Abstract
Background
The triglyceride–glucose index (TyG) is a reliable indicator for predicting the prognosis of patients with coronary heart disease (CAD) after percutaneous coronary intervention (PCI). However, its influence on patients with in-stent restenosis (ISR) is unclear. This study was designed to evaluate the association between the TyG index and the occurrence of major adverse cardiovascular events (MACEs) after PCI in patients with ISR.
Methods
This retrospective study included 1654 patients who underwent PCI between 2016 and 2022 at Nanjing First Hospital. Patients were stratified into three groups based on the quantile level of the TyG index. The TyG index was determined as Ln (triglycerides [mg/dL] × fasting plasma glucose [mg/dL]/2).
Results
Individuals with the highest TyG index showed an increased risk of MACEs compared to those with the lowest level of the TyG index (HR 1.60; 95% CI 1.11–2.30; P = 0.01). When analyzing the TyG index as a continuous variable, each standard deviation increase was associated with an HR of 1.51 (95% CI: 1.11–2.05; P = 0.01). For the male subgroup and the diabetes subgroup, this trend was even more pronounced (HR 1.269; 95% CI 1.055–1.527; P = 0.011; HR 1.385; 95% CI 1.125–1.706; P = 0.002). Additionally, the landmark analysis showed that patients with the highest level of TyG had an increased risk of MACEs 6 months after the PCI (P = 0.019).
Conclusion
Elevated TyG index is associated with increased risk of adverse cardiovascular events in patients with ISR, and the extent of increase in the risk is more significant in male patients with diabetes.
Introduction
Percutaneous coronary intervention (PCI) is a prevalent therapeutic approach for coronary artery disease (CAD) and has been used extensively worldwide.Citation1 Stent implantation, a major treatment method, is performed to support narrow arteries, restoring blood flow and subsequently improving physiological function.Citation2 As a common stent failure event,Citation3 although the incidence of in-stent restenosis (ISR) has decreased with the advent of new-generation drug-eluting stents (DES), the occurrence of in-stent restenosis (ISR) and the need for target lesion revascularization (TLR) after PCI still increases with an annual growth rate of 1% to 2%.Citation4 Additionally, the probability of restenosis exceeds that of primary lesions, reaching up to 30%, particularly in patients without a clear etiology.Citation5–7 Identifying factors that increase the risk of major cardiovascular adverse events (MACEs) in patients with ISR is crucial for risk classification and future management of health.
Previous studies have shown that irrespective of BMI, IR elevates the risk of cardiovascular adverse events.Citation8,Citation9 Traditional methods for assessing IR, such as the hypoglycemic-hyperinsulinemic clamp test, although is widely regarded as the gold standard, is cumbersome and expensive. For several decades, the triglyceride-glucose (TyG) index has been recognized as a reliable and cost-effective alternative for diagnosing IR.Citation10 Zhu et al reported that elevated TyG index was associated with increased risk of adverse cardiovascular events in patients with primary coronary lesions.Citation11 This study aims to assess the potential prognostic value of TyG index in post-PCI patients who are diagnosed with ISR.
Methods
Study Population
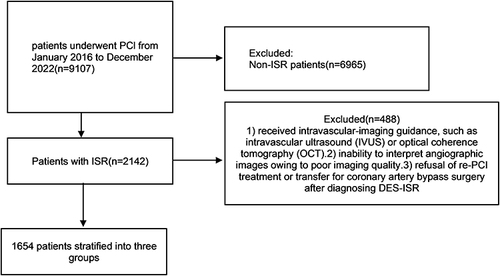
This study retrospectively included post-PCI patients who were diagnosed with DES-ISR at Nanjing First Hospital between January 2016 and December 2022. The exclusion criteria for patients were as follows: 1) received intravascular-imaging guidance, such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT). 2) inability to interpret angiographic images owing to poor imaging quality. 3) refusal of re-PCI treatment or transfer for coronary artery bypass surgery after diagnosing DES-ISR.
