Abstract
Background
Diabetes mellitus is associated with a high risk of cardiovascular disease. Carotid intima-media thickness (CIMT) is increasingly used as a surrogate marker for atherosclerosis. Its use relies on its ability to predict future clinical cardiovascular end points.
Methods
This review examines the evidence linking CIMT as a surrogate marker of vascular complications in people with type 1 and type 2 diabetes. We have also reviewed the various treatment strategies which have been shown to influence CIMT.
Conclusions
CIMT measurement is an effective, noninvasive tool which can assist in identifying people with diabetes who are at higher risk of developing microvascular and macrovascular complications. It may also help to evaluate the effectiveness of various treatment strategies used to treat people with diabetes.
Cardiovascular disease in diabetes
Diabetes mellitus is associated with a high risk of cardiovascular disease (CVD) which is the most common cause of mortality in people with diabetes.Citation1,Citation2 CVD accounts for more than 80% of deaths in people with diabetes.Citation3,Citation4 A two- to fourfold increased risk of CVD in people with diabetes compared with the background population has been reported by various research groups.Citation5,Citation6
The risk of stroke is increased 150% to 400% in people with diabetes.Citation7–Citation9 In the Multiple Risk Factor Intervention Trial (MRFIT), people taking medications for diabetes were three times as likely to develop cerebrovascular disease compared with those not receiving medications for diabetes.Citation5 In type 1 diabetes, the prevalence of cerebrovascular disease has varied from 4% to 21% depending on the duration of diabetes and the population studiedCitation10–Citation13 and was found to confer an increased risk of stroke (odds ratio 11.6; 95% confidence interval [CI]: 1.2–115.2) in a study of 201 people younger than 55 years who developed a stroke due to cerebral infarction.Citation14
Diabetes is also associated with increased incidence and extent of peripheral arterial disease.Citation15 Thus, not only does atherosclerosis develop at a younger age in people with diabetes, it is also more diffuse and severe than that found in people without diabetes. People with diabetes have a two- to fourfold increased risk of peripheral arterial disease.Citation16
Ultrasonographic assessment of endothelial function of brachial artery flow-mediated dilatation and evaluation of carotid intima-media thickness (CIMT) have been used as a surrogate marker of CVD in people with diabetes.
Endothelial function and CVD
Endothelial dysfunction precedes the development of atherosclerosis and is believed to play a central role in its pathophysiology. Ludmer and colleagues first demonstrated impaired endothelial-dependent vasodilatation in the presence of atherosclerosis.Citation17 Endothelial dysfunction in the peripheral vessels are modestly correlated with the endothelial function in the coronary vessels.Citation18,Citation19
Flow-mediated dilatation in response to postocclusive reactive hyperemia has been used to noninvasively assess endothelial function in the peripheral vascular system.Citation20 Brachial flow-mediated dilation (FMD) has been found to be inversely associated with CIMT.Citation21–Citation23 In the Cardiovascular Risk in Young Finns Study, FMD and CIMT were measured in 2109 healthy people aged 20 to 39 years.Citation21 Individuals were classified into subgroups as those with impaired, intermediate, and enhanced FMD if the FMD was <10th percentile, between 10th to 90th percentile, and >90th percentile, respectively. The number of cardiovascular risk factors was correlated with increased CIMT in those individuals with impaired or intermediate FMD, but not in those with enhanced FMD, which suggests a crucial link between CIMT and endothelial dysfunction, with the latter appearing to be essential for cardiovascular risk factors to be able to contribute to atherosclerosis in the arterial wall.
CIMT
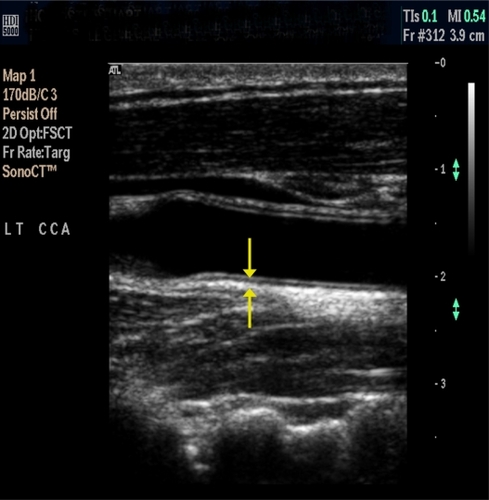
CIMT is the area of tissue starting at the luminal edge of the artery and ending at the boundary between the media and the adventitia ().Citation24 It is measured using B-mode ultrasound as the composite thickness of the intima and media. The ‘double-line pattern’ is thus the distance between the two echogenic lines that represent the lumen–intima interface and the media–adventitia interface. CIMT in healthy middle-aged adults measures 0.6 to 0.7 mm and greater than 1.20 mm is considered abnormal.Citation25 CIMT is age-dependent and increases at a rate of 0.005 to 0.010 mm/year.Citation26 Thus, in younger individuals, a CIMT of greater than 1.00 mm would be considered abnormal.Citation27
Figure 1 Carotid intima-media thickness measured at the far wall of the common carotid artery using the double-line pattern.
Iglesias del Sol and colleagues measured the CIMT at the common carotid, bifurcation, internal carotid, and combined CIMT and found that the area under the receiver operator characteristic (ROC) curves, as a predictor of coronary artery disease, for these segments were 0.67 (95% CI: 0.61–0.73), 0.69 (0.63–0.75), 0.67 (0.61–0.73), and 0.67 (0.61–0.73), respectively.Citation28 Thus the authors concluded that all the measurement sites had the same ability to predict future cardiovascular events.
Limitations of CIMT measurement
There is no standardized protocol for measurement of CIMT. This can result in inaccurate measurements of the progression or regression of CIMT during the follow up studies or in the assessment of any therapeutic interevention on the measured CIMT. Since the implementation of the edge detection software there has been improved reproducibility and reduced interobserever variation.Citation29
Different portions of the carotid artery have been used to measure the CIMT, common carotid, bifurcation, internal carotid, and combined CIMT which may influence the value of the measured CIMT. However in the study by Iglesias del Sol and colleagues CIMT was measured at the common carotid, bifurcation, internal carotid, and combined CIMT and they found that all the measurement sites had the same ability to predict future cardiovascular events.Citation28
Measurement of CIMT involves a combined measure of the intimal and medial layer of the arterial wall, whereas the atherosclerotic process is restricted in the intimal layer, particularly in its early phase of atherosclerosis. Furthermore, CIMT is only an indirect assessment of the possible atherosclerotic burden in the coronary artereries which is the commonest cause of cardiovascular death. In a systematic review, Bots and colleagues reviewed 34 studies on the relationship of CIMT to coronary atherosclerosis. Thirty of these studies showed a modest positive relationship, the magnitude of which was similar to that found in autopsy studies. The modest relationship between CIMT and coronary atherosclerosis most likely reflects variability in atherosclerosis development between the vascular beds rather than limitations of CIMT measurements.Citation30
Lastly, measured CIMT is not only a reflection of the atherosclerotic burden in the carotid arteies but also reflects age-related changes, and it is imperative that the age of an individual is taken into account when CIMT is measured.
CIMT – ultrasound vs histology
Ultrasonographic measurements of CIMT compared with histological measurements at the far-wall have been found to provide an accurate estimation of the IMT.Citation31–Citation33 Pignoli and colleagues compared pathological findings in vitro or in situ at autopsy with ultrasonographic measurement of intima-media thickness (IMT) of the aorta and the common carotid arteries.Citation34 The authors found an error of less than 20% for measurements in three-quarters of normal and pathological aortic walls. In addition, no significant difference was found between the ultrasonographic measurement in the common carotid arteries evaluated in vitro and that determined by this method in vivo in young subjects indicating that ultrasonography represents a useful approach for the measurement of IMT in human arteries in vivo.
