Abstract
In type 2 diabetes (T2D), early combination therapy using agents that target a number of the underlying pathophysiologic defects contributing to hyperglycemia may improve patient outcomes. For many patients, the combination of metformin with a sodium–glucose cotransporter-2 (SGLT-2) inhibitor may be a good option because these agents have complementary mechanisms of action, neutral-to-positive effects on body weight, and a low risk of hypoglycemia. This review focuses on the combination of metformin with dapagliflozin, a member of the SGLT-2 inhibitor class of antidiabetes agents. In clinical trials, the combination of dapagliflozin with metformin produced significant and sustained reductions in glycated hemoglobin and body weight in a broad range of adult patients with T2D, including those initiating pharmacotherapy and those with more advanced disease. These reductions were accompanied by modest decreases in blood pressure. Dapagliflozin as add-on therapy to metformin was well tolerated and associated with low rates of hypoglycemia. Genital infections and, in some studies, urinary tract infections were more frequent with dapagliflozin than with placebo. Early combination therapy with dapagliflozin and metformin may be a safe and appropriate treatment option that enables patients with T2D to achieve individualized glycemic goals as either initial combination therapy in treatment-naïve patients or as dapagliflozin add-on in patients inadequately controlled with metformin therapy.
Introduction
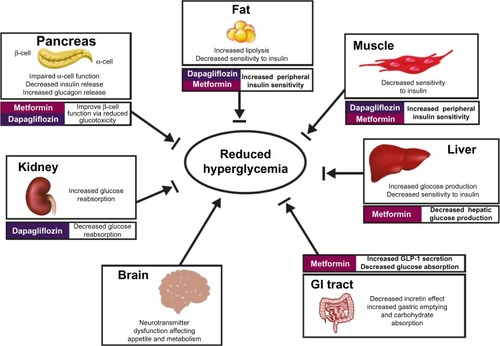
The prevalence of diabetes is rapidly increasing coincident with the obesity epidemic.Citation1 In 2014, the global prevalence of diabetes was estimated at 387 million people, mostly with type 2 diabetes (T2D), and this is expected to rise to 592 million by 2035.Citation2 In healthy individuals, numerous organs, hormones, and neurotransmitters work in concert via complex feedback mechanisms to tightly control plasma glucose concentrations.Citation3 The pathophysiology of T2D involves dysfunction at multiple levels of this complex systemCitation3,Citation4 (), and β-cell dysfunction and insulin resistance are major contributors to the development and progression of T2D.Citation5
Figure 1 Mechanisms involved in hyperglycemia in T2D and site of action of metformin and dapagliflozin.
Abbreviations: GI, gastrointestinal; GLP-1, glucagon-like peptide-1; T2D, type 2 diabetes.
The progressive nature of T2D, its complex pathophysiology, and the frequent presence of multiple comorbiditiesCitation6 make management challenging. Although lifestyle changes (ie, diet and exercise) can improve glycemic control and cardiovascular (CV) risk factors in T2D,Citation7 most patients do not adhere to such changes over the long term and subsequently require pharmacotherapy to achieve glycemic goals.Citation8 Furthermore, despite a wide range of available treatment options, only ~50% of patients with diabetes in the United States have glycated hemoglobin (A1C) <7%.Citation9,Citation10
Chronic uncontrolled hyperglycemia increases the risk of microvascular complications (nephropathy, retinopathy, and neuropathy), macrovascular complications (CV disease), and mortality.Citation11–Citation13 Data from the Diabetes Control and Complications Trial (DCCT)Citation14 and its long-term follow-up study, Epidemiology of Diabetes Interventions and Complications (EDIC)Citation15 in patients with type 1 diabetes, and from the UK Prospective Diabetes Study (UKPDS)Citation16,Citation17 in patients with T2D suggest that intensive glycemic control, particularly when achieved early in the disease course, can reduce the risk of microvascular and, to a lesser extent, macrovascular complications and mortality. In the Steno-2 trial,Citation18 intensive glycemic control (targeted A1C <6.5%) and multifactorial intervention that targeted hypertension, dyslipidemia, microalbuminuria, and secondary prevention of CV disease with aspirin resulted in a lower risk of CV disease and microvascular complications compared with conventional treatment. A long-term follow-up of the Steno-2 trial (13.3 years)Citation19 found a 20% reduction in all-cause mortality among patients receiving intensive therapy vs patients receiving conventional therapy, even though the between-group differences in glycemic control and CV risk factors had disappeared during the follow-up period. A similar “legacy effect” or “metabolic memory” was observed in the UKPDSCitation20 and DCCT/EDIC trials,Citation15 supporting the view that early glycemic intervention in patients with diabetes reduces complications over the long term.
Conflicting results were observed in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial,Citation21 the Veterans Affairs Diabetes Trial (VADT),Citation22 and the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial,Citation23 in which intensive glycemic control resulted in no significant reductions in CV outcomes in patients with T2D and established CV disease and/or multiple CV risk factors. In the ACCORD trial, intensive glycemic control (target A1C <6.0%) compared with standard therapy (target A1C 7.0%–7.9%) was associated with an increase in mortality.Citation21 Subsequent analysis of the ACCORD data suggested that persistently high A1C on treatment was associated with an increased risk of mortality in the intensive treatment arm.Citation24 Severe hypoglycemia was associated with an increased risk of death in both treatment arms.Citation25 Although individuals in the intensive treatment arm had more episodes of hypoglycemia and severe hypoglycemia than those in the standard treatment arm, differences in the number and severity of hypoglycemic events did not appear to account for the increased mortality observed in the intensive treatment arm.Citation25,Citation26 However, it should be noted that hypoglycemia was only assessed by patients reporting events post hoc, during routine visits. Moreover, blood glucose measurements were not available at the time of death for patients who died. Weight gain was higher in the intensive treatment arm,Citation21 likely associated with the use of insulin and thiazolidinediones,Citation27 and may have contributed to the increased mortality risk. In a recently published analysis of the ACCORD trial data, there was no significant association of insulin dose with CV mortality.Citation28 Our view is that hypoglycemia and weight gain should be avoided in patients under our care.
Taken together, the results from the large interventional trials suggest that improved glycemic control early in the course of the disease with agents associated with low risk of hypoglycemia and weight gain, combined with treatment of CV risk factors, may be the best approach to comprehensive care for individuals with T2D.