Patients were stratified into three groups based on the tertile of the TyG index (Lowest/Median/Highest): T1 (<8.50), T2 (8.50 ≤ TyG index <9.01), and T3 (≥9.01).
Following local standards of diagnosis and treatment, the patients received standardized care and clinical health management during and post-re-PCI.Citation12 Additionally, they were provided with medication and lifestyle guidance upon discharge. Patients were treated with dual antiplatelet therapy (DAPT) including aspirin 100 mg/d + clopidogrel 75 mg/d or ticagrelor 90 mg bid and switched to aspirin single antiplatelet therapy 12 months post-PCI. All participants provided informed consent, either in written or oral form. The detailed process for the inclusion and exclusion of patients is illustrated in .
Data Collection and Definition
The data were collected from the electronic health systems from databases at Nanjing First Hospital during hospitalization, including age, sex, body mass index (BMI), disease history, laboratory test results, angiography characteristics, and discharge medication. The TyG index was determined as Ln (triglycerides [mg/dL] × fasting plasma glucose [mg/dL]/2).Citation10 Diabetes was defined as a history of diagnosed diabetes mellitus, receiving hypoglycemic drugs, or presenting typical symptoms of diabetes with the level of fasting plasma glucose (FBG)>7 mmol/L or an HbA1c≥6.5% (ie meeting any one of these criteria).Citation11 In-stent restenosis (ISR) was defined as the presence of significant diameter stenosis (≥50%) at the segment inside the stent or involving its 5-mm edges, which is consistent with previous studies.Citation13
Endpoint Definition and Follow-Up
The primary endpoint of this study was a composite of major cardiovascular adverse events (MACEs), including all-cause death, myocardial infarction (MI), TLR/TVR (target lesion/vessel revascularization), stroke, and heart failure (HF). Patients received regular follow-up by letters, phone or re-hospitalization at 3–6 month intervals. This work is conducted using an independent follow-up term consisting of well-trained researchers who were ignorant of the aim of this research.
Statistical Analysis
Continuous variables with a normal distribution were calculated using the mean ± standard deviation, others were calculated using the median and interquartile range (IQR). Subtype variables are presented as numerical values accompanied by corresponding percentages (%). The chi-square test was used to compare subtype variables, ANOVA was used to analyze normally distributed continuous variables, and the Kruskal‒Wallis test was used for skewed continuous variables. Kaplan–Meier survival analysis and long-rank tests were performed for patients with different levels of the TyG index.
Additionally, Cox regression analysis was used to estimate the hazard ratio (HR) and 95% confidence interval (CI) of the TyG index at the risk of MACEs. In the final adjusted model, age, BMI, LDL-C, TG, Lp(a), gender, smoking, STEMI, hypertension, β-block, ACEI/ARB were included. All the statistical analyses were performed using R (software version 4.3.1), with P value <0.05 considered to indicate statistical significance.
Results
Baseline Characteristics
The study included a total of 1654 patients diagnosed with ISR. Based on the tertile of the TyG index, the patients were further divided into three groups (). The mean age of the individuals was 66.74±10.44 years, and 1261 (76.24%) patients were male. The occurrence of hypertension, diabetes, and smoking were 72.61%, 41.66%, and 27.09%. The incidence of all conditions, except smoking, significantly increased with increasing TyG index. Patients with the highest level of TyG index were significantly younger (P = 0.004), and had hypertension and diabetes more regularly (P all <0.001). Furthermore, the distribution of target lesion vessels and treatment strategies were comparable among individuals with different levels of TyG index. Detailed information on baseline characteristics was described in .
Table 1 Baseline Characteristics of Patients with ISR
The Association Between the TyG Index and the Occurrence of Major Cardiovascular Adverse Events After PCI
Cox regression analysis was used to explore the relationship between the TyG index and post-PCI MACEs (). According to the unadjusted model, Individuals with the highest level of TyG index had an increased risk of MACEs compared to others (HR = 1.30; 95% CI: 1.02–1.67; P = 0.03). Additionally, consistent results were observed when the TyG index was analyzed as a continuous variable (HR = 1.18; 95% CI: 1.01–1.38; P = 0.03). When analyzing the TyG index as a continuous variable, each standard deviation increase was associated with an HR of 1.51 (95% CI: 1.11–2.05; P = 0.01).