CIMT and CVD
CIMT is a surrogate marker of atherosclerosis and provides a noninvasive method for the risk assessment of CVD.Citation35–Citation38 It is a strong predictor of future cardiovascular events and is associated with conventional markers of cardiovascular risk such as age, diabetes and serum cholesterol.Citation39,Citation40
CIMT is a well-established index of atherosclerosis that correlates with prevalent and incident coronary artery diseaseCitation41,Citation42 and stroke.Citation43,Citation44 Studies have shown a relationship between atherosclerosis in the carotid and coronary arteries.Citation45,Citation46 Furthermore, statistically significant correlations (range 0.3–0.5) between CIMT and coronary atherosclerosis, the latter based on a coronary angiogram, coronary calcium studies, or intravascular ultrasound, have been noted.Citation30,Citation47,Citation48
CIMT is associated with cardiovascular risk factorsCitation49 and both prevalent and incident coronary artery disease and stroke.Citation41,Citation44,Citation50,Citation51 Furthermore, the progression of CIMT is influenced by cardiovascular risk factors and is directly related to the risk of future cardiovascular events.Citation48,Citation52 CIMT has therefore become a valuable research tool in clinical trials in the assessment of therapeutic agents directed against atherosclerosis. Thus, on account of these characteristics, CIMT has been used as an intermediate end point to assess the therapeutic efficacy of various interventions in a number of clinical studies.Citation53
In a meta-analysis of 37197 individuals followed-up for a mean duration of 5.5 years, Lorenz and colleagues found that a 0.1 mm absolute difference in CIMT was associated with a relative risk of myocardial infarction of 1.15 (95% CI: 1.12–1.17) and a relative risk of stroke of 1.18 (95% CI: 1.16–1.21).Citation54
Studies have also demonstrated association between cardiovascular risk and increased CIMT in people with type 1 diabetes.Citation55–Citation57
In the recent Multi-Ethnic Study of Atherosclerosis (MESA), coronary artery calcium (CAC) scoring was compared to CIMT in predicting CVD incidence in 6698 individuals aged 45 to 84 years who were asymptomatic and free of CVD at baseline. The study found that compared with CIMT, CAC was more strongly associated with incident CVD in the overall population. In contrast, CIMT was found to be a modestly better predictor of stroke than CAC scoring, which could be perhaps the result of the difference between vascular territories targeted by the two measures.Citation58 Although the CAC estimation was a better predictor of incident CVD in this study, measurement of CAC has a major disadvantage of exposing people to ionizing radiation.
CIMT and cardiovascular risk factors
A number of risk factors have been associated with the development of atherosclerosis in the carotid arteries. The findings that the risk factors that predict CIMT are those that also predict coronary artery disease is concordant with the evidence that atherosclerosis is a diffuse disease.Citation59 These risk factors include increasing age,Citation60–Citation62 male sex,Citation63 smoking,Citation61–Citation64 blood pressure,Citation61–Citation64 measures of adiposity such as body mass index,Citation60,Citation65 waist-to-hip ratio,Citation66 sedentary lifestyle,Citation66 family history,Citation67 ethnicity,Citation68 and the presence of diabetes or glucose intolerance.Citation63,Citation64,Citation66 CIMT has also been reported to be associated with serum cholesterol,Citation60–Citation64 triglyceride levels,Citation60 high-density lipoprotein (HDL) cholesterol,Citation60–Citation64 low-density lipoprotein LDL cholesterol,Citation65 high-sensitivity C-reactive protein,Citation69 and asymmetric dimethylarginine.Citation70
A number of studies have evaluated the determinants of change in CIMT over time.Citation71 The Atherosclerosis Risk in Communities (ARIC) study among 15,792 individuals aged 45 to 64 years reported statistically significant associations of change in CIMT with baseline diabetes, current smoking, HDL cholesterol, pulse pressure, white blood cell count, and fibrinogen during the follow-up from 1987 to 1998.Citation72 Furthermore, significant associations were found between change in CIMT and change in LDL cholesterol, and serum triglyceride and with onset of diabetes and hypertension, during the follow-up. Data from the Rotterdam study among 3409 men and women aged ≥55 years, in which CIMT was measured twice 6.5 years apart, indicated that moderate to severe progression of CIMT (above the 60th and 90th percentile of CIMT, respectively) was related to age, body mass index, male sex, current smoking, systolic blood pressure, and the presence of hypertension.Citation73 Lipid levels, however, were not related to increased progression of CIMT. Recently, the Carotid Atherosclerosis Progression Study among 3383 men and women found that age, male sex, hypertension, presence of diabetes, and smoking were related to increased progression of internal CIMT over 3 years, whereas no relation was found for common CIMT.Citation74
These studies suggest that CIMT is increased in the presence of risk factors associated with CVD and furthermore, the progression of CIMT is associated with cardiovascular risk factors.
CIMT in people with type 1 diabetes
Several research groups have found an association between type 1 diabetes and CIMT.Citation55,Citation57,Citation75–Citation79 Yamasaki and colleagues evaluated CIMT to assess the carotid arteries in 105 young patients with type 1 diabetes, 529 patients with type 2 diabetes, and 104 nondiabetic healthy people subjects. People with type 1 diabetes had significantly higher CIMT than healthy controls, whereas people with noninsulin-dependent diabetes showed CIMT values equivalent to those in normal adults. They reported that on multiple regression analysis CIMT in insulin-dependent diabetes patients was positively related to the duration of diabetes as well as to age. No other possible risk factors, such as serum total cholesterol level, serum HDL cholesterol level, LDL cholesterol, serum triglycerides, serum lipoprotein(a) level, or systolic or diastolic blood pressure showed any significant correlations. However, non-HDL cholesterol, smoking, and systolic hypertension were independently responsible for increases in CIMT values of type 2 diabetes patients as well as age and duration of diabetes.Citation55 Larsen and colleagues reported higher CIMT values in people with type 1 diabetes. They also reported a significant association between the glycosylated hemoglobin (HbA1c) levels and CIMT (r 2 = 0.77; P < 0.0001 when adjusted for age) in women with type 1 diabetes, though no such correlation was seen in men. Among women, a significant association was also found between CIMT and the percentage of coronary vessel area stenosis, measured by intravascular ultrasound.Citation57 The Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group found that traditional cardiovascular risk factors including increasing age, smoking, and LDL cholesterol were related to CIMT.Citation80 In a further study, 40 people aged 11 to 30 years with duration of type 1 diabetes of 3 to 25 years compared with 40 healthy controls confirmed a higher CIMT in the cohort with diabetes (0.6 ± 0.1 vs 0.4 ± 0.1 mm; P < 0.001). CIMT was found to correlate with age (r = 0.76; P < 0.001), body mass index (r = 0.82; P < 0.001), duration of diabetes (r = 0.66; P < 0.001), systolic blood pressure (r = 0.82; P < 0.001), diastolic blood pressure (r = 0.83; P < 0.001), HbA1c (r = 0.40; P = 0.004) and HDL (r = −0.88; P < 0.001).Citation81
In an observational longitudinal study over a period of 2.5 years of 102 people with type 1 diabetes, CIMT increased by a mean of 0.033 mm per year.Citation82 Furthermore, CIMT was found to correlate with age (r = 0.34; P < 0.01), diabetes duration (r = 0.25; P < 0.05) and systolic blood pressure (r = 0.28; P < 0.05) at baseline. In addition, the maximum change in CIMT was observed in people who had hypertension and nephropathy. CIMT has been reported to be increased in children with type 1 diabetes compared with healthy controls.Citation83,Citation84 Atherogenic risk factors such as systolic blood pressure, duration of diabetes, and body weight were positively correlated with CIMT in children and adolescents with type 1 diabetes.Citation84
In type 1 diabetes, the increase in CIMT has been shown to start in childhood and adolescence by someCitation55,Citation75 but not all studies.Citation85,Citation86 In a recent study of young children with type 1 diabetes with modest glycemic control, Margeirsdottir and colleagues reported increased CIMT despite intensive insulin treatment.Citation86 In another study, Schwab and colleagues reported increased CIMT in the pediatric population (body mass index), markers of sustained inflammation, endothelial dysfunction, and fibrinolytic activity were increased in diabetic versus nondiabetic children, none of these measures being significant correlates of CIMT. The authors reported that that in well-controlled type 1 diabetes, systolic blood pressure may be of greater importance than dyslipidemia in early atherogenesis.Citation84
In a study of young people with type 1 diabetes without known macrovascular disease or microalbuminuria, CIMT was found to be increased by 25% (P < 0.001) in type 1 diabetes compared with healthy controls.Citation22
CIMT in people with impaired glucose tolerance and type 2 diabetes
People with impaired glucose tolerance (IGT) have been shown to have endothelial dysfunction and are at increased risk of CVD. CIMT has been observed to be increased in people who would subsequently develop diabetes.Citation87 Yamasaki and colleagues have reported that people with IGT had increased CIMT and there was no difference in CIMT among the people with IGT and age- and sex-matched people with type 2 diabetes.Citation88 In another study postchallenge glucose levels were strongly associated with CIMT in people at risk of diabetes or who were at the early stages of type 2 diabetes.Citation89 These studies suggest that people with IGT or at the early stages of type 2 diabetes are already at increased risk of CVD.
