Abstract
Purpose
The prevalence of obesity continues to rise. People with obesity are at increased risk of several diseases. We tested an algorithm-based screening program for people with a BMI above 30 kg/m2 and present data on the prevalence of previously undiagnosed obesity-related diseases.
Patients and Methods
Seven hundred and sixty-nine persons with BMI > 30 kg/m2 and age 18–60 years were screened for diabetes (assessed by glycosylated hemoglobin and oral glucose tolerance test at HbA1c 43–48 mmol/mol), sleep apnea (screened by questionnaires and assessed by cardiorespiratory monitoring at indication of sleep disorder), liver steatosis or liver fibrosis (assessed by biochemistry and fibroscan) and arterial hypertension (assessed by both office and 24-hour blood pressure measurement). A reference group of people with a BMI of 18.5–29.9 kg/m2 was established.
Results
Of those referred, 73.0% were women. We identified new diabetes in 4.2%, prediabetes in 9.1%, moderate-to-severe sleep apnea in 25.1%, increased liver fat and increased liver stiffness in 68.1% and 17.4%, respectively, and hypertension or masked hypertension in 19.0%. The prevalence of diseases was much higher among men and increased with BMI. Except for hypertension, we found few participants with undiagnosed disease in the reference group.
Conclusion
An algorithm-based screening program is feasible and reveals undiagnosed obesity-related disease in a large proportion of the participants. The disproportional referral pattern calls for a tailored approach aiming to include more men with obesity.
Trial Registration
Inclusion of the non-obese group was approved by the Scientific Ethics Committee of The Region of Southern Denmark (project identification number: S-20210091), and the study was reported at clinicaltrials.gov (NCT05176132).
Plain Language Summary
The number of people with obesity is going up, and they are at a higher risk for various diseases. We tested a screening program for people referred with a BMI over 30 kg/m2 and presented the prevalence of diseases related to obesity. We screened 769 people aged 18 to 60 years with a BMI over 30 kg/m2 for diabetes (biochemistry and glucose tolerance test), sleep apnea (both questionnaires and home monitoring), liver disease (biochemistry and liver scan) and high blood pressure (office and 24-hour readings). We also tested a reference group of people with BMI 18.5-30 kg/m2. Among those screened, 73.0% were women. We found new cases of diabetes in 4.2%, prediabetes in 9.1%, sleep apnea in 25.1%, increased liver fat in 68.1%, increased liver stiffness in 17.4%, and hypertension or masked hypertension in 19.0%. The diseases were more common in men and increased with both higher BMI and age. Except for hypertension, we found few cases in the reference groups. The screening program uncovered undiagnosed obesity-related diseases in a large group of individuals. The uneven distribution of referrals suggests we need a customized approach to include more men with obesity.
Introduction
Obesity is a major global health challenge and the prevalence of obesity increases in almost every country in the world.Citation1 Despite being among the countries with a smaller than average prevalence of obesity, Denmark has experienced a significant increase in the proportion of people with obesity. Thus, from 2010 to 2021 the proportion of adults with BMI above 25 kg/m2 rose from 46.8% to 52.6%, and the proportion of people with BMI above 30 kg/m2 increased from 13.6% to 18.6%.Citation2
The presence of obesity increases the risk of type 2 diabetes (T2D), obstructive sleep apnea, metabolic dysfunction-associated steatotic liver disease (MASLD), hypertension, osteoarthritis, and several other health-threatening conditions.Citation3–5 Mortality is significantly increased, and a 35-year-old male person with class III obesity (BMI ≥ 40 kg/m2) is predicted to live ten years shorter than a normal weight person of same age.Citation6 People living with obesity work significantly less than normal weight individuals, have more days of sick leave, and experience social disadvantages.Citation7 In addition, people living with obesity report an overall poorer health-related quality of life compared to non-obese people.Citation8
Many cases of obesity-related diseases remain undiagnosed, even though the link to obesity is well established and the diagnosis of obesity is straightforward. This was recently demonstrated for T2D, obstructive sleep apnea, hypertension, and MASLD.Citation9–12 Timely diagnosis is essential for appropriate treatment and for the long-term disease outcome. For example, optimal disease management for T2D in the first years after diagnosis reduces the long-term occurrence of both microvascular complications and death.Citation13
We hypothesize that unrecognized obesity-related disease is frequent in a population of people with obesity. The aim of the present study was to test an algorithm-based screening program in people with BMI above 30 kg/m2. We here report results from the first 769 persons with obesity and a control group of people with BMI 18.5–29.9 kg/m2; (N = 161).
