Abstract
Introduction
Obesity is associated with a state of chronic inflammation, and increased cardiometabolic disease risk. The present study examined the relationship between body mass index (BMI) and cardiometabolic and inflammatory biomarkers among normal weight, overweight, and obese Canadian adults.
Methods
Subjects (n = 1805, aged 18 to 79 years) from the Canadian Health Measures Survey (CHMS) were examined for associations between BMI, cardiometabolic markers (apolipoprotein [Apo] A1, ApoB, low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C], total cholesterol, total cholesterol/HDL ratio [total:HDL-C ratio], triglycerides, and glycosylated hemoglobin [HbA1c]), inflammatory factors (C-reactive protein [CRP], fibrinogen, and homocysteine), and 25-hydroxyvitamin D [25(OH)D]. Bootstrap weights for variance and sampling weights for point estimates were applied to account for the complex survey design. Linear regression models adjusted for age, sex, physical activity, smoking status, and ethnicity (in addition to season of clinic visit, for vitamin D analyses only) were used to examine the association between cardiometabolic markers, inflammatory factors, and BMI in Canadian adults.
Results
All biomarkers were significantly associated with BMI (P ≤ 0.001). ApoA1 (β = −0.31, P < 0.0001), HDL-C (β = −0.61, P < 0.0001), and 25(OH)D (β = −0.25, P < 0.0001) were inversely associated with BMI, while all other biomarkers showed positive linear associations. Distinct patterns of association were noted among normal weight, overweight, and obese groups, excluding CRP which showed a significant positive association with BMI in the overall population (β = 2.80, P < 0.0001) and in the normal weight (β = 3.20, P = 0.02), overweight (β = 3.53, P = 0.002), and obese (β = 2.22, P = 0.0002) groups.
Conclusions
There is an apparent profile of cardiometabolic and inflammatory biomarkers that emerges as BMI increases from normal weight to obesity. Understanding these profiles may permit developing an effective approach for early risk prediction for cardiometabolic disease.
Background
Approximately 25% of Canadians are obese according to measured height and weight data from 2007–2009.Citation1 Obesity reduces length and quality of life and is associated with a number of chronic conditions including type 2 diabetes mellitus (T2DM), hypertension, cardiovascular disease (CVD), and some forms of cancer.Citation2 In addition, obesity has been shown to adversely impact psychosocial and psychological wellbeing. Citation3 As levels of obesity continue to rise globally, it is critical to understand the metabolic consequences of this condition and its etiological role in the development of chronic diseases.
Once thought only to be an energy storehouse, it is now well recognized that adipose tissue has endocrine functions including the secretion of proinflammatory cytokines. Indeed, a common link between obesity and several comorbid conditions, including CVD and T2DM, is a state of chronic low-grade inflammation that accompanies these chronic conditions.Citation4,Citation5 Obesity is associated with an increase in adipose tissue that results in higher circulating levels of free fatty acids, which in turn, inhibit insulin-stimulated glucose uptake.Citation6 This ultimately leads to increased plasma glucose levels, and elevated insulin synthesis and production.Citation6 Adipose tissue also secretes a variety of cytokines, such as the proinflammatory Tumor necrosis factor (TNF-α) and Interleukin-6 (IL-6),Citation5 which can activate signal transduction cascades that inhibit insulin action.Citation7 IL-6 also stimulates production of acute phase proteins, such as C-reactive protein (CRP) and fibrinogen in the liver, which are markers of increased CVD risk.Citation8,Citation9
Currently, there is great interest in understanding the potential role of vitamin D, a micronutrient with anti-inflammatory properties, in modulating low-grade inflammation.Citation10 Low circulating levels of 25(OH)D, the vitamin D metabolite used to determine vitamin D status, have been associated with an increased number of metabolic syndrome components and insulin resistance in the Canadian population,Citation11 suggesting that low concentrations of this micronutrient may be a biomarker of cardiometabolic risk. However, the relationship between vitamin D and obesity among Canadians remains poorly explored. Furthermore, despite evidence suggesting a role for cardiometabolic and inflammatory markers in chronic disorders,Citation12 the change in their profile as body weight increases from normal to obese remains poorly explored. Elucidating these relationships may enable us to further understand the metabolic changes in obesity that can be involved in the early stages of T2DM and CVD. Furthermore, it may provide the basis for developing effective population-based preventive strategies for the range of chronic diseases that are linked to obesity. The objective of the present study was to examine the association between the different body mass index (BMI) states and a number of cardiometabolic and inflammatory biomarkers, and circulating 25(OH)D, in a representative sample of the adult Canadian population.
