?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Multiple sclerosis (MS) is a disease that heavily affects postural control, predisposing patients to accidental falls and fall-related injuries, with a relevant burden on their families, health care systems and themselves. Clinical scales aimed to assess balance are easy to administer in daily clinical setting, but suffer from several limitations including their variable execution, subjective judgment in the scoring system, poor performance in identifying patients at higher risk of falls, and statistical concerns mainly related to distribution of their scores. Today we are able to objectively and reliably assess postural control not only with laboratory-grade standard force platform, but also with low-cost systems based on commercial devices that provide acceptable comparability to gold-standard equipment. The sensitivity of measurements derived from force platforms is such that we can detect balance abnormalities even in minimally impaired patients and predict the risk of future accidental falls accurately. By manipulating sensory inputs (dynamic posturography) or by adding a concurrent cognitive task (dual-task paradigm) to the standard postural assessment, we can unmask postural control deficit even in patients at first demyelinating event or in those with a radiologic isolated syndrome. Studies on neuroanatomical correlates support the multifactorial etiology of postural control deficit in MS, with the association with balance impairment being correlated with cerebellum, spinal cord, and highly ordered processing network according to different studies. Postural control deficit can be managed by means of rehabilitation, which is the most important way to improve balance in patients with MS, but there are also suggestions of a beneficial effect of some pharmacologic interventions. On the other hand, it would be useful to pay attention to some drugs that are currently used to manage other symptoms in daily clinical setting because they can further impair postural controls of patients with MS.
Introduction
Postural control can be defined as the ability to uphold the body’s center of gravity within the base of support while maintaining a specified posture, making a voluntary movement or reacting to an external disturbance.Citation1
Postural control strategies include either compensatory postural adjustments following an unpredicted disturbance or anticipatory postural adjustments that counteract any destabilizing consequences of voluntary movement or predicted disturbance.Citation2
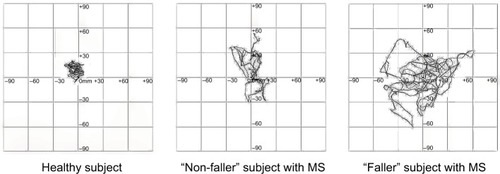
Postural responses cannot be considered as “reflex-like” automatic response, but rather balance control represents a complex task that is controlled by a combination of central and peripheral components including spinal reflexes, supraspinal commands, and the integration of afferent and/or efferent signals passing through the visual, vestibular and somatosensory systems, respectively, by the central nervous system (CNS).Citation3 Biometric factors, physiologic functions, cognitive processing, emotional status, visual feedback and cerebellar activity have shown to influence postural sway. Consequently, numerous disorders including injuries, aging or neurologic, otologic and orthopedic pathologies can adversely affect postural sway. Deficiency in any one of the mechanisms involved in postural control can produce detrimental effects on balance, causing a sense of instability, vulnerability, as well as predisposing to accidental falls and further injury.Citation4
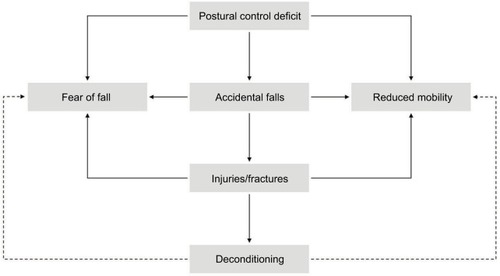
Multiple sclerosis (MS) is the most common cause of nontraumatic, progressive disability in young adults.Citation5 MS is both an inflammatory and neurodegenerative disease characterized by demyelination and several degrees of axonal loss of the brain and spinal cord.Citation6 By affecting the ability of neurons to communicate with each other effectively, MS can also be depicted as a “disconnection syndrome” leading to a variety of neurologic and neuropsychological deficit.Citation7 The deficient integration of neural pathways, due to the widespread and variable distribution of CNS damage in patients with MS, can also affect postural control and the ability to maintain adequate balance.Citation8 Postural control can even be impaired by MS-driven damage to peripheral organs providing sensory inputs to CNS or involved in motor output ().
Figure 1 Schematic of postural control and its alterations in MS.
