordisk Inc.
Disclosure
The author has participated on advisory boards for Abbott, Allergan, Amylin, Arena, Johnson & Johnson, Merck, Orexegin, and Sanofi-Aventis, and has received research funding from Amylin, Lilly, MetaProteomics, Orexigen, Pfizer, Sanofi-Aventis, and the Dr Robert C and Veronica Atkins Foundation.
References
- National Diabetes Information Clearinghouse National Diabetes Statistics, 2011 2 2011 Available from: http://diabetes.niddk.nih.gov/dm/pubs/statistics/#allages Accessed July 28, 2011
- Geiss LS Pan L Cadwell B Gregg EW Benjamin SM Engelgau MM Changes in incidence of diabetes in US adults, 1997–2003 Am J Prev Med 2006 30 5 371 377 16627124
- Khaodhiar L Cummings S Apovian CM Treating diabetes and prediabetes by focusing on obesity management Curr Diab Rep 2009 9 5 348 354 19793504
- Bays HE Chapman RH Grandy S The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys Int J Clin Pract 2007 61 5 737 747 17493087
- Nathan BM Moran A Metabolic complications of obesity in childhood and adolescence: more than just diabetes Curr Opin Endocrinol Diabetes Obes 2008 15 1 21 29 18185059
- Meigs JB Wilson PW Fox CS Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease J Clin Endocrinol Metab 2006 91 8 2906 2912 16735483
- Haffner SM Lehto S Rönnemaa T Pyörälä K Laakso M Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction N Engl J Med 1998 339 4 229 234 9673301
- Eeg-Olofsson K Cederholm J Nilsson PM Risk of cardiovascular disease and mortality in overweight and obese patients with type 2 diabetes: an observational study in 13,087 patients Diabetologia 2009 52 1 65 73 18985314
- Wei M Gaskill SP Haffner SM Stern MP Effects of diabetes and level of glycemia on all-cause and cardiovascular mortality. The San Antonio Heart Study Diabetes Care 1998 21 7 1167 1172 9653614
- La Vecchia C Giordano SH Hortobagyi GN Chabner B Overweight, obesity, diabetes, and risk of breast cancer: interlocking pieces of the puzzle Oncologist 2011 16 6 726 729 21632448
- Larsson SC Permert J Hakansson N Naslund I Bergkvist L Wolk A Overall obesity, abdominal adiposity, diabetes and cigarette smoking in relation to the risk of pancreatic cancer in two Swedish population-based cohorts Br J Cancer 2005 93 11 1310 1315 16288300
- Campbell RK Type 2 diabetes: where we are today. An overview of disease burden, current treatments, and treatment strategies J Am Pharm Assoc (2003) 2009 49 Suppl 1 S3 S9 19801365
- Fisman EZ Tenenbaum A A cardiologic approach to non-insulin antidiabetic pharmacotherapy in patients with heart disease Cardiovasc Diabetol 2009 8 38 50 19619327
- Wilson PWF Kannel WB Silbershatz H D’Agostino RB Clustering of metabolic factors and coronary heart disease Arch Intern Med 1999 159 10 1104 1109 10335688
- Dagenais GR Yi Q Mann JF Bosch J Pogue J Yusuf S Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease Am Heart J 2005 149 1 54 60 15660034
- Pi-Sunyer X Blackburn G Brancati FL Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial Diabetes Care 2007 30 6 1374 1383 17363746
- Shai I Schwarzfuchs D Henkin Y Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet N Engl J Med 2008 359 3 229 241 18635428
- Wing RR Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial Arch Intern Med 2010 170 17 1566 1575 20876408
- Williamson DF Thompson TJ Thun M Flanders D Pamuk E Byers T Intentional weight loss and mortality among overweight individuals with diabetes Diabetes Care 2000 23 10 1499 1504 11023143
- Stevens VJ Obarzanek E Cook NR Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II Ann Intern Med 2001 134 1 1 11 11187414
- Eriksson KF Lindgarde F Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. The 6-year Malmo feasibility study Diabetologia 1991 34 12 891 898 1778354
- Kosaka K Noda M Kuzuya T Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males Diabetes Res Clin Pract 2005 67 2 152 162 15649575
- Hamman RF Wing RR Edelstein SL Effect of weight loss with lifestyle intervention on risk of diabetes Diabetes Care 2006 29 2 2102 2107 16936160