Methods
Study design and population
Data come from the Canadian Health Measures Survey (CHMS) cycle 3.1, which is a population-based survey designed to collect information on the health and wellness of Canadians aged 6 to 79 years, from households in the ten provinces and three territories of Canada. Complete details of the study design and data collection have been published elsewhere.Citation13–Citation16 Briefly, a multi-stage sampling strategy was used to identify 15 collection sites from which data was collected between March 2007 and February 2009. Those living on Aboriginal Reserves or Crown Lands, in institutions and certain remote regions, and full-time members of the Canadian Forces were not captured by this survey. The CHMS represents 96.3% of the Canadian population. A total of 8772 dwellings were selected for survey with 6106 agreeing to participate, for a household response rate of 69.6%. From these households, 6604 subjects of the 7483 selected agreed to respond to the study questionnaire, for a response rate of 88.3%. Of those who agreed, 5604 also visited the mobile examination centre for collection of physical measurements, for a response rate of 84.9%. This resulted in an overall response rate of 51.7% at the national level.
The study was reviewed and approved by the Health Canada Research Ethics Board.Citation15 All subjects signed a consent form prior to participating in the study. Participation was voluntary and included a household interview, and visit to a mobile examination centre for physical measurements, and collection of blood and urine samples. Each dwelling was randomly selected to receive a morning or afternoon clinic appointment. Only those who received a morning appointment were required to be fasted for blood measures. In the present study, only fasting responders were included in the analysis (n = 2634). As Health Canada recommends the use of BMI classifications for adults aged 18 years and older only,Citation17 all subjects under the age of 18 were also excluded (n = 829). Therefore, the present analysis includes 1805 subjects, representing, when weighted, 24,624,702 Canadians.
Metabolic markers, BMI classification, and other covariates
Assessment of biomarkers from blood samples were analyzed at the Health Canada Laboratory, Bureau of Nutritional Sciences, Nutrition Research Division using standard operating procedures. Blind replicates and quality control samples including known analyte concentrations, and field blanks were periodically sent with collected samples to monitor precision and accuracy.Citation14 A number of metabolic indices and disease markers were measured in the CHMS,Citation14 and were available for the present study. These included cardiometabolic disease markers (apolipoprotein [Apo] A1 [g/L], ApoB [g/L], low-density lipoprotein cholesterol [LDL-C] [mmol/L], high-density lipoprotein cholesterol [HDL-C] [mmol/L], total cholesterol [mmol/L], total cholesterol/HDL ratio [total:HDL-C ratio], triglycerides [mmol/L], and glycosylated hemoglobin [HbA1c] [%]); inflammatory biomarkers (CRP [mg/L], fibrinogen [g/L], and homocysteine [μmol/L]); systolic and diastolic blood pressure; and plasma 25-hydroxyvitamin D (25(OH)D) (nmol/L).