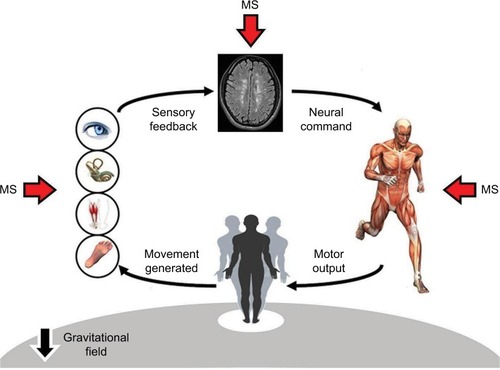
Indeed, impaired postural control is often observed in MS, with approximately two-thirds of these patients reporting lack of balance and coordination as the main symptom affecting their mobility in daily living.Citation9 Balance deficit reduces mobility and independence, leads to falls and injuries, and impacts upon overall quality of life.Citation10 Fatigue, muscle weakness and spasticity further contribute to compromise adequate balance and predispose patients to accidental falls ().Citation8,Citation11–Citation14
Accidental falls
Overall, frequency of accidental falls in people affected by MS is greater than in general population, as indirectly suggested by case–control studies documenting an approximately twofold increased risk of fall-related fractures and/or injuries in patients with MS compared with sex/age-matched individuals without MS ().Citation15–Citation20
Table 1 Case–control studies exploring the incidence of fall-related fractures and injuries in patients with multiple sclerosis
Observational studies conducted on young and middle-aged MS sample also showed that the proportion of fallers may range from 30% to 63% in a time frame of 1–12 months, with about 29%–45% being recurrent fallers.Citation14 These proportions are quite impressive if we consider that about 30% of community-dwelling healthy adults over 65 years fall in a 12-month period, and only 10% are recurrent fallers.Citation21 Furthermore, the number of accidental falls was collected retrospectively in most of these observational studies, thus leading to an underestimation of events occurred. In fact, although there is a good correlation (r=0.82) between prospective recording and retrospective self-reporting of accidental falls, retrospective data are prone to recall bias, mainly because only falls resulting in injury are more likely to be reported by patients.Citation22
Fall tendency may occur early in the course of the disease, even before walking and balance impairment become clinically evident and even after the first demyelinating event.Citation23 Near-falls (i.e., a trip or stumble) occur commonly, but are underreported by patients with MS, despite the fact that near-falls and accidental falls share similar circumstances surrounding fall events, such as transferring outside the home and tripping over an obstacle; however, accidental falls can happen even indoor, especially in the kitchen or bathroom.Citation24,Citation25
Factors that predispose patients with MS to accidental falls are a higher level of disability, a progressive disease course, the use of assistive devices for ambulation, a worse postural control and an impaired cognition.Citation13,Citation14,Citation26
Assessment of postural control
Evaluating the level of impairment in postural control is clinically relevant for several purposes, including early detection of subjects at risk of falling, understanding of underlying pathophysiology and objective documentation of therapeutic efficacy.
Balance deficit can be quantified by means of clinical scales and force platforms. Clinical scales to evaluate balance encompass physician-rated scales, stop-watch measures and even self-administered questionnaires. Although some clinical scales are easy and relatively quick to use, they are hampered by their variable execution and subjective judgment in the scoring system.Citation27,Citation28 Moreover, when used to predict patients at risk of falls, clinical scales have poor performance in discriminating between fallers and nonfallers, mainly due to their low sensitivity (i.e., performance in detecting fallers) and moderate–good specificity (i.e., performance in detecting nonfallers).Citation29 Other limits of clinical scales are their nonlinear distribution and floor or ceiling effect, especially when evaluating patients with subtle balance deficit (). Therefore, some authors suggest that, in clinical practice, multiple tests should be administered for accurately identifying fallers.Citation11 Alternatively, the Balance Evaluation Systems Test (BEST-est)Citation30 exhibits very good accuracy in predicting accidental falls (>90%),Citation31 but it is time-consuming and requires many tools for the assessment of six different aspects of human balance, namely biomechanical constraints, stability limits, postural responses, anticipatory postural adjustments, sensory orientation and stability in gait.Citation30 The use of a shorter version (mini-BESTest), with only a 10-minute administration time, could be more applicable to daily clinical setting.Citation32
Table 2 Clinical scales currently used to assess postural control and balance in multiple sclerosis
To overcome all the aforementioned limitations of clinical scales, there has been an increased interest about computer-based and objective instrumented measurements of balance. Posturography is an umbrella term that indicates all the techniques used to quantify postural control in upright stance, in either static or dynamic conditions, by means of a force platform.Citation33 Force platforms are instruments that measure ground reaction forces generated by a body standing on or moving across them, to quantify biomechanical parameters of human balance control. Static posturography refers to the measurement of postural sway of the body’s center of pressure (COP) during quiet standing on a fixed support surface, while dynamic posturography involves the use of induced balance perturbation, such as shifting the support surface, using an unstable support surface, moving the visual surround, applying stimuli to upper body parts or performing voluntary weight shift.Citation33
Static posturography provides objective measurements of postural control that have been shown to be not only highly reliable, but also valid in differentiating healthy controls from patients with MS.Citation34–Citation38 Furthermore, static standing balance measurements are more sensitive and accurate than a common clinical test (the Berg Balance Scale) in predicting accidental falls in MS.Citation35 This can be also displayed by the statokinesigram, that is, layout of a line connecting the successive positions of the body’s COP during a stop-watch recording ().
Figure 3 Statokinesigrams collected by one healthy volunteer, one patient who did not report any fall and one patient who reported three accidental falls within the last 3 months.