Failure to initiate or intensify treatment to achieve glycemic goals (ie, treatment inertia) represents a major barrier to effective management of T2D. For example, in a retrospective cohort study of 81,573 patients with T2D, time to intensification of treatment in some patients was ≥7 years, resulting in prolonged duration of poor glycemic control.Citation29 Evidence-based treatment guidelines recommend metformin as first-line pharmacotherapy for most patients, adding other classes of antidiabetes agents if glycemic goals are not achieved within 3 months.Citation30,Citation31 Early combination therapy with agents that target several of the underlying defects contributing to hyperglycemia, especially when A1C is ≥9%, may improve patient outcomes.Citation30,Citation32 The combination of metformin with a sodium–glucose cotransporter-2 (SGLT-2) inhibitor may be a good option for many patients, because these agents have complementary mechanisms of action, neutral-to-positive effects on body weight, and low risk of hypoglycemia. This review focuses on the combination of metformin with dapagliflozin, a member of the SGLT-2 inhibitor class of antidiabetes agents.
Mechanisms of action of dapagliflozin and metformin
The kidney plays an important role in glucose homeostasis. The kidney uses glucose for its energy needs and, in the fasting state, ~10% of total systemic glucose uptake is by the kidneys.Citation33 In addition, it is the only organ capable of gluconeogenesis other than the liver;Citation33 after an overnight fast, ~20% of total glucose production can be attributed to kidney gluconeogenesis. Most important, the major contribution of the kidneys to glucose homeostasis is the reabsorption of filtered glucose. In healthy individuals, virtually all of the glucose that is filtered by the glomerulus is reabsorbed.Citation34 SGLT-2 is responsible for approximately 90% of the glucose reabsorption under normal conditions. In individuals with T2D, the capacity of the kidney to reabsorb glucose is increased,Citation35 possibly a result of SGLT-2 upregulation in response to chronic hyperglycemia,Citation34 leading to excessive glucose reabsorption and further exacerbation of the existing hyperglycemia.
Dapagliflozin is a highly selective SGLT-2 inhibitor that improves glycemic control independently of insulin secretion or action by reducing the reabsorption of filtered glucose and increasing glucose excretion in the urine.Citation36 Dapagliflozin is associated with a reduction in body weight, secondary to increased glucose excretion and related caloric loss,Citation37 and a reduction in blood pressure postulated to be related, at least in part, to its mild diuretic effect and the associated reduction in body weight.Citation38 The consequences of long-term pharmacological inhibition of SGLT-2 are unknown. Individuals with familial renal glucosuria, in whom mutations in the gene coding for SGLT-2 result in substantial glucosuria, are generally healthy.Citation39 Data from large clinical trials of up to 4 years in duration suggest that dapagliflozin is well tolerated and produces sustained reductions in A1C and body weight.Citation40–Citation43 Additional data on the long-term benefits and risks associated with dapagliflozin use are being accumulated through postmarketing surveillance and in the ongoing CV outcomes trial of dapagliflozin (Dapagliflozin Effect on Cardiovascular Events [DECLARE-TIMI 58]), which is assessing the CV safety and potential benefit of dapagliflozin in patients with T2D at high risk for CV events.Citation44
In the recently published CV outcomes trial with empagliflozin (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients [EMPA-REG OUTCOME]) in patients with T2D and established CV disease receiving standard of care for other CV risk factors, the primary composite CV outcome of death from CV causes, nonfatal myocardial infarction, or nonfatal stroke occurred in a significantly lower proportion of patients receiving empagliflozin (10.5%) compared with placebo (12.1%; hazard ratio [95% confidence interval], 0.86 [0.74, 0.99]; P=0.04 for superiority).Citation45 Empagliflozin treatment was also associated with a significantly lower risk of death from any cause (0.68 [0.57, 0.82]; P<0.001), death from CV causes (0.62 [0.49, 0.77]; P<0.001), and hospitalization for heart failure (0.65 [0.50, 0.85]; P=0.002) compared with placebo. There were no significant differences between the empagliflozin and placebo groups in the occurrence of nonfatal myocardial infarction (4.5% vs 5.2%; 0.87 [0.70, 1.09]; P=0.22) or nonfatal stroke (3.2% vs 2.6%; 1.24 [0.92, 1.67]; P=0.16). Whether or not these findings are a class effect of SGLT-2 inhibitors remains to be determined. Results of ongoing CV outcome trials with dapagliflozin (DECLARE-TIMI 58)Citation44 and canagliflozin (Canagliflozin Cardiovascular Assessment Study [CANVAS])Citation46 may shed additional light on the potential of SGLT-2 inhibitors to be cardioprotective in patients with T2D.
Dapagliflozin and other SGLT-2 inhibitors are associated with increases in endogenous glucose production and glucagon concentrations that appear to be independent of the reduction in plasma glucose by SGLT-2 inhibition and may partially blunt the glucose-lowering effects of SGLT-2 inhibitors.Citation47,Citation48 SGLT-2 is expressed in pancreatic α-cells, and inhibition of SGLT-2 with dapagliflozin was shown to increase glucagon secretion from α-cells in vitro via activation of ATP-sensitive potassium channels, suggesting a potential mechanism for the increase in glucagon.Citation49
Metformin is a biguanide that has been used for several decades to reduce hyperglycemia in patients with T2D, yet its mechanism of action is still incompletely understood.Citation50 Recently, it has been shown that metformin reduces hepatic glucose production by noncompetitively inhibiting the redox shuttle enzyme mitochondrial glycerophosphate dehydrogenase, thereby altering the hepatocellular redox state,Citation51 which results in activation of AMP-activated protein kinaseCitation52 and reduction of hepatic gluconeogenesis.Citation53 Although the main effect of metformin is to suppress hepatic glucose production,Citation54 it may also reduce intestinal absorption of glucoseCitation55 and increase peripheral glucose uptake, thereby improving insulin sensitivity.Citation54 Metformin also increases glucagon-like peptide-1 (GLP-1) concentrationsCitation56 via a muscarinic 3 receptor and gastrin-releasing peptide receptor–dependent mechanism.Citation57
The combination of metformin and dapagliflozin targets both insulin-dependent and insulin-independent mechanisms to reduce hyperglycemia. Through both direct and indirect effects, the combination of metformin and dapagliflozin may affect several of the underlying mechanisms that contribute to hyperglycemia (), leading to decreased hepatic glucose production (metformin), inhibition of renal reabsorption of glucose (dapagliflozin), improved peripheral insulin sensitivity (metformin and dapagliflozinCitation48), improved β-cell function via reduced glucotoxicity (metformin and dapagliflozin), reduced intestinal absorption of glucose (metformin), and possibly increased GLP-1 secretion by L-cells in the colon (metforminCitation58,Citation59).
