Abstract
Benign lymphoepithelial cysts are a widely recognized cause of parotid gland swelling in patients infected with the human immunodeficiency virus (HIV). These cysts are pathognomonic for HIV. The cysts frequently grow to be exceptionally large, causing physical deformity and gross asymmetry of facial contour. This clinical commentary analyzes this cosmetically deforming disease entity and the many treatments that accompany it. The patient presented in this paper is a surgical case-control. The case is a microcosm for our findings upon review of the literature. Treatment options for benign lymphoepithelial cysts include repeated fine-needle aspiration and drainage, surgery, radiotherapy, sclerotherapy, and conservative therapy, with institution of highly active antiretroviral therapy medication. Based on this surgical case-control and our review of the literature, it is concluded that surgical intervention offers the best cosmetic result for these patients.
Introduction
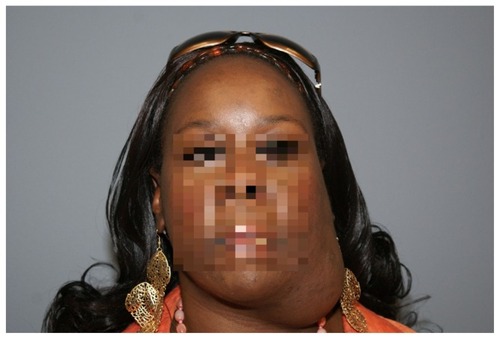
A 32-year-old female with human immunodeficiency virus (HIV) infection presented to our office six years after we had performed a right superficial parotidectomy for a 10 cm × 8 cm benign lymphoepithelial cyst (BLEC). This was cured surgically with excellent cosmetic outcome. The patient presented at this time with a similarly large lesion on the contralateral side which was removed in a similar fashion (see ). The patient tolerated the procedure well with no postoperative morbidity, normal facial nerve function, and a well healed scar.
Figure 1 Patient with HIV BLEC of the left parotid gland.
Abbreviation: BLEC, benign lymphoepithelial cyst.
The 6-year follow-up on this patient represents a case control study demonstrating the efficacy of parotidectomy in the treatment of BLEC. The only indication for removal of BLEC is when there is an expanding lesion distorting the patient’s facial appearance. In order to delve further into the best treatment for this cosmetic problem, a Medline search and review of the literature on BLEC was performed. To the best of the authors’ knowledge, this paper is the first to review the etiology, diagnosis, and treatment options for BLEC.
Literature review
Benign lymphoepithelial cysts (BLECs) are a widely recognized cause of parotid gland swelling in HIV-infected patients. Although they are neither invasive nor associated with malignant degeneration, BLECs can become large and disfiguring. These lesions can be a cosmetically devastating physical deformity, causing isolation and depression.Citation1–Citation6 They are easily recognized as a manifestation of HIV in the aware population.
BLEC of the parotid gland is the most common salivary gland pathology in HIV.Citation1,Citation2 BLEC has two hypothesized etiologic mechanisms. The first theorized pathogenesis of BLEC is the “obstructive theory” which states that lymphoid proliferation in the parotid gland leads to ductal obstruction and salivary dilation that mimics a true cyst.Citation1,Citation3,Citation4,Citation7–Citation9 The second hypothesized theory is that HIV-related reactive lymphoproliferation occurs in the lymph nodes of the parotid gland. The parotid glandular epithelium becomes trapped in normal intraparotid lymph nodes, resulting in cystic enlargement.Citation1,Citation7,Citation8
Diagnosis of BLEC is made based on history, physical examination, and fine-needle aspiration biopsy. BLEC is nearly diagnostic for HIV.Citation1,Citation2 Physical examination will show obvious fluctuant cystic facial deformity. Fine-needle aspiration biopsy of BLEC results in clear, proteinaceous (straw-colored) fluid, with a mixture of epithelial (squamous) and benign lymphoid cells.Citation7,Citation10 This combination of history, physical examination, and fine-needle aspiration biopsy is diagnostic for BLEC.Citation3,Citation10
Treatment of this particular pathology has been widely debated in the literature. Previous treatments for BLEC have included repeated fine-needle aspiration and drainage, surgery, radiotherapy, sclerotherapy, and conservative therapy with institution of highly active antiretroviral therapy (HAART) medications.Citation2–Citation6,Citation10–Citation22 summarizes the advantages and disadvantages, duration of procedures, and the cost of treatment for BLEC. A literature review of the aforementioned treatments for BLEC is summarized in the remainder of this paper and in .