A review of 21 studies including 24,111 people with type 2 diabetes (n = 4019) and IGT (n = 1110) found that CIMT was higher in individuals with diabetes compared to the healthy controls. Compared with healthy controls, CIMT was increased in individuals with type 2 diabetes by 0.13 (95% CI: 0.12–0.14) mm and by 0.04 (95% CI: 0.01–0.07) mm in individuals with IGT.Citation90 Other research groups have found CIMT to be increased in type 2 diabetes.Citation91–Citation93 Furthermore, CIMT has been demonstrated to be higher in people with diabetes and macrovascular disease.Citation94 In a prospective study, Bernard and colleagues reported that CIMT provides a similar predictive value for coronary events compared with the Framingham score, and suggested that the combination of these two indexes would significantly improve risk prediction in these patients.Citation95
A study was conducted in 98 people with type 2 diabetes with no known CVD to ascertain the clinical usefulness of CIMT in identifying those individuals in whom the single-photon emission computed tomography myocardial perfusion imaging is abnormal.Citation96 An increased CIMT was found to be significantly related to the presence and extent of abnormal myocardial perfusion. In another study, the usefulness of CIMT in predicting the presence of coronary artery disease, as detected by noninvasive computed tomographic coronary angiography, in asymptomatic people with diabetes was investigated (n = 150, aged 50 ± 13 years, 83 men).Citation97 Mean CIMT increased from 0.58 ± 0.08 mm in those with normal coronary arteries (n = 59, 39%), to 0.67 ± 0.12 mm in those with nonobstructive atherosclerosis (n = 54, 36%) and 0.75 ± 0.12 mm in those with obstructive stenosis defined as a ≥50% narrowing of the luminal diameter (n = 36, 25%; P < 0.01). Furthermore, a cut-off value of 0.67 mm for CIMT predicted obstructive coronary atherosclerosis with a sensitivity of 85% and specificity of 72%.
CIMT has been shown to be a predictor of incidence and recurrence of stroke.Citation44,Citation98 Similarily, increased CIMT has been found to be associated with increased risk of ischemic stroke in people with type 2 diabetes.Citation99,Citation100 Increased CIMT and plaque score have been demonstrated to correlate with acute ischemic stroke in patients with type 2 diabetes.Citation99
Along with hyperglycemia, other metabolic factors associated with diabetes that are known to increase cardiovascular risk including obesity, insulin resistance, hypertension, hyperlipidemia, and increased inflammatory state have all been shown to contribute to progression of CIMT in people with diabetes.Citation98,Citation99,Citation101,Citation102 The Relationship between Insulin Sensitivity and Cardiovascular disease (RISC) study conducted in 1326 European nondiabetic healthy individuals aged 30 to 60 years measured CIMT and its associations with fasting insulin and insulin resistance by performing standard oral glucose tolerance tests and hyperinsulinemic euglycemic clamps.Citation103 CIMT was statistically significantly associated with fasting insulin in healthy people. In contrast, Kong and colleagues studied normotensive individuals with type 2 diabetes and found no association between CIMT and fasting insulin or insulin sensitivity as assessed with an insulin-modified frequently sampled intravenous glucose tolerance test.Citation104
Thus CIMT is increased in people with diabetes from a young age. The progression of CIMT is associated with the traditional risk factors of CVD such as hypertension and dyslipidemia.
CIMT and microvascular complications
CIMT has been shown to be increased in people with type 1 diabetes and retinopathy.Citation105,Citation106 In a cross-sectional study, the severity of retinopathy was found to be associated with CIMT (odds ratio per 0.1 mm CIMT 1.09 [95% CI: 1.01–1.17; P = 0.01]),Citation107 consistent with studies in people with type 2 diabetes.Citation108,Citation109 In a recent study, Vigili de Kreutzenberg and colleagues studied the association between diabetic retinopathy and CIMT in people with type 2 diabetes. The authors reported that retinopathy either alone or in combination with nephropathy, is independently associated with CIMT in people with type 2 diabetes, and the severity of microangiopathy correlates with severity of carotid atherosclerosis.Citation110 In another study of people with type 1 diabetes, the association between CIMT and microangiopathic complications including retinopathy or nephropathy was reported.Citation111
Effect of therapeutic interventions on CIMT in people with diabetes
Blood glucose lowering in type 1 and type 2 diabetes and CIMT
A 16-week intensive lifestyle modification program and subsequent monthly meetings during the 6-month study period in 58 people with type 2 diabetes was found to be associated with a significantly reduced mean CIMT progression after 6 months (−0.040 ± 0.136 vs +0.083 ± 0.167 mm; P = 0.007).Citation112 Furthermore, changes in HbA1c (r = 0.34; P = 0.028), fasting plasma glucose (r = 0.31; P = 0.045), and 2-hour postprandial plasma glucose (r = 0.37; P = 0.015) correlated with the mean CIMT change after adjustment for age and sex. Thus, in addition to improved blood glucose control, lifestyle measures have decreased progression of CIMT. Data analyses from 11 studies (n = 1578) in people with type 2 diabetes and IGT evaluated the effect of interventions on change in CIMT. The annual increase of CIMT was 0.034 mm/y (95% CI: 0.029–0.039) in people with type 2 diabetes without any specific interventions in which mean HbA1c was 7.86%. A significant close correlation of HbA1c with rate of CIMT change was found (r = 0.35; P = 0.01). Agents for lowering of blood glucose, platelet activation, or blood pressure significantly reduced the CIMT increase, independent of blood glucose control.Citation113
As part of the EDIC study, the long-term follow-up of the Diabetes Control and Complications Trial (DCCT), 1229 people with type 1 diabetes (intensive blood glucose lowering arm n = 618; conventional blood glucose lowering arm n = 611) underwent internal and common CIMT measurements in 1994 to 1996 and again in 1998 to 2000.Citation56 Although CIMT was not statistically significantly different between the people with diabetes and the healthy controls after 1 year of follow-up in the EDIC study,Citation114 CIMT was significantly greater in people with type 1 diabetes compared with the healthy controls after a follow-up of 6 years in the EDIC study.Citation56 Furthermore, the progression of CIMT in the common carotid artery was significantly less in the group that received intensive therapy than in the group that received conventional therapy during the DCCT (0.032 vs 0.046 mm; P = 0.01) after adjustment for other risk factors. Factors that were associated with progression of CIMT were age, the EDIC base-line systolic blood pressure, smoking, ratio of LDL to HDL cholesterol, urinary albumin excretion rate, and the mean HbA1c during the DCCT.
