Abstract
To examine the effect of anti-vascular endothelial growth factor (anti-VEGF) agents on refractive error in the setting of retinopathy of prematurity (ROP) through a review of the literature, a PubMed search was performed of appropriate search terms, and the results of all relevant studies were extracted and compiled. Eleven relevant articles were identified in the literature, totaling 466 eyes, treated with varied anti-VEGF agents (bevacizumab, ranibizumab, and aflibercept) with mean spherical equivalent refractions ranging from +0.75 D to −3.57 D, with prevalence of high myopia ranging from 0 to 35%. Anti-VEGF monotherapy for ROP leads to low levels of myopia, and there may be a differential effect of specific anti-VEGF agents utilized on refractive outcomes.
Introduction
Advances in treatment for retinopathy of prematurity (ROP) are allowing better anatomical and functional outcomes, with further prevention of blindness from retinal detachment. Perhaps the most recent addition to the ROP-treatment armamentarium are anti-VEGF agents. Anti-VEGF agents have considerable clinical benefits, including reduction in the rate of high and very high myopia following treatment, compared with peripheral ablation.Citation1
Previously, as seen following cryotherapy and laser ablative therapy, these eyes would often develop high and very high myopia, which was attributed to the severity of ROP and not to the treatment modality itself.Citation2–Citation4 Similar, though much lower degrees of myopia, termed “myopia of prematurity”, are also seen in children born prematurely without ROP,Citation2,Citation5–Citation8 as well as in children with ROP that spontaneously regresses, called “myopia of spontaneously regressed ROP”.Citation2,Citation5–Citation12 In all of these cases, the myopia is nonaxial in nature with a steepened cornea, shallow anterior chamber, and thickened crystalline lens.Citation9,Citation10,Citation13–Citation15 These features are thought to be due to an arrested state of development of the immature eye.Citation12,Citation16
The myopia associated with prematurity and ROP develops along a spectrum, with myopia of prematurity of the lowest order, followed by myopia of spontaneously regressed ROP, with myopia of laser ablation creating the highest myopia.Citation1–Citation12,Citation16–Citation19 These factors alone are suggestive of an effect of severity of ROP on the development of myopia. However, with increasing research and recent data,Citation1,Citation16–Citation19 it seems the myopia seen in the face of prematurity and ROP is multifactorial in etiology, with three main causative factors: 1) prematurity, 2) the severity of ROP, and 3) changes related to the treatment administered for ROP (ie, peripheral retinal ablation or anti-VEGF administration). Peripheral retinal ablation causing increased myopia has been described in several reports,Citation16–Citation19 including a recent report of the refractive outcomes of the BEAT-ROP clinical trial at age 2.5 years.Citation1 The purpose of this review is to investigate the contributions of these causative factors to the resulting refractive error seen in children treated by anti-VEGF agents for ROP.
Materials and methods
A PubMed search was performed of several combinations of the following search terms: retinopathy of prematurity, ROP, refraction, refractive error, myopia, bevacizumab, ranibizumab, aflibercept, pegaptanib, anti-vascular endothelial growth factor, and anti-VEGF. The last search update was performed on January 13, 2016. The reference list of each identified article was also reviewed to ensure completeness. Extracted information from each relevant article included the first author’s name, year of publication, country in which the study was conducted, average gestational age of each cohort, average birth weight of each cohort, percentage of eyes treated for zone I ROP, specific treatment modalities utilized, average adjusted age (gestational age + number of weeks of life) at time of treatment, average age at time of refraction, average spherical equivalent (SE) refractive error in diopters, prevalence of myopia (SE >−0.25 D), and prevalence of high myopia (SE >−5 D).
Results
After a thorough PubMed review, eleven articlesCitation1,Citation20–Citation29 were identified relevant to the topic. In total, this amounted to 466 eyes (the number of infants was not consistently reported) treated with anti-VEGF agents for ROP: 378 eyes with intravitreal bevacizumab monotherapy (dosage ranging from 0.375 to 1.25 mg, with the majority administered 0.625 mg), 31 eyes with intravitreal ranibizumab monotherapy (0.25 mg), and 26 eyes with intravitreal aflibercept monotherapy (1 mg). The extracted information from each article is compiled in . The average SE refractive error reported after anti-VEGF monotherapy ranged from +0.75 D to −3.57 D. The average age at time of refraction in these studies ranged from 11.4 months to 5 years.