All posturographic techniques provide detailed and objective measurements of a wide range of time-domain or frequency-domain features of postural control, based on the sway of COP, that is, the point of application of the resultant from the vertical force’s action. These measurements consist of many different parameters, including (but not limited to) speed, range, root mean square distance, path, area and 95% confidence ellipse, and can be characterized on the anteroposterior or mediolateral axis or as the sum of the COP displacements.Citation33
However, while static posturography is performed in conditions that are somewhat away from those encountered in daily-life activities, dynamic posturography seems to be a more ecologic approach to investigate postural control. Dynamic posturography assessment provides data on the motor and sensory contribution to balance control by manipulating one or more specific inputs (visual, vestibular or proprioceptive) involved in postural control.Citation39 Moreover, these data can be combined into composite scores, such as the equilibrium score or the postural stability index.Citation40 However, it has been found that 13%–22% of patients with MS fell under the more difficult conditions of dynamic posturography, especially when forced to rely only on a single input.Citation41 Therefore, dynamic posturography seems to be less suitable than static posturography to assess postural control in patients with MS. Moreover, dynamic posturography requires an administration time longer than static posturography, and a more expensive and bulky equipment with respect to standard force platform.
Recently, low-cost force platforms using commercial devices have been proposed as a solution to overcome the aforementioned limitations of an expensive and bulky equipment. The commercial Wii balance board, an off-the-shelf accessory used for playing with Wii and Wii U video game consoles (Nintendo, Kyoto, Japan), contains load cells detecting body’s weight shifts. Although less accurate than standard force platforms because of their low-resolution measurements, low-cost systems based on Wii balance board can be useful in situations where lower accuracy and precision may be acceptable, as in daily clinical setting.Citation42–Citation44 While excellent test–retest reliability (>75%) was reported for Wii balance board-based low-cost systems, their agreement with standard force platform is at best adequate (40%–74%).Citation42 In fact, postural measurements obtained from Wii balance board are wider than those obtained from standard force platform, especially in conditions where there is lower performance variability (e.g., assessment of postural sway with eyes opened in subjects with mild disability). By contrast, Wii balance board performs more consistently with standard force platforms where there is higher performance variability (e.g., assessment of postural sway with eyes closed in subjects with greater disability). All these considerations imply that, from a clinical standpoint, low-cost systems can be effectively used in longitudinal study to test relative change in the same individual, while they are not recommendable to test absolute difference across individuals in cross-sectional study. Therefore, the clear advantage of these low-cost systems, representing a time-/space-/money-saving alternative to bulky and expensive laboratory-grade force platform, should be balanced with their disadvantages of a lower accuracy and worse signal-to-noise ratio.
Postural control can be reliably assessed also by the visual perception computing systems enabled with the Kinect camera, a motion-sensing input device developed for playing video games running on Xbox 360, Xbox One and Windows-equipped personal computers (Microsoft, Redmond, WA, USA). The Kinect system contains an RGB color Video Graphic Accelerator camera and an infrared depth sensor that work together to detect body motion and to display a real-time physical image. Other than as a surrogate for static posturography assessment,Citation45 the Kinect has also been used as a surrogate for gait analysis in MS populations.Citation46–Citation48
Cognitive-posture interference
Patients with MS often exhibit deficits in both postural control and cognitive functions, and there is emerging evidence that a postural task and a cognitive task may interfere with each other when performed simultaneously,Citation49 raising the hypothesis of an overlap between network subserving the postural control and some cognitive functions.Citation50,Citation51 This phenomenon is generally defined as cognitive-motor interference and, in the specific case of balance, is called cognitive-posture interference.Citation52
Cognitive-posture interference can be purposely investigated by means of dual-task paradigm experiments, that is, a study procedure that requires an individual to perform two tasks simultaneously.Citation53 Ideally, a dual-task experiment should assess a cognitive task and a motor task without any mutual interference (single-task condition) and while performed concurrently (dual-task condition). This framework allows the estimation of the so-called dual-task cost, that is, the percentage change from single-task to dual-task condition, for the cognitive and the motor task.Citation54
To better elucidate the relationship between the cognitive task and the motor task in dual-task situations, Plummer and EskesCitation54 proposed a graphical representation of the cognitive-motor interference patterns. This can be applied also to cognitive-postural interference phenomenon, by calculating the dual-task cost of balance and cognition according to the following formulas:
where DTC is dual-task cost, DT is dual-task, and ST is single-task.
Afterwards, the two dual-task costs, that of cognition and that of balance, can be plotted against each other to identify a specific pattern among nine possible patterns: mutual interference or facilitation, balance interference or facilitation, cognitive interference or facilitation, balance-priority or cognitive-priority tradeoff, and no interference (). Worthy of note, no literature data and specific rules are currently available to define the boundaries of the no-interference area.Citation54
Figure 4 Patterns of cognitive-postural interference based on the reciprocal DTC of balance and cognition.
Abbreviation: DTC, dual-task cost.