A Japanese study randomized individuals with type 2 diabetes without known macrovascular disease to pioglitazone with or without other oral glucose-lowering agents (n = 89) or other oral glucose-lowering agents excluding thiazolidenediones (n = 97), with treatment goal of HbA1c <6.5%. The authors found that pioglitazone induced regression of mean CIMT from 0.839 ± 0.1873 to 0.780 ± 0.1571 mm; P =0.002), although the between-group difference did not reach statistical significance.Citation115
The Pioglitazone in the Prevention of Diabetes (PIPOD) study assessed the effects of pioglitazone in Hispanic women with prior gestational diabetes mellitus who had previously completed the troglitazone in the Prevention of Diabetes (TRIPOD) study.Citation116–Citation118 Thirty-one women came to PIPOD from the troglitazone arm while 30 came from the placebo arm of TRIPOD. During the 3-year follow-up, the 31 women who came to PIPOD from the troglitazone arm of TRIPOD were found to have a lower progression of CIMT of 38% during pioglitazone treatment than during troglitazone treatment, although this was not statistically significant (0.0037 vs 0.0060 mm/year; P = 0.260). The progression of CIMT was 69% lower during pioglitazone treatment than it had been during placebo in the 30 women who came to PIPOD from the placebo arm of TRIPOD (0.0031 vs 0.0100 mm/year; P = 0.006). The authors concluded that pioglitazone slows progression of CIMT in women who had been on placebo in the TRIPOD study and maintained a low rate of progression in those who had previously been treated with troglitazone. The low CIMT progression during treatment with the thiazolidendiones was speculated to be due to PPAR-γ activation in the vasculature and change in proinflammatory and prothrombotic markers.Citation119,Citation120
A greater reduction in CIMT independent of improved glycemic control, after 12 and 24 weeks of pioglitazone treatment, compared to glimeperide in 173 people with type 2 diabetes has been reported.Citation121 These data were later confirmed by Mazzone and colleagues in 462 people with type 2 diabetes (mean age 60 years) during a 72-week study. The authors found that the mean change in CIMT was less with pioglitazone than with glimepiride (−0.001 mm vs +0.012 mm, respectively; difference −0.013 mm; P = 0.020).Citation122
In another study, pioglitazone, but not glibenclamide or voglibose, was found to reduce CIMT in people with type 2 diabetes and diabetic nephropathy at 6- and 12-month follow-up.Citation123
In the randomized, placebo-controlled, Study of Atherosclerosis with Ramipril and Rosiglitazone (STARR), the effect of ramipril and of rosiglitazone on CIMT in people with IGT or impaired fasting glucose (IFG) was investigated.Citation124 People with IGT and/or IFG but without CVD or diabetes (n = 1425) were randomized to ramipril 15 mg/day or its placebo and to rosiglitazone 8 mg/day or its placebo with a 2 × 2 factorial design. The annual change of the maximum CIMT and the mean common CIMT were measured after a median follow-up of 3 years. Rosiglitazone significantly reduced the mean CIMT (difference 0.0043 ± 0.0017 mm/y, P = 0.010) but not the maximum CIMT. In contrast, there was no statistically significant difference between the ramipril and placebo groups.
In another study, glibenclamide in combination with metformin was associated with reduced progression of CIMT (0.003 ± 0.048 mm) compared with glibenclamide alone (0.064 ± 0.045 mm) and gliclazide group (0.032 ± 0.036 mm) (P < 0.0001 and P = 0.043 respectively).Citation125 The annual progression of maximum CIMT in the gliclazide group (0.044 ± 0.106 mm) and the glibenclamide plus metformin group (0.041 ± 0.105 mm) was smaller than that of the glibenclamide group (0.114 ± 0.131 mm). Attenuation of the CIMT progression by metformin in people with type 2 diabetes has been confirmed by others.Citation126 Metformin has antithrombotic effects, modulates the generation of reactive oxygen species, and reduces systemic methylglyoxal concentration, all of which might contribute to the beneficial effect on CIMT.Citation127,Citation128
The Copenhagen Insulin and Metformin Therapy trial aims to assess the effect of an 18-month treatment with metformin versus placebo in combination with one of three insulin analog regimens, with CIMT being the primary outcome measured in 950 individuals with type 2 diabetes. The three insulin regimens compared are 1) insulin detemir before bedtime (n ∼315 patients), 2) biphasic insulin aspart 30 before dinner with the possibility to increase to 2 or 4 injections daily (n ∼ 315 patients), and 3) insulin aspart before the main meals (three times daily) and insulin detemir before bedtime (n ∼ 315 patients).Citation129
In the prospective, randomized, placebo-controlled, Study to Prevent Non-Insulin Dependent Diabetes Mellitus (STOP-NIDDM) trial, an α-glucosidase inhibitor, acarbose, delayed progression from IGT to overt type 2 diabetes and reduced cardiovascular events.Citation130 A subgroup analysis of the STOP-NIDDM study examined the efficacy of acarbose on progression of CIMT in people with IGT.Citation131 One hundred thirty-two individuals with IGT were randomized to placebo (n = 66) or acarbose (n = 66). After a mean follow-up of 3.9 years, significant reduction in the progression of CIMT was observed in the acarbose group versus placebo. CIMT increased by 0.02 ± 0.07 mm in the acarbose group versus 0.05 ± 0.06 mm in the placebo group (P = 0.027). The annual increase of CIMT was reduced by approximately 50% in the acarbose group versus placebo. CIMT progression was significantly related to acarbose intake on multiple linear regression analyses. As the primary effect of acarbose is on meal-time hyperglycemia, these data supported the importance of postprandial hyperglycemia.
A substudy was performed in 175 of 401 individuals with type 2 diabetes who had participated in an epidemiological study to assess the relationship between postprandial hyperglycemia and surrogate markers of atherosclerosis.Citation132 The effects of repaglinide (n = 88) and glyburide (n = 87) on CIMT were compared after 12 months. Although, HbA1c improved to a comparable extent in both groups (−0.9%), the postprandial glucose peak was lower in the repaglinide group (P < 0.010). CIMT regression, defined as a decrease of >0.020 mm, was noted in a greater proportion of people on repaglinide (52%) than on glyburide 18% (P < 0.010). Furthermore, the reduction in CIMT was associated with changes in postprandial but not fasting hyperglycemia. These data add to recent research, which suggests that postprandial hyperglycemic excursions may be more important than basal hyperglycemia in triggering atherosclerosis.
Antihypertensive agents and CIMT in people with diabetes
Post-hoc analyses of the association between antihypertensive treatment and CIMT in the Troglitazone Atherosclerosis Regression Trial (TART), which assessed CIMT progression in adults with insulin-treated type 2 diabetes, found that higher systolic blood pressure was associated with a higher CIMT progression rate (P = 0.03). Furthermore, anti-hypertensive treatment reduced this association in a duration-dependent manner (interaction P = 0.035).Citation133
Hosomi and colleagues did a prospective randomized clinical trial of 98 patients with type 2 diabetes who were randomized to either enalapril 10 mg/d (n = 48) or to a control group (n = 50) for 2 years.Citation134 The enalapril-treated group was found to have reduced annual thickening of the common carotid arteries by 0.01 ± 0.004 mm/y relative to the control group over the course of this study. These data concur with other data which showed that angiotensin-converting enzyme (ACE) inhibitors led to a reduction in myocardial infarction, stroke, cardiovascular death, total mortality, revascularization, and overt nephropathy.Citation135 Importantly, the D allele of the ACE gene has been shown to be an independent risk factor for coronary artery disease and with CIMT in individuals with type 2 diabetes.Citation136,Citation137
Lipid-lowering treatment and CIMT in people with diabetes
People with type 2 diabetes without prior cardiovascular events participated in the Stop Atherosclerosis in Native Diabetics Study (SANDS) trial and were randomized to a standard group (target LDL cholesterol ≤2.6 mmol/L; non-HDL cholesterol ≤3.4mmol/L; systolic blood pressure ≤130mmHg) and an aggressive group with tighter targets (target LDL cholesterol ≤ 1.8 mmol/L; non-HDL cholesterol ≤2.6 mmol/L; systolic blood pressure ≤115 mmHg), and were treated with statins alone or statins plus ezetimibe.Citation138 The CIMT changes in both aggressive subgroups were compared with changes in the standard subgroups (target LDL cholesterol ≤2.6 mmolL; non-HDL cholesterol ≤3.4 mmol/L; systolic blood pressure ≤130 mmHg). Within the aggressive group, mean CIMT at 36 months regressed from baseline similarly in the ezetimibe (−0.025 mm, range −0.05 to 0.003 mm) and nonezetimibe subgroups (−0.012 mm, range −0.03 to 0.008 mm) but progressed in the standard treatment arm (0.039 mm, range 0.02–0.06 mm; intergroup; P < 0.0001). The authors concluded that reducing LDL cholesterol to aggressive targets resulted in similar regression of CIMT in patients who attained equivalent LDL cholesterol reductions from a statin alone or statin plus ezetimibe. CIMT increased in those achieving standard targets.
The Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol 6: HDL and LDL Treatment Strategies in Atherosclerosis (ARBITER 6-HALTS) study found that niacin resulted in a significant regression of mean and maximal CIMT whereas there was no significant change in CIMT in the ezetimibe-treated subgroup.Citation139 Although not powered for clinical outcomes, there were more major cardiovascular events in the ezetimibe arm than in the niacin arm (9 events vs 2 events, respectively; P = 0.040).
Anti-platelet therapy and CIMT in people with diabetes
Kodama and colleagues followed up 150 people aged 52 to 76 years with type 2 diabetes and without known CVD whose baseline CIMT was >1.1 mm.Citation140 Antiplatelet agents (aspirin 81 mg/day, n = 40; ticlopidine 200 mg/day, n = 36; no drugs n = 74) were administered. Individuals without anti-platelet agents had an annual progression of CIMT of 0.067 mm/y. In contrast, low-dose aspirin or ticlopidine attenuated the progression of CIMT by 50% (0.033 mm and 0.034 mm/year, respectively).
More recently, the prospective, randomized, open-label, blinded Diabetic Atherosclerosis Prevention by Cilostazol (DAPC) study showed that in people with type 2 diabetes suspected of peripheral artery disease, a phosphodiesterase inhibitor, cilostazol (100–200 mg/day) caused greater regression in the maximum and mean CIMT compared with aspirin (81–100 mg/day) during a 2-year observation period (mean left CIMT −0.043 ± 0.182 vs 0.028 ± 0.202 mm; P = 0.004; mean right CIMT −0.024 ± 0.182 vs 0.048 ± 0.169 mm; P < 0.001).Citation141
Conclusions
Diabetes is associated with increased cardiovascular and cerebrovascular disease-related mortality. Early identification of people at higher risk can influence the treatment strategies to reduce the morbidity and mortality. CIMT measurement is a relatively easy, noninvasive technique to identify atherosclerosis. People with diabetes have higher CIMT than the healthy population. CIMT increases in the presence of micro- and macrovascular complications of diabetes. Several treatment strategies in diabetes which have been shown to reduce diabetic complications also cause regression of CIMT. Thus, routine measurement of CIMT may add value to risk stratification and facilitate better use of various treatment strategies in people with diabetes.
Assessment of CIMT provides an excellent opportunity to evaluate the atherosclerotic risk in people with diabetes and can further be used to facilitate better use of various treatment strategies in people with diabetes. Further randomized studies would be required to assess the role of CIMT in predicting the development of various complications and how various available treatment strategies could be incorporated to influence the outcome.
Disclosure
The authors report no conflicts of interest in this work.
References
- Abbott RD Donahue RP Kannel WB Wilson PW The impact of diabetes on survival following myocardial infarction in men vs women. The Framingham Study JAMA 1988 260 23 3456 3460 2974889
- Gu K Cowie CC Harris MI Mortality in adults with and without diabetes in a national cohort of the US population, 1971–1993 Diabetes Care 1998 21 7 1138 1145 9653609
- Savage PJ Cardiovascular complications of diabetes mellitus: what we know and what we need to know about their prevention Ann Intern Med 1996 124 1 Pt 2 123 126 8554203
- Webster MW Scott RS What cardiologists need to know about diabetes Lancet 1997 350 Suppl 1 SI23 SI28 9250280
- Stamler J Vaccaro O Neaton JD Wentworth D Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial Diabetes Care 1993 16 2 434 444 8432214
- Kannel WB McGee DL Diabetes and cardiovascular disease. The Framingham study JAMA 1979 241 19 2035 2038 430798
- Jamrozik K Broadhurst RJ Forbes S Hankey GJ Anderson CS Predictors of death and vascular events in the elderly: the Perth Community Stroke Study Stroke 2000 31 4 863 868 10753989
- Folsom AR Rasmussen ML Chambless LE Prospective associations of fasting insulin, body fat distribution, and diabetes with risk of ischemic stroke. The Atherosclerosis Risk in Communities (ARIC) Study Investigators Diabetes Care 1999 22 7 1077 1083 10388971
- Kuusisto J Mykkanen L Pyorala K Laakso M Non-insulin-dependent diabetes and its metabolic control are important predictors of stroke in elderly subjects Stroke 1994 25 6 1157 1164 8202973
- Donahue RP Orchard TJ Diabetes mellitus and macrovascular complications. An epidemiological perspective Diabetes Care 1992 15 9 1141 1155 1396012
- Maser RE Wolfson SKJr Ellis D Cardiovascular disease and arterial calcification in insulin-dependent diabetes mellitus: interrelations and risk factor profiles. Pittsburgh Epidemiology of Diabetes Complications Study-V Arterioscler Thromb 1991 11 4 958 965 2065046
- Orchard TJ Dorman JS Maser RE Prevalence of complications in IDDM by sex and duration. Pittsburgh Epidemiology of Diabetes Complications Study II Diabetes 1990 39 9 1116 1124 2384191
- Orchard TJ Dorman JS Maser RE Factors associated with avoidance of severe complications after 25 yr of IDDM. Pittsburgh Epidemiology of Diabetes Complications Study I Diabetes Care 1990 13 7 741 747 2387194
- You RX McNeil JJ O’Malley HM Davis SM Thrift AG Donnan GA Risk factors for stroke due to cerebral infarction in young adults Stroke 1997 28 10 1913 1918 9341695
- Jude EB Oyibo SO Chalmers N Boulton AJ Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome Diabetes Care 2001 24 8 1433 1437 11473082
- Newman AB Siscovick DS Manolio TA Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Heart Study (CHS) Collaborative Research Group Circulation 1993 88 3 837 845 8353913
- Ludmer PL Selwyn AP Shook TL Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries N Engl J Med 1986 315 17 1046 1051 3093861
- Anderson TJ Uehata A Gerhard MD Close relation of endothelial function in the human coronary and peripheral circulations J Am Coll Cardiol 1995 26 5 1235 1241 7594037
- Sorensen KE Kristensen IB Celermajer DS Atherosclerosis in the human brachial artery J Am Coll Cardiol 1997 29 2 318 322 9014983
- Celermajer DS Sorensen KE Gooch VM Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis Lancet 1992 340 8828 1111 1115 1359209
- Juonala M Viikari JS Laitinen T Interrelations between brachial endothelial function and carotid intima-media thickness in young adults: the cardiovascular risk in young Finns study Circulation 2004 110 18 2918 2923 15505080
- Sibal L Aldibbiat A Agarwal SC Circulating endothelial progenitor cells, endothelial function, carotid intima-media thickness and circulating markers of endothelial dysfunction in people with type 1 diabetes without macrovascular disease or microalbuminuria Diabetologia 2009 52 8 1464 1473 19484217
- Ravikumar R Deepa R Shanthirani C Mohan V Comparison of carotid intima-media thickness, arterial stiffness, and brachial artery flow mediated dilatation in diabetic and nondiabetic subjects (The Chennai Urban Population Study [CUPS-9]) Am J Cardiol 2002 90 7 702 707 12356381
- Touboul PJ Hennerici MG Meairs S Mannheim carotid intima-media thickness consensus (2004–2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006 Cerebrovasc Dis 2007 23 1 75 80 17108679
- Jacoby DS Mohler IE Rader DJ Noninvasive atherosclerosis imaging for predicting cardiovascular events and assessing therapeutic interventions Curr Atheroscler Rep 2004 6 1 20 26 14662104
- O’Leary DH Bots ML Imaging of atherosclerosis: carotid intima-media thickness Eur Heart J 2010 31 14 1682 1689 20542989
- Mukherjee D Yadav JS Carotid artery intimal-medial thickness: indicator of atherosclerotic burden and response to risk factor modification Am Heart J 2002 144 5 753 759 12422142
- Iglesias del Sol A Bots ML Grobbee DE Hofman A Witteman JC Carotid intima-media thickness at different sites: relation to incident myocardial infarction; The Rotterdam Study Eur Heart J 2002 23 12 934 940 12069447