Efficacy studies with the combination of dapagliflozin and metformin
Add-on of dapagliflozin to metformin
Patients with inadequate glycemic control (baseline A1C 7.9%–8.2%) on stable metformin doses (≥1,500 mg/d) were randomized to placebo or dapagliflozin (5 or 10 mg/d) in addition to background metformin.Citation60 At 24 weeks, the adjusted mean change in A1C was significantly greater in patients receiving dapagliflozin 5 (−0.70%) or 10 mg/d (−0.84%, both P<0.0001) than in those receiving placebo (−0.30%; ). Significantly larger reductions in body weight (−3.0 and −2.9 kg, respectively, P<0.0001) were observed with both doses of dapagliflozin vs placebo (−0.9 kg). More patients achieved A1C <7% with dapagliflozin 5 (37.5%, P=0.0275) or 10 mg/d (40.6%, P=0.0062) than with placebo (25.9%). Systolic and diastolic blood pressure, measured as safety variables, decreased by 4–5 and 2–3 mmHg, respectively, with dapagliflozin, compared with decreases of 0.2 and 0.1 mmHg with placebo. The reductions in A1C and body weight were sustained over 102 weeks of treatmentCitation41 ().
Table 1 Efficacy results of randomized clinical trials with dapagliflozin add-on to metformin
Effects of dapagliflozin add-on to metformin on body weight and composition
A randomized, double-blind, placebo-controlled study was conducted to assess changes in body weight and composition by dual-energy X-ray absorptiometry in patients with T2D (baseline A1C, 7.2%, body mass index, 32 kg/m2) receiving placebo or dapagliflozin (10 mg/d) add-on to metformin (≥1,500 mg/d).Citation37 After 24 weeks, dapagliflozin produced a significantly greater reduction in body weight than placebo (2.96 vs 0.88 kg, P<0.0001; ). A reduction in fat mass accounted for two-thirds of the total weight reduction with dapagliflozin. Although not a primary end point in this trial, dapagliflozin also significantly reduced A1C compared with placebo (−0.39% vs −0.10%, P<0.0001). Changes in seated systolic and diastolic blood pressure were −2.7 and −0.7 mmHg with dapagliflozin, respectively, and 0.1 and 0.3 mmHg with placebo. The decreases in body weight, fat mass, and A1C were maintained over 102 weeks of treatment.Citation42
Add-on of dapagliflozin to insulin ± metformin
Management of patients with inadequate glycemic control on insulin is challenging because increasing insulin dose carries the risks of additional weight gain and hypoglycemia. Treatment guidelines suggest considering the addition of other agents, including SGLT-2 inhibitors, to insulin in order to improve glycemic control and reduce the need for additional insulin.Citation30 In a randomized, placebo-controlled trial,Citation61 patients with baseline A1C of 8.5%–8.6% and a 13- to 14-year history of T2D received placebo or dapagliflozin (5 or 10 mg/d) in addition to insulin (mean daily dose 77 U) for 24 weeks, followed by extensions up to 104 weeks. Approximately 50% of patients received up to two other oral antidiabetes medications in addition to insulin, primarily metformin (45%–48% of patients). After 24 weeks, dapagliflozin add-on to insulin ± metformin produced larger reductions in A1C (5 mg/d, −0.89%; 10 mg/d, −0.96%, P<0.001 for both) compared with placebo add-on to insulin ± metformin (−0.39%). Body weight was significantly reduced (P<0.001) in the dapagliflozin groups compared with weight gain in the placebo group (). At 24 weeks, only 9.7%–10.6% of patients receiving dapagliflozin required insulin uptitration or discontinued from the study because of poor glycemic control compared with 29.2% in the placebo group. The adjusted mean change from baseline to 24 weeks in daily insulin dose was 5.65 U in the placebo group compared with −0.63 and −1.18 U in the dapagliflozin 5 and 10 mg groups, respectively. The favorable changes in A1C, body weight, and insulin requirements with dapagliflozin were maintained when assessed at 48Citation61 and 104 weeks.Citation43
In the subgroup of patients treated with both insulin and metformin, the addition of dapagliflozin produced numerically larger reductions in A1C (5 mg/d, −0.89%; 10 mg/d, −0.95%) compared with patients receiving placebo (−0.27%). Changes in body weight with dapagliflozin (5 mg/d, −1.58 kg; 10 mg/d, −1.85 kg) were also greater than with placebo (−0.05 kg).Citation62 Similar to the results from the entire study population, the mean change from baseline to 24 weeks in insulin dose was 6.19 U in the placebo group compared with −0.74 and −1.88 U in the dapagliflozin 5 and 10 mg groups, respectively; 10.2% and 7.7% of patients receiving dapagliflozin 5 or 10 mg/d, respectively, required insulin uptitration or discontinued from the study because of poor glycemic control compared with 26.3% in the placebo group.