- Orozco LJ Buchleitner AM Gimenez-Perez G Roque i Figuls M Richter B Mauricio D Exercise or exercise and diet for preventing type 2 diabetes mellitus Cochrane Database Syst Rev 2008 3 CD003054 18646086
- Klein S Sheard NF Pi-Sunyer X Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition Diabetes Care 2004 27 8 2067 2073 15277443
- American Diabetes Association Standards of medical care in diabetes– 2011 Diabetes Care 2011 34 Suppl 1 S11 S61 21193625
- Nathan DM Buse JB Davidson MB Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes Diabetes Care 2009 32 1 193 203 18945920
- Rodbard HW Jellinger PS Davidson JA Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control Endocr Pract 2009 15 6 540 559 19858063
- Albu JB Heilbronn LK Kelley DE Metabolic changes following a 1-year diet and exercise intervention in patients with type 2 diabetes Diabetes 2010 59 3 627 633 20028945
- Thomas D Elliott EJ Low glycaemic index, or low glycaemic load, diets for diabetes mellitus Cochrane Database Syst Rev 2009 1 CD006296 19160276
- Westman EC Yancy WSJr Mavropoulos JC Marquart M McDuffie JR The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus Nutr Metab (Lond) 2008 5 36 19099589
- Nuttall FQ Schweim K Hoover H Gannon MC Effect of the LoBAG30 diet on blood glucose control in people with type 2 diabetes Br J Nutr 2008 99 3 511 519 17868489
- Jazet IM de Craen AJ van Schie EM Meinders AE Sustained beneficial metabolic effects 18 months after a 30-day very low calorie diet in severely obese, insulin-treated patients with type 2 diabetes Diabetes Res Clin Pract 2007 77 1 70 76 17134786
- Joslin Diabetes Center and Joslin Clinic Clinical Guideline for Pharmacological Management of Type 2 Diabetes January 9 2009 updated November, 2010. Available from: http://www.joslin.org/bin_from_cms/Pharma_guideline_11._10.pdf Accessed July 28, 2011
- Bolen S Feldman L Vassy J Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus Ann Intern Med 2007 147 6 386 399 17638715
- Schernthaner G Matthews DR Charbonnel B Hanefeld M Brunetti P Efficacy and safety of pioglitazone versus metformin in patients with type 2 diabetes mellitus: a double-blind, randomized trial J Clin Endocrinol Metab 2004 89 12 6068 6076 15579760
- Siraj ES Is there a role for metformin or acarbose as a weight-loss agent in the absence of diabetes? Cleve Clin J Med 2003 70 8 702 704 12959396
- Virtanen KA Hallsten K Parkkola R Differential effects of rosiglitazone and metformin on adipose tissue distribution and glucose uptake in type 2 diabetic subjects Diabetes 2003 52 2 283 290 12540598
- Jorgensen CH Gislason GH Andersson C Effects of oral glucose-lowering drugs on long term outcomes in patients with diabetes mellitus following myocardial infarction not treated with emergent percutaneous coronary intervention–a retrospective nationwide cohort study Cardiovasc Diabetol 2010 9 54 20843380
- Brownstein JS Murphy SN Goldfine AB Rapid identification of myocardial infarction risk associated with diabetes medications using electronic medical records Diabetes Care 2010 33 3 526 531 20009093
- Chaudhry ZW Gannon MC Nuttall FQ Stability of body weight in type 2 diabetes Diabetes Care 2006 29 3 493 497 16505494
- Moses R Slobodniuk R Boyages S Effect of repaglinide addition to metformin monotherapy on glycemic control in patients with type 2 diabetes Diabetes Care 1999 22 1 119 124 10333912
- Black C Donnelly P McIntyre L Royle PL Shepherd JP Thomas S Meglitinide analogues for type 2 diabetes mellitus Cochrane Database Syst Rev 2007 2 CD004654 17443551
- van de Laar FA Lucassen PL Akkermans RP van de Lisdonk EH Rutten GE van Weel C Alpha-glucosidase inhibitors for type 2 diabetes mellitus Cochrane Database Syst Rev 2005 2 CD003639 15846673
- Chiasson JL Acarbose for the prevention of diabetes, hypertension, and cardiovascular disease in subjects with impaired glucose tolerance: the Study to Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM) Trial Endocr Pract 2006 12 Suppl 1 25 30 16627376
- Hsieh SH Shih KC Chou CW Chu CH Evaluation of the efficacy and tolerability of miglitol in Chinese patients with type 2 diabetes mellitus inadequately controlled by diet and sulfonylureas Acta Diabetol 2011 48 1 71 77 20963449