- Gepner AD Korcarz CE Aeschlimann SE Validation of a carotid intima-media thickness border detection program for use in an office setting J Am Soc Echocardiogr 2006 19 2 223 228 16455429
- Bots ML Baldassarre D Simon A Carotid intima-media thickness and coronary atherosclerosis: weak or strong relations? Eur Heart J 2007 28 4 398 406 17277033
- Gamble G Beaumont B Smith H B-mode ultrasound images of the carotid artery wall: correlation of ultrasound with histological measurements Atherosclerosis 1993 102 2 163 173 8251002
- Graf S Gariepy J Massonneau M Experimental and clinical validation of arterial diameter waveform and intimal media thickness obtained from B-mode ultrasound image processing Ultrasound Med Biol 1999 25 9 1353 1363 10626622
- Wong M Edelstein J Wollman J Bond MG Ultrasonic-pathological comparison of the human arterial wall. Verification of intima-media thickness Arterioscler Thromb 1993 13 4 482 486 8466883
- Pignoli P Tremoli E Poli A Oreste P Paoletti R Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging Circulation 1986 74 6 1399 1406 3536154
- Grobbee DE Bots ML Carotid artery intima-media thickness as an indicator of generalized atherosclerosis J Intern Med 1994 236 5 567 573 7964435
- Yamakado M Fukuda I Kiyose H Ultrasonographically assessed carotid intima-media thickness and risk for asymptomatic cerebral infarction J Med Syst 1998 22 1 15 18 9554105
- Bots ML Dijk JM Oren A Grobbee DE Carotid intima-media thickness, arterial stiffness and risk of cardiovascular disease: current evidence J Hypertens 2002 20 12 2317 2325 12473847
- Oren A Vos LE Uiterwaal CS Grobbee DE Bots ML Cardiovascular risk factors and increased carotid intima-media thickness in healthy young adults: the Atherosclerosis Risk in Young Adults (ARYA) Study Arch Intern Med 2003 163 15 1787 1792 12912713
- Crouse JR3rd Tang R Espeland MA Terry JG Morgan T Mercuri M Associations of extracranial carotid atherosclerosis progression with coronary status and risk factors in patients with and without coronary artery disease Circulation 2002 106 16 2061 2066 12379574
- Espeland MA Craven TE Riley WA Corson J Romont A Furberg CD Reliability of longitudinal ultrasonographic measurements of carotid intimal-medial thicknesses. Asymptomatic Carotid Artery Progression Study Research Group Stroke 1996 27 3 480 485 8610317
- Bots ML Hoes AW Koudstaal PJ Hofman A Grobbee DE Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study Circulation 1997 96 5 1432 1437 9315528
- Burke GL Evans GW Riley WA Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study Stroke 1995 26 3 386 391 7886711
- Chambless LE Folsom AR Clegg LX Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study Am J Epidemiol 2000 151 5 478 487 10707916
- O’Leary DH Polak JF Kronmal RA Manolio TA Burke GL Wolfson SKJr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group N Engl J Med 1999 340 1 14 22 9878640
- Holme I Enger SC Helgeland A Risk factors and raised athero-sclerotic lesions in coronary and cerebral arteries. Statistical analysis from the Oslo study Arteriosclerosis 1981 1 4 250 256 7295196
- Mitchell JR Schwartz CJ Relationship between arterial disease in different sites. A study of the aorta and coronary, carotid, and iliac arteries Br Med J 1962 1 5288 1293 1301 14474632
- Craven TE Ryu JE Espeland MA Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study Circulation 1990 82 4 1230 1242 2205416
- Hodis HN Mack WJ LaBree L The role of carotid arterial intima-media thickness in predicting clinical coronary events Ann Intern Med 1998 128 4 262 269 9471928
- Dawson JD Sonka M Blecha MB Lin W Davis PH Risk factors associated with aortic and carotid intima-media thickness in adolescents and young adults: the Muscatine Offspring Study J Am Coll Cardiol 2009 53 24 2273 2279 19520251
- Lorenz MW von Kegler S Steinmetz H Markus HS Sitzer M Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS) Stroke 2006 37 1 87 92 16339465
- Cao JJ Arnold AM Manolio TA Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study Circulation 2007 116 1 32 38 17576871
- Johnson HM Douglas PS Srinivasan SR Predictors of carotid intima-media thickness progression in young adults: the Bogalusa Heart Study Stroke 2007 38 3 900 905 17272779
- Liu L Zhao F Yang Y The clinical significance of carotid intima-media thickness in cardiovascular diseases: a survey in Beijing J Hum Hypertens 2008 22 4 259 265 17960166
- Lorenz MW Markus HS Bots ML Rosvall M Sitzer M Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis Circulation 2007 115 4 459 467 17242284
- Yamasaki Y Kawamori R Matsushima H Atherosclerosis in carotid artery of young IDDM patients monitored by ultrasound high-resolution B-mode imaging Diabetes 1994 43 5 634 639 8168638
- Nathan DM Lachin J Cleary P Intensive diabetes therapy and carotid intima-media thickness in type 1 diabetes mellitus N Engl J Med 2003 348 23 2294 2303 12788993
- Larsen JR Brekke M Bergengen L Mean HbA1c over 18 years predicts carotid intima media thickness in women with type 1 diabetes Diabetologia 2005 48 4 776 779 15759107
- Folsom AR Kronmal RA Detrano RC Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med 2008 168 12 1333 1339 18574091
- Mancini GB Dahlof B Diez J Surrogate markers for cardiovascular disease: structural markers Circulation 2004 109 25 Suppl 1 IV22 IV30 15226248
- Davis PH Dawson JD Riley WA Lauer RM Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study Circulation 2001 104 23 2815 2819 11733400
- Bonithon-Kopp C Scarabin PY Taquet A Touboul PJ Malmejac A Guize L Risk factors for early carotid atherosclerosis in middle-aged French women Arterioscler Thromb 1991 11 4 966 972 2065047
- Ferrieres J Elias A Ruidavets JB Carotid intima-media thickness and coronary heart disease risk factors in a low-risk population J Hypertens 1999 17 6 743 748 10459870
- Mannami T Konishi M Baba S Nishi N Terao A Prevalence of asymptomatic carotid atherosclerotic lesions detected by high-resolution ultrasonography and its relation to cardiovascular risk factors in the general population of a Japanese city: the Suita study Stroke 1997 28 3 518 525 9056605
- Kuller L Borhani N Furberg C Prevalence of subclinical atherosclerosis and cardiovascular disease and association with risk factors in the Cardiovascular Health Study Am J Epidemiol 1994 139 12 1164 1179 8209875
- Li S Chen W Srinivasan SR Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study JAMA 2003 290 17 2271 2276 14600185
- Folsom AR Eckfeldt JH Weitzman S Relation of carotid artery wall thickness to diabetes mellitus, fasting glucose and insulin, body size, and physical activity. Atherosclerosis Risk in Communities (ARIC) Study Investigators Stroke 1994 25 1 66 73 8266385
- Bensen JT Li R Hutchinson RG Province MA Tyroler HA Family history of coronary heart disease and pre-clinical carotid artery atherosclerosis in African-Americans and whites: the ARIC study: Atherosclerosis Risk in Communities Genet Epidemiol 1999 16 2 165 178 10030399
- Li R Duncan BB Metcalf PA B-mode-detected carotid artery plaque in a general population. Atherosclerosis Risk in Communities (ARIC) Study Investigators Stroke 1994 25 12 2377 2383 7974576
- Wang TJ Nam BH Wilson PW Association of C-reactive protein with carotid atherosclerosis in men and women: the Framingham Heart Study Arterioscler Thromb Vasc Biol 2002 22 10 1662 1667 12377746
- Ayer JG Harmer JA Nakhla S HDL-cholesterol, blood pressure, and asymmetric dimethylarginine are significantly associated with arterial wall thickness in children Arterioscler Thromb Vasc Biol 2009 29 6 943 949 19359663
- Zureik M Touboul PJ Bonithon-Kopp C Cross-sectional and 4-year longitudinal associations between brachial pulse pressure and common carotid intima-media thickness in a general population. The EVA study Stroke 1999 30 3 550 555 10066851
- Chambless LE Folsom AR Davis V Risk factors for progression of common carotid atherosclerosis: the Atherosclerosis Risk in Communities Study, 1987–1998 Am J Epidemiol 2002 155 1 38 47 11772783