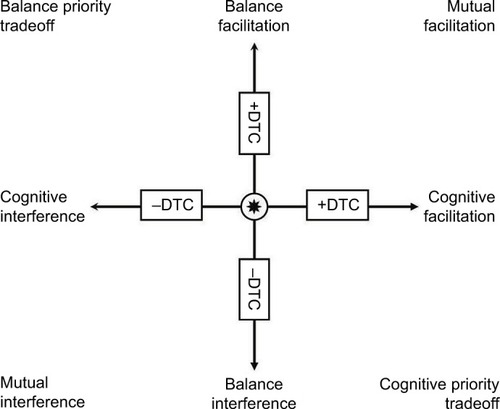
Dual-task studies aimed at exploring the cognitive-postural interference phenomenon in MS populations were mainly based on static posturography assessment while performing a concomitant cognitive test. Most of these studies suggested a predominant pattern of balance interference, that is, the dual-task condition causes deterioration of postural control.Citation49
However, the reciprocal effect of dual-tasking on the cognitive and a static balance task is not always explored in the literature, with the changes of cognitive performance during balance testing being reported only rarely. Another unsolved issue is which concurrent cognitive task has the most detrimental effect on postural control in patients with MS. Recently, it has been reported that cognitive task exploring executive functions are the most suitable to unmask the cognitive-posture interference phenomenon, but these data require further confirmation.Citation50
The clear advantage of dual-task paradigms is that they increase efficiently the sensitivity of a clinical test by exacerbating existing subtle deficits. Deterioration in balance when performed in conjunction with a concurrent cognitive task has been described indeed not only at the latest stage of MS, but also in patients without any overt cognitive deficit and even in subjects at the first demyelinating event or radiologically isolated syndrome, that is, asymptomatic subjects with neuroimaging findings suggestive of demyelinating disease.Citation50,Citation55,Citation56 Several detrimental consequences of cognitive-postural interference have been reported in patients with MS, including an increased risk of accidental falls, a higher level of fatigue and a reduced quality of life, especially in terms of social function and physical role perception.Citation57–Citation60 Nonetheless, the clinical relevance of this phenomenon in MS populations needs to be investigated more deeply.
Neuroanatomical correlates of postural control deficit
The deficit of postural control observed in patients with MS, who have a widespread, variable and sometimes extensive damage into CNS, may be due to multifactorial causes that differ from person to person. Therefore, postural balance deficit has been generally interpreted as a result of an impaired central integration of visual, vestibular and somatosensory inputs.Citation61 However, it is also possible that damage in specific locations of CNS is the primary contributor to MS-related balance deficit, as suggested by magnetic resonance imaging (MRI) studies.
One preliminary study found that the presence of a greater lesion volume (as seen on T2-weighted images) at brainstem level might be considered as a risk factor for multiple accidental falls (collected in a time frame of 6 months), regardless of the patient’s disability level.Citation62
Both slowed afferent proprioceptive conduction along demyelinated dorsal columns of spinal cord and damage of proprioceptive neural pathways originating from right brain hemisphere have been proposed as important causes of impaired postural control.Citation63–Citation65 Another hypothesis proposes the damage of cerebellar connections as the primary contributor to the balance impairmentCitation66 or, more extensively, the focal and diffuse involvement of the cerebellum, its connections, and other associative regions.Citation67
The severity of balance impairment has been shown to be related with both damage along specific white matter tracts – including cerebellar peduncles, pons, thalamus and some supratentorial associative bundles – and regional atrophy of anterior lobules of the cerebellum (IV, V, VI) and lobule VIII. The remarkable disparity between the widespread abnormalities in white matter tracts and the selective grey matter damage of the cerebellum also suggests that postural control deficit is caused by a cerebellar atrophy secondary to disconnection from the cerebral cortex and the spinal cord.Citation67
Clinically relevant association between impaired postural sway and damage of cerebellar connections has been demonstrated not only with conventional and nonconventional structural MRI, but also with resting-state functional MRI techniques. Compared to healthy subjects, patients with MS exhibit abnormalities of cortico-cerebellar circuits, with decreased connectivity in caudate nuclei and thalami, and increased connectivity in the cerebellum, pons, left amygdala and orbitofrontal cortices. In particular, decreased connectivity between dentate nuclei of cerebellum and the left caudate nucleus has been related with worse postural control.Citation68 This altered connectivity within the cerebellar network suggests a compensatory mechanism leading to an adaptive role in maintaining an adequate balance, as also supported by a recent study showing an association between better postural control and greater connectivity within a specific area of the anterior lobe of cerebellum belonging to the leg motor network.Citation69
However, networks involved in postural control regulation can be different in diverse situations. Consequently, damage at different levels of CNS can result in different types of balance deficit. When all sensory inputs (visual, proprioceptive and vestibular) are available, the resulting balance deficit is related mainly to cerebellum atrophy and demyelinating lesions along cerebellar connections, while spinal cord atrophy and demyelinating lesions in brainstem are the principal contributors of a worse postural control when the visual input is lacking.Citation70