Table 2 The Association Between the TyG Index and the Occurrence of Major Cardiovascular Adverse Events (MACEs) After PCI
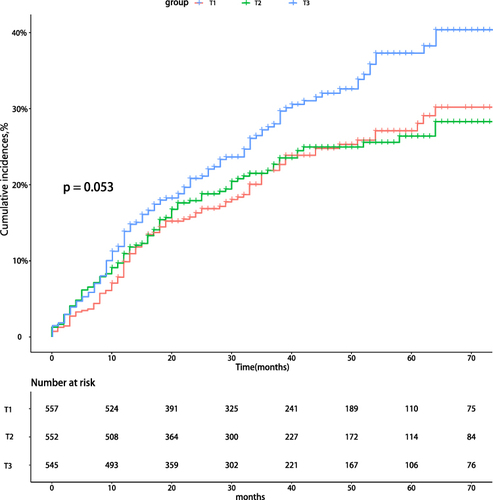
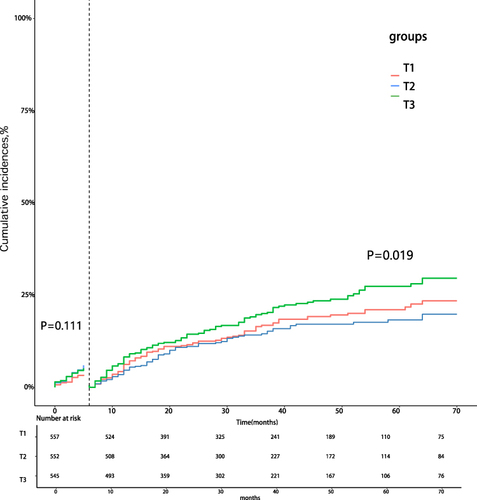
Among patients with different levels of the TyG index, there was a marginally significant discrepancy in the risk of MACEs (P = 0.053) (). The further landmark analysis revealed that individuals with elevated levels of TyG index had a significantly increased risk of MACEs starting from 6 months after PCI (P = 0.019) ().
Subgroup Analysis
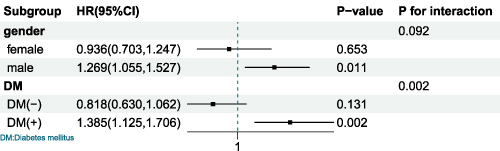
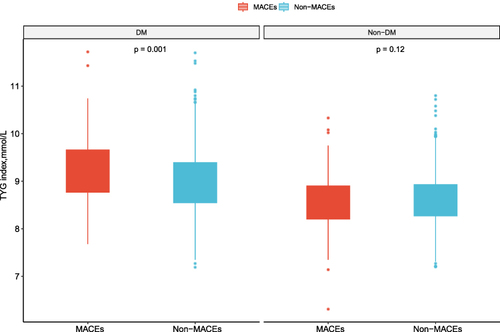
In subgroup analysis, the associations between the risk of experiencing MACEs and the TyG index were evaluated (). The results indicated that the TyG index was significantly associated with the risk of post-PCI MACEs in male (HR 1.269; 95% CI 1.055–1.527; P = 0.011) and diabetic patients (HR 1.385; 95% CI 1.125–1.706; P = 0.002). As depicted in , among individuals with diabetes, the MACEs group had a significantly higher TyG index than the non-MACEs group (P = 0.001).
Discussion
This study first analyzed the association between the TyG index and the risk of post-PCI MACEs in patients diagnosed with ISR. We found elevated TyG index is associated with increased risk of major adverse cardiovascular events in patients with ISR, and the extent of increase in the risk is more significant in male patients with diabetes.
Previous study based on primary coronary artery disease (CAD) by Zhu et al investigated the association between the TyG index and the incidence of ISR in patients underwent PCI.Citation10,Citation11 Our previous study revealed that elevated TyG index may lead to coronary revealed a significant correlation between the TyG index and the risk of MACEs. Thus, it is noted that the TyG index impacts the occurrence, development and prognosis of ISR.