- Van der Meer IM Iglesias del Sol A Hak AE Bots ML Hofman A Witteman JC Risk factors for progression of atherosclerosis measured at multiple sites in the arterial tree: the Rotterdam Study Stroke 2003 34 10 2374 2379 12947155
- Mackinnon AD Jerrard-Dunne P Sitzer M Buehler A von Kegler S Markus HS Rates and determinants of site-specific progression of carotid artery intima-media thickness: the carotid atherosclerosis progression study Stroke 2004 35 9 2150 2154 15243147
- Jarvisalo MJ Putto-Laurila A Jartti L Carotid artery intima-media thickness in children with type 1 diabetes Diabetes 2002 51 2 493 498 11812760
- Frost D Beischer W Determinants of carotid artery wall thickening in young patients with Type 1 diabetes mellitus Diabet Med 1998 15 10 851 857 9796886
- Mohan V Ravikumar R Shanthi Rani S Deepa R Intimal medial thickness of the carotid artery in South Indian diabetic and non-diabetic subjects: the Chennai Urban Population Study (CUPS) Diabetologia 2000 43 4 494 499 10819244
- Peppa-Patrikiou M Scordili M Antoniou A Giannaki M Dracopoulou M Dacou-Voutetakis C Carotid atherosclerosis in adolescents and young adults with IDDM. Relation to urinary endothelin, albumin, free cortisol, and other factors Diabetes Care 1998 21 6 1004 1007 9614622
- Yokoyama H Yoshitake E Otani T Carotid atherosclerosis in young-aged IDDM associated with diabetic retinopathy and diastolic blood pressure Diabetes Res Clin Pract 1993 21 2–3 155 159 8269816
- Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group Effect of intensive diabetes treatment on carotid artery wall thickness in the epidemiology of diabetes interventions and complications Diabetes 1999 48 2 383 390 10334318
- Abdelghaffar S El Amir M El Hadidi A El Mougi F Carotid intima-media thickness: an index for subclinical atherosclerosis in type 1 diabetes J Trop Pediatr 2006 52 1 39 45 16000343
- Frost D Friedl A Beischer W Determinants of early carotid atherosclerosis progression in young patients with type 1 diabetes mellitus Exp Clin Endocrinol Diabetes 2002 110 2 92 94 11928073
- Rabago Rodriguez R Gomez-Diaz RA Tanus Haj J Carotid intima-media thickness in pediatric type 1 diabetic patients Diabetes Care 2007 30 10 2599 2602 17644614
- Schwab KO Doerfer J Krebs A Early atherosclerosis in childhood type 1 diabetes: role of raised systolic blood pressure in the absence of dyslipidaemia Eur J Pediatr 2007 166 6 541 548 17387514
- Singh TP Groehn H Kazmers A Vascular function and carotid intimal-medial thickness in children with insulin-dependent diabetes mellitus J Am Coll Cardiol 2003 41 4 661 665 12598080
- Margeirsdottir HD Stensaeth KH Larsen JR Brunborg C Dahl-Jorgensen K Early signs of atherosclerosis in diabetic children on intensive insulin treatment: a population-based study Diabetes Care 33 9 2043 2048 20530748
- Hunt KJ Williams K Rivera D Elevated carotid artery intima-media thickness levels in individuals who subsequently develop type 2 diabetes Arterioscler Thromb Vasc Biol 2003 23 10 1845 1850 12958039
- Yamasaki Y Kawamori R Matsushima H Asymptomatic hyperglycaemia is associated with increased intimal plus medial thickness of the carotid artery Diabetologia 1995 38 5 585 591 7489842
- Temelkova-Kurktschiev TS Koehler C Henkel E Leonhardt W Fuecker K Hanefeld M Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level Diabetes Care 2000 23 12 1830 1834 11128361
- Brohall G Oden A Fagerberg B Carotid artery intima-media thickness in patients with Type 2 diabetes mellitus and impaired glucose tolerance: a systematic review Diabet Med 2006 23 6 609 616 16759301
- Niskanen L Rauramaa R Miettinen H Haffner SM Mercuri M Uusitupa M Carotid artery intima-media thickness in elderly patients with NIDDM and in nondiabetic subjects Stroke 1996 27 11 1986 1992 8898803
- Temelkova-Kurktschiev TS Koehler C Leonhardt W Increased intimal-medial thickness in newly detected type 2 diabetes: risk factors Diabetes Care 1999 22 2 333 338 10333954
- Wagenknecht LE D’Agostino RBJr Haffner SM Savage PJ Rewers M Impaired glucose tolerance, type 2 diabetes, and carotid wall thickness: the Insulin Resistance Atherosclerosis Study Diabetes Care 1998 21 11 1812 1818 9802726
- Lee CD Folsom AR Pankow JS Brancati FL Cardiovascular events in diabetic and nondiabetic adults with or without history of myocardial infarction Circulation 2004 109 7 855 860 14757692
- Bernard S Serusclat A Targe F Incremental predictive value of carotid ultrasonography in the assessment of coronary risk in a cohort of asymptomatic type 2 diabetic subjects Diabetes Care 2005 28 5 1158 1162 15855582
- Djaberi R Schuijf JD Jukema JW Increased carotid intima-media thickness as a predictor of the presence and extent of abnormal myocardial perfusion in type 2 diabetes Diabetes Care 2010 33 2 372 374 19918012
- Djaberi R Schuijf JD de Koning EJ Usefulness of carotid intima-media thickness in patients with diabetes mellitus as a predictor of coronary artery disease Am J Cardiol 2009 104 8 1041 1046 19801021
- Li C Engstrom G Berglund G Janzon L Hedblad B Incidence of ischemic stroke in relation to asymptomatic carotid artery atherosclerosis in subjects with normal blood pressure. A prospective cohort study Cerebrovasc Dis 2008 26 3 297 303 18667810
- Lee EJ Kim HJ Bae JM Relevance of common carotid intima-media thickness and carotid plaque as risk factors for ischemic stroke in patients with type 2 diabetes mellitus AJNR Am J Neuroradiol 2007 28 5 916 919 17494669
- Matsumoto K Sera Y Nakamura H Ueki Y Miyake S Correlation between common carotid arterial wall thickness and ischemic stroke in patients with type 2 diabetes mellitus Metabolism 2002 51 2 244 247 11833056
- Davis TM Millns H Stratton IM Holman RR Turner RC Risk factors for stroke in type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS) 29 Arch Intern Med 1999 159 10 1097 1103 10335687
- Urbina EM Kimball TR McCoy CE Khoury PR Daniels SR Dolan LM Youth with obesity and obesity-related type 2 diabetes mellitus demonstrate abnormalities in carotid structure and function Circulation 2009 119 22 2913 2919 19470890
- De Rooij SR Dekker JM Kozakova M Fasting insulin has a stronger association with an adverse cardiometabolic risk profile than insulin resistance: the RISC study Eur J Endocrinol 2009 161 2 223 230 19439511
- Kong C Elatrozy T Anyaoku V Robinson S Richmond W Elkeles RS Insulin resistance, cardiovascular risk factors and ultrasonically measured early arterial disease in normotensive Type 2 diabetic subjects Diabetes Metab Res Rev 2000 16 6 448 453 11114104
- Distiller LA Joffe BI Melville V Welman T Distiller GB Carotid artery intima-media complex thickening in patients with relatively long-surviving type 1 diabetes mellitus J Diabetes Complications 2006 20 5 280 284 16949514
- Glowinska-Olszewska B Urban M Urban B Tolwinska J Szadkowska A The association of early atherosclerosis and retinopathy in adolescents with type 1 diabetes: preliminary report Acta Diabetol 2007 44 3 131 137 17721751
- Klein R Sharrett AR Klein BE The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes : the atherosclerosis risk in communities study Ophthalmology 2002 109 7 1225 1234 12093643
- Malecki MT Osmenda G Walus-Miarka M Retinopathy in type 2 diabetes mellitus is associated with increased intima-media thickness and endothelial dysfunction Eur J Clin Invest 2008 38 12 925 930 19021717
- Rema M Mohan V Deepa R Ravikumar R Association of carotid intima-media thickness and arterial stiffness with diabetic retinopathy: the Chennai Urban Rural Epidemiology Study (CURES-2) Diabetes Care 2004 27 8 1962 1967 15277424
- Vigili de Kreutzenberg S Coracina A Volpi A Microangiopathy is independently associated with presence, severity and composition of carotid atherosclerosis in type 2 diabetes Nutr Metab Cardiovasc Dis 2010 2 15 [Epub ahead of print].
