Abstract
Background
Currently, provider-initiated human immunodeficiency virus (HIV) testing (PIHT) in health facilities is one of the strategies to advance HIV testing and related services. However, many HIV infected clients are missing the opportunities. This study intends to identify predictors of refusal of PIHT among clients visiting adult outpatient departments (OPDs) in Jimma town.
Methods
An unmatched case control study was conducted among 296 clients: 149 cases refusing HIV testing and 147 controls accepting HIV testing. The study recruited clients from OPDs of four public health facilities between March 6 and April 8, 2011 using consecutive sampling. The study instrument was adapted mainly considering health belief model (HBM). Jimma University ethical committee reviewed the study protocol. Data were collected by face-to-face interview and analyzed using SPSS Statistics (IBM Corporation, Somers, NY) software, version 16.0. Data were subjected to factor and reliability analysis. For prediction analysis, the study used logistic regression and odds ratio (OR) with 95% confidence interval (CI). To see the effects among HBM constructs, the study used standardized beta (β) coefficients at P < 0.05.
Results
The study findings showed adjusted protective effects on refusal of PIHT for residence outside study town [adjusted OR (AOR) (95% CI) = 0.41 (0.22–0.79)] and higher scores of perceived benefit of early testing [AOR (95% CI)] = 0.86 (0.69–0.99)], self efficacy to live with HIV [AOR (95% CI) = 0.79 (0.66–0.93)], nondisclosure agreement [AOR (95% CI) = 0.74 (0.58–0.93)], perceived explicitness of opt-out right during initiation [AOR (95% CI) = 0.74 (0.56–0.98)] and clients’ perceptions of selective initiation of HIV suspected [AOR (95% CI) = 0.54 (0.41–0.73)]. On the other hand, report of recent testing [AOR (95% CI) = 3.82 (1.71–8.55)] and perceived unpreparedness for testing [AOR (95% CI) = 1.86 (1.57–2.21)] aggravated refusal of PIHT. Exposure to cues to testing significantly reduced perceived barriers [β (P) = −0.05 (0.037)].
Conclusion
Clients’ perceived barriers: feeling of unpreparedness for testing strongly aggravated refusal of test. Enhanced self-efficacy to live with HIV and presence of cues to HIV testing would reduce unpreparedness and protect from refusing PIHT.
Keywords:
Background
Globally, human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) is killing millions of people, and the epidemic is continuing to grow.Citation1 It has become a major public health problem in sub-Saharan Africa.Citation2 At the end of 2008, more than two-thirds of worldwide estimates of HIV prevalence, incidence, and deaths accounted to sub-Saharan Africa.Citation3 This epidemic of HIV/AIDS in the region has often been associated with social and economic problems such as stigma and reduced productivity from death of productive forces.Citation4,Citation5 To combat the epidemic and transmission of HIV/AIDS, many advances have been made in developing effective and affordable interventions. These include safer-sex education, access to condoms, HIV treatment, and HIV counseling and testing (HCT).Citation1,Citation2,Citation6 HCT is an essential tool in HIV/AIDS prevention and control strategies. It is a critical entry point for early engagement into treatment and care, linkages to other relevant services such as sexually transmitted infection (STI) treatment, family planning, and prevention of motherto- child-transmission programs.Citation7–Citation9
For over 20 years, until 2007, the predominant HIV testing approach had been voluntary counseling and testing (VCT). This approach allowed clients to actively seek HIV testing.Citation6,Citation10 Despite the startling number of people unknowingly infected, the number of people who seek testing on their own is unacceptably low.Citation8,Citation11 The World Health Organization (WHO) reported in 2004 that only 5% of people living with HIV/AIDS (PLWHA) were estimated to be aware of their serostatus. It again witnessed very low global use of HIV testing in 2007.Citation8,Citation12 Across the world, missing HIV testing has been related with further problems; only small segment of PLWHA enrolled on Anti-Retroviral Therapy (ART) and continuing transmission of HIV.Citation10–Citation13 Despite VCT assisting millions to know their HIV status, it could not reach many people.Citation14 WHO recommends VCT to scale up to provider-initiated HIV testing and counseling (PIHT). This is intended to increase the number of people who know their status early on, decrease the prevalence of undiagnosed infection, and to promote early treatment for HIV infection.Citation6
In Ethiopia, national HIV/AIDS policy issued in 1998 incorporated VCT as one of HIV/AIDS services. It updated VCT to include PIHT in 2007. PIHT then became part of routine clinical management of illnesses by identifying unsuspected HIV infection.Citation15–Citation17 Currently, PIHT is routinely offered to all clients presenting to every outpatient and inpatient ward if they have not recently been tested.Citation6,Citation10,Citation14,Citation17