Materials and Methods
Study Design and Population
The South Danish Obesity Initiative (SDOI) is a population-based cohort study. The study population consists of people with BMI above 30 kg/m2 aged 18 to 60 years at inclusion. No further inclusion or exclusion criteria are defined. Participants were referred either from their general practitioners or from hospital departments. Inclusion started in September 2020, and data until December 31st, 2023, are included in the present manuscript. In order to be able to draw valid conclusions regarding the impact of obesity, we also included a reference group of people with BMI 18.5–29.9 kg/m2. Inclusion of the non-obese control group was approved by The Regional Committees on Health Research Ethics for Southern Denmark (project identification number: S-20210091), and the study is registered at clinicaltrials.gov (NCT05176132). The study procedures comply with the Declaration of Helsinki. Participants in the group of people living with obesity participated as part of a voluntary screening program, while the reference groups gave written informed consent to participate in the examinations. Both groups gave written consent to the use of their data for clinical and research purposes.
Recruitment
Participants complying with the inclusion criteria were referred to the Department of Endocrinology from general practitioners in the uptake area of the hospital and from any departments of the University Hospital Southern Denmark, Esbjerg and the Department of Psychiatry, Esbjerg, Denmark. The reference group was recruited by announcements on social media, notices at the hospital, and on the online Recruitment platform www.forsøgsperson.dk. Recruitment of participants, both people living with obesity and the reference population, is ongoing. Data for this manuscript were extracted by December 31st, 2023.
Establishment of a Board of Participants
To ensure that the procedures of the screening program comply with the needs of the target group, we established a participant advisory board. We invited people through advertisement on the Facebook profile of the hospital to join the board. Applicants were interviewed, and representatives were selected for the board. The role of the board is to advise the hospital about the clinical procedures and research projects related to the treatment of obesity.
Overall Structure of the Study
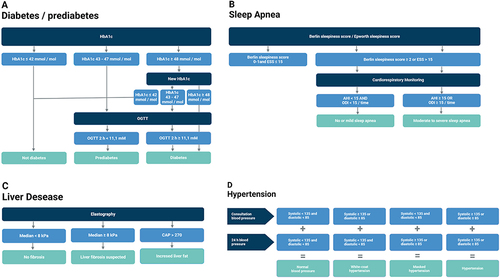
Through patient files, questionnaires, and interviews we achieved information about medical history including history of diabetes of any type, sleep apnea, MASLD and hypertension. We registered medical treatment according to the Anatomical Therapeutic Chemical Classification System. Further diagnostic procedures are described below and outlined in ).
Anthropometric Measures
Participants were weighed on a T7336 scale (ADE, Hamburg, Germany) in light clothes with no shoes or pocket items. Height was measured by a stadiometer. BMI was calculated as weight in kg divided by height in square meters. Waist circumference was measured at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest, while hip circumference was measured around the widest portion of the buttocks.Citation14
Blood Sampling
Blood samples were obtained by venipuncture after at least eight hours of fasting. Glycosylated hemoglobin (HbA1c), glucose, lipids, thrombocytes, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) were measured. People with HbA1c ≥48 mmol/mol were re-tested within two weeks. People with HbA1c >42 and <48 mmol/mol were subjected to an oral glucose tolerance test (OGTT) by ingestion of 75 g dissolved glucose within five minutes. At 120 minutes, venous blood was sampled for measurement of plasma glucose.
Diabetes was defined as HbA1c ≥48 mmol/mol at both measures or HbA1c >42 and ≤47 mmol/mol and a 120-minute OGTT value of glucose ≥11.1 mmol/l. Prediabetes was defined as HbA1c 42–47 mmol/mol with a subsequent normal OGTT. Impaired fasting glucose (IFG) was defined as fasting plasma glucose ≥6.1 mmol/l and HbA1c ≤47 mmol/mol. The metabolic syndrome was defined as a minimum of three of the following: Increased waist circumference (>88 cm for women and >102 cm for men), fasting triglycerides ≥1.7 mmol/l, HDL > 1.295 mmol/l for women and >1.036 mmol/l for men, and high blood pressure defined as office blood pressure >135 mmHg (systolic) or >85 mmHg (diastolic) or current treatment for hypertension ().