Table 1 Advantages and disadvantages of treatment for benign lymphoepithelial cysts of the parotid gland as well as treatment duration and cost of treatment
Table 2 Treatment of benign lymphoepithelial cysts: review of the literature
HAART
Instituting HAART for BLEC has been shown to be effective in decreasing the size of the lesions.Citation2,Citation7 HAART treats systemic HIV by inhibiting retroviral transcription and viral replication. HAART therapy is theorized to correct the root cause of BLEC, ie, HIV infection. In a study by Syebele and Bütow, nine of ten patients with BLEC were found to have “a significant decrease in cyst size” (which was not quantified) after institution of HAART.Citation2 Cysts were still present at completion of the study. medications instituted in the study included two nucleoside analog reverse transcriptase inhibitors (stavudine and lamivudine) and one non-nucleoside reverse transcriptase inhibitor (efavirenz).Citation2
Fine-needle aspiration and drainage
Repeated fine-needle aspiration and drainage is a popular treatment for BLEC. The first aspiration typically occurs in the setting of the fine-needle aspiration biopsy, which rules out the possibility of another pathologic condition. Cysts can be drained up to twice per month, but there is a 100% recurrence rate in spite of this treatment.Citation15,Citation16,Citation20
Radiation therapy
In 1995, 12 patients with BLEC were given 8–10 Gray of radiation therapy. Although initial results were encouraging, longer follow-up revealed that only one of 12 patients had adequate cosmetic control at 9.5 months.Citation18 Worse, after initial failure, retreatment of eight patients with 8–10 Gray produced fewer responses and no long-term local control.Citation18 In 1999, Beitler et al studied 20 patients with BLEC, each treated with 18–24 Gray of radiation therapy to the parotid glands.Citation3 They were able to demonstrate partial cosmetic control of the disease in 14 of 20 patients. Side effects of treatment included xerostomia and mucositis.Citation3
Sclerotherapy
Sclerotherapy injections for BLEC includes multiple sclerotic agents, eg, sodium morrhuate, doxycycline, ethanol, bleomycin, and OK-432.Citation4,Citation6,Citation12,Citation13,Citation21 The studies on ethanol only evaluated patients subjectively as being pleased or displeased with their results, and therefore will not be discussed. Citation12 Doxycycline injection into the cysts resulted in a 22% (2/9 cysts) complete response rate.Citation22 Two of the patients in the doxycycline treatment group opted for superficial parotidectomy as definitive treatment for their cysts.Citation13 In two studies evaluating sodium morrhuate sclerotherapy, injections resulted in 17% (1/6 cysts) and 44% (4/9) complete response rates, respectively.Citation4,Citation9 Although limited in patient population size, sclerotherapy with bleomycin resulted in completed resolution in 3/3 patients (100%) with no side effects (although it has been noted to cause life-threatening irreversible pulmonary fibrosis when given as chemotherapy).Citation6 OK-432 (picibanil) has been strongly advocated as the treatment of choice for macrocystic lymphatic malformations.Citation23 Although BLEC is a different pathologic entity from cystic hygroma, there has been one reported case of BLEC that was satisfactorily treated with OK-432. Heran and Legiehn reported on multiple injections of OK-432 performed in one patient over the course of three months. The patient initially had the common side effects of low-grade fever and local swelling/erythema at the injection site, but these were self-limiting and resolved after one month. At one-year follow-up, the patient had no significant clinical recurrence.Citation21 Of note, this study was not published in a peer-reviewed journal, but was presented in its entirety at the 2009 meeting of the Cardiovascular and Interventional Radiological Society of Europe in Lisbon, Portugal.Citation21
Surgery
The initial studies regarding BLEC and surgery were performed in the early 1990s. Shaha et al undertook a retrospective review of 35 parotidectomies (20 superficial parotidectomies, 15 removal of the parotid tail for isolated cysts) for BLEC with up to six years of follow-up.Citation15 A complete response was seen in all 35 patients, although cysts did develop on the contralateral side in several patients. A study by Ferraro et al looked at surgical enucleation of 10 patients with bilateral BLEC (20 cysts total). Follow-up ranged from 3 to 36 months, with 19 complete responses and one recurrence.Citation16
Discussion
The indication for treatment of BLEC is cosmetic. As stated earlier, this pathology can be a cosmetically devastating physical deformity, causing social isolation and depression. Citation1–Citation6 The treatment that provides the best cosmetic outcome should be the treatment of choice. All treatments for BLEC show a partial response, but the only treatment to show a complete response in this pathology consistently with no recurrence is surgical intervention. Although bleomycin and OK-432 sclerotherapy injections have shown promising results, the data are currently limited to a case series (bleomycin, three patients) and a case report (OK-432). Limited data on the aforementioned therapies are available because these pilot studies were only recently performed. There is a need for further clinical data to support the use of bleomycin and OK-432 sclerosants in the treatment of BLEC. The side effect profile of OK-432 is mostly inflammatory in nature, with the major side effect being airway obstruction in patients treated for lymphatic malformations.Citation23 Fatal side effects have been associated with bleomycin in the form of irreversible pulmonary fibrosis.Citation23 In addition, the majority of BLECs are multiloculated, making injections into each loculation on multiple occasions challenging, time-consuming, and often unsuccessful. In 2009, Smith et al reported no response to treatment with OK-432 in 17 cases of microcystic multiloculated lymphatic malformations. Citation23 The last potential pitfall of sclerotherapy is that these agents aim to scar the particular area of injection to cause obliteration. If sclerotherapy is unsuccessful, then surgical intervention for cure is more difficult in the setting of scarring and sclerosis. The doxycycline study by Lustig et alCitation17 shows how failures of sclerotherapy must resort to surgical intervention for definitive treatment (2 patients). The scarring caused by sclerotherapy could cause more postsurgical morbidity in the setting of a scarred operative field (eg, facial nerve injury).