Insulin resistance and disturbances in glucose metabolism led to oxidative stress, inflammation, and dysfunctional immune modulation and then exacerbates the development of arteriosclerosis and promotes the formation of plaques.Citation14–17 As a common stent failure event, ISR may be triggered by inflammation, which is induced by insulin resistance and following disturbances in glucose metabolism. In the context of atherosclerosis, the mitogen-activated protein kinase signaling pathway can facilitate its development, and IR is known to activate this pathway. It is also implicated in causing endothelial dysfunction and excessive proliferation of vascular smooth muscle cells,Citation18–20 accelerating the generation of neointimal hyperplasia (NIH), which serves as a restenosis substrate within the stent. Additionally, in patients with ISR, IR-induced impaired endothelial function may trigger neotenic atherosclerosis, leading to plaque rupture and impaired blood flow dynamics.Citation18–21 Previous study revealed that elevated TyG index may lead to coronary slow flow, and this abnormal blood flow dynamic may worsen the prognosis.Citation21
ISR ranks among the most common long-term complications following stent implantation. The prognosis varied among different pathological patterns and tissue characteristics.Citation22 For example, diffuse ISR tends to result in the occurrence of earlier and more severe MACEs.Citation23 Furthermore, studies have shown a correlation between the adverse prognosis of ISR and various metabolic factors and metabolic disorders.Citation24 Patients with this etiology have an increased risk of experiencing MACEs or greater disease severity than patients with the primary disease.Citation25 Considering that, we thought future research should analysis the potential association between the TyG index and dynamic morphologies and component changes in atherosclerosis to clarify the predictive value of the TyG index profoundly by intravascular imaging (OCT&IVUS).
Subgroup analysis indicated that the extent of increase in the risk of MACEs is more significant in male patients with diabetes, which is consistent with previous study.Citation26–28 Conversely, Wu et al found that the TyG index was an independent predictor of MACEs for non-diabetic patients who underwent coronary artery bypass grafting (CABG) and significantly enhanced the accuracy of existing risk-predictive model.Citation29 As a physiological response to acute syndrome, there may be an abnormal elevation of blood glucose level owing to the existence of stress-induced hyperglycemia (SIH) and the level of TyG may be influenced.Citation30–32 Confounding factors such as SIH may influence the predictive ability of the TyG index, and relevant study which combined the elimination of collinear factors with following subgroup analysis based on diabetes was absent.
Previous research has identified that integrating the TyG index into the GRACE risk score could improve the prognostic predictive capability for patients who underwent PCI (18, 30). Although further research was needed, we thought our research clarified the predictive value of the TyG index and provided useful information for the management of prognosis in patients diagnosed with ISR.
Strengths and Limitations of the Study
The strength of this study lies in the inclusion of a sufficiently large sample population, specifically for in-stent restenosis. However, there were still some limitations. Firstly, it was a single-center retrospective study therefore could not determine the causality between the TyG index and DES-IS. Secondly, limited information was available about the changes in patients’ TyG index levels among the duration of follow-up, suggesting that future research is needed to explore the utility of dynamic monitoring of the TyG index or cumulative TyG index.
Conclusion
Elevated TyG index is associated with increased risk of adverse cardiovascular events in patients with ISR, and the extent of increase in the risk is more significant in male patients with diabetes.
Ethics Approval and Consent to Participate
The Ethics Review Committee of Nanjing First Hospital approved this study. As a retrospective study, follow-up was conducted through telephone, letters or rehospitalization, with verbal consent from the ethics committee.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
Yi-fei Wang and Xiao-han Kong are co-first authors for this study. Huimin Tao and Li Tao shared a second authorship. This paper has been updated to a preprint server as a preprint. Link: https://www.researchgate.net/publication/377642728).
Data Sharing Statement
Applicants could apply by visiting the official website of the hospital and accessing relevant data after approval by the committee.