Respiratory Sleep Monitoring
We measured daytime sleepiness, the tendency to fall asleep during daytime, and patient-reported snoring by the Danish translations of the Berlin Questionnaire for sleep apneaCitation15 and the Epworth Sleepiness Scale.Citation16 Respiratory sleep monitoring was conducted by NOX T3 portable respiratory sleep monitor (Nox Medical, Reykjavík, Iceland) in participants who scored two or more on the Berlin sleep apnea score or more than fifteen on the Epworth sleepiness scale. People with known sleep apnea were not subjected to cardiorespiratory monitoring (CRM). The apnea/hypopnea index (AHI) and oxygen desaturation index (ODI) were registered. Mild sleep apnea was defined as an AHI of 5–14 events per hour, moderate sleep apnea as an AHI of 15–29 events per hour, and severe sleep apnea as an AHI ≥ 30 events per hour ().
Liver Elastography and Fibrosis Scores
Elastography of the liver was performed by skilled nurses using a Fibroscan Compact 530 (Echosens™, Waltham, MA, US) with XL probe for assessment of people with obesity. Increased liver stiffness was defined as a median liver stiffness value above 8 kPa, and increased fat in the liver was defined as controlled attenuation parameter (CAP) >270 dB/meter.
Fib-4 score is calculated as age × AST divided by platelet count × √ALT. A score of 1.45–2.67 indicates a moderate risk of fibrosis, while a score >2.67 indicates a high risk of fibrosis. The aspartate aminotransferase-to-platelet ratio index (APRI) is calculated as AST divided by the upper limit of normal for AST × 100 divided by platelet count. An APRI of 0.5–1.5 indicates a moderate risk of fibrosis, while a score >1.5 indicates a high risk of fibrosis ().
Blood Pressure
Participants underwent automated office blood pressure measurement by Connex Spot Monitor (Welch Allyn, Skaneateles Falls, NY, US). The device measured blood pressure three times with an interval of five minutes and the last measurement was registered. In addition, all participants underwent 24-hour blood pressure measurement by Cardio Perfect ABPM7100 (Welch Allyn, Skaneateles Falls, NY, US) using a cuff appropriate for the arm size of the individual. Whole-day average, daytime average, and nighttime average of systolic and diastolic blood pressure were noted. Hypertension was defined as blood pressure >135 (systolic) or >85 (diastolic) mmHg measured by office blood pressure only (white coat hypertension, WCH), 24-hour average mean blood pressure only (masked hypertension), or both (hypertension) ().
Statistics
Statistical analyses were conducted using either Excel or Stata® version 18 (StataCorp LLC, Texas, USA). An unpaired t-test was used to compare the age and BMI between women and men, as shown in . Data in regarding new and known diseases are presented as percentages of the total group of people living with obesity. In cases of missing data, measures were considered to fall within the normal range. The impact of sex, BMI, and age on the analyzed variables was assessed between groups using multivariate regression analysis, with sex (categorical), BMI (continuous), and age (continuous) as independent variables.
Table 1 Participants as Stratified by Sex, BMI and Age Group
Table 2 Diabetes, Pre-Diabetic Conditions, and Metabolic Syndrome
Table 3 Obstructive Sleep Apnea
Table 4 Increased Liver Fat or Liver Fibrosis
Table 5 Arterial Hypertension
Results
presents the number of participants in the different weight groups according to sex and age. Among the people with obesity, 73.0% were women. Female participants had a slightly lower mean age (42.2 years) compared to male participants (43.8 years) (p = 0.11), while BMI was equal between the two sexes (female: 41.6 years, male: 42.0 years (p = 0.4)). Participants were distributed across the BMI groups with a notable representation also in groups with the highest BMI. Thus, among females, 54.4% had a BMI exceeding 40 kg/m2, and 12.1% had a BMI above 50 kg/m2, while among male participants corresponding figures were 55.8% and 13.4%, respectively. The distribution of participants encompassed all age groups, but there was a preponderance of participants above 50 years of age.