Subject’s BMI (weight in kg/height in m2) derived from measured height and weight was used to categorize subjects into underweight (BMI < 18.5, n = 26 – this group was excluded from the stratified analyses), normal weight (18.5 ≤ BMI < 25, n = 660), overweight (25 ≤ BMI < 30, n = 680), and obese (BMI ≥ 30, n = 429) groups (n = 10 missing BMI data). Waist circumference was measured at the mid-point between the top of the iliac crest and the last floating rib in the midaxillary line using a Gulick measuring tape (Fitness Mart®, Grays Mills, WI).Citation18 Smoking status was self-reported and was further subdivided into ever (daily, occasional, former daily, and former occasional) or never smoked. Ethnicity was categorized into three main subgroups from the twelve ethnic groups reported in the CHMS, to allow for adequate sample size within each group, and to minimize the associated degrees of freedom in adjusted models. The three groups included Caucasians, Asians (Koreans, Filipinos, Japanese, Chinese, South Asians, Southeast Asians, Arabs, and West Asians), and Others (African Canadians, Latin Americans, and mixed). Subjects were dichotomized based on the past-month use of cardiac medications (lipid lowering medications, blood pressure medication, or other medications with direct effects on the circulatory system). Self-reported use of medication was collected, and coded using the American Hospital Formulary Service drug code. Physical activity was assessed based on average daily energy expenditure in leisure time physical activities (kcal/kg/day) in the past 3 months, and were categorized as inactive (0–1.5), moderate (1.5–3), and active (≥3).
Statistical analysis
Data analysis was conducted using survey procedures in SAS version 9.2 (SAS Institute, Inc, Cary, NC). In all analyses, bootstrap weights for variance estimates and sampling weights for point estimates were applied to account for the complex survey design. All tests were conducted with eleven degrees of freedom. The distribution of continuous variables was examined by plotting histograms. If skewed, variables were natural log transformed to improve linearity of relationships and normality of residuals. Scatter plots of the untransformed, unadjusted, and unweighted data for BMI and biomarkers were generated using linear regression lines to fit within each BMI group. The top 1% of biomarker values for HbA1c, and 25(OH)D were excluded from the plots as potential outliers.
Linear regression was used to examine the association between BMI and biomarkers in the entire population with adjustments for age, sex, smoking status (ever, never), physical activity (inactive, moderate, active), and ethnicity (Caucasian, Asian, Other). Regressions examining associations with 25(OH)D were additionally adjusted for season of clinic visit. Linear regression was also run within each BMI group. To assess potential confounding by medications which impact on CVD markers, analyses were also run with the addition of a dichotomized variable for cardiac drug use. To further analyze potential confounding by diabetes diagnosis, analyses were also run after excluding subjects self-reporting having been diagnosed with type 1 or type 2 diabetes by a health professional, or who had a fasting plasma glucose > 7.0 mmol/L. All P-values < 0.05 were considered significant.
To generate adjusted mean levels of the biomarkers within each of the BMI groups, least square means were produced in regression models which examined biomarkers and BMI categories adjusted for age, sex, smoking status, physical activity, and ethnicity. Least square means for vitamin D by BMI group were adjusted for age, sex, physical activity, ethnicity, and season of clinic visit. Untransformed means are presented for interpretability.
Results
Subject characteristics including mean levels of cardiometabolic biomarkers are presented in . Approximately half of the study population was female, with a mean age of 44 years. The majority of the sample was made up of inactive subjects (55%) and those who never smoked (53%). The population was predominantly Caucasian (84%), free of diabetes (96%), and not taking any cardiac medications (82%). Mean levels of cardiometabolic biomarkers, including blood pressure and waist circumference, fell within normal clinical ranges; however, the average BMI of the population fell within the overweight range (26.9).