- Gul K Ustun I Aydin Y Carotid intima-media thickness and its relations with the complications in patients with type 1 diabetes mellitus Anadolu Kardiyol Derg 10 1 52 58 20150006
- Kim SH Lee SJ Kang ES Effects of lifestyle modification on metabolic parameters and carotid intima-media thickness in patients with type 2 diabetes mellitus Metabolism 2006 55 8 1053 1059 16839841
- Yokoyama H Katakami N Yamasaki Y Recent advances of intervention to inhibit progression of carotid intima-media thickness in patients with type 2 diabetes mellitus Stroke 2006 37 9 2420 2427 16888250
- Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group Effect of intensive diabetes treatment on carotid artery wall thickness in the epidemiology of diabetes interventions and complications Diabetes 1999 48 2 383 390 10334318
- Yamasaki Y Katakami N Furukado S Long-Term Effects of Pioglitazone on Carotid Atherosclerosis in Japanese Patients with Type 2 Diabetes without a Recent History of Macrovascular Morbidity J Atheroscler Thromb 2010
- Xiang AH Peters RK Kjos SL Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes J Clin Endocrinol Metab 2005 90 4 1986 1991 15623809
- Azen SP Peters RK Berkowitz K Kjos S Xiang A Buchanan TA TRIPOD (TRoglitazone In the Prevention Of Diabetes): a randomized, placebo-controlled trial of troglitazone in women with prior gestational diabetes mellitus Control Clin Trials 1998 19 2 217 231 9551285
- Xiang AH Hodis HN Kawakubo M Effect of pioglitazone on progression of subclinical atherosclerosis in non-diabetic premenopausal Hispanic women with prior gestational diabetes Atherosclerosis 2008 199 1 207 214 18054942
- Hsueh WA Law RE PPARgamma and atherosclerosis: effects on cell growth and movement Arterioscler Thromb Vasc Biol 2001 21 12 1891 1895 11742860
- Kruszynska YT Yu JG Olefsky JM Sobel BE Effects of troglitazone on blood concentrations of plasminogen activator inhibitor 1 in patients with type 2 diabetes and in lean and obese normal subjects Diabetes 2000 49 4 633 639 10871202
- Langenfeld MR Forst T Hohberg C Pioglitazone decreases carotid intima-media thickness independently of glycemic control in patients with type 2 diabetes mellitus: results from a controlled randomized study Circulation 2005 111 19 2525 2531 15883215
- Mazzone T Meyer PM Feinstein SB Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial JAMA 2006 296 21 2572 2581 17101640
- Nakamura T Matsuda T Kawagoe Y Effect of pioglitazone on carotid intima-media thickness and arterial stiffness in type 2 diabetic nephropathy patients Metabolism 2004 53 10 1382 1386 15375799
- Lonn EM Gerstein HC Sheridan P Effect of ramipril and of rosiglitazone on carotid intima-media thickness in people with impaired glucose tolerance or impaired fasting glucose: STARR (STudy of Atherosclerosis with Ramipril and Rosiglitazone) J Am Coll Cardiol 2009 53 22 2028 2035 19477351
- Katakami N Yamasaki Y Hayaishi-Okano R Metformin or gliclazide, rather than glibenclamide, attenuate progression of carotid intima-media thickness in subjects with type 2 diabetes Diabetologia 2004 47 11 1906 1913 15565373
- Matsumoto K Sera Y Abe Y Tominaga T Yeki Y Miyake S Metformin attenuates progression of carotid arterial wall thickness in patients with type 2 diabetes Diabetes Res Clin Pract 2004 64 3 225 228 15126012
- Nagi DK Yudkin JS Effects of metformin on insulin resistance, risk factors for cardiovascular disease, and plasminogen activator inhibitor in NIDDM subjects. A study of two ethnic groups Diabetes Care 1993 16 4 621 629 8462390
- Bonnefont-Rousselot D Raji B Walrand S An intracellular modulation of free radical production could contribute to the beneficial effects of metformin towards oxidative stress Metabolism 2003 52 5 586 589 12759888
- Lundby Christensen L Almdal T Boesgaard T Study rationale and design of the CIMT trial: the Copenhagen Insulin and Metformin Therapy trial Diabetes Obes Metab 2009 11 4 315 322 19267709
- Chiasson JL Josse RG Gomis R Hanefeld M Karasik A Laakso M Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial Lancet 2002 359 9323 2072 2077 12086760
- Hanefeld M Chiasson JL Koehler C Henkel E Schaper F Temelkova-Kurktschiev T Acarbose slows progression of intima-media thickness of the carotid arteries in subjects with impaired glucose tolerance Stroke 2004 35 5 1073 1078 15073402
- Esposito K Giugliano D Nappo F Marfella R Regression of carotid atherosclerosis by control of postprandial hyperglycemia in type 2 diabetes mellitus Circulation 2004 110 2 214 219 15197140
- Zheng L Hodis HN Buchanan TA Li Y Mack WJ Effect of antihypertensive therapy on progression of carotid intima-media thickness in patients with type 2 diabetes mellitus Am J Cardiol 2007 99 7 956 960 17398191
- Hosomi N Mizushige K Ohyama H Angiotensin-converting enzyme inhibition with enalapril slows progressive intima-media thickening of the common carotid artery in patients with non-insulin-dependent diabetes mellitus Stroke 2001 32 7 1539 1545 11441198
- Heart Outcomes Prevention Evaluation Study Investigators Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy Lancet 2000 355 9200 253 259 10675071
- Hosoi M Nishizawa Y Kogawa K Angiotensin-converting enzyme gene polymorphism is associated with carotid arterial wall thickness in non-insulin-dependent diabetic patients Circulation 1996 94 4 704 707 8772691
- Ruiz J Blanche H Cohen N Insertion/deletion polymorphism of the angiotensin-converting enzyme gene is strongly associated with coronary heart disease in non-insulin-dependent diabetes mellitus Proc Natl Acad Sci U S A 1994 91 9 3662 3665 8170965
- Fleg JL Mete M Howard BV Effect of statins alone versus statins plus ezetimibe on carotid atherosclerosis in type 2 diabetes: the SANDS (Stop Atherosclerosis in Native Diabetics Study) trial J Am Coll Cardiol 2008 52 25 2198 2205 19095139
- Taylor AJ Villines TC Stanek EJ Extended-release niacin or ezetimibe and carotid intima-media thickness N Engl J Med 2009 361 22 2113 2122 19915217
- Kodama M Yamasaki Y Sakamoto K Antiplatelet drugs attenuate progression of carotid intima-media thickness in subjects with type 2 diabetes Thromb Res 2000 97 4 239 245 10674411
- Katakami N Kim YS Kawamori R Yamasaki Y The phosphodiesterase inhibitor cilostazol induces regression of carotid atherosclerosis in subjects with type 2 diabetes mellitus: principal results of the Diabetic Atherosclerosis Prevention by Cilostazol (DAPC) study: a randomized trial Circulation 2010 121 23 2584 2591 20516379