Additional information
Funding
References
- Giustino G, Colombo A, Camaj A, et al.. Coronary in-stent restenosis: JACC State-of-The-Art Review. J Am Coll Cardiol. 2022;80(4):348–372. doi:10.1016/j.jacc.2022.05.017
- Collet JP, Thiele H, Barbato E, et al. ESC Scientific Document Group. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289–1367.
- Byrne RA, Joner M, Kastrati A. Stent thrombosis and restenosis: what have we learned and where are we going? The Andreas gruentzig lecture ESC 2014. Eur Heart J. 2015;36(47):3320–3331. doi:10.1093/eurheartj/ehv511
- Madhavan MV, Kirtane AJ, Redfors B, et al. Stent-related adverse events >1 year after percutaneous coronary intervention. J Am Coll Cardiol. 2020;75(6):590–604. doi:10.1016/j.jacc.2019.11.058
- Goto K, Zhao Z, Matsumura M, et al. Mechanisms and patterns of intravascular ultrasound in-stent restenosis among bare metal stents and first- and second-generation drug-eluting stents. Am J Cardiol. 2015;116(9):1351–1357. doi:10.1016/j.amjcard.2015.07.058
- Park SJ, Kim KH, Oh IY, et al. Comparison of plain balloon and cutting balloon angioplasty for the treatment of restenosis with drug-eluting stents vs bare metal stents. Circ J. 2010;74(9):1837–1845. doi:10.1253/circj.CJ-09-1041
- Iqbal J, Serruys PW, Silber S, et al. Comparison of zotarolimus- and everolimus-eluting coronary stents: final 5-year report of the RESOLUTE all-comers trial. Circ Cardiovasc Interv. 2015;8(6):e002230. doi:10.1161/CIRCINTERVENTIONS.114.002230
- Nathan DM. Clinical practice. Initial management of glycemia in type 2 diabetes mellitus. N Engl J Med. 2002;347(17):1342–1349. doi:10.1056/NEJMcp021106
- Adeva-Andany MM, Martínez-Rodríguez J, González-Lucán M, Fernández-Fernández C, Castro-Quintela E. Insulin resistance is a cardiovascular risk factor in humans. Diabetes Metab Syndr. 2019;13(2):1449–1455. doi:10.1016/j.dsx.2019.02.023
- Zhu Y, Liu K, Chen M, et al.. Triglyceride-glucose index is associated with in-stent restenosis in patients with acute coronary syndrome after percutaneous coronary intervention with drug-eluting stents. Cardiovasc Diabetol. 2021;20(1):137. doi:10.1186/s12933-021-01332-4
- Guo X, Shen R, Yan S, Su Y, Ma L. Triglyceride-glucose index for predicting repeat revascularization and in-stent restenosis in patients with chronic coronary syndrome undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2023;22(1):43. doi:10.1186/s12933-023-01779-7
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/ EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. doi:10.1093/eurheartj/ehy394
- Nusca A, Viscusi MM, Piccirillo F, et al. In stent neo-atherosclerosis: pathophysiology, clinical implications, prevention, and therapeutic approaches. Life. 2022;12(3):393. doi:10.3390/life12030393
- Brito ADM, Hermsdorff HHM, Filgueiras MS, et al.. Predictive capacity of triglyceride glucose (TyG) index for insulin resistance and cardiometabolic risk in children and adolescents: a systematic review. Crit Rev Food Sci Nutr. 2021;61(16):2783–2792. doi:10.1080/10408398.2020.1788501
- Laakso M, Kuusisto J. Insulin resistance and hyperglycemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10(5):293–302. doi:10.1038/nrendo.2014.29
- Zhou Y, Wang C, Che H, et al. Correction to: association between the triglyceride-glucose index and the risk of mortality among patients with chronic heart failure: results from a retrospective cohort study in China. Cardiovasc Diabetol.2023;22(1):171
- Bonora E, Kiechl S, Willeit J, et al. Insulin resistance as estimated by homeostasis model assessment predicts incident symptomatic cardiovascular disease in caucasian subjects from the general population: the bruneck study. Diabetes Care. 2007;30:318–324. doi:10.2337/dc06-0919
- Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010;56(23):1897–1907. doi:10.1016/j.jacc.2010.07.028
- Kitta Y, Nakamura T, Kodama Y, et al. Endothelial vasomotor dysfunction in the brachial artery is associated with late in-stent coronary restenosis. J Am Coll Cardiol. 2005;46(4):648–655.