Table 1 Reports of refractive error after the use of anti-vascular endothelial growth factor agents for the treatment of retinopathy of prematurity
Discussion
The use of anti-VEGF agents in the treatment of ROP is being increasingly studied and utilized. The average SE refractive error following the administration of anti-VEGF agents is in the low-myopia range (mean ranging from +0.1 to −3.57 D).Citation1,Citation20–Citation29 There is some suggestion, however, that different anti-VEGF agents may yield different prevalence of high myopia (defined as SE ≤−5 D), with intravitreal bevacizumab yielding high myopia in 8%–35% of eyesCitation1,Citation20–Citation23,Citation25–Citation27 versus in 0 following intravitreal ranibizumab treatment.Citation27 However, more data are needed to better establish any differential effects on refractive error.
In the BEAT-ROP study, infants with stage 3+ or aggressive posterior ROP in zone I or zone II posterior were randomized to receive peripheral retinal laser ablation or intravitreal bevacizumab monotherapy.Citation30 In the 2.5-year refractive outcome results of the BEAT-ROP cohort, eyes matched for severity of ROP receiving anti-VEGF therapy were found to have significantly lower myopia on average than those receiving peripheral laser ablation ().Citation1 Mean SE refractions for those with zone I disease were −1.51±3.42 D in eyes treated with anti-VEGF and −8.44±7.57 D in eyes that received laser treatment. Mean SE refractions for those with zone II posterior disease were −0.58±2.53 D after treatment with anti-VEGF and −5.83±5.87 D after treatment with retinal laser. Specifically, very high myopia (≥−8 D) occurred in significantly fewer eyes treated with anti-VEGF (3.8% zone I, 1.7% zone II posterior) than in those treated with peripheral laser (51.4% zone I, 36.4% zone II posterior). These findings suggest a possible significant contribution of laser ablation to the increased myopia seen in these infants ( and ).
Figure 1 Zone I distribution of refractive error by treatment modality.
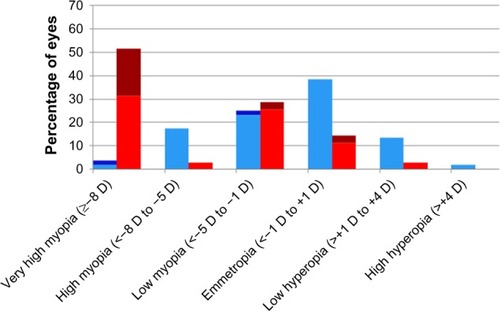
Figure 2 Zone II posterior distribution of refractive error by treatment modality.
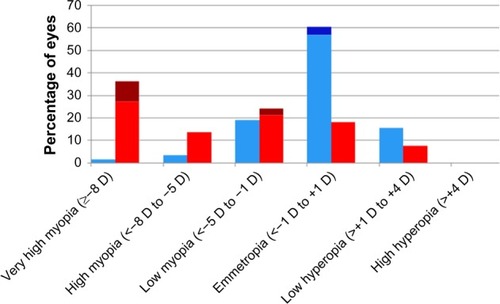
Table 2 Cycloplegic retinoscopic refractive error at age 2.5 years in the Bevacizumab Eliminates the Angiogenic Threat for Retinopathy of Prematurity clinical trialCitation1
In eyes treated for recurrence of ROP with additional anti-VEGF, as was done in the BEAT-ROP clinical trial, there was a further increase in myopia. This increased myopia was also seen in the control arm (laser ablation) of BEAT-ROP.Citation1 This increased myopia in eyes treated for recurrence of ROP is likely due to two of the three main etiological factors responsible for myopia in the premature population: increase in severity of ROP, and changes related to the treatment administered. Recurrence of ROP causes an equivalent reexposure to the disease process in both arms, and should therefore be expected to cause an equivalent increase in resultant myopia. However, there was a much higher incidence of very high myopia in eyes receiving additional laser (76.5%) for recurrence than in those receiving additional anti-VEGF (25%), suggestive of an added contribution from the treatment modality itself.Citation1 Increase in myopia and high myopia (defined in this study as SE ≤−5 D) in eyes (n=17) treated with laser for recurrence following initial anti-VEGF therapy was also seen in a recent study by Chen et al, suggesting again the role of both severity and possibly treatment modality in the development of increased myopia in eyes treated for recurrent ROP.Citation23
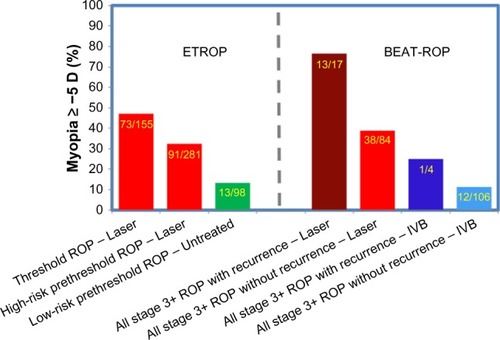
To better understand the impact of the refractive outcomes following anti-VEGF therapy, it is necessary to appreciate them in the setting of the current standard of care for ROP derived from the ETROP clinical trial.Citation31 A historical comparison of ETROP and BEAT-ROP was compiled to highlight some similarities and differences in the refractive outcomes of these studies (). In the ETROP study,Citation3,Citation4 the control group (laser treatment at threshold ROP) had a slightly greater percentage of eyes with myopia of −5 D or higher than the experimental group (laser treatment at high-risk prethreshold ROP). The percentage of eyes with myopia of −5 D or greater following laser therapy in the BEAT-ROP trial (for high-risk prethreshold to threshold ROP) was between that seen following laser treatment for both the control and experimental eyes in the ETROP clinical trial.Citation1 In contrast, the percentage of eyes with myopia of −5 D or greater after intravitreal bevacizumab treatment in the BEAT-ROP cohort was far less than that seen following peripheral retinal ablation. The myopia following anti-VEGF monotherapy for ROP in eyes that received intravitreal bevacizumab in the BEAT-ROP trial was similar to the myopia of spontaneously regressed ROP seen in the ETROP trial.Citation1,Citation3,Citation4
Figure 3 Percentage of eyes ≥−5 D in ETROP and BEAT-ROP by ROP severity at treatment.