The severity of cognitive-posture interference due to MS has been related with a higher probability of detecting demyelinating lesions in distinct anatomical regions – namely the superior and anterior radiate – bilaterally.Citation51 Therefore, it is possible that disconnection of brain circuitry between cerebellum, thalami, striatum and prefrontal areas – connected through the anterior and superior corona radiate – can impair the higher-level postural control required to maintain an adequate balance in dual-task situations.Citation71
Interventions to improve postural control
Rehabilitation is currently the cornerstone for managing and improving postural control in patients with MS. There are a lot of strategies that have been proposed, including proprioceptive training, motor and sensory training, endurance training, step training, Pilates exercises, whole-body vibration, hippotherapy (equine-assisted therapy), balance-based torso weighting, Tai-Chi Chuan, vestibular rehabilitation, robot-assisted gait training, virtual reality and exergames. A recently published meta-analysis specifically addressing this topic revealed that gait and balance functional training interventions yielded the greatest effect on postural control, and showed that higher-intensity programs maximized effectiveness.Citation72 Overall, these rehabilitative interventions promoted only a small decrease in fall risk, thus suggesting also that the magnitude of the improvements achieved was not sufficient to influence fall outcomes.Citation72 However, the use of fall event as outcome measures is affected by several methodologic concerns, as discussed earlier (see also “Accidental falls” section).Citation22 Furthermore, published studies suffer from a number of limitations that represent an avenue for future investigation, including small sample sizes, few data on long-term effect and retention of training-induced improvement, lack of standardized postural control outcomes, wide variability in terms of schedule, duration, frequency and intensity of rehabilitative interventions.
Postural control impairment cannot be effectively managed with pharmacologic interventions, because there is not yet any medication with indication for improving balance. Furthermore, some drugs that are broadly used in neurologic setting may even worsen gait and balance of patients with MS, including antidepressants (selective serotonin reuptake inhibitor and serotonin and norepinephrine reuptake inhibitor), centrally acting muscle relaxants, genitourinary medications and sex hormones ().Citation73,Citation74 If there is also a dose-dependent effect of the aforementioned classes of medications on the risk of accidental falls is still controversial.Citation22,Citation75,Citation76
Table 3 List of medications potentially affecting postural control in multiple sclerosis
The potential effect of cannabinoids and its derivatives on postural control is still unclear. There are few case reports showing clinical improvement of motor coordination in patients with MS affected by ataxia.Citation77,Citation78 By contrast, it has also been reported that cannabis smoking further impairs posture and balance in patients with MSCitation79 and, more recently, a large multicenter, postmarketing experience in Italy showed that drowsiness and dizziness are two relevant reasons for premature discontinuation of nabiximols, a plant-derived δ-9-tetrahydrocannabinol-cannabidiol oromucosal spray medicine for add-on treatment of refractory MS-related spasticity.Citation80 Furthermore, an independent study conducted on a small sample of patients with MS (n=22) has suggested a detrimental effect of nabiximols on postural control (detected at static posturography), especially in dual-task condition.Citation81
Short-term improvement of postural control has been reported with prolonged-release oral dalfampridine, a voltage-gated potassium-channel blocker able to improve action potential conduction in demyelinated axons that was specifically licensed to improve walking in patients with MS.Citation82,Citation83 More specifically, the beneficial effect of dalfampridine on balance might be mediated by an enhanced inhibitory drive and precision of pacemaking of cerebellar Purkinje cells.Citation84
A potential efficacy of riluzole as symptomatic therapy in different forms of cerebellar ataxia, including two patients with MS, has been suggested in a double-blind randomized clinical trial.Citation85 By opening small-conductance calcium-activated potassium channels, riluzole might reduce hyperexcitability of the neurons in the deep cerebellar nuclei that receive altered inhibitory input from Purkinje cells.Citation86
Finally, the suggestive theory that dopamine agonists can reduce cognitive-posture interference has been recently raised,Citation87 under the hypothesis that disconnection of CNS areas innervated by dopaminergic neurons (striatum and prefrontal cortex) is responsible for an increased dual-task cost of balance in patients with MS.Citation51,Citation88 However, to our knowledge, there are no data available to support the use of dopamine-agonist therapy in the MS setting.
Conclusion
Postural control is impaired early in the MS course, even in patients with minimal or no disability. Balance problems result in accidental falls and reduced mobility, negatively affecting quality of life and daily living activity.
Impaired postural control has multifactorial causes in MS, given the variable and extensive damage to the CNS. The role of rehabilitation in improving postural control deficit and, to a lesser extent, in reducing the risk of accidental falls is well established. At the moment there is no pharmacologic intervention specifically indicated for balance problems, but there are promising data favoring drugs that modulate neural transmission at cerebellar and prefrontal network level.
Acknowledgments
The authors wish to thank Ms. Eleonora Boni for the English language assistance.