Dapagliflozin add-on vs glipizide add-on to metformin
The efficacy and safety of dapagliflozin compared with glipizide as add-on to metformin was assessed in a 52-week noninferiority trial in patients with T2D inadequately controlled with metformin.Citation63 Patients with baseline A1C of 7.7% on stable metformin doses (1,500–2,500 mg/d) received double-blind dapagliflozin uptitrated from 2.5 mg/d to a maximum of 10 mg/d or glipizide 5 mg/d uptitrated to a maximum of 20 mg/d if fasting plasma glucose was ≥6.1 mmol/L during an 18-week titration period. At the end of the titration period, the mean doses of dapagliflozin and glipizide were 9.2 and 16.4 mg/d, respectively. After 52 weeks of treatment, the adjusted mean change from baseline in A1C was −0.52% in the two groups, meeting the study’s primary end point of noninferiority. Dapagliflozin produced body weight reduction (−3.2 kg; P<0.0001), whereas glipizide led to an increase in weight (1.4 kg; ). Mean changes from baseline in systolic and diastolic blood pressure with dapagliflozin were −4.3 and −1.6 mmHg vs 0.8 and −0.4 mmHg with glipizide, respectively. A1C reduction and decreases in body weight appeared more sustained with dapagliflozin than glipizide over 208 weeks of treatment (), and reductions in blood pressure with dapagliflozin were sustained with continued treatment.Citation40,Citation64
Initial combination of dapagliflozin with metformin in treatment-naïve patients
For patients presenting with A1C ≥9%, treatment guidelines recommend combination therapy to achieve individualized glycemic targets.Citation30,Citation31 Two studies assessed the effects of initial combination of dapagliflozin (one study with a dose of 5 mg/d and the other study with a dose of 10 mg/d) and metformin extended release (median dose 2,000 mg/d) compared with dapagliflozin plus placebo and metformin plus placebo in treatment-naïve patients with baseline A1C 9.1%–9.2%.Citation65 In the study with the 5 mg/d dose, after 24 weeks of treatment, mean reductions from baseline in A1C were −2.05% for dapagliflozin plus metformin (P<0.0001 vs metformin plus placebo), −1.35% for metformin plus placebo, and −1.19% for dapagliflozin plus placebo. In the study with the 10 mg/d dose, mean reductions from baseline to 24 weeks in A1C were −1.98%, −1.44%, and −1.45% for dapagliflozin plus metformin (P<0.0001 vs metformin plus placebo), metformin plus placebo, and dapagliflozin plus placebo, respectively (). In a prespecified analysis, the change in A1C with dapagliflozin 10 mg/d plus placebo was noninferior to the change with metformin plus placebo. In both studies, weight reduction was greater with dapagliflozin vs placebo, and a larger proportion of patients achieved A1C <7% with dapagliflozin than with placebo ().
Dual add-on of saxagliptin plus dapagliflozin to metformin
As glycemic control worsens, patients typically receive stepwise therapy with sequential addition of single oral agents to metformin. A clinical trial evaluated dual add-on of combination treatment consisting of the dipeptidyl peptidase-4 inhibitor saxagliptin (5 mg/d) and dapagliflozin (10 mg/d) to metformin (≥1,500 mg/d) as triple therapy compared with the addition of each of the individual components singly to metformin as dual therapy.Citation66 Patients had a mean baseline A1C of 8.94% and T2D duration of 7.6 years. The addition of saxagliptin plus dapagliflozin to metformin therapy resulted in significantly greater adjusted mean reductions from baseline in A1C at 24 weeks than did therapy with saxagliptin add-on to metformin (P<0.0001) or dapagliflozin add-on to metformin (P=0.0166; ). The reduction in body weight was greatest in the dapagliflozin-containing treatment arms, and the proportion of patients achieving A1C <7% at week 24 with the dual add-on, although not tested for statistical significance, was almost double that seen in the single add-on groups.
In these clinical trials, dapagliflozin produced significant and sustained reductions in A1C and body weight when given in combination with metformin. Although not shown, dapagliflozin also significantly reduced fasting plasma glucoseCitation37,Citation60,Citation61,Citation65,Citation66 and, when measured, postprandial glucose.Citation66 These changes were accompanied by modest decreases in blood pressure. In an analysis of data pooled from 13 placebo-controlled trials, dapagliflozin reduced blood pressure in both normotensive and hypertensive patients with T2D, without changes in heart rate.Citation67 The changes in blood pressure may be partly the result of mild osmotic diuresisCitation38 and weight loss.Citation68 Thus, dapagliflozin add-on to metformin improves glycemic control and has favorable effects on CV risk factors.
Safety and tolerability of dapagliflozin and metformin combination therapy
In clinical trials with dapagliflozin, the most common (≥5%) adverse events (AEs) included nasopharyngitis, headache, upper respiratory infection, diarrhea, and back pain. In addition, certain AEs were considered to be of special interest based on the mechanism of action of dapagliflozin. These included signs, symptoms, or other reports suggestive of genital and urinary tract infections, renal AEs (renal failure or impairment), diuresis/volume-related AEs (hypotension, hypovolemia, and dehydration), and hypoglycemia.Citation37,Citation60,Citation61,Citation63,Citation65,Citation66 Occurrence of these AEs in clinical trials of 24- to 52-week duration will now be discussed. For trials with long-term extension periods, with total duration of up to 102–208 weeks, a similar pattern of AEs was observed.Citation40–Citation43,Citation64
Add-on of dapagliflozin to metformin
The proportion of patients with ≥1 AE was similar in the dapagliflozin (69%–73%) and placebo (64%) groups.Citation60 The incidence of urinary tract infections with dapagliflozin (7%–8%) was similar to placebo (8%), but genital infections were more frequent in the dapagliflozin groups (9%–13%) compared with placebo (5%). Diuresis-related AEs were uncommon (≤1%) across all treatment groups, as were events of hypoglycemia (dapagliflozin, 4%; placebo, 3%).
Effects of dapagliflozin add-on to metformin on body weight and composition
Similar proportions of patients had ≥1 AE with dapagliflozin (43%) and placebo (40%). Genital (3% vs 0%) and urinary tract infections (7% vs 2%) were more common with dapagliflozin than with placebo.Citation37 Hypoglycemia events were similar in the dapagliflozin (2%) and placebo (3%) groups.
Add-on of dapagliflozin to insulin ± metformin
The percentage of patients experiencing ≥1 AE was similar across treatment groups (72%–74%).Citation61 Patients receiving dapagliflozin, compared with those receiving placebo, had more genital infections (10%–11% vs 3%) and urinary tract infections (10%–11% vs 5%). Renal AEs (2%–3% vs 2%) and volume-related AEs (2% vs 1%) were infrequent and similar between the dapagliflozin and placebo groups. As expected with insulin therapy, sizable but similar proportions of patients had ≥1 episode of hypoglycemia with dapagliflozin (54%–56%) and placebo (52%). Major episodes of hypoglycemia (defined as a symptomatic episode in which the patient required external assistance because of severe impairment in consciousness or behavior, had a capillary or plasma glucose level <54 mg/dL, and promptly recovered after receiving glucose or glucagon) occurred in 1%–2% of patients in the dapagliflozin groups and 1% of patients in the placebo group.