Table 1 Population characteristics
The associations between cardiometabolic markers of disease and BMI are shown in the overall population in . The number of subjects, adjusted mean level, and standard error for each biomarker are also shown stratified by BMI group. All biomarkers were significantly associated with BMI in the overall study population. The association between BMI and homocysteine was no longer significant after adjustment for use of cardiac medications (P = 0.1), or when individuals with diabetes were excluded from the analysis (P = 0.6). Most biomarkers were positively associated with BMI. Only ApoA1 (β = −0.31, P < 0.0001), HDL-C (β = −0.61, P < 0.0001), and 25(OH)D (β = −0.25, P < 0.0001) were inversely associated with BMI. Some metabolic markers remained significantly associated with BMI within the normal weight and overweight BMI groups individually (). Total:HDL-C ratio and triglycerides remained positively associated, while HDL-C remained inversely associated with BMI, in both the normal weight and overweight groups. ApoB, LDL-C, and total cholesterol remained positively associated with BMI in the normal weight group, while ApoA1 remained inversely associated with BMI in the overweight group. HbA1c was not significantly associated with BMI in the normal weight, overweight, or obese groups separately. Among the inflammatory markers, homocysteine was not associated with BMI in the normal weight, overweight, or obese groups, but fibrinogen was positively associated with BMI in the obese group (β = 0.50, P = 0.01, ). CRP remained strongly and positively associated with BMI in normal weight (β = 3.20, P = 0.02), overweight (β = 3.53, P = 0.002), and obese groups (β = 2.22, P = 0.0002). Vitamin D was not significantly associated with BMI in any one BMI group.
Figure 1 Relationship between metabolic markers and BMI by BMI group.
Abbreviations: BMI, body mass index; HbA1c, glycosylated hemoglobin; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; Total:HDL-C ratio, total cholesterol/HDL ratio; SE, standard error.
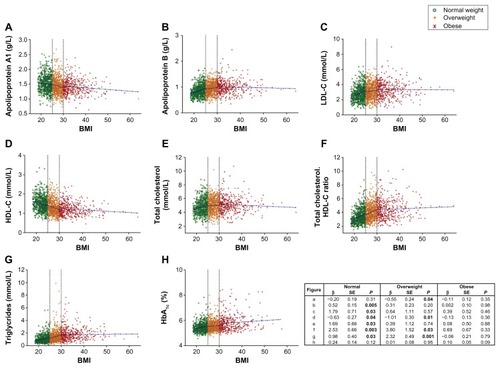
Figure 2 Relationship between BMI and biomarkers of inflammation and plasma vitamin D by BMI groups.
Abbreviations: BMI, body mass index; 25(OH)D, 25-hydroxyvitamin D; CRP, C-reactive protein; SE, standard error.
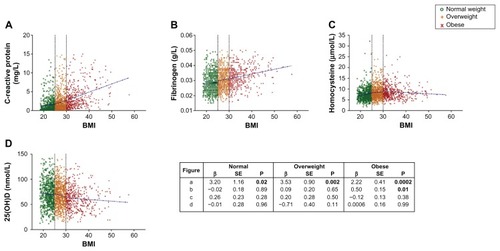
Table 2 Adjusted mean levels of biomarkers by BMI groups
Discussion
Obesity and its associated cardiometabolic and inflammatory changes contribute to increased risk of chronic conditions including T2DM and CVD.Citation4,Citation5 Dyslipidemia associated with obesity is an example of such a change, and is characterized by increased small, dense LDL, ApoB, and triglycerides, and low HDL.Citation19 In obesity, an increase in lipolysis and fatty acid release, paired with impaired fatty acid uptake in adipocytes, results in increased hepatic uptake of fatty acids. The fatty acids are re-esterified into triglycerides, which are incorporated into VLDL along with ApoB.Citation20 One molecule of ApoB is found in atherogenic lipoprotein particles including VLDL, intermediate density lipoprotein, (IDL) and LDL, making it an important marker of CVD riskCitation21 that has been shown to be positively associated with obesity.Citation22 Levels of ApoB, LDL-C, total cholesterol, total:HDL-C ratio, and triglycerides were all positively associated with BMI in the overall population (). While these positive associations remained significant in the normal weight group, only total:HDL-C ratio and triglycerides remained significant in the overweight group, and none of these markers were significantly associated with BMI in the obese group. In contrast, HDL-C levels tend to be lower in obesity. This may be attributed to increased cholesteryl ester transfer protein and hepatic lipase activity, which results in increased HDL-C catabolism and clearance.Citation20 HDL-C has antioxidant, anti-inflammatory, and antithrombotic roles which may be attributable to the presence of ApoA1,Citation23,Citation24 another important biomarker of CVD risk.Citation25 In the present study, levels of both ApoA1 and HDL-C were inversely associated with BMI in the overall population and among overweight subjects.