Disclosure
LP received consulting fees, and/or lecture fees, and/or travel grants from Almirall, Biogen, Genzyme, Merck Serono, Novartis, Roche and Teva. LC received consulting fees and travel grants from Almirall. The authors report no other conflicts of interest in this work.
References
- PollockASDurwardBRRowePJPaulJPWhat is balance?Clin Rehabil200014440240610945424
- MassionJPostural control systems in developmental perspectiveNeurosci Biobehav Rev19982244654729595556
- MarsdenCDMertonPAMortonHBHuman postural responsesBrain J Neurol19811043513534
- FasanoAPlotnikMBoveFBerardelliAThe neurobiology of fallsNeurol Sci20123361215122322673818
- CompstonAColesAMultiple sclerosisLancet Lond Engl2008372964815021517
- MatthewsPMRoncaroliFWaldmanAA practical review of the neuropathology and neuroimaging of multiple sclerosisPract Neurol201616427928727009310
- DineenRAVilisaarJHlinkaJDisconnection as a mechanism for cognitive dysfunction in multiple sclerosisBrain J Neurol2009132Pt 1239249
- CameronMHLordSPostural control in multiple sclerosis: implications for fall preventionCurr Neurol Neurosci Rep201010540741220567946
- Van AschPImpact of mobility impairment in multiple sclerosis 2–patients’ perspectivesEur Neurol Rev20116115120
- PetersonEWChoCCFinlaysonMLFear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosisMult Scler20071391168117517881391
- NilsagårdYDenisonEGunnarssonL-GBoströmKFactors perceived as being related to accidental falls by persons with multiple sclerosisDisabil Rehabil200931161301131019479575
- FinlaysonMLPetersonEWChoCCRisk factors for falling among people aged 45 to 90 years with multiple sclerosisArch Phys Med Rehabil200687912741279 quiz 128716935067
- GunnHJNewellPHaasBMarsdenJFFreemanJAIdentification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysisPhys Ther201393450451323237970
- GiannìCProsperiniLJonsdottirJCattaneoDA systematic review of factors associated with accidental falls in people with multiple sclerosis: a meta-analytic approachClin Rehabil201428770471624569653
- BazelierMTvan StaaTUitdehaagBMThe risk of fracture in patients with multiple sclerosis: the UK general practice research databaseJ Bone Miner Res20112692271227921557309
- CameronMHPoelAJHaselkornJKLinkeABourdetteDFalls requiring medical attention among veterans with multiple sclerosis: a cohort studyJ Rehabil Res Dev2011481132021328159
- BazelierMTvan StaaTPUitdehaagBMRisk of fractures in patients with multiple sclerosis: a population-based cohort studyNeurology201278241967197322592374
- BazelierMTBentzenJVestergaardPThe risk of fracture in incident multiple sclerosis patients: the Danish National Health RegistersMult Scler201218111609161622472998
- RamagopalanSVSeminogOGoldacreRGoldacreMJRisk of fractures in patients with multiple sclerosis: record-linkage studyBMC Neurol20121213523126555
- BhattacharyaRKVaishnavNDubinskyRMIs there an increased risk of hip fracture in multiple sclerosis? Analysis of the Nationwide Inpatient SampleJ Multidiscip Healthc2014711912224600232
- GillespieLDRobertsonMCGillespieWJInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20092CD00714619370674
- NilsagårdYLundholmCDenisonEGunnarssonL-GPredicting accidental falls in people with multiple sclerosis–a longitudinal studyClin Rehabil200923325926919218300
- MoenSMCeliusEGNordslettenLHolmøyTFractures and falls in patients with newly diagnosed clinically isolated syndrome and multiple sclerosisActa Neurol Scand Suppl2011191798221711261
- CarlingAForsbergANilsagårdYFalls in people with multiple sclerosis: experiences of 115 fall situationsClin Rehabil Epub201791
- FritzNEEloyanABaynesMDistinguishing among multiple sclerosis fallers, near-fallers and non-fallersMult Scler Relat Disord2017199910429182996
- D’OrioVLFoleyFWArmentanoFCognitive and motor functioning in patients with multiple sclerosis: neuropsychological predictors of walking speed and fallsJ Neurol Sci20123161–2424622353853
- ManciniMHorakFBThe relevance of clinical balance assessment tools to differentiate balance deficitsEur J Phys Rehabil Med201046223924820485226
- ProsperiniLPozzilliCThe clinical relevance of force platform measures in multiple sclerosis: a reviewMult Scler Int2013201375656423766910
- CattaneoDRegolaAMeottiMValidity of six balance disorders scales in persons with multiple sclerosisDisabil Rehabil2006281278979516754576
- HorakFBWrisleyDMFrankJThe Balance Evaluation Systems Test (BESTest) to differentiate balance deficitsPhys Ther200989548449819329772
- JacobsJVKasserSLBalance impairment in people with multiple sclerosis: preliminary evidence for the Balance Evaluation Systems TestGait Posture201236341441822525422