- Nemoto M Tajima N Kawamori R Efficacy of combined use of miglitol in Type 2 diabetes patients receiving insulin therapy-placebo-controlled double-blind comparative study Acta Diabetol 2011 48 1 15 20 20617348
- Defronzo RA Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus Diabetes 2009 58 4 773 795 19336687
- Singh S Loke YK Furberg CD Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis JAMA 2007 298 10 1189 1195 17848653
- Wertz DA Chang CL Sarawate CA Willey VJ Cziraky MJ Bohn RL Risk of cardiovascular events and all-cause mortality in patients treated with thiazolidinediones in a managed-care population Circ Cardiovasc Qual Outcomes 2010 3 5 538 545 20736441
- Buyken AE von Eckardstein A Schulte H Cullen P Assmann G Type 2 diabetes mellitus and risk of coronary heart disease: results of the 10-year follow-up of the PROCAM study Eur J Cardiovasc Prev Rehabil 2007 14 2 230 236 17446801
- Lecka-Czernik B Bone loss in diabetes: use of antidiabetic thiazolidinediones and secondary osteoporosis Curr Osteoporos Rep 2010 8 4 178 184 20809203
- Lewis JD Ferrara A Peng T Risk of bladder cancer among diabetic patients treated with pioglitazone: interim report of a longitudinal cohort study Diabetes Care 2011 34 4 916 922 21447663
- Victoza® (liraglutide [rDNA origin] injection), solution for subcutaneous use (prescribing information) Princeton, NJ Novo Nordisk Inc. 5 2011
- Fonseca VA Zinman B Nauck MA Goldfine AB Plutzky J Confronting the type 2 diabetes epidemic: the emerging role of incretin-based therapies Am J Med 2010 123 7 S2 S10 20609666
- Neumiller JJ Differential chemistry (structure), mechanism of action, and pharmacology of GLP-1 receptor agonists and DPP-4 inhibitors J Am Pharm Assoc (2003) 2009 49 Suppl 1 S16 S29 19801361
- Monami M Marchionni N Mannucci E Glucagon-like peptide-1 receptor agonists in type 2 diabetes: a meta-analysis of randomized clinical trials Eur J Endocrinol 2009 160 6 909 917 19318378
- Amori RE Lau J Pittas AG Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis JAMA 2007 298 2 194 206 17622601
- Buse JB Rosenstock J Sesti G Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6) Lancet 2009 374 9683 39 47 19515413
- Jendle J Nauck MA Matthews DR Weight loss with liraglutide, a once-daily human glucagon-like peptide-1 analogue for type 2 diabetes treatment as monotherapy or added to metformin, is primarily as a result of a reduction in fat tissue Diabetes Obes Metab 2009 11 12 1163 1172 19930006
- Pinkney J Fox T Ranganath L Selecting GLP-1 agonists in the management of type 2 diabetes: differential pharmacology and therapeutic benefits of liraglutide and exenatide Ther Clin Risk Manage 2010 6 401 411
- Anderson SL Trujillo JM Association of pancreatitis with glucagon-like peptide-1 agonist use Ann Pharmacother 2010 44 904 909 20371755
- Pratley RE Overview of glucagon-like peptide-1 analogs and dipeptidyl peptidase-4 inhibitors for type 2 diabetes Medscape J Med 2008 10 7 171 18769687
- Richter B Bandeira-Echtler E Bergerhoff K Lerch CL Dipeptidyl peptidase-4 (DPP-4) inhibitors for type 2 diabetes mellitus Cochrane Database Syst Rev 2008 2 CD006739 18425967
- Frederich R Alexander JH Fiedorek FT A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes Postgrad Med 2010 122 3 16 27 20463410
- Pratley RE Nauck M Bailey T Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial Lancet 2010 375 9724 1447 1456 20417856
- Younk LM Mikeladze M Davis SN Pramlintide and the treatment of diabetes: a review of the data since its introduction Expert Opin Pharmacother 2011 12 9 1439 1451 21564002
- Singh-Franco D Perez A Harrington C The effect of pramlintide acetate on glycemic control and weight in patients with type 2 diabetes mellitus and in obese patients without diabetes: a systematic review and meta-analysis Diabetes Obes Metab 2011 13 2 169 180 21199269
- Ryan GJ Jobe LJ Martin R Pramlintide in the treatment of type 1 and type 2 diabetes mellitus Clin Ther 2005 27 10 1500 1512 16330288
- Chao EC A paradigm shift in diabetes therapy – dapagliflozin and other SGLT2 inhibitors Discov Med 2011 11 58 255 263 21447284