Several of the associations identified between metabolic markers and BMI in the population as a whole were only significant in the normal weight and/or overweight groups when examined separately. This plateau effect seen in for the obese group would seem to suggest no further change in metabolic markers with increasing BMI in the obese group; however, these findings should be interpreted cautiously as the obese group had the smallest sample size of the BMI groups, and a strong relationship between obesity and several of these markers is well established.Citation19,Citation20,Citation22
CRP and fibrinogen are acute phase proteins whose concentrations increase in response to inflammation and injury, and both biomarkers are positively associated with CVD risk.Citation8 Homocysteine, an amino acid and byproduct of methionine catabolism, is also a biomarker of inflammationCitation26 and CVD risk, although its utility with regard to the latter has been questioned.Citation27,Citation28 All three of these inflammatory biomarkers have been positively associated with obesity.Citation29,Citation30 In the present study, homocysteine was not associated with BMI among normal weight, overweight, or obese subjects, nor in the whole population after adjusting for cardiac medication use, or when looking exclusively at those without diabetes. Conflicting results between BMI and circulating homocysteine levels have been reported, and a recent study of men and women in Western Japan also showed no association between BMI and plasma homocysteine.Citation31 In contrast, CRP and fibrinogen were positively associated with BMI in the overall population and among obese subjects, with strong positive associations additionally noted among overweight and normal weight subjects for CRP. A wealth of evidence suggests a mechanistic role for increased adiposity in the development of chronic systemic inflammation (for review, see Badawi et al, 2010)Citation4. Adipose tissue secretes numerous cytokines, such as the proinflammatory TNF-α and IL-6, which in turn trigger the hepatic production of acute phase proteins such as CRP and fibrinogen.Citation4,Citation8,Citation9 In particular, visceral lipid accumulations may contribute to cytokine secretion, and exacerbate cardiometabolic risk.Citation32–Citation34 Overall, our results support an association between chronic inflammation and increased BMI, and identify the innate immunity-related inflammatory cascade as a potential target pathway for intervention strategies aimed at reducing the risk of obesity-related chronic diseases in the general population.
Obesity is a key risk factor for T2DM, and is associated with an increased production of inflammatory cytokines and release of free fatty acids, which disrupt insulin signaling and action, and contribute to insulin resistance.Citation4,Citation6 HbA1c, a measure of long-term blood glucose regulation, is a diagnostic measure of T2DM,Citation35 and has been shown to be positively associated with BMI in someCitation36,Citation37 but not all studies.Citation38 In the present study, HbA1c was positively associated with BMI in the entire study population. This significant, albeit weaker (β = 0.11, P < 0.0001) association, however, was not significant within the normal weight, overweight, or obese groups when examined separately. The absence of a significant association with BMI among the BMI subgroups may be due to lower power in these smaller groups, or may be due to the influence of other factors influencing HbA1c not accounted for here, including diet.Citation37
Circulating levels of vitamin D have been inversely associated with obesity.Citation39–Citation43 A potential explanation for such associations may relate to vitamin D sequestration in adipose tissue.Citation44 It has also been suggested that vitamin D may play an active role in obesity, with low levels stimulating synthesis and release of parathyroid hormone, increasing calcium in adipocytes, and promoting weight gain.Citation45 In the present study, BMI was inversely associated with plasma 25(OH)D in the entire study population (), but not within the normal weight, overweight, or obese groups (). This lack of association within BMI subgroups may be a consequence of small sample sizes. Previous research from our group, using the same study population, showed an inverse association between circulating 25(OH)D and number of metabolic syndrome components.Citation11 Vitamin D is thought to modulate cardiometabolic disease risk through its anti-inflammatory and immunomodulatory properties.Citation10,Citation46 When considering the population as a whole, our results lend support to previous research suggesting that 25(OH)D is inversely associated with BMI, but we are unable to determine, based on the available data, whether a low vitamin D status contributes to the development of obesity.