Diabetes and Related Conditions ()
Among the participants in the cohort, 9.8% had a documented history of diabetes, including both type 1 diabetes and T2D. Subsequent to the screening procedure, an additional 4.2% of participants received a new diagnosis of diabetes, all of which were T2D as indicated by normal to high c-peptide. When considering both known and undiagnosed cases of diabetes, there was a significant impact of increasing BMI and age. Similarly, IFG was more prevalent among male participants. The presence of the metabolic syndrome was prevalent across all groups, with a higher prevalence observed among men. There was a significant positive association between the metabolic syndrome and increasing BMI; however, no significant association was found with higher age.
Obstructive Sleep Apnea ()
Among people living with obesity, 69.1% were subjected to CRM based on the results obtained from the two sleep apnea questionnaires, and 25.1% were diagnosed with moderate-to-severe sleep apnea. The prevalence of severe sleep apnea was higher among men (18.3%) than women (7.0%) and increased with both BMI and age. When we included those with a documented history of sleep apnea, more than half of the participants had a diagnosis of sleep apnea if their BMI was higher than 40 kg/m2 or their age was above 40 years.
Liver Disease ()
A Fib-4 score between 1.45 and 2.67 indicating a moderate risk of having liver fibrosis was found in 2.7% of women and 7.2% of men, while the number of participants with Fib-4 score >2.67 was low. Similarly, 2.5% and 6.7% in women and men, respectively, had an APRI score above 0.5 indicating moderate-to-high risk of liver fibrosis. A significant number of participants exhibited a diagnosis of elevated liver stiffness as assessed by fibroscan. Specifically, 12.3% of female participants and 31.3% of male participants had a medium resistance of 8 kPa or higher (women compared with men, p < 0.001). The proportion of people with elevated liver stiffness increased with higher BMI (p < 0.001) but not with age. Liver steatosis, identified by CAP >270, was prevalent, especially in men, and showed an increase with higher BMI and age. In the reference group, one participant was found to have increased liver stiffness as assessed by fibroscan.
Arterial Hypertension ()
Known hypertension, new hypertension, and masked hypertension were all frequent findings in the group of people living with obesity. Both new hypertension and total hypertension were more frequent among male participants (p < 0.001), and almost three of four male participants were diagnosed with hypertension. Total prevalence of hypertension as defined by either known hypertension, new hypertension, or masked hypertension increased both with increasing age and increasing BMI, while WCH was frequent (overall prevalence 10.8%) and increased with BMI. Also in the reference group, arterial hypertension was a relatively frequent finding.
Discussion
In the present paper, we report the initial findings of a prospective screening program targeted people with BMI 30 kg/m2 or higher. We found a large proportion of people with diabetes and related conditions, sleep apnea, liver disease, and arterial hypertension.
The occurrence of T2D is known to increase with higher BMI in both males and females.Citation17 Moreover, there tends to be an association between the degree of obesity and the prevalence of diabetes.Citation18 However, diabetes prevalence in the highest BMI classes is often not reported as the distribution of subjects does not allow accurate estimates in people with BMI above 45 or 50 kg/m2.Citation19 The high BMI in our cohort allows us to suggest estimates even in the highest BMI-groups. Among those without the diagnosis of diabetes, we found unexpectedly few new subjects with diabetes. Thus, the overall prevalence of new diabetes was 4.2%, which was also found in the group of people with a BMI above 50 kg/m2. As T2D increases markedly with age, this low number might be ascribed to the relatively young age of our study population, of which half of the subjects were below 40 years of age. The absence of subjects with diabetes and few subjects with pre-diabetes in the reference group indicate that a BMI of 30 kg/m2 is an appropriate threshold for testing.
Obstructive sleep apnea is a risk factor for cardiovascular disease in line with the presence of diabetes or a family history of cardiovascular disease, but the condition seems to remain undiagnosed in many cases.Citation20 This could be caused by the fact that the symptoms, in part, occur during sleep and that daytime symptoms, such as the tendency to fall asleep or tiredness during daytime, are considered normal occurrences. The Berlin score has a high sensitivity in the present population as one out of two points necessary to raise suspicion of sleep apnea was met by the referral criteria of a BMI > 30 kg/m2. Thus, among those without a previous diagnosis of sleep apnea, 69.2% were subjected to CRM, and in the total population of people living with obesity, 25.1% met the criteria of moderate-to-severe sleep apnea. The overall prevalence and the higher risk among men compared to women is in concordance with previous cohort studies.Citation21 Of notice is the fact that one of ten in the group of people living with obesity had unrecognized severe sleep apnea with more than 30 pauses of breathing per hour, thus clearly needing treatment for the condition. Six subjects of 161 in the reference groups were found to have sleep apnea among the 26 subjected to CRM, indicating that daytime sleepiness and sleep apnea are relatively rare in this population.