In the subgroup of patients on background metformin, the proportion of patients with ≤1 AE was higher with dapagliflozin (68%) than with placebo (59%) during the 104-week extended treatment period.Citation62 Urinary tract and genital infections were more frequent with dapagliflozin (11%–18% and 12%–15%, respectively) than with placebo (3% and 5%, respectively). Renal and volume-related AEs were infrequent (2%–3%) and similar between dapagliflozin and placebo groups. A greater proportion of patients experienced hypoglycemia with dapagliflozin (54%–60%) than with placebo (39%). There was one event (1%) of major hypoglycemia with dapagliflozin and none with placebo.
Dapagliflozin add-on vs glipizide add-on to metformin
The proportion of patients with ≥1 AE was 78% with both dapagliflozin and glipizide.Citation63 Genital and urinary tract infections were more common with dapagliflozin (12% and 11%, respectively) than with glipizide (3% and 6%, respectively). Renal AEs with dapagliflozin (6%) were more frequent than with glipizide (3%). Volume-related AEs were infrequent (dapagliflozin, 2%; glipizide, 1%). Events of hypoglycemia were ≥10-fold lower with dapagliflozin (3%) compared with glipizide (40%). Three patients (0.7%) in the glipizide group had a major episode of hypoglycemia compared with none in the dapagliflozin group.
Initial combination of dapagliflozin with metformin in treatment-naïve patients
Similar proportions of patients had ≥1 AE with dapagliflozin 5 and 10 mg/d plus metformin (69% and 60%, respectively) compared with dapagliflozin plus placebo (53% and 60%) and metformin plus placebo (59% and 57%).Citation65 Genital infections were more common with dapagliflozin 5 (7%) and 10 mg/d (9%) plus metformin and dapagliflozin plus placebo (7% and 13%) compared with metformin plus placebo (2%). The incidence of urinary tract infections was 8% for dapagliflozin 5 mg/d plus metformin, metformin plus placebo, and dapagliflozin 5 mg/d plus placebo but was higher with dapagliflozin 10 mg/d plus metformin (8%) and dapagliflozin 10 mg/d plus placebo (11%) than with metformin plus placebo (4%). Volume-related AEs were infrequent with dapagliflozin plus metformin (≤0.5%) and dapagliflozin plus placebo (≤2%), and no events were reported with metformin plus placebo. Hypoglycemia occurrence was similar with dapagliflozin plus metformin (3%), dapagliflozin plus placebo (0%–1%), and metformin plus placebo (0%–3%), and no episodes of major hypoglycemia were reported in either study.
Dual add-on of saxagliptin plus dapagliflozin to metformin
The proportion of patients experiencing ≥1 AE was similar across treatment groups (49%–53%).Citation66 Genital infections were more common in the dapagliflozin plus metformin group (6%) compared with the saxagliptin and dapagliflozin plus metformin group (0) and the saxagliptin plus metformin group (<1%). Urinary tract infections were more common in the saxagliptin plus metformin (5%) and dapagliflozin plus metformin groups (4%) than in the saxagliptin and dapagliflozin plus metformin group (0.6%). Events of hypoglycemia were few and occurred in similar proportions across the three treatment groups (1%), and no episodes of major hypoglycemia were reported.
Overall summary of safety
Overall, dapagliflozin as add-on therapy to metformin was well tolerated and associated with low rates of hypoglycemia. Genital infections and, in some studies, urinary tract infections were more frequent with dapagliflozin than with placebo. This appears to be a class effect of the SGLT-2 inhibitors.Citation69 The increase in genital infections in patients with T2D receiving dapagliflozin may be related to glucosuria,Citation70 but a relationship between urinary tract infections and glucosuria in the context of SGLT-2 inhibition is less clear.Citation71 In the dapagliflozin clinical development program, both genital and urinary tract infections were generally mild to moderate, rarely led to discontinuation, and were typically managed with standard antimicrobial or antifungal agents.Citation70,Citation71 According to spontaneous reports to the US Food and Drug Administration (FDA) Adverse Event Reporting System (FAERS), 19 patients receiving SGLT-2 inhibitors experienced urosepsis or pyelonephritis from March 2013 through October 2014.Citation72 All patients were hospitalized, and a few were admitted to an intensive care unit or underwent dialysis for the treatment of kidney failure. However, we note that FAERS provides no data on the denominator or the incidence of pyelonephritis in patients with T2D not taking SGLT-2 inhibitors. Dapagliflozin has a mild diuretic effect, but volume-related AEs were uncommon in clinical trials. Because the mechanism of action of SGLT-2 inhibitors depends on glomerular filtration rate (GFR)Citation34 and because of concerns of increased AE frequency in patients with moderate renal impairment, dapagliflozin should not be used in patients with an estimated GFR <60 mL/min/1.73 m2.Citation73
The FDA recently issued a drug safety communication that warned of an increased risk of diabetic ketoacidosis (DKA) associated with SGLT-2 inhibitor use.Citation72 Between March 2013 and May 2015, 73 cases of DKA were identified in patients (mostly with T2D) treated with SGLT-2 inhibitors. In the dapagliflozin clinical development program of more than 18,000 patients treated with dapagliflozin, reports of events suggestive of DKA were rare (<0.1%).Citation74 DKA is usually associated with marked hyperglycemia (>250 mg/dL) as the result of insulin deficiency.Citation75 DKA associated with SGLT-2 inhibitor use may present with smaller or even no increases in plasma glucose concentrations (“euglycemic DKA”) likely related to increased urinary glucose excretion.Citation74,Citation76 In addition, it has been shown that SGLT-2 inhibitors increase plasma glucagon concentrations.Citation47,Citation48 It is postulated that lipolysis and ketogenesis are stimulated as a result of a lower insulin:glucagon ratio and reduced glucose availability.Citation74 An assessment of DKA risk in both T1D and T2D has recently been conducted by the American Association of Clinical Endocrinologists, a summary of which is available online.Citation77 Patients and health care providers need to be aware of the signs and symptoms of DKA and the measures used to recognize and treat it.