- Strojek K Yoon K Hruba V Elze M Langkilde A Parikh S Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomised, 24-week, double-blind, placebo-controlled trial Diabetes Obes Metab 2011 13 10 928 938 21672123
- Bailey CJ Gross JL Yadav M Nayyar I Mansfield TA List JF Long-term efficacy of dapagliflozin as add-on to metformin (MET) in T2DM inadequately controlled with MET alone [abstract] Diabetes 2011 60 Suppl 1 Abstract 0988-P
- Fiore K MedPage Today. ADA: Novel drug controls glucose, but may have cancer risk June 29 2011 Available from: http://www.medpagetoday.com/MeetingCoverage/ADA/27345 Accessed August 4, 2011
- Meece J Dispelling myths and removing barriers about insulin in type 2 diabetes Diabetes Educ 2006 32 1 Suppl 9S 18S 16439485
- Hartman I Insulin analogs: impact on treatment success, satisfaction, quality of life, and adherence Clin Med Res 2008 6 2 54 67 18801953
- Groop L Widen E Franssila-Kallunki A Different effects of insulin and oral antidiabetic agents on glucose and energy metabolism in type 2 (non-insulin-dependent) diabetes mellitus Diabetologia 1989 32 8 599 605 2506091
- Birkeland KI Hanssen KF Urdal P Berg K Vaaler S A long-term, randomized, comparative study of insulin versus sulfonylurea therapy in type 2 diabetes J Intern Med 1994 236 3 305 313 8077888
- Sinha A Formica C Tsalamandris C Effects of insulin on body composition in patients with insulin-dependent and non-insulin-dependent diabetes Diabet Med 1996 13 1 40 46 8741811
- Monami M Marchionni N Mannucci E Long-acting insulin analogues versus NPH human insulin in type 2 diabetes: a meta-analysis Diabetes Res Clin Pract 2008 81 2 184 189 18495286
- Bazzano LA Lee LJ Shi L Reynolds K Jackson JA Fonseca V Safety and efficacy of glargine compared with NPH insulin for the treatment of type 2 diabetes: a meta-analysis of randomized controlled trials Diabet Med 2008 25 8 924 932 18959605
- Hermansen K Davies M Derezinski T Martinez Ravn G Clauson P Home P A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes Diabetes Care 2006 29 6 1269 1274 16732007
- Fajardo Montanana C Hernandez Herrero C Rivas Fernandez M Less weight gain and hypoglycaemia with once-daily insulin detemir than NPH insulin in intensification of insulin therapy in overweight type 2 diabetes patients – the PREDICTIVE™ BMI clinical trial Diabet Med 2008 25 8 916 923 18959604
- Haak T Tiengo A Draeger E Suntum M Waldhausl W Lower within-subject variability of fasting blood glucose and reduced weight gain with insulin detemir compared to NPH insulin in patients with type 2 diabetes Diabetes Obes Metab 2005 7 1 56 64 15642076
- Raskin P Gylvin T Weng W Chaykin L Comparison of insulin detemir and insulin glargine using a basal-bolus regimen in a randomized, controlled clinical study in patients with type 2 diabetes Diabetes Metab Res Rev 2009 25 6 542 548 19565569
- Hermansen K Davies M Does insulin detemir have a role in reducing risk of insulin-associated weight gain? Diabetes Obes Metab 2007 9 3 209 217 17391147
- Hallschmid M Jauch-Chara K Korn O Euglycemic infusion of insulin detemir compared to human insulin appears to increase direct current brain potential response and reduces food intake while inducing similar systemic effects Diabetes 2010 59 4 1101 1107 20068139
- Plank J Bodenlenz M Sinner F A double-blind, randomized, dose-response study investigating the pharmacodynamic and pharmacokinetic properties of the long-acting insulin analog detemir Diabetes Care 2005 28 5 1107 1112 15855574
- Tone A Iseda I Higuchi C Comparison of insulin detemir and insulin glargine on glycemic variability in patients with type 1 and type 2 diabetes Exp Clin Endocrinol Diabetes 2010 118 5 320 324 20072962
- Apovian CM Gokce N Clinician update: obesity and cardiovascular disease Circulation 2011
- Weight Control Information Network; National Institute of Diabetes and Digestive and Kidney Diseases Prescription medications for the treatment of obesity 11 2004 updated Dec, 2010. Available from: http://win.niddk.nih.gov/Publications/prescription.htm Accessed July 28, 2011