The present study has several limitations. Although BMI is a commonly used indicator of obesity and health risks in large epidemiological studies, BMI provides no information on the distribution and type of body fat, or amount of lean tissue. Therefore, we cannot rule out the possibility of different patterns of cardiometabolic risk being associated with different distributions of body fat (ie, android or gynecoid). However, this study aimed to characterize novel relationships between specific biomarkers and increasing obesity in the Canadian population, and therefore we employed the Health Canada weight classification scheme, which is based on BMI.Citation17 Future research efforts should be directed towards examining whether the observed associations differ across specific obesity types. In addition, detailed information on diet was not available for the present study and associations could not be adjusted for differences in total energy or macro-nutrient intake. Diet can influence many of the biomarkers examined and may confound some of the associations presented. The self-reported nature of some of the data in this study is also a limitation, including the measure of physical activity, which only captures leisure-time physical activities. We cannot rule out the possibility of residual confounding from measured and unmeasured sources, including diet, work- or transportation-related physical activity, sun exposure, or other unmeasured biomarkers, such as leptin. Furthermore, metabolic dysregulation of physiological processes including for eg, glycemic control, might contribute to some of the observed associations, but this study did not consider measures of glucose metabolism such as homeostatic model assessment of insulin resistance (HOMA-IR). This study was cross-sectional in nature, and therefore causality cannot be determined from the presented associations. It is also possible that a single measure of these biomarkers may not be reflective of long-term status and disease risk. In addition, the small size of the obese subgroup may have resulted in insufficient power to detect associations. The present study consisted mainly of Caucasian subjects, and associations may differ in different ethnocultural groups. Future research should examine the association between cardiometabolic biomarkers and obesity in different ethnocultural groups, given known differences in cardiometabolic disease rates in different ethnicities. However, strength of this study includes its measurement of a range of cardiometabolic and inflammatory biomarkers, as well as anthropometrics in a nationally representative sample of the adult Canadian population.
In conclusion, we observed a distinctive profile of metabolic phenotypes – including cardiometabolic disease markers and inflammatory biomarkers – that emerges as BMI increases from normal weight to obesity. These findings may have important implications in developing public health intervention and prevention strategies to reduce the burden of chronic diseases associated with obesity in the general population.
Acknowledgements
Research relating to this manuscript was funded by Public Health Agency of Canada. A. E-S holds a Canada Research Chair in Nutrigenomics.
Disclosure
The authors report no conflicts of interest in this work.