Abbreviations: ROP, retinopathy of prematurity; IVB, intravitreal bevacizumab.
Similar amounts of low myopia and a tendency for emmetropia following treatment with anti-VEGF agents were also reported in several other case series.Citation20–Citation29,Citation32 Although purely speculative at this time, it is possible that intravitreal anti-VEGF agents allow for minimal disruption in the local growth-factor milieu and signaling pathways responsible for development of the anterior segment. As others have previously hypothesized, the incomplete development of the retina in prematurity with or without ROP may alter local ocular growth signals,Citation12,Citation16,Citation33 which may account for the anterior-segment changes seen in myopia of prematurity and in myopia of spontaneously regressed ROP. Intravitreal bevacizumab allows for continued development of the retinal vessels beyond the neovascular ridges, while this continuation is minimal following laser ablation.Citation30 The allowance of further migration of retinal vessels toward but not always necessarily to the ora serrata and the further maturation of photoreceptors may allow for more normal levels of the local growth factors required for proper signaling cascades in anterior-segment development.Citation11,Citation34 This would account for the lower amounts of myopia seen following anti-VEGF therapy. This is in contrast to the increased myopia and high myopia seen following treatment with laser, in which conceivably peripheral retinal ablation is more disruptive of the local growth-factor milieu and signaling pathways, leading to further impedance of anterior-segment development.
By potentially allowing more normal anterior-segment development in eyes treated with anti-VEGF agents, the cornea might be less steep, the anterior chamber deeper, and the lens less thickened. Thereby, these eyes may have the added benefit of also being at less risk of secondary long-term effects of high myopia, namely late angle-closure glaucoma, which is not uncommonly seen in eyes that have received prior laser therapy for ROP.Citation35,Citation36
Most recently, questions regarding the most appropriate anti-VEGF agent to use for the treatment of ROP have arisen and received much attention. The main two anti-VEGF agents being discussed for use in ROP, which have shown similar efficacy in the treatment of choroidal neovascularization in adults with age-related macular degeneration, are bevacizumab (Avastin; Genentech Inc, San Francisco, CA, USA) and ranibizumab (Lucentis; Genentech).Citation37 These two agents differ in biochemical structure, size and half-life, with bevacizumab having the longer half-life of 20 days versus ranibizumab’s half-life of 2 hours.Citation38,Citation39 These differences in structure, size, and half-life are of particular interest in their systemic and ocular effects on neonates following treatment for ROP. Studies have shown systemic VEGF levels are blunted for several weeks following treatment with bevacizumab for ROP.Citation40–Citation42 However, this blunting of systemic VEGF is not as prolonged following treatment with intravitreal ranibizumab for ROP. Recent evidence has shown that systemic VEGF levels immediately following intravitreal ranibizumab administration for ROP are diminished (at 1 day), but this effect does not persist at 1 week or later.Citation43
The differential ocular effects of these two anti-VEGF agents in eyes with ROP are just now being elucidated. While the efficacy in treatment of ROP (ie, regression and recurrence patterns) has been reported as similar between bevacizumab and ranibizumab,Citation27 the refractive outcomes may differ. More high myopia was seen in eyes treated with bevacizumab than in those treated with ranibizumab at 1 year of age (14.6% versus 0, respectively; P=0.03).Citation27 Chen et al hypothesized that the longer half-life of bevacizumab may be responsible for these refractive differences, perhaps by allowing increased apoptosis of retinal structures responsible for developmental signaling cascades.Citation27 This theory is based on a murine model, in which inhibition of VEGF receptors led to loss of Müller cells, astrocytes, and ganglion cells from the inner retina.Citation44 While this was just a single retrospective review, it raises interest in the differential effects on anterior-segment development and subsequent refractive error, which deserve further investigation and longer-term outcome data.