- RossEPurtillHUszynskiMCohort study comparing the Berg balance scale and the mini-BESTest in people who have multiple sclerosis and are ambulatoryPhys Ther20169691448145526916925
- VisserJECarpenterMGvan der KooijHBloemBRThe clinical utility of posturographyClin Neurophysiol2008119112424243618789756
- SosnoffJJSocieMJBoesMKMobility, balance and falls in persons with multiple sclerosisPLoS One2011611e2802122132196
- ProsperiniLFortunaDGiannìCLeonardiLPozzilliCThe diagnostic accuracy of static posturography in predicting accidental falls in people with multiple sclerosisNeurorehabil Neural Repair2013271455222593115
- KalronAAchironAPostural control, falls and fear of falling in people with multiple sclerosis without mobility aidsJ Neurol Sci20133351–218619024095270
- WajdaDAMotlRWSosnoffJJThree-month test-retest reliability of center of pressure motion during standing balance in individuals with multiple sclerosisInt J MS Care2016182596227134578
- Reguera-GarcíaMMde Souza-TeixeiraFFernándezJA de PTest-retest reliability of static postural control in people with multiple sclerosisJ Phys Ther Sci20172981399140428878471
- NashnerLMShupertCLHorakFBBlackFOOrganization of posture controls: an analysis of sensory and mechanical constraintsProg Brain Res198980411418 discussion 395–3972699375
- ChaudhryHFindleyTQuigleyKSMeasures of postural stabilityJ Rehabil Res Dev200441571372015558401
- CattaneoDJonsdottirJSensory impairments in quiet standing in subjects with multiple sclerosisMult Scler2009151596718845654
- CastelliLStocchiLPatrignaniMSellittoGGiulianiMProsperiniLWe-Measure: toward a low-cost portable posturography for patients with multiple sclerosis using the commercial Wii balance boardJ Neurol Sci20153591–244044426490321
- SeveriniGStraudiSPavarelliCUse of Nintendo Wii Balance Board for posturographic analysis of Multiple Sclerosis patients with minimal balance impairmentJ Neuroeng Rehabil20171411928284217
- KeunePMYoungWRParaskevopoulosITMeasuring standing balance in multiple sclerosis: further progress towards an automatic and reliable method in clinical practiceJ Neurol Sci201737915716228716231
- BehrensJRMertensSKrügerTValidity of visual perceptive computing for static posturography in patients with multiple sclerosisMult Scler201622121596160626814201
- NewlandPWagnerJMSalterAExploring the feasibility and acceptability of sensor monitoring of gait and falls in the homes of persons with multiple sclerosisGait Posture20164927728227474948
- OtteKKayserBMansow-ModelSThomasFPSkubicMRantzMAccuracy and reliability of the kinect version 2 for clinical measurement of motor functionPLoS One20161111e016653227861541
- GholamiFTrojanDAKovecsesJHaddadWMGholamiBA microsoft kinect-based point-of-care gait assessment framework for multiple sclerosis patientsIEEE J Biomed Health Inform20172151376138527455529
- WajdaDASosnoffJJCognitive-motor interference in multiple sclerosis: a systematic review of evidence, correlates, and consequencesBioMed Res Int2015201572085625839039
- ProsperiniLCastelliLDe LucaFFabianoFFerranteIDe GiglioLTask-dependent deterioration of balance underpinning cognitive-postural interference in MSNeurology201687111085109227521436
- RuggieriSFanelliFCastelliLPetsasNDe GiglioLProsperiniLLesion symptom map of cognitive-postural interference in multiple sclerosisMult Scler Epub201731
- LeoneCPattiFFeysPMeasuring the cost of cognitive-motor dual tasking during walking in multiple sclerosisMult Scler201521212313125178543
- Della SalaSBaddeleyAPapagnoCSpinnlerHDual-task paradigm: a means to examine the central executiveAnn NY Acad Sci19957691611718595023
- PlummerPEskesGMeasuring treatment effects on dual-task performance: a framework for research and clinical practiceFront Hum Neurosci2015922525972801
- KalronADvirZAchironAEffect of a cognitive task on postural control in patients with a clinically isolated syndrome suggestive of multiple sclerosisEur J Phys Rehabil Med201147457958621304449
- DattolaVLogiudiceALBonannoLDoes the radiologically isolated syndrome exist? A dual-task cost pilot studyNeurol Sci201738112007201328831591
- JacobsJVKasserSLEffects of dual tasking on the postural performance of people with and without multiple sclerosis: a pilot studyJ Neurol201225961166117622160432
- WajdaDAMotlRWSosnoffJJCorrelates of dual task cost of standing balance in individuals with multiple sclerosisGait Posture201440335235624909581
- CastelliLDe LucaFMarchettiMRSellittoGFanelliFProsperiniLThe dual task-cost of standing balance affects quality of life in mildly disabled MS peopleNeurol Sci201637567367926728268