References
- Public Health Agency of Canada Obesity in Canada: A Joint Report from the Public Health Agency of Canada and the Canadian Institute for Health Information 2011 Available from: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/oic-oac/index-eng.php Accessed August 13, 2012
- Guh DP Zhang W Bansback N Amarsi Z Birmingham CL Anis AH The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis BMC Public Health 2009 9 88 19320986
- Fontaine KR Barofsky I Obesity and health-related quality of life Obes Rev 2001 2 3 173 182 12120102
- Badawi A Klip A Haddad P Cole DE Garcia-Bailo B El-Sohemy A Type 2 diabetes mellitus and inflammation: Prospects for biomarkers of risk and nutritional intervention Diabetes Metab Syndr Obes 2010 3 173 186 21437087
- Van Gaal LF Mertens IL De Block CE Mechanisms linking obesity with cardiovascular disease Nature 2006 444 7121 875 880 17167476
- Bray GA Clearfield MB Fintel DJ Nelinson DS Overweight and obesity: the pathogenesis of cardiometabolic risk Clin Cornerstone 2009 9 4 30 40 19789062
- Hotamisligil GS Inflammation and metabolic disorders Nature 2006 444 7121 860 867 17167474
- Danesh J Collins R Appleby P Peto R Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies JAMA 1998 279 18 1477 1482 9600484
- Ridker PM Inflammatory biomarkers and risks of myocardial infarction, stroke, diabetes, and total mortality: implications for longevity Nutr Rev 2007 65 12 Pt 2 S253 S259 18240558
- García-Bailo B El-Sohemy A Haddad PS Vitamins D, C, and E in the prevention of type 2 diabetes mellitus: modulation of inflammation and oxidative stress Biologics 2011 5 7 19 21383912
- Brenner DR Arora P García-Bailo B Plasma vitamin D levels and risk of metabolic syndrome in Canadians Clin Invest Med 2011 34 6 E377 22129928
- Brenner DR Arora P García-Bailo B The relationship between metabolic syndrome and markers of cardiometabolic disease among Canadian adults J Diabetes Metab 2011 S2 3
- Tremblay M Wolfson M Gorber SC Canadian Health Measures Survey: rationale, background and overview Health Rep 2007 18 Suppl S7 S20
- Bryan S St-Denis M Wojtas D Canadian Health Measures Survey: clinic operations and logistics Health Rep 2007 18 Suppl S53 S70
- Day B Langlois R Tremblay M Knoppers BM Canadian Health Measures Survey: ethical, legal and social issues Health Rep 2007 18 Suppl S37 S51
- Giroux S Canadian Health Measures Survey: sampling strategy overview Health Rep 2007 18 Suppl S31 S36
- Health Canada Canadian Guidelines for Body Weight Classification in Adults 2003 Available from: http://www.hc-sc.gc.ca/fn-an/nutrition/weights-poids/guide-ld-adult/index-eng.php Accessed August 13, 2012
- Shields M Tremblay MS Laviolette M Craig CL Janssen I Gorber SC Fitness of Canadian adults: results from the 2007–2009 Canadian Health Measures Survey Health Rep 2010 21 1 21 35 20426224
- Miller WM Nori-Janosz KE Lillystone M Yanez J McCullough PA Obesity and lipids Curr Cardiol Rep 2005 7 6 465 470 16256017
- Bamba V Rader DJ Obesity and atherogenic dyslipidemia Gastroenterology 2007 132 6 2181 2190 17498511
- Carr MC Brunzell JD Abdominal obesity and dyslipidemia in the metabolic syndrome: importance of type 2 diabetes and familial combined hyperlipidemia in coronary artery disease risk J Clin Endocrinol Metab 2004 89 6 2601 2607 15181030
- Zhong L Li Q Jiang Y The ApoB/ApoA1 ratio is associated with metabolic syndrome and its components in a Chinese population Inflammation 2010 33 353 358 20213498
- Walldius G Jungner I Apolipoprotein A-I versus HDL cholesterol in the prediction of risk for myocardial infarction and stroke Curr Opin Cardiol 2007 22 4 359 367 17556890
- Barter PJ Ballantyne CM Carmena R Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: a report of the thirty-person/ten-country panel J Intern Med 2006 259 3 247 258 16476102
- Florvall G Basu S Larsson A Apolipoprotein A1 is a stronger prognostic marker than are HDL and LDL cholesterol for cardiovascular disease and mortality in elderly men J Gerontol Ser A Biol Sci Med Sci 2006 61 12 1262 1266 17234819