MASLD is very frequent among people living with obesity, and the development of liver fibrosis is a major determinant of the long-term clinical outcome. FIB-4 and APRI have been suggested to serve as accessible and cheap biochemical fibrosis screening methods, and both have a fairly good prognostic value.Citation22 Normal FIB-4 and APRI scores may rule out severe fibrosis. Fibroscan is, however, more accurate but also expensive, and is therefore used in secondary centers to determine fibrosis stage in those with elevated FIB-4 or APRI.Citation23 In our study, we performed a fibroscan on all participants independent of FIB-4 and APRI results. Both Fib-4 and APRI identified subjects with a moderate risk of having liver fibrosis, and the presence of fibrosis was further supported by the finding of increased liver stiffness by fibroscan in 17.4% of the population of people with obesity. These findings align with global estimates of MASLD around 25% in larger cohort studies.Citation24 As expected, we found the prevalence to be much higher among men than women, with a positive correlation to both BMI and age. Notably, we found only one participant with increased median liver stiffness among the reference population. As obesity is now the leading cause of MASLD, our data support the use of fibroscan in the algorithm of fibrosis detection in obesity.
All participants underwent both office blood pressure by three consecutive measurements and 24-hour blood pressure monitoring. This was done as the literature indicates that approximately one-third of persons with normal blood pressure exhibit high blood pressure using out-of-office measures.Citation25 In addition, masked hypertension, defined as normal office blood pressure and high blood pressure by either home blood pressure or 24-hour blood pressure monitoring, seems to be a stronger risk factor for cardiovascular disease than office blood pressure.Citation26,Citation27 We found that 49.2% of the participants complied with the diagnosis of hypertension. This is similar to the findings in the NHANES cohort, where 42.5% of people with BMI > 30kg/m2 compared with 27.8% of individuals with BMI 25.0–29.9 kg m2 and 15.3% for those with BMI below 25 had hypertension.Citation28 In our population, 4.7% had masked hypertension, and 14.3% had hypertension without a previously established diagnosis of hypertension. Another important finding is the large percentage of people with WCH. While the total prevalence of hypertension was associated with both higher BMI and age, WCH showed a slight association with BMI only. WCH does not appear to be an independent risk factor for cardiovascular disease, and accordingly, it is of utmost importance to establish a correct diagnosis before initiating life-long antihypertensive treatment.Citation29 When it comes to WCH, specific focus should be put on the group of people living with the most severe degree of obesity, as 12.5% of those with a BMI above 50 kg/m2 exhibited WCH.
Our study has several strengths. First, we included people with BMI ≥30 kg/m2 and age between 18 and 60 years. These broad inclusion criteria make it conceivable to generalize our results to the general population of people living with obesity. Secondly, our cohort was well distributed across all obesity classes, which allows us to estimate the prevalence of obesity-related disease also in people with a BMI above 45 kg/m2 and 50 kg/m2 respectively and in addition we included a reference group of people with normal weight or overweight. Finally, state-of-the-art methods, including CRM, 24-hour blood pressure monitoring and fibroscan, were used in our algorithms to uncover obesity-related diseases.
The study also has limitations. We did not include people above the age of 60 years. Our rationale is that obesity-related disease exerts less impact if diagnosed later in life. For instance, the late onset phenotype of T2D associates with milder metabolic derangements.Citation30 Likewise, the number of lost life years due to obesity is lower in people over 60 years of age.Citation6 Although all people with BMI above 30 kg/m2 within the defined age limit can be referred to the screening program, the referred population did not mirror the background population of people living with obesity. As seen in most cohorts of bariatric surgery, women seek treatment more frequently than do men, and often women comprise more than two-thirds of a cohort in bariatric surgery.Citation31 It is evident that men tend to underestimate their weight, exhibit lower concern regarding weight-related issues, and engage less in weight loss efforts compared to women.Citation32 All of these factors may contribute to the observed lower male representation which results in a risk of bias. People who experience weight-related adverse health effects may feel more inclined to ask for a referral, which may lead to an overestimation of disease frequency. On the other hand, incidents of missing data were considered normal which will tend to underestimate the frequencies of diseases.