Patient-focused perspectives: quality of life, satisfaction, and acceptability
Patient preference and quality of life (QoL) are important considerations when choosing pharmacotherapy in T2D,Citation30 especially in view of the relatively low patient adherence to antidiabetes medicationsCitation78,Citation79 that can lead to increased hospitalization and mortality.Citation80 Health-related QoL was evaluated in patients participating in a dapagliflozin add-on to metformin trial.Citation37,Citation42 Perceived health status and QoL were evaluated with the EuroQol-5 (EQ-5D), a standardized index of health status that consists of measures of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.Citation81 Overall, patient-reported QoL was high at weeks 24, 50, and 102, and there were no statistical differences in EQ-5D scores at any time point between dapagliflozin and placebo groups. Thus, high health-related QoL scores were maintained from baseline to 102 weeks with dapagliflozin add-on to metformin.Citation81
Weight loss-related QoL was also analyzed using the Study to Help Improve Early Evaluation and Management of Risk Factors Leading to Diabetes Weight Questionnaire-9 (SHIELD-WQ-9), a weight change-related QoL survey.Citation82 At week 24, significantly more patients in the dapagliflozin group reported improvements in overall health-related QoL (29.3%, P=0.02) than those in the placebo group (14.0%). QoL scores were numerically higher with dapagliflozin vs placebo at week 50 (26.6% vs 17.9%) and at week 102 (32.4% vs 18.3%), but the differences were not statistically significant. In both treatment groups, significantly more patients (P<0.05) who had weight loss reported improvements in physical health, self-esteem, and overall QoL than those who had gained weight.Citation82
Clinical practice experience
Dapagliflozin reduces blood glucose concentrations, body weight, and systolic blood pressure when combined with metformin. Although dapagliflozin is generally well tolerated, there are some practical recommendations to reduce potential side effects. For example, because of the modest diuretic effect of dapagliflozin,Citation38 volume status should be checked, especially in the elderly, and doses of diuretics and other antihypertensive medications should be adjusted to avoid the potential for hypovolemia. Patients should be encouraged to increase fluid intake and to expect an increase in urination and possibly nocturia. Renal function should be assessed before initiating dapagliflozin treatment and monitored during therapy.
Patients should be advised of the increased risk of genital and urinary tract infections associated with SGLT-2 inhibitors, especially in patients with a history of such infections. Patients need to be counseled that the risk of infection can be minimized by increasing fluid intake and by fastidious bathroom habits and preventative measures such as the routine use of hygienic wipes or sprays.
Conclusion and the place of dapagliflozin add-on to metformin in therapy
Guidelines generally recommend sequential treatment of T2D with addition of agents if treatment goals are not achieved after a specified period, typically 3 months.Citation30,Citation31 By using serum fructosamine concentrations, which reflect average glycemic control over 1 month,Citation83 therapeutic decisions can be made even faster. Because of the risks of hypoglycemia and concerns coming from the ADVANCE,Citation23 ACCORD,Citation21 and VADTCitation22 data, guidelines also suggest less stringent glycemic targets for some patients, including older patients, those with longer disease duration, shorter life expectancy, significant comorbidities, established vascular complications, limited support systems, or diminished capacity for self-care.
However, given the known consequences of chronic hyperglycemia and our emerging understanding of the pathophysiology of T2D, early combination therapy with agents with complementary mechanisms of action that are not associated with weight gain and do not increase the risk of hypoglycemia may be appropriate therapy to enable patients, including the elderly and those with longer disease duration, short life expectancy, significant comorbidities, or established vascular complications, to achieve individualized glycemic goals.
The combination of dapagliflozin and metformin provided sustained glycemic control and reductions in body weight for up to 208 weeks, without increased risk of hypoglycemia, both as initial combination therapy in treatment-naïve patients and in patients with inadequate response to metformin monotherapy. The combination of dapagliflozin and metformin is an attractive alternative to a sulfonylurea or thiazolidinedione plus metformin, especially in patients at risk of hypoglycemia or in patients who want to avoid weight gain.
Acknowledgments
Medical writing support for the preparation of this manuscript was provided by Richard Edwards, PhD, and Janet Matsuura, PhD, from Complete Healthcare Communications, LLC (Chadds Ford, PA), with funding from AstraZeneca.
Disclosure
SS has served as an advisory board member for Janssen, Merck, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, Salix, Novo Nordisk, Takeda, and Genesis Biotechnology Group and on the speakers bureaus of Takeda, Janssen, Merck, Novo Nordisk, Salix, Boehringer Ingelheim, Eli Lilly, Eisai, AstraZeneca, GlaxoSmithKline, and Amgen. AK was an employee of AstraZeneca during the development of this manuscript. The authors report no other conflicts of interest in this work.
References
- World Health Organization Obesity and Overweight Geneva, Switzerland World Health Organization 2015 Available from: http://www.who.int/mediacentre/factsheets/fs311/en/ Accessed August 30, 2015
- International Diabetes Federation Diabetes: Facts and Figures Brussels, Belgium International Diabetes Federation 2014 Available from: https://www.idf.org/worlddiabetesday/toolkit/gp/facts-figures Accessed August 30, 2015
- Kahn SE Cooper ME Del Prato S Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future Lancet 2014 383 9922 1068 1083 24315620
- Fonseca VA Defining and characterizing the progression of type 2 diabetes Diabetes Care 2009 32 Suppl 2 S151 S156 19875543
- DeFronzo R Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus Diabetes 2009 58 4 773 795 19336687
- Centers for Disease Control and Prevention National Diabetes Statistics Report: Estimates of Diabetes and its Burden in the United States, 2014 Atlanta, GA Centers for Disease Control and Prevention 2014 Available from: http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf Accessed September 23, 2015