In spite of the arrangements made to advance HIV testing and related services, evidence suggests that many opportunities to diagnose individuals at health facilities are still being missed. This is attributed to clients’ passivity to seek testing, refusal of testing offer, and lack of an active role of providers to initiate testing.Citation6,Citation18,Citation19 Many studies in Africa have revealed that missing HCT is partly attributed to low acceptance of PIHT in health care settings. This seems a critical problem as high HIV positivity rate detection is being observed among acceptors of the testing offer.Citation1,Citation8,Citation10,Citation20–Citation26
In Ethiopia, evidence shows problems related to HCT. In 2005, only 7.6% of HIV infected individuals knew their status. HIV testing rate was 121 tests per 1000 population in 2009.Citation24,Citation27 Studies among different populations between 2008 and 2009 revealed less than expected acceptance of PIHT and high HIV positivity rate in health care settings.Citation19,Citation28–Citation31 For example, the respective PIHT uptake and HIV positivity rates among tuberculosis (TB) patients were 70.6% and 36.2% in Northern Ethiopia, and 35% and 20.6% in Southern Ethiopia.Citation28,Citation29 These similar rates among clients visiting health facilities were 36.5% and 6.9% in North Eastern Ethiopia.Citation19 The rate of readiness to accept PIHT among antenatal care (ANC) attendees was 74.5% in southern Ethiopia.Citation30 These evidences of low acceptance of PIHT and high HIV positivity rate in different countries.Citation1,Citation19,Citation20,Citation22,Citation28–Citation31 imply loss of access to ART services and continued existence of high transmission.Citation32 Developing countries, including Ethiopia, that are undergoing single or repeated HCT is contributing to a reduction in infection rate and increase in safe sexual behaviors, which is encouraging.Citation33–Citation35
Thus, to achieve the purpose of PIHT, it is crucial to investigate clients’ reasons for missing PIHT in health care settings.Citation26 To date, most studies related to acceptance of PIHT in Ethiopia and other countries were done in TB, ANC, and STI clinics.Citation19,Citation20,Citation28–Citation30,Citation36 These clinics are generally composed of a cohort of clients in terms of risk to HIV and higher HIV suspected wards than adult outpatient department (OPD) wards. PIHT-related studies are limited in these OPD wards. Therefore, it is timely and appropriate to study factors that hinder client use of PIHT, particularly in OPDs. This study seeks to identify psychosocial predictors of refusal of PIHT in adult OPDs in public health facilities in Jimma town.
Methods
Study design and setting
This study used an unmatched case control design and was conducted among clients who were provider initiated for HIV testing in eight OPDs of four public health facilities in Jimma town. Jimma town is located in Oromia, Ethiopia. There are four public health care facilities in the town routinely providing on HIV testing service free of charge: three health centers, namely Jimma Health Center (JHC), Kefitegnahulet Health Center (KHC), and Mendera Kochi Health Center (MKHC); and one hospital, Jimma University Specialized Hospital (JUSH). The health centers on average give primary health care (PHC) services to 38,325 clients per year. JUSH provides PHC and specialized clinical services to approximately 9000 inpatients and 80,000 outpatient clients each year. It gives specialized clinical services to clients, including those referred from different regions of the country. In the facilities, both HIV testing models, VCT and PIHT, are currently in use. PIHT is mandatory, under informed consent, to all clients presenting to the facilities.
Participants and sampling
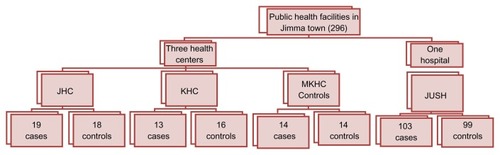
To be included in the study, a participant must be ≥15 years old, clients of adult OPDs of the four study facilities, and initiated by health care providers to undergo HIV testing. Clients were recruited from eight adult OPDs in the four study facilities: one OPD in each of the three health centers, and five in JUSH. Before recruitment, clients gave their informed consent. Clients who refused provider-initiated HIV testing were considered as cases while acceptors of the test as controls. The study excluded clients who were critically sick. A total of 304 outpatients were recruited for the study (152 cases and 152 controls) considering 10% of nonresponse rate. Sample sizes were calculated using the two-population proportion formula in Epi Info™ (Centers for Disease Control and Prevention, Druid Hills, GA) software, version 3.03.17, for unmatched case control studies, considering the following assumptions: level of significance (α = 5%), power (1 – β) of the test (80%), case to control ratio (1:1), proportion of HIV risk perception among cases (P1 = 26.81%), and proportion of HIV risk perception among controls (P2 = 43.64%). P1 and P2 were taken from a similar study.Citation36 The samples were then proportionally allocated to the four study facilities, considering one month outpatient flows before the start of the study (see ). A consecutive sampling method was then employed to select eligible cases and controls until the allocated sample size was filled from the respective health facilities. Inclusion of samples were consecutively continued until the corresponding sizes of cases and controls were independently filled from each facility.