Conclusion
As intravitreal anti-VEGF agents are still new in the treatment armamentarium for ROP, there are several aspects of this therapy requiring further investigation, specifically longer-term refractive and visual outcomes following anti-VEGF treatment, as well as establishment of the long-term safety and a refinement of the dose and best specific anti-VEGF agent. However, outcomes thus far have been exciting, and the lesser myopia and decreased incidence of high myopia seen following anti-VEGF treatment compared to that following retinal laser ablation is not trivial.
Disclosure
The authors report no conflicts of interests in this work.
References
- GeloneckMMChuangAZClarkWLRefractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trialJAMA Ophthalmol2014132111327133325103848
- QuinnGEDobsonVKivlinJPrevalence of myopia between 3 months and 5½ years in preterm infants with and without retinopathy of prematurityOphthalmology19981057129213009663236
- QuinnGEDobsonVDavittBVProgression of myopia and high myopia in the Early Treatment for Retinopathy of Prematurity study: findings to 3 years of ageOphthalmology2008115610581064.e118423871
- QuinnGEDobsonVDavittBVProgression of myopia and high myopia in the Early Treatment for Retinopathy of Prematurity study: findings at 4 to 6 years of ageJ AAPOS201317212412823622444
- NissenkornIYassurYMashkowskiDSherfIBen-SiraIMyopia in premature babies with and without retinopathy of prematurityBr J Ophthalmol19836731701736687430
- O’ConnorARStephensonTJohnsonALong-term ophthalmic outcome of low birth weight children with and without retinopathy of prematurityPediatrics20021091121811773536
- O’ConnorARStephensonTJJohnsonATobinMJRatibSFielderARChange of refractive state and eye size in children of birth weight less than 1701 gBr J Ophthalmol200690445646016547327
- CookAWhiteSBatterburyMClarkDOcular growth and refractive error development in premature infants with or without retinopathy of prematurityInvest Ophthalmol Vis Sci200849125199520719036998
- Mintz-HittnerHARhodesLMMcPhersonARAnterior segment abnormalities in cicatricial retinopathy of prematurityOphthalmology1979865803816583499
- WuWCLinRIShihCPVisual acuity, optical components, and macular abnormalities in patients with a history of retinopathy of prematurityOphthalmology201211991907191622578258
- LueCLHansenRMReisnerDSFindlOPetersenAFultonABThe course of myopia in children with mild retinopathy of prematurityVision Res1995359132913357610594
- WangJRenXShenLYanniSELefflerJNBirchEEDevelopment of refractive error in individual children with regressed retinopathy of prematurityInvest Ophthalmol Vis Sci20135496018602423920368
- ChenTCTsaiTHShihYFLong-term evaluation of refractive status and optical components in eyes of children born prematurelyInvest Ophthalmol Vis Sci201051126140614820688740
- FledeliusHCFledeliusCEye size in threshold retinopathy of prematurity, based on a Danish preterm infant series: early axial eye growth, pre- and postnatal aspectsInvest Ophthalmol Vis Sci20125374177418422628207
- YangCSWangAGShihYFHsuWMLong-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of ageActa Ophthalmol2013914e276e28223601812
- AlgawiKGogginMO’KeefeMRefractive outcome following diode laser versus cryotherapy for eyes with retinopathy of prematurityBr J Ophthalmol19947886126147918287
- LawsFLawsDClarkDCryotherapy and laser treatment for acute retinopathy of prematurity: refractive outcomes, a longitudinal studyBr J Ophthalmol199781112159135401
- McLooneEMO’KeefeMMcLooneSFLaniganBMLong-term refractive and biometric outcomes following diode laser therapy for retinopathy of prematurityJ AAPOS200610545445917070482
- QuinnGEDobsonVSiatkowskiRDoes cryotherapy affect refractive error? Results from treated versus control eyes in the Cryotherapy for Retinopathy of Prematurity trialOphthalmology2001108234334711158812
- WuWCKuoHKYehPTYangCMLaiCCChenSNAn updated study of the use of bevacizumab in the treatment of patients with prethreshold retinopathy of prematurity in TaiwanAm J Ophthalmol20131551150158.e122967867