- Wing RR Lang W Wadden TA Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes Diabetes Care 2011 34 7 1481 1486 21593294
- Nathan DM Buse JB Davidson MB Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the study of diabetes Diabetes Care 2009 32 1 193 203 18945920
- Ali MK Bullard KM Saaddine JB Cowie CC Imperatore G Gregg EW Achievement of goals in US diabetes care, 1999–2010 N Engl J Med 2013 368 17 1613 1624 23614587
- Stark Casagrande S Fradkin JE Saydah SH Rust KF Cowie CC The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010 Diabetes Care 2013 36 8 2271 2279 23418368
- Gerstein HC Swedberg K Carlsson J The hemoglobin A1C level as a progressive risk factor for cardiovascular death, hospitalization for heart failure, or death in patients with chronic heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and Morbidity (CHARM) program Arch Intern Med 2008 168 15 1699 1704 18695086
- Selvin E Marinopoulos S Berkenblit G Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus Ann Intern Med 2004 141 6 421 431 15381515
- Stratton IM Adler AI Neil HA Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study BMJ 2000 321 7258 405 412 10938048
- The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus N Engl J Med 1993 329 14 977 986 8366922
- Nathan DM Cleary PA Backlund JY Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes N Engl J Med 2005 353 25 2643 2653 16371630
- UK Prospective Diabetes Study Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet 1998 352 9131 837 853 9742976
- UK Prospective Diabetes Study Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet 1998 352 9131 854 865 9742977
- Gaede P Vedel P Larsen N Jensen GV Parving HH Pedersen O Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes N Engl J Med 2003 348 5 383 393 12556541
- Gaede P Lund-Andersen H Parving HH Pedersen O Effect of a multi-factorial intervention on mortality in type 2 diabetes: results and projections from the Steno-2 study N Engl J Med 2008 358 6 580 591 18256393
- Holman RR Paul SK Bethel MA Matthews DR Neil HA 10-year follow-up of intensive glucose control in type 2 diabetes N Engl J Med 2008 359 15 1577 1589 18784090
- Gerstein HC Miller ME Byington RP Effects of intensive glucose lowering in type 2 diabetes N Engl J Med 2008 358 24 2545 2559 18539917
- Duckworth W Abraira C Moritz T Glucose control and vascular complications in veterans with type 2 diabetes N Engl J Med 2009 360 2 129 139 19092145
- Patel A MacMahon S Chalmers J Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes N Engl J Med 2008 358 24 2560 2572 18539916
- Riddle MC Ambrosius WT Brillon DJ Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial Diabetes Care 2010 33 983 990 20427682
- Bonds DE Miller ME Bergenstal RM The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study BMJ 2010 340 b4909 20061358
- Seaquist ER Miller ME Bonds DE The impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study Diabetes Care 2012 35 2 409 414 22179956
- Fonseca V McDuffie R Calles J Determinants of weight gain in the action to control cardiovascular risk in diabetes trial Diabetes Care 2013 36 8 2162 2168 23412077
- Siraj ES Rubin DJ Riddle MC Insulin dose and cardiovascular mortality in the ACCORD trial Diabetes Care 2015 38 11 2000 2008 26464212
- Khunti K Wolden ML Thorsted BL Andersen M Davies MJ Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people Diabetes Care 2013 36 11 3411 3417 23877982
- American Diabetes Association Standards of medical care in diabetes-2015 Diabetes Care 2015 38 Suppl 1 S88 S89
- Garber AJ Abrahamson MJ Barzilay JI AACE/ACE comprehensive diabetes management algorithm 2015 Endocr Pract 2015 21 4 e1 e10
- DeFronzo RA Eldor R Abdul-Ghani M Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes Diabetes Care 2013 36 Suppl 2 S127 S138 23882037
- Gerich JE Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications Diabet Med 2010 27 2 136 142 20546255
- Wilding JP The role of the kidneys in glucose homeostasis in type 2 diabetes: clinical implications and therapeutic significance through sodium glucose co-transporter 2 inhibitors Metabolism 2014 63 10 1228 1237 25104103
- DeFronzo RA Hompesch M Kasichayanula S Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes Diabetes Care 2013 36 10 3169 3176 23735727
- Whaley JM Tirmenstein M Reilly TP Targeting the kidney and glucose excretion with dapagliflozin: preclinical and clinical evidence for SGLT2 inhibition as a new option for treatment of type 2 diabetes mellitus Diabetes Metab Syndr Obes 2012 5 135 148 22923998
- Bolinder J Ljunggren O Kullberg J Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin J Clin Endocrinol Metab 2012 97 3 1020 1031 22238392
- Lambers Heerspink HJ de Zeeuw D Wie L Leslie B List J Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes Diabetes Obes Metab 2013 15 9 853 862 23668478
- Calado J Santer R Rueff J Effect of kidney disease on glucose handling (including genetic defects) Kidney Int Suppl 2011 120 S7 S13 21358700
- Del Prato S Nauck M Duran-Garcia S Long-term glycaemic response and tolerability of dapagliflozin versus a sulphonylurea as add-on therapy to metformin in patients with type 2 diabetes: 4-year data Diabetes Obes Metab 2015 17 6 581 590 25735400
- Bailey CJ Gross JL Hennicken D Iqbal N Mansfield TA List JF Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial BMC Med 2013 11 43 23425012
- Bolinder J Ljunggren O Johansson L Dapagliflozin maintains glycaemic control while reducing weight and body fat mass over 2 years in patients with type 2 diabetes mellitus inadequately controlled on metformin Diabetes Obes Metab 2014 16 2 159 169 23906445
- Wilding JP Woo V Rohwedder K Sugg J Parikh S Dapagliflozin 006 Study G Dapagliflozin in patients with type 2 diabetes receiving high doses of insulin: efficacy and safety over 2 years Diabetes Obes Metab 2014 16 2 124 136 23911013
- Astra Zeneca Multicenter trial to evaluate the effect of dapagliflozin on the incidence of cardiovascular events (DECLARE-TIMI58) NLM identifier: NCT01730534. Available from: https://clinicaltrials.gov/ct2/show/NCT01730534 Accessed September 22, 2015
- Zinman B Wanner C Lachin JM Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes N Engl J Med 2015 373 22 2117 2128 26378978
- Neal B Perkovic V de Zeeuw D Rationale, design, and baseline characteristics of the Canagliflozin Cardiovascular Assessment Study (CANVAS) – a randomized placebo-controlled trial Am Heart J 2013 166 2 217 223.e211 23895803
- Ferrannini E Muscelli E Frascerra S Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients J Clin Invest 2014 124 2 499 508 24463454