Data collection procedures
The study recruited the sampled cases and controls from eight adult OPD units between March 6 and April 8, 2011. Eight trained health professionals collected the data. Health care providers working in OPDs and PIHT assisted the data collection process for identifying and referring cases and controls to data collectors. The health providers used blue and green cards to refer cases and controls respectively. The data collectors received and disposed the cards before going on the interview. For those who accepted the test, the data collection was conducted before they received the test result. The data collection process was supervised by trained supervisors at each of the study facilities.
Conceptual framework
This study used the health belief model (HBM) as a conceptual framework. HBM is a sociopsychological model. It addresses the likelihood of taking recommended health action as influenced by specific health beliefs related to the health problem and recommended health actions. These beliefs are the individual’s perceptions of the threat posed by a health problem (susceptibility, severity), the benefits of avoiding the threat, and factors influencing the decision to act (barriers, cues to action, and self-efficacy).Citation37,Citation38 The core constructs of the model include: (1) perceived susceptibility, ie, one’s subjective perception of the risk of contracting a health condition; (2) perceived severity, ie, feelings concerning the seriousness of contracting an illness or of leaving it untreated; (3) perceived benefits, ie, the believed effectiveness of strategies designed to reduce the threat of illness and risk; (4) perceived barriers, ie, feeling a nuisance as someone who takes particular health actions or results from the actions. (5) cues to action, ie, events, either bodily or environmental, that motivate people to take action; and (6) self-efficacy, ie, the belief in being able to successfully execute the behavior required to produce the desired outcomes.Citation37–Citation39
In addition to the basic constructs, originators and researchers included some variables called modifying factors. These factors can influence individual perceptions and, indirectly, health-related behaviors. These factors are expected to modify the variances explained by the main HBM constructs. The variables included under modifying factors are demographic, sociopsychological, and structural.Citation39 Therefore, in this study the relationship of core constructs of HBM, the modifying factors (sociodemographic variables, health motivation, and clients’ perceptions of contexts during test initiation), and other factors such as sexual and previous testing behaviors, predict HIV testing behavior.
Instruments
The study used a structured questionnaire adapted from the literature.Citation40–Citation49 The instrument comprised dimensions indicated in a previous conceptual framework: sociodemographic characteristics, health motivation (five items), perception obedience (three items), perception of initiation (four items), perception of susceptibility to HIV (seven items), perception of severity of HIV/AIDS (seven items), perceived benefits of testing (16 items), perceived barrier of testing (17 items), self efficacy to live with HIV test results (six items), cues to HIV testing (five items), past sexual behavior (eight items), and testing experience (eight items). Each dimension of HBM, except cues to testing and other perception items, elicited responses on a five-point Likert scale: “strongly disagree (1),” “somewhat disagree (2),” “neither agree nor disagree (3),” “somewhat agree (4),” “strongly agree (5).” Negatively worded items were reversed during analysis.
Confirmatory and explanatory factor analysis (FA) was executed to examine the underlying factors for Likert scale format items depending on the purpose of FA. Eigen value of >1 was considered for construct validity. Factor loading score of ≥40% and varimax method of rotation was considered to load items on confirmed or identified subdimension scales. For each scale Cronbanch’s alpha (α) score of ≥70% was taken as an acceptable measure of internal consistency of items on the scale. In line with the expectations, confirmatory FA (CFA) for most of the scales confirmed only one meaningful underlying factor. Accordingly, the factor underlying health motivation explained 90.2% of the variance, obedience level (66.1%), perceived selective HIV suspect initiation (75.0%), and perceived explicitness of opt-out right (73.0%). Some scales relating to HBM also depicted only one underlying factor component. Consequently, the factor underlying perceived susceptibility explained 62.6% of the variance. Similarly, cues to testing and self efficacy to live with HIV explained 80.9% and 75.0% of the variances respectively. However, two meaningful factor components were emerged from perceived severity scale, and the subscales were named as clinical severity (variance = 83.9%) and social severity (variance = 78.0%).