- Li Z Maglione M Tu W Meta-analysis: pharmacologic treatment of obesity Ann Intern Med 2005 142 7 532 546 15809465
- Hutton B Fergusson D Changes in body weight and serum lipid profile in obese patients treated with orlistat in addition to a hypocaloric diet: a systematic review of randomized clinical trials Am J Clin Nutr 2004 80 6 1461 1468 15585756
- Torgerson JS Hauptman J Boldrin MN Sjostrom L XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients Diabetes Care 2004 27 1 155 161 14693982
- Kopelman P Groot Gde H Rissanen A Weight loss, HbA1c reduction, and tolerability of cetilistat in a randomized, placebo-controlled phase 2 trial in obese diabetics: comparison with orlistat (Xenical) Obesity (Silver Spring) 2010 18 1 108 115 19461584
- Le Riche WH Van Belle G Study of phendimetrazine bitartrate as an appetite suppressant in relation to dosage, weight loss and side effects Can Med Assoc J 1962 87 29 31 14463177
- Fletcher PC Napolitano A Skeggs A Distinct modulatory effects of satiety and sibutramine on brain responses to food images in humans: a double dissociation across hypothalamus, amygdala, and ventral striatum J Neurosci 2010 30 43 14346 14355 20980590
- US Food and Drug Administration Abbott Laboratories agrees to withdraw its obesity drug Meridia [press release] October 8 2010 Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm228812.htm Accessed July 28, 2011
- James WP Caterson ID Coutinho W Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects N Engl J Med 2010 363 10 905 917 20818901
- Harrison-Woolrych M Ashton J Herbison P Fatal and non-fatal cardiovascular events in a general population prescribed sibutramine in New Zealand: a prospective cohort study Drug Saf 2010 33 7 605 613 20553061
- Bello NT Liang NC The use of serotonergic drugs to treat obesity – is there any hope? Drug Des Devel Ther 2011 5 95 109
- Smith SR Weissman NJ Anderson CM Multicenter, placebo-controlled trial of lorcaserin for weight management N Engl J Med 2010 363 3 245 256 20647200
- Astrup A Madsbad S Breum L Jensen TJ Kroustrup JP Larsen TM Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial Lancet 2008 372 9653 1906 1913 18950853
- Fraende M Reuters. Neurosearch seeking partner for obesity drug [press release] May 26 2011 Available from: http://www.reuters.com/article/2011/05/26/neurosearch-idUSLDE74212620110526 Accessed July 28, 2011
- Shionogi and Co, Ltd Research and development at Shionogi March 10 2011 Available from: http://www.shionogi.co.jp/ir_en/explanatory/pdf/e_p110310.pdf Accessed July 28, 2011
- Yukioka H A potent and selective neuropeptide Y Y5-receptor antagonist, S-2367, as an anti-obesity agent Nippon Yakurigaku Zasshi 2010 136 5 270 274 Japanese 21079365
- Klonoff DC Greenway F Drugs in the pipeline for the obesity market J Diabetes Sci Technol 2008 2 5 913 918 19885278
- Wadden TA Foreyt JP Foster GD Weight loss with naltrexone SR/Bupropion SR combination therapy as an adjunct to behavior modification: The COR-BMOD Trial Obesity (Silver Spring) 2011 19 1 110 120 20559296
- Wood S Heartwire. FDA declines approval for Contrave diet drug; asks for CVD outcomes studies [press release] February 1 2011 Available from: http://www.medscape.com/viewarticle/736616 Accessed July 28, 2011
- Ioannides-Demos LL Piccenna L McNeil JJ Pharmacotherapies for obesity: past, current, and future therapies J Obes 2011 2011 179674 21197148
- Bays H Phentermine, topiramate and their combination for the treatment of adiposopathy (‘sick fat’) and metabolic disease Expert Rev Cardiovasc Ther 2010 8 12 1777 1801 20707765
- Miller R Heartwire. FDA rejects Qnexa, asks for more info [press release] October 29 2010 Available from: http://www.medscape.com/viewarticle/731653 Accessed July 28, 2011
- Hunt S Russell A Smithson WH Topiramate in pregnancy: preliminary experience from the UK Epilepsy and Pregnancy Register Neurology 2008 71 4 272 276 18645165
- US Food and Drug Administration FDA Drug Safety Communication: risk of oral clefts in children born to mothers taking Topamax (topiramate) March 4 2011 Available from: http://www.fda.gov/Drugs/DrugSafety/ucm245085.htm Accessed July 28, 2011