- Merovci A Solis-Herrera C Daniele G Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production J Clin Invest 2014 124 2 509 514 24463448
- Bonner C Kerr-Conte J Gmyr V Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion Nat Med 2015 21 5 512 517 25894829
- Witters LA The blooming of the French lilac J Clin Invest 2001 108 8 1105 1107 11602616
- Madiraju AK Erion DM Rahimi Y Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase Nature 2014 510 7506 542 546 24847880
- Stephenne X Foretz M Taleux N Metformin activates AMP-activated protein kinase in primary human hepatocytes by decreasing cellular energy status Diabetologia 2011 54 12 3101 3110 21947382
- Zhou G Myers R Li Y Role of AMP-activated protein kinase in mechanism of metformin action J Clin Invest 2001 108 8 1167 1174 11602624
- Viollet B Guigas B Sanz Garcia N Leclerc J Foretz M Andreelli F Cellular and molecular mechanisms of metformin: an overview Clin Sci (Lond) 2012 122 6 253 270 22117616
- Glucophage® (Metformin HCl tablets) and Glucophage XR® (Metformin HCl) extended-release tablets [prescribing information] Princeton, NJ Bristol-Myers Squibb Company 2009
- Mannucci E Ognibene A Cremasco F Effect of metformin on glucagon-like peptide 1 (GLP-1) and leptin levels in obese nondiabetic subjects Diabetes Care 2001 24 3 489 494 11289473
- Mulherin AJ Oh AH Kim H Grieco A Lauffer LM Brubaker PL Mechanisms underlying metformin-induced secretion of glucagon-like peptide-1 from the intestinal L cell Endocrinology 2011 152 12 4610 4619 21971158
- Buse JB DeFronzo RA Rosenstock J The primary glucose-lowering effect of metformin resides in the gut, not the circulation. Results from short-term pharmacokinetic and 12-week dose-ranging studies Diabetes Care 2015 39 2 198 205 26285584
- Napolitano A Miller S Nicholls AW Novel gut-based pharmacology of metformin in patients with type 2 diabetes mellitus PLoS One 2014 9 7 e100778 24988476
- Bailey CJ Gross JL Pieters A Bastien A List JF Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial Lancet 2010 375 9733 2223 2233 20609968
- Wilding JP Woo V Soler NG Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial Ann Intern Med 2012 156 6 405 415 22431673
- Katz A Yeh HC Efficacy and safety of dapagliflozin in patients with type 2 diabetes on insulin ± metformin regimens Diabetes 2015 64 Suppl 1 A317
- Nauck MA Del Prato S Meier JJ Dapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin: a randomized, 52-week, double-blind, active-controlled noninferiority trial Diabetes Care 2011 34 9 2015 2022 21816980
- Nauck MA Del Prato S Duran-Garcia S Durability of glycaemic efficacy over 2 years with dapagliflozin versus glipizide as add-on therapies in patients whose type 2 diabetes mellitus is inadequately controlled with metformin Diabetes Obes Metab 2014 16 11 1111 1120 24919526
- Henry RR Murray AV Marmolejo MH Hennicken D Ptaszynska A List JF Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial Int J Clin Pract 2012 66 5 446 456 22413962
- Rosenstock J Hansen L Zee P Dual add-on therapy in type 2 diabetes poorly controlled with metformin monotherapy: a randomized double-blind trial of saxagliptin plus dapagliflozin addition versus single addition of saxagliptin or dapagliflozin to metformin Diabetes Care 2015 38 3 376 383 25352655
- Sjostrom CD Johansson P Ptaszynska A List J Johnsson E Dapagliflozin lowers blood pressure in hypertensive and non-hypertensive patients with type 2 diabetes Diab Vasc Dis Res 2015 12 5 352 358 26008804
- Sjostrom CD Hashemi M Sugg J Ptaszynska A Johnsson E Dapagliflozin-induced weight loss affects 24-week glycated haemoglobin and blood pressure levels Diabetes Obes Metab 2015 17 8 809 812 25997813
- Geerlings S Fonseca V Castro-Diaz D List J Parikh S Genital and urinary tract infections in diabetes: impact of pharmacologically-induced glucosuria Diabetes Res Clin Pract 2014 103 3 373 381 24529566
- Johnsson KM Ptaszynska A Schmitz B Sugg J Parikh SJ List JF Vulvovaginitis and balanitis in patients with diabetes treated with dapagliflozin J Diabetes Complications 2013 27 5 479 484 23806570
- Johnsson KM Ptaszynska A Schmitz B Sugg J Parikh SJ List JF Urinary tract infections in patients with diabetes treated with dapagliflozin J Diabetes Complications 2013 27 5 473 478 23849632
- US Food Drug Administration FDA Drug Safety Communication: FDA Revises Labels of SGLT2 Inhibitors for Diabetes to Include Warnings about too Much Acid in the Blood and Serious Urinary Tract Infections Silver Spring, MD US Food and Drug Administration 2015 Available from: http://www.fda.gov/Drugs/DrugSafety/ucm475463.htm Accessed February 16, 2016
- Farxiga® (Dapagliflozin) [prescribing information] Wilmington, DE AstraZeneca 2015
- Rosenstock J Ferrannini E Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors Diabetes Care 2015 38 9 1638 1642 26294774
- Westerberg DP Diabetic ketoacidosis: evaluation and treatment Am Fam Physician 2013 87 5 337 346 23547550
- Peters AL Buschur EO Buse JB Cohan P Diner JC Hirsch IB Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter 2 inhibition Diabetes Care 2015 38 9 1687 1693 26078479
- American Association of Clinical Endocrinologists AACE/ACE Scientific and Clinical Review: Association of SGLT2 Inhibitors and DKA 2015 Available from: http://resources.aace.com/in-the-news/aaceace-scientific-and-clinical-review-association-sglt2-inhibitors-and-dka Accessed January 11, 2016
- Curkendall SM Thomas N Bell KF Juneau PL Weiss AJ Predictors of medication adherence in patients with type 2 diabetes mellitus Curr Med Res Opin 2013 29 10 1275 1286 23815104
- Tiv M Viel JF Mauny F Medication adherence in type 2 diabetes: the ENTRED study 2007, a French Population-Based Study PLoS One 2012 7 3 e32412 22403654
- Zhu VJ Tu W Rosenman MB Overhage JM Nonadherence to oral antihyperglycemic agents: subsequent hospitalization and mortality among patients with type 2 diabetes in clinical practice Stud Health Technol Inform 2015 216 60 63 26262010
- Grandy S Langkilde AM Sugg JE Parikh S Sjostrom CD Health-related quality of life (EQ-5D) among type 2 diabetes mellitus patients treated with dapagliflozin over 2 years Int J Clin Pract 2014 68 4 486 494 24499168
- Grandy S Hashemi M Langkilde AM Parikh S Sjostrom CD Changes in weight loss-related quality of life among type 2 diabetes mellitus patients treated with dapagliflozin Diabetes Obes Metab 2014 16 7 645 650 24443876
- Selvin E Francis LM Ballantyne CM Nontraditional markers of glycemia: associations with microvascular conditions Diabetes Care 2011 34 4 960 967 21335368