Similarly, for perceived benefit of HIV testing, three factors with Eigen value greater than one were indentified using explanatory FA (EFA). The factors were named as perceived importance of testing to plan future life explaining a variance of 82%, perceived benefits from early testing (78%), and weighted attitude towards ART (86%). (Attitude towards ART is a multiplicative output of two belief items and two evaluations of beliefs items). Perceived barrier items were also subjected to EFA, and six underlying factors were identified; namely, perceived stigma (variance = 69.5%), nondisclosure agreement (variance = 91.0%), perceived unpreparedness (variance = 84.0%), perceived unmet preferred condition (variance = 83.4%), and perceived fear (variance = 76.0%). Finally, the questionnaires were translated into two local languages, Afan Oromo and Amharic, and back-translated to English by different individuals.
Statistical analysis
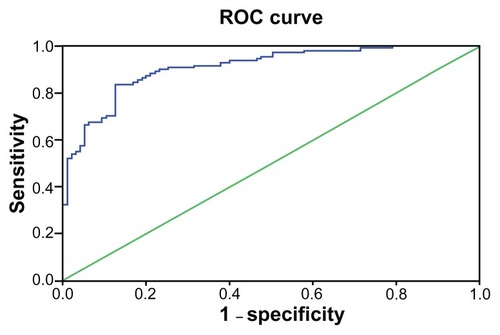
The data were analyzed using SPSS Statistics (IBM Corporation, Somers, NY) software, version 16.0. Data cleaning and assumption checking were performed before proceeding to analysis. Data were then subjected to FA. After FA, items were summed up and used for further prediction analysis. Multivariate logistic regression analysis was used for prediction of refusal of PIHT. In the first regression model, the effect of variables related to HBM was assessed. While in the second and third regression models, the effect of modifying factors and past HIV and testing-related behaviors was examined. Multivariate analysis used forward likelihood binomial logistic regression model. To claim statistically significant effect, crude and adjusted odds ratio with 95% confidence interval (CI) was employed. Finally, all significant variables were put into regression to fit parsimonious prediction model for refusal of PIHT. The ratio of chi squared (χ2) for goodness of fit to degrees of freedom (df) between 0 and 3 was considered as goodness of fit to the model; the score nearer to zero indicating good fit. The analysis used R-squared (r2). A receiver operating characteristic (ROC) curve was used to measure sensitivity and specificity of the fitted final model at 95% CI and P < 0.05. Linear regression coefficient (beta) with P-value was used to examine standardized effect among HBM constructs.
Ethical consideration
The ethical issue of this study was reviewed and approved by the ethical committee of the College of Public Health and Medical Sciences of Jimma University. Written informed consent was sought from each respondent before recruiting them to participate in the study.
Results
A total of 296 clients were included in this study, making a response rate of 97.05%. Of the respondents, 149 were cases and 147 were controls, with corresponding response rates of 98% and 96.07% respectively.
Clients’ sociodemographic characteristics
shows sociodemographic characteristics of respondents. Accordingly, the majority, 162 (54.9%), of the respondents were males. The median age was 30 years. Nearly half, 152 (51.4%), were of the Muslim religion. More than half, 171 (57.8%), of the respondents belonged to the Oromo ethnic group. With regards to marital status, 173 (58.4%) were married, and only 15 (5.1%) were either widowed or divorced. Regarding educational level more than half, 163 (55.1%) have attended primary school or less. For occupation, 72 (24.3%) were farmers, while 62 (20.9%) were government employed. The median monthly income was 500 Ethiopian Birr, with mean ± standard deviation (737.33 ± 690.29).
Table 1 Sociodemographic characteristics by PIHT-acceptance status among clients in Jimma town adult outpatient departments, Oromia region, April 2011 (N = 296)
HBM constructs and refusal of PIHT
As shown in , the stepwise binomial logistic regression for constructs of HBM showed statistically significant adjusted protective effects on refusal of PIHT for perceived benefit of early testing [adjusted odds ratio (AOR) (95% CI) = 0.86 (0.69–0.99)], nondisclosure agreement of positive results [AOR (95% CI) = 0.73 (0.58–0.93)], and self efficacy to live with HIV [AOR (95% CI) = 0.79 (0.66–0.93)]. On the other hand, it showed adjusted aggravating effect for perceived unpreparedness to undergo testing [AOR (95% CI) = 1.86 (1.57–2.21)] and perceived clinical severity of HIV/AIDS [AOR (95% CI) = 1.67 (1.06–2.66)]. However, perceived susceptibility to HIV, report of higher number of cues to HIV testing, perceived importance of HIV testing to plan future life, and perceived benefit of early testing had unadjusted protective effect on refusal of PIHT with respective crude OR (COR) (95% CI) = 0.91 (0.83–0.99), COR (95% CI) = 0.67 (0.51–0.89), COR (95% CI) = 0.88 (0.79–0.98), and COR (95% CI) = 0.81 (0.69–0.93). Perceived unmet preferred condition to testing had unadjusted aggravating effect on refusal of PIHT with COR (95% CI) = 1.20 (1.06–1.37). The regression model for HBM constructs explained 43.6% (r2) variance of refusal of PIHT in OPDs with goodness of fit to the model (χ2/df) of 1.6.