The lower BMI-limit of 30 kg/m2 in our study was chosen arbitrarily based on the established obesity classification. To assess the impact of obesity per se, we also established a reference group of people with BMI 18.5 to 30 kg/m2. The limited size of the reference group does not allow us to make solid conclusions, but apparently diabetes and related conditions, sleep apnea, and increased liver stiffness rarely occur in this group. Arterial hypertension, on the other hand, was relatively frequent also in the reference group, pinpointing that this condition is not solely a condition seen in people with obesity.
Screening programs should only be carried out when appropriate treatment is available to cure or to change the prognosis of the disease.Citation33 This prerequisite is met for diabetes, sleep apnea and arterial hypertension. When it comes to MASLD, this is more complex. Weight loss is an effective treatment option but is difficult to maintain, and currently we have no medical treatment for MASLD. It is uncertain whether individuals get more motivated to make lifestyle changes upon receiving a diagnosis. In men, the fear of disease appears to serve as a motivating factor (35), but the long-term effects of this remain unresolved and are likely to vary from person to person.
Conclusion
We found that obesity is associated with the occurrence of a plethora of diseases, of which many remain undiagnosed. Both male sex, the degree of obesity and higher age are important risk factors of disease. A BMI threshold of 30 kg/m2 seemed appropriate for the screening program with the exception of the occurrence of hypertension. The underrepresentation of male subjects is worrying and should be a focus when establishing screening programs for obesity-related diseases.
Abbreviations
T2D, type 2 diabetes; MASLD, metabolic dysfunction-associated steatotic liver disease; SDOI, South Danish Obesity Initiative; Hb1c, glycosylated hemoglobin or hemoglobin a1c; ALT, alanine aminotransferase; AST, aspartate aminotransferase; OGTT, Oral glucose tolerance test; IFG, Impaired fasting glucose; WCH, White coat hypertension; CRM, Cardiorespiratory monitoring; AHI, apnea-hypopnea index; ODI, Oxygen desaturation index.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The Hospital Management of University Hospital of Southern Denmark, Esbjerg, Denmark, is thanked for extensive support. The staff of SDOI (Birgitte Nielsen, Pia Hansen, Hanne Slemmings, Trine Ekblad and Martin Skriver Nicolaisen) are thanked for their dedicated attitude to the initiative.
Data Sharing Statement
De-identified individual participant data can be provided upon specific request to corresponding author (CBJ) and subsequent application and approval from the relevant authority. This will be available for five years from the day of publication.
References
- World Health Organization. Obesity Update 2017. World Health Organization; 2017.
- Danskernes Sundhed. Den Nationale Sundhedsprofil 2017; 2018. Available from: https://www.sst.dk. Accessed June 14, 2024.
- Mainous AG, Tanner RJ, Jo A, Anton SD. Prevalence of prediabetes and abdominal obesity among healthy-weight adults: 18-year trend. Ann Fam Med. 2016;14(4):304–310. doi:10.1370/afm.1946
- George ES, Roberts SK, Nicoll AJ, et al. Non-alcoholic fatty liver disease patients attending two metropolitan hospitals in Melbourne, Australia: high risk status and low prevalence. Intern Med J. 2018;48(11):1369–1376. doi:10.1111/imj.13973
- Luque-Ramirez M, Marti D, Fernandez-Duran E, Alpanes M, Alvarez-Blasco F, Escobar-Morreale HF. Office blood pressure, ambulatory blood pressure monitoring, and echocardiographic abnormalities in women with polycystic ovary syndrome: role of obesity and androgen excess. Hypertension. 2014;63(3):624–629. doi:10.1161/HYPERTENSIONAHA.113.02468
- Finkelstein EA, Brown DS, Wrage LA, Allaire BT, Hoerger TJ. Individual and aggregate years-of-life-lost associated with overweight and obesity. Obesity. 2010;18(2):333–339. doi:10.1038/oby.2009.253
- Hernaes UJ, Andersen JR, Norheim OF, Vage V. Work participation among the morbidly obese seeking bariatric surgery: an exploratory study from Norway. Obes Surg. 2015;25(2):271–278. doi:10.1007/s11695-014-1333-8
- Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7(5):273–289. doi:10.1111/cob.12203
- Heltberg A, Andersen JS, Sandholdt H, Siersma V, Kragstrup J, Ellervik C. Predictors of undiagnosed prevalent type 2 diabetes - the Danish general suburban population study. Prim Care Diabetes. 2018;12(1):13–22. doi:10.1016/j.pcd.2017.08.005
- Peromaa-Haavisto P, Tuomilehto H, Kossi J, et al. Prevalence of obstructive sleep apnoea among patients admitted for bariatric surgery. a prospective multicentre trial. Obes Surg. 2016;26(7):1384–1390. doi:10.1007/s11695-015-1953-7
- Spurr S, Bally J, Hill P, Gray K, Newman P, Hutton A. Exploring the prevalence of undiagnosed prediabetes, type 2 diabetes mellitus, and risk factors in adolescents: a systematic review. J Pediatr Nurs. 2020;50:94–104. doi:10.1016/j.pedn.2019.09.025
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology. 2018;67(1):328–357. doi:10.1002/hep.29367
- Laiteerapong N, Ham SA, Gao Y, et al. The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (The Diabetes & Aging Study). Diabetes Care. 2019;42(3):416–426. doi:10.2337/dc17-1144
- Consultation WE. Waist circumference and waist-hip ratio report of a WHO expert consultation; 2008.