- Kurmuş Ferik Ö, Yetiş Sayın B, Akbuğa K, Zorlu Ç. Association between insulin resistance estimated by Triglyceride Glucose Index and In-stent restenosis in non-diabetic patients. EJCM. 2022;10(1):12–17. doi:10.32596/ejcm.galenos.2022.2021-11-060
- Kaplangoray M, Toprak K, Başanalan F, et al.. Investigation of the relationship between triglycerides-glucose index and coronary slow flow: a retrospective case-control study. Arq Bras Cardiol. 2023;120(6):e20220679. doi:10.36660/abc.20220679
- Otsuka F, Byrne RA, Yahagi K, et al. Neoatherosclerosis: overview of histopathologic findings and implications for intravascular imaging assessment. Eur Heart J. 2015;36(32):2147–2159. doi:10.1093/eurheartj/ehv205
- Rathore S, Kinoshita Y, Terashima M, et al. A comparison of clinical presentations, angio-graphic patterns and outcomes of in-stent restenosis between bare metal stents and drug eluting stents. Euro Intervent. 2010;5(7):841–846. doi:10.4244/eijv5i7a141
- Nakano H, Kataoka Y, Otsuka F, et al. Refractory In-stent restenosis attributable to eruptive calcified nodule. J Am Coll Cardiol Case Rep. 2020;2(12):1872–1878.
- Assali AR, Moustapha A, Sdringola S, et al. Acute coronary syndrome may occur with in-stent restenosis and is associated with adverse outcomes (the PRESTO trial). Am J Cardiol. 2006;98(6):729–733. doi:10.1016/j.amjcard.2006.04.007
- Yang J, Tang YD, Zheng Y, et al.. The impact of the Triglyceride-Glucose Index on poor prognosis in nondiabetic patients undergoing percutaneous coronary intervention. Front Endocrinol. 2021;12:710240. doi:10.3389/fendo.2021.710240
- Chen L, Ding XH, Fan KJ, et al. Association between Triglyceride-Glucose Index and 2-year adverse cardiovascular and cerebrovascular events in patients with type 2 diabetes mellitus who underwent off-pump coronary artery bypass grafting. Diabetes Metab Syndr Obes. 2022;15:439–450. doi:10.2147/DMSO.S343374
- Qin Z, Xu S, Yuan R, et al.. Combination of tyg index and grace risk score as long-term prognostic marker in patients with acs complicated with t2dm undergoing PCI. Diabetes Metab Syndr Obes. 2022;15:3015–3025. doi:10.2147/DMSO.S376178
- Wu Z, Xie L, Guo D, et al.. Triglyceride-glucose index in the prediction of adverse cardiovascular events in patients without diabetes mellitus after coronary artery bypass grafting: a multicenter retrospective cohort study. Cardiovasc Diabetol. 2023;22(1):230. doi:10.1186/s12933-023-01969-3
- Zhao Q, Zhang TY, Cheng YJ, et al. Triglyceride-Glucose Index as a surrogate marker of insulin resistance for predicting cardiovascular outcomes in nondiabetic patients with non-st-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. J Atheroscler Thromb. 2021;28(11):1175–1194. doi:10.5551/jat.59840
- Al Jumaily T, Rose’Meyer RB, Sweeny A, Jayasinghe R. Cardiac damage associated with stress hyperglycaemia and acute coronary syndrome changes according to level of presenting blood glucose. Int J Cardiol. 2015;196:16–21. doi:10.1016/j.ijcard.2015.05.143
- Alizargar J, Bai CH, Hsieh NC, Wu SV. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol. 2020;19(1):8. doi:10.1186/s12933-019-0982-2