- Wu JT Circulating homocysteine is an inflammation marker and a risk factor of life-threatening inflammatory diseases J Biomed Lab Sci 2007 19 4 107 111
- Martí-Carvajal AJ Solà I Lathyris D Salanti G Homocysteine lowering interventions for preventing cardiovascular events Cochrane Database Syst Rev 10 7 2009 4 CD006612 19821378
- Abraham JM Cho L The homocysteine hypothesis: still relevant to the prevention and treatment of cardiovascular disease? Cleve Clin J Med 2010 77 12 911 918 21147945
- Nguyen XM Lane J Smith BR Nguyen NT Changes in inflammatory biomarkers across weight classes in a representative US population: a link between obesity and inflammation J Gastrointest Surg 2009 13 7 1205 1212 19415399
- Papandreou D Mavromichalis I Makedou A Rousso I Arvanitidou M Total serum homocysteine, folate and vitamin B12 in a Greek school age population Clin Nutr 2006 25 5 797 802 16690175
- Nakazato M Maeda T Takamura N Relation of body mass index to blood folate and total homocysteine concentrations in Japanese adults Eur J Nutr 2011 50 7 581 585 21221977
- Matsuzawa Y Funahashi T Nakamura T The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism J Atheroscler Thromb 2011 18 8 629 639 21737960
- Ghanim H Aljada A Hofmeyer D Syed T Mohanty P Dandona P Circulating mononuclear cells in the obese are in a proinflammatory state Circulation 2004 110 12 1564 1571 15364812
- Pfützner A Schöndorf T Tschöpe D PIOfix-study: effects of pioglitazone/metformin fixed combination in comparison with a combination of metformin with glimepiride on diabetic dyslipidemia Diabetes Technol Ther 2011 13 6 637 643 21457065
- American Diabetes Association Executive summary: Standards of medical care in diabetes – 2010 Diabetes Care 2010 33 Suppl 1 S4 S10 20042774
- Zajacova A Dowd JB Burgard SA Overweight adults may have the lowest mortality – do they have the best health? Am J Epidemiol 2011 173 4 430 437 21228416
- Boeing H Weisgerber UM Jeckel A Rose H-J Kroke A Association between glycated hemoglobin and diet and other lifestyle factors in a nondiabetic population: cross-sectional evaluation of data from the Potsdam cohort of the European Prospective Investigation into Cancer and Nutrition Study Am J Clin Nutr 2000 71 5 1115 1122 10799373
- Koga M Matsumoto S Saito H Kasayama S Body mass index negatively influences glycated albumin, but not glycated hemoglobin, in diabetic patients Endocr J 2006 53 3 387 391 16717395
- Mai XM Chen Y Camargo CAJr Langhammer A Cross-sectional and prospective cohort study of serum 25-hydroxyvitamin D level and obesity in adults: The HUNT study Am J Epidemiol 2012 175 10 1029 1036 22312120
- Brock K Huang WY Fraser DR Low vitamin D status is associated with physical inactivity, obesity and low vitamin D intake in a large US sample of healthy middle-aged men and women J Steroid Biochem Mol Biol 2010 121 1–2 462 466 20399270
- Young KA Engelman CD Langefeld CD Association of plasma vitamin D levels with adiposity in Hispanic and African Americans J Clin Endocrinol Metab 2009 94 9 3306 3313 19549738
- Hyppönen E Power C Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors Am J Clin Nutr 2007 85 3 860 868 17344510
- Snijder MB van Dam RM Visser M Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women J Clin Endocrinol Metab 2005 90 7 4119 4123 15855256
- Wortsman J Matsuoka LY Chen TC Lu Z Holick MF Decreased bioavailability of vitamin D in obesity Am J Clin Nutr 2000 72 3 690 693 10966885
- McCarty MF Thomas CA PTH excess may promote weight gain by impeding catecholamine-induced lipolysis-implications for the impact of calcium, vitamin D, and alcohol on body weight Med Hypotheses 2003 61 5–6 535 542 14592784
- Veldman CM Cantorna MT DeLuca HF Expression of 1,25-dihydroxyvitamin D(3) receptor in the immune system Arch Biochem Biophys 2000 374 2 334 338 10666315