Reservations regarding parotidectomy in HIV-infected patients include the following: immunocompromised patients have a higher rate of postoperative infections, there is an unnecessary risk of HIV transmission imposed on the surgeon and the surgical team, and there could be facial nerve injury. Recent studies show that the postoperative rate of infection in HIV-infected patients is similar to that in the normal population, and is likely due to advances in the treatment of this disease.Citation24 New drug regimens for the medical treatment of HIV patients in the perioperative period have been developed, and with the advent of viral load measurement, the risks of HIV transmission during surgery have been dramatically reduced.Citation25 Regarding the complications of parotidectomy in the treatment of BLEC, surgical intervention has been compared with routine superficial parotidectomy for pleomorphic adenoma.Citation26 In the hands of an experienced surgeon, parotid gland surgery for benign disease has been shown to have a permanent paresis rate of 2.3% (one or more branches of the facial nerve), while partial superficial parotidectomy has a permanent paresis rate of 0% ().Citation26,Citation27
There are two other issues that must be addressed regarding surgical intervention. The prognosis of HIV has changed markedly in the past 30 years. From 1981 to 1996, the disease had a dismal prognosis, but since the establishment of HAART therapy in 1996, HIV has become a chronic disease with an excellent prognosis.Citation28 Given the success of surgery in BLEC, the argument for surgical intervention is further strengthened by the improved health and longevity of HIV-infected patients. The second issue regarding surgical intervention is that some surgeons believe that the surgical defect caused by removal of these large cysts will cause a substantial cosmetically deforming indentation. Parotidectomy defects can be cosmetically reconstructed in a variety of ways, including use of a cadaveric dermal matrix (Alloderm®), abdominal fat grafts, sternocleidomastoid muscle flaps, de-epithelialized radial forearm free flaps, and rectus abdominus free flaps.Citation29 In the case presented here, a cervical rotation flap with placement of Alloderm was performed to correct the patient’s left-sided parotid defect. In order to avoid donor site morbidity, the authors decided that Alloderm was the best reconstructive option for this patient. At 6 weeks postoperatively, the patient was doing well, with excellent facial symmetry ().
Figure 2 Patient 6 weeks postoperatively after left superficial parotidectomy. A similar result can be seen as compared to the right side. Facial contour and symmetry has been restored with excellent cosmetic outcome.

The case presented here illustrates excellent postsurgical control of BLEC after 6 years and demonstrates the disease course of untreated progression on the contralateral side. This patient represents an unblinded surgical case-control which demonstrates the efficacy of surgery for this condition.
Conclusion
There are many suboptimal cosmetic therapies used in the treatment of BLEC. Surgery is the gold standard treatment for BLEC, as evidenced by this literature review and case example.
Disclosure
The authors report no conflicts of interest in this work.
References
- ShantiRMAzizSRHIV-associated salivary gland diseaseOral Maxillofac Surg Clin North Am20092133934319608050
- SyebeleKBütowKWComparative study of the effect of antiretroviral therapy on benign lymphoepithelial cyst of parotid glands and ranulas in HIV-positive patientsOral Surg Oral Med Oral Pathol Oral Radiol Endod201111120521021237435
- BeitlerJJVikramBSilverCELow dose radiotherapy for multicystic benign lymphoepithelial lesions of the parotid gland in HIV-positive patients: Long-term resultsHead Neck19951731357533750
- MarcusAMooreCESodium morrhuate sclerotherapy for treatment of benign lymphoepithelial cysts of parotid gland in an HIV patientLaryngoscope2005474674915805892
- MichelowPDezubeBJPantanowitzLFine needle aspiration of salivary gland masses in HIV-infected patientsDiagn Cytopathol162011 [Epub ahead of print.]