- Martínez-CastellanosMASchwartzSHernández-RojasMLLong-term effect of antiangiogenic therapy for retinopathy of prematurity up to 5 years of follow-upRetina201333232933823099498
- HarderBCSchlichtenbredeFCvon BaltzSJendritzaWJendritzaBJonasJBIntravitreal bevacizumab for retinopathy of prematurity: refractive error resultsAm J Ophthalmol2013155611191124.e123490192
- ChenYHChenSNLienRIRefractive errors after the use of bevacizumab for the treatment of retinopathy of prematurity: 2-year outcomesEye (Lond)20142891080108625104736
- SalmanAGSaidAMStructural, visual and refractive outcomes of intravitreal aflibercept injection in high-risk prethreshold type 1 retin-opathy of prematurityOphthalmic Res2015531152025471087
- IsaacMMireskandariKTehraniNTreatment of type 1 retin-opathy of prematurity with bevacizumab versus laserJ AAPOS201519214014425892041
- KuoHKSunITChungMYChenYHRefractive error in patients with retinopathy of prematurity after laser photocoagulation or bevacizumab monotherapyOphthalmologica2015234421121726393895
- ChenSNLianIHwangYCIntravitreal anti-vascular endothelial growth factor treatment for retinopathy of prematurity: comparison between ranibizumab and bevacizumabRetina201535466767425462435
- HwangCKHubbardGBHutchinsonAKLambertSROutcomes after intravitreal bevacizumab versus laser photocoagulation for retin-opathy of prematurity: a 5-year retrospective analysisOphthalmology201512251008101525687024
- GunayMCelikGGunayBOAktasAKaratekinGOvaliFEvaluation of 2-year outcomes following intravitreal bevacizumab (IVB) for aggressive posterior retinopathy of prematurityArq Bras Oftalmol2015785300300426466229
- Mintz-HittnerHAKennedyKAChuangAZEfficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurityN Engl J Med2011364760361521323540
- Early Treatment for Retinopathy of Prematurity Cooperative GroupRevised indications for the treatment of retinopathy of prematurity: results of the Early Treatment for Retinopathy of Prematurity random-ized trialArch Ophthalmol2003121121684169414662586
- HarderBCvon BaltzSSchlichtenbredeFCJonasJBEarly refractive outcome after intravitreous bevacizumab for retinopathy of prematurityArch Ophthalmol2012130680080122801850
- Mintz-HittnerHAKretzerFLPostnatal retinal vascularization in former preterm infants with retinopathy of prematurityOphthalmology199410135485588127576
- Cryotherapy for Retinopathy of Prematurity Cooperative GroupMulticenter trial of cryotherapy for retinopathy of prematurity: preliminary resultsArch Ophthalmol198810644714792895630
- MichaelAJPesinSRKatzLJTasmanWSManagement of late-onset angle-closure glaucoma associated with retinopathy of prematurityOphthalmology1991987109310981891218
- RitchRChangBMLiebmannJMAngle closure in younger patientsOphthalmology2003110101880188914522758
- Comparison of Age-Related Macular Degeneration Treatments Trials (CATT) Research GroupMartinDFMaguireMGRanibizumab and bevacizumab for neovascular age-related macular degeneration: two-year resultsOphthalmology201211971388139822555112
- BakriSJSnyderMRReidJMPulidoJSSinghRJPharma-cokinetics of intravitreal bevacizumab (Avastin)Ophthalmology2007114585585917467524
- BakriSJSnyderMRReidJMPulidoJSEzzatMKSinghRJPharma-cokinetics of intravitreal ranibizumab (Lucentis)Ophthalmology2007114122179218218054637
- SatoTWadaKArahoriHSerum concentrations of bevaci-zumab (Avastin) and vascular endothelial growth factor in infants with retinopathy of prematurityAm J Ophthalmol2012153232733321930258
- MatsuyamaKOgataNMatsuokaMWadaMTakahashiKNishimuraTPlasma levels of vascular endothelial growth factor and pigment epithelium-derived factor before and after intravitreal injection of bevacizumabBr J Ophthalmol20109491215121820538658
- TolentinoMSystemic and ocular safety of intravitreal anti-VEGF therapies for ocular neovascular diseaseSurv Ophthalmol2011569511321335144
- ZhouYJiangYBaiYWenJChenLVascular endothelial growth factor plasma levels before and after treatment of retinopathy of prematurity with ranibizumabGraefes Arch Clin Exp Ophthalmol20162541313625851862
- RobinsonGSJuMShihSCNonvascular role for VEGF: VEGFR-1, 2 activity is critical for neural retinal developmentFASEB J20011571215121711344092