- Lauritzen E, Korvel-Hanquist A, Homoe P. The Danish translation and validation of the Berlin Questionnaire for sleep apnoea. Dan Med J. 2018;65(9):1.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
- Hauguel-Moreau M, Hergault H, Cazabat L, et al. Prevalence of prediabetes and undiagnosed diabetes in a large urban middle-aged population: the CARVAR 92 cohort. Cardiovasc Diabetol. 2023;22(1):31. doi:10.1186/s12933-023-01761-3
- Kuwabara M, Kuwabara R, Niwa K, et al. Different risk for hypertension, diabetes, dyslipidemia, and hyperuricemia according to level of body mass index in Japanese and American Subjects. Nutrients. 2018;10(8):1011. doi:10.3390/nu10081011
- Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497. doi:10.1136/bmj.k1497
- Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;144(3):e56–e67. doi:10.1161/CIR.0000000000000988
- Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002
- Lee J, Vali Y, Boursier J, et al. Prognostic accuracy of FIB-4, NAFLD fibrosis score and APRI for NAFLD-related events: a systematic review. Liver Int. 2021;41(2):261–270. doi:10.1111/liv.14669
- Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J Hepatol. 2018;68(2):305–315. doi:10.1016/j.jhep.2017.11.013
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi:10.1002/hep.28431
- Thakkar HV, Pope A, Anpalahan M. Masked Hypertension: a Systematic Review. Heart Lung Circ. 2020;29(1):102–111. doi:10.1016/j.hlc.2019.08.006
- Asayama K, Stolarz-Skrzypek K, Yang WY, et al. What did we learn from the International databases on ambulatory and home blood pressure in relation to cardiovascular outcome? Hypertens Res. 2023;46(4):934–949. doi:10.1038/s41440-023-01191-4
- Staplin N, de la Sierra A, Ruilope LM, et al. Relationship between clinic and ambulatory blood pressure and mortality: an observational cohort study in 59 124 patients. Lancet. 2023;401(10393):2041–2050. doi:10.1016/S0140-6736(23)00733-X
- Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164(19):2126–2134. doi:10.1001/archinte.164.19.2126
- Kario K, Thijs L, Staessen JA. Blood Pressure Measurement and Treatment Decisions. Circ Res. 2019;124(7):990–1008. doi:10.1161/CIRCRESAHA.118.313219
- Ahlqvist E, Storm P, Karajamaki A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6(5):361–369. doi:10.1016/S2213-8587(18)30051-2
- Tang B, Zhang Y, Wang Y, Wang X, An Z, Yu X. Effect of bariatric surgery on long-term cardiovascular outcomes: a systematic review and meta-analysis of population-based cohort studies. Surg Obes Relat Dis. 2022;18(8):1074–1086. doi:10.1016/j.soard.2022.05.007
- Tsai SA, Lv N, Xiao L, Ma J. Gender differences in weight-related attitudes and behaviors among overweight and obese adults in the United States. Am J Mens Health. 2016;10(5):389–398. doi:10.1177/1557988314567223
- World Health Organization. Screening Programmes: A Short Guide. Increase Effectiveness, Maximize Benefits and Minimize Harm. World Health Organization; 2020.