- MonamaGMTshifularoMIIntralesional bleomycin injections in the treatment of benign lymphoepithelial cysts of the parotid gland in HIV-positive patients: case reportsLaryngoscope201012024324619950379
- WuLChengJMaruyamaSLymphoepithelial cyst of the parotid gland: its possible histopathogenesis based on clinicopathologic analysis of 64 casesHum Pathol20094068369219157503
- MaloranoEFaviaGVialeGLymphoepithelial cysts of salivary glands: an immunohistochemical study of HIV-related and HIV-unrelated lesionsHum Pathol1998292602659496829
- MandelLSurattanontFRegression of HIV parotid swellings after antiviral therapy: case reports with computed tomographic scan evidenceOral Surg Oral Med Oral Pathol Oral Radiol Endod20029445445912374919
- WittRLSalivary Gland Diseases: Surgical and Medical ManagementNew York, NYThieme Publishing2005
- SyebeleKRegression of both oral mucocele and parotid swellings, following antiretroviral therapyInt J Pediatr Otorhinolaryngol201074899219879006
- MeyerELubbeDEFaganJJAlcohol sclerotherapy of human immunodeficiency virus related parotid lymphoepithelial cystsJ Laryngol Otol200912342242518590602
- SuskindDLTavillMAHandlerSDDoxycycline sclerotherapy of benign lymphoepithelial cysts of the parotid: a minimally invasive treatmentInt J Pediatr Otorhinolaryngol20005215716110767463
- EchavezMILeeKCSooyCDTetracycline sclerosis for treatment of benign lymphoepithelial cysts of the parotid gland in patients infected with human immunodeficiency virusLaryngoscope1994104149915027990641
- ShahaARDiMaioTWebberCThelmoWJaffeBMBenign lymphoepithelial lesions of the parotidAm J Surg19931664034068214302
- FerraroFJJrRushBFJrRuarkDOleskeJEnucleation of parotid lymphoepithelial cyst in patients who are human immunodeficiency virus positiveSurg Gynecol Obstet19931775245268211607
- LustigLRLeeKCMurrADoxycycline sclerosis of benign lymphoepithelial cysts in patients infected with HIVLaryngoscope1998108119912059707244
- BeitlerJJSmithRVBrookABenign parotid hypertrophy in HIV+ patients: limited late failures after external radiationInt J Radiat Oncol Biol Phys19994545145510487570
- GoldsteinJRubinJSilverCRadiation therapy as a treatment for benign lymphoepithelial parotid cysts in patients infected with human immunodeficiency virus-1Int J Radiat Oncol Biol Phys199223104510501639639
- TerryJHLoreeTRThomasMDMajor salivary gland lymphoepithelial lesions and the acquired immunodeficiency syndromeAm J Surg19911623243291951883
- HeranMKSLegiehnGMOK-432 sclerotherapy of parotid lymphoepithelial cysts in an HIV patientPoster presented at the Cardiovascular and Interventional Radiological Society of Europe meetingSeptember 19–23, 2009Lisbon, Portugal
- BergEEMooreCEOffice-based sclerotherapy for benign parotid lymphoepithelial cysts in the HIV-positive patientLaryngoscope200911986887019358192
- SmithMCZimmermanMBBurkeDKEfficacy and safety of OK-432 immunotherapy of lymphatic malformationsLaryngoscope200911910711519117316
- CavasinHDolaTUribeOPostoperative infectious morbidities of cesarean delivery in human immunodeficiency virus-infected womenInfect Dis Obstet Gynecol5252009 [Epub ahead of print.]
- PapendorpSGvan den BerkGEPreoperative use of raltegravir-containing regimen as induction therapy: very rapid decline of HIV-1 viral loadAIDS2010241603160820539094
- KochMZenkJIroHLong-term results of morbidity after parotid gland surgery in benign diseaseLaryngoscope201012072473020205175
- Guntinas-LichiusOKlussmannJPWittekindtCStennertEParotidectomy for benign parotid disease at a university teaching hospital: outcome of 963 operationsLaryngoscope2006116453454016585855
- LisetteOMansiSRoviniHHIV combination productsNat Rev Drug Discov20076951952
- GhanemTParotid defectsFacial Plast Surg Clin North Am20091726326919393948