- EtemadiYDual task cost of cognition is related to fall risk in patients with multiple sclerosis: a prospective studyClin Rehabil201731227828426951347
- JacksonRTEpsteinCMDe l’AuneWRAbnormalities in posturography and estimations of visual vertical and horizontal in multiple sclerosisAm J Otol199516188938579184
- ProsperiniLCastelliLSellittoGConventional magnetic resonance imaging features associated with accidental falls in multiple sclerosisMult Scler201521449228080224
- CameronMHHorakFBHerndonRRBourdetteDImbalance in multiple sclerosis: a result of slowed spinal somatosensory conductionSomatosens Mot Res200825211312218570015
- ZackowskiKMSmithSAReichDSSensorimotor dysfunction in multiple sclerosis and column-specific magnetization transfer-imaging abnormalities in the spinal cordBrain2009132Pt 51200120919297508
- FlingBWDuttaGGSchlueterHCameronMHHorakFBAssociations between proprioceptive neural pathway structural connectivity and balance in people with multiple sclerosisFront Hum Neurosci2014881425368564
- ProsperiniLKouleridouAPetsasNThe relationship between infratentorial lesions, balance deficit and accidental falls in multiple sclerosisJ Neurol Sci20113041–2556021402386
- ProsperiniLSbardellaERazEMultiple sclerosis: white and gray matter damage associated with balance deficit detected at static posturographyRadiology2013268118118923533287
- TonaFDe GiglioLPetsasNMultiple sclerosis: the role of cerebellar dentate functional connectivity in balance deficitsRadiology Epub20171222
- FlingBWGera DuttaGHorakFBFunctional connectivity underlying postural motor adaptation in people with multiple sclerosisNeuroimage Clin2015828128926106552
- ProsperiniLPetsasNRazEBalance deficit with opened or closed eyes reveals involvement of different structures of the central nervous system in multiple sclerosisMult Scler2014201819023756679
- LeoneCFeysPMoumdjianLD’AmicoEZappiaMPattiFCognitive-motor dual-task interference: a systematic review of neural correlatesNeurosci Biobehav Rev20177534836028104413
- GunnHMarkevicsSHaasBMarsdenJFreemanJSystematic review: the effectiveness of interventions to reduce falls and improve balance in adults with multiple sclerosisArch Phys Med Rehabil201596101898191226070975
- StolzeHKlebeSZechlinCBaeckerCFriegeLDeuschlGFalls in frequent neurological diseases–prevalence, risk factors and aetiologyJ Neurol20042511798414999493
- ComberLQuinnGMcGuiganCGalvinRCooteSMedication usage and falls in people with multiple sclerosisMult Scler Epub201791
- GunnHCreanorSHaasBMarsdenJFreemanJRisk factors for falls in multiple sclerosis: an observational studyMult Scler201319141913192223633067
- CameronMHKarstensLHoangPBourdetteDLordSMedications are associated with falls in people with multiple sclerosis: a prospective cohort studyInt J MS Care201517520721426472941
- CliffordDBTetrahydrocannabinol for tremor in multiple sclerosisAnn Neurol19831366696716309074
- MeinckHMSchönlePWConradBEffect of cannabinoids on spasticity and ataxia in multiple sclerosisJ Neurol198923621201222709054
- GreenbergHSWernessSAPughJEAndrusROAndersonDJDominoEFShort-term effects of smoking marijuana on balance in patients with multiple sclerosis and normal volunteersClin Pharmacol Ther19945533243288143398
- PattiFMessinaSSolaroCEfficacy and safety of cannabinoid oromucosal spray for multiple sclerosis spasticityJ Neurol Neurosurg Psychiatry201687994495127160523
- CastelliLProsperiniLPozzilliCBalance worsening associated with nabiximols in multiple sclerosisMult Scler Epub201831
- ProsperiniLGiannìCFortunaDMarchettiMRPozzilliCOral dalfampridine improves standing balance detected at static posturography in multiple sclerosisMult Scler Int2014201480230724800078
- HuppertsRLyckeJShortCProlonged-release fampridine and walking and balance in MS: randomised controlled MOBILE trialMult Scler201622221222125921050
- AlviñaKKhodakhahKThe therapeutic mode of action of 4-aminopyridine in cerebellar ataxiaJ Neurosci201030217258726820505092
- RistoriGRomanoSViscontiARiluzole in cerebellar ataxia: a randomized, double-blind, placebo-controlled pilot trialNeurology2010741083984520211908
- RamanIMGustafsonAEPadgettDIonic currents and spontaneous firing in neurons isolated from the cerebellar nucleiJ Neurosci200020249004901611124976
- YildizAChmielewskiWBesteCDual-task performance is differentially modulated by rewards and punishmentsBehav Brain Res201325030430723680164
- DobryakovaEGenovaHMDeLucaJWylieGRThe dopamine imbalance hypothesis of fatigue in multiple sclerosis and other neurological disordersFront Neurol201565225814977