- Ravussin E Smith SR Mitchell JA Enhanced weight loss with pramlintide/metreleptin: an integrated neurohormonal approach to obesity pharmacotherapy Obesity (Silver Spring) 2009 17 9 1736 1743 19521351
- Astrup A Rossner S van Gaal L Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study Lancet 2009 374 9701 1606 1616 19853906
- Weight Control Information Network and National Institute of Diabetes and Digestive and Kidney Diseases Bariatric surgery for severe obesity. [Page on the Internet.] 3 2009 Available from: http://win.niddk.nih.gov/publications/gastric.htm#whataresurg Accessed July 28, 2011
- Ferchak CV Meneghini LF Obesity, bariatric surgery and type 2 diabetes – a systematic review Diabetes Metab Res Rev 2004 20 6 438 445 15386803
- Buchwald H Avidor Y Braunwald E Bariatric surgery: a systematic review and meta-analysis JAMA 2004 292 14 1724 1737 15479938
- Rubino F Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis Diabetes Care 2008 31 Suppl 2 S290 S296 18227499
- Rubino F Kaplan LM Schauer PR Cummings DE The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus Ann Surg 2010 251 3 399 405 19934752
- Rodriguez-Grunert L Galvao Neto MP Alamo M Ramos AC Baez PB Tarnoff M First human experience with endoscopically delivered and retrieved duodenal-jejunal bypass sleeve Surg Obes Relat Dis 2008 4 1 55 59 18201671
- US Food and Drug Administration Gastroenterology and Urology Devices Panel Meeting December 3 2010 Available from: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/Gastroenterology-UrologyDevicesPanel/UCM236137.pdf Accessed July 28, 2011
- Ponce J Haynes B Paynter S Effect of lap-band-induced weight loss on type 2 diabetes mellitus and hypertension Obes Surg 2004 14 10 1335 1342 15603648
- Sjostrom L Narbro K Sjostrom CD Effects of bariatric surgery on mortality in Swedish obese subjects N Engl J Med 2007 357 8 741 752 17715408
- Pournaras DJ Osborne A Hawkins SC Remission of type 2 diabetes after gastric bypass and banding: mechanisms and 2 year outcomes Ann Surg 2010 252 6 966 971 21107106
- Kashyap SR Daud S Kelly KR Acute effects of gastric bypass versus gastric restrictive surgery on beta-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes Int J Obes (Lond) 2010 34 3 462 471 20029383
- Thaler JP Cummings DE Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery Endocrinology 2009 150 6 2518 2525 19372197
- Rubino F Moo TA Rosen DJ Dakin GF Pomp A Diabetes surgery: a new approach to an old disease Diabetes Care 2009 32 Suppl 2 S368 S372 19875583
- le Roux CW Aylwin SJ Batterham RL Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters Ann Surg 2006 243 1 108 114 16371744
- Bose M Machineni S Olivan B Superior appetite hormone profile after equivalent weight loss by gastric bypass compared to gastric banding Obesity (Silver Spring) 2010 18 6 1085 1091 20057364
- Laferrere B Swerdlow N Bawa B Rise of oxyntomodulin in response to oral glucose after gastric bypass surgery in patients with type 2 diabetes J Clin Endocrinol Metab 2010 95 8 4072 4076 20501690
- Moore TJ Alsabeeh N Apovian CM Weight, blood pressure, and dietary benefits after 12 months of a Web-based Nutrition Education Program (DASH for health): longitudinal observational study J Med Internet Res 2008 10 4 e52 19073541
- Lee WC Conner C Hammer M Cost-effectiveness of liraglutide versus rosiglitazone, both in combination with glimepiride in treatment of type 2 diabetes in the US Curr Med Res Opin 2011 27 5 897 906 21348806
- Minshall ME Oglesby AK Wintle ME Valentine WJ Roze S Palmer AJ Estimating the long-term cost-effectiveness of exenatide in the United States: an adjunctive treatment for type 2 diabetes mellitus Value Health 2008 11 1 22 33 18237357
- Tunis SL Minshall ME Conner C Cost-effectiveness of insulin detemir compared to NPH insulin for type 1 and type 2 diabetes mellitus in the Canadian payer setting: modeling analysis Curr Med Res Opin 2009 25 5 1273 1284 19366302
- Picot J Jones J Colquitt JL The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation [review] Health Technol Assess 2009 13 41 iii iv 1 190