Table 2 The effects of health belief model constructs on refusal of PIHT, among clients in Jimma town adult outpatient departments, Oromia region, April 2011 (N = 294)
Relationship among constructs of HBM
In addition to finding the effects of HBM constructs, as shown in , linear regression showed a statistically significant relationship among most of the constructs. Perceived susceptibility showed no effect with any of the other independent constructs of HBM (perceived threat is the product of susceptibility and severity). Perceived severity showed standardized effect with all constructs other than susceptibility. It showed a negative effect with perceived benefits of testing and cues to testing and a positive effect with self efficacy and perceived barriers. Clients’ weighted perceived threat showed similar effect with perceived severity, although no effect was observed with perceived benefit. Perceived barriers showed standardized negative effect with self efficacy to live with an HIV-positive test result and perceived benefit of testing. Perceived benefit of testing showed positive effect with self efficacy. However, exposure to cues to testing showed negative effect with self efficacy.
Table 3 Relationship between HBM constructs regarding refusal of PIHT among clients visiting outpatient departments in Jimma town, Oromia region, April 2011 (N = 296)
HBM-modifying factors and refusal of PIHT: the effects of contexts modifying HBM
As shown in , HBM modifying factors (psychosocial and sociodemographic dimensions) adjusted together included clients’ sociodemographic variables, health motivation, perceived obedience to providers, perceived selective HIV suspected initiation, and perceived explicitness of opt-out right during initiation. The adjustment showed statistically significant protective effect on refusal of PIHT in OPDs. The significant variables were: Jimma zone rural resident [AOR (95% CI) = 0.41 (0.22–0.79)], health motivation [AOR (95% CI) = 0.68 (0.52–0.89)], perceived selective HIV suspected initiation [AOR (95% CI) = 0.54 (0.41–0.73)], and perceived explicitness of opt-out right [AOR (95% CI) = 0.74(0.56–0.98)]. Some variables showed only crude effect on refusal of PIHT. Being divorced/widowed showed crude positive effect on refusal, while obedience to health provider reduced risk of refusal, with COR (95% CI) = 4.54 (1.24–16.70) and COR (95% CI) = 0.88 (0.80–0.97) respectively. The regression model of the HBM modifying factors explained 17.4% (r2) variance of refusal of PIHT with goodness of fit to the model (χ2/df) of 2.8.
Table 4 Regression effects of HBM-modifying contexts on refusal of PIHT among clients visiting Jimma town outpatient departments, Oromia region, April 2011 (N = 294)
Clients’ past behaviors and refusal of PIHT: the effect of sexual and HIV testing experience
As shown in , reporting clients’ sexual behavior and history of HIV testing, the majority, 263 (88.9%), of the respondents were sexually active. Among these, 39 (14.8%) engaged in sex with either causal or previous partners who were neither steady nor married spouses. Regarding use of condoms, only 31 (11.8%) of respondents used them either usually or consistently. More than three quarters, 231 (78%), of clients had history of ever undergoing HIV testing. Of these, 162 (74.1%) had undergone testing twice or less. However, only nearly a quarter, 56 (24.3%) reported having recently been tested (within the last 3 months before commencement of this study).
Table 5 Sexual behavior and history of HIV testing by PIHT-acceptance status, among clients in Jimma town adult outpatient departments, Oromia region, April 2011
As shown in , to see the predictive effects of past behaviors on refusal of PIHT, clients’ sexual behaviors and previous experience of HIV testing were adjusted. The adjustment showed statistically significant aggravating effect on refusal of PIHT only for undergoing recent testing [AOR (95% CI) = 3.82 (1.71–8.55)]. However, having no history of either testing or initiation by health providers reduced the risk of refusing PIHT, with [COR (95% CI) = 0.51 (0.28–0.88)] and [COR (95% CI) = 0.49 (0.30–0.80)] respectively. This adjustment explained 8.5% (r2) variance of refusal of PIHT in OPDs with goodness of fit to the model (χ2/df) of 10.94.
Table 6 Effect of sexual behavior and history of HIV testing on refusal of PIHT among clients visiting outpatient departments in Jimma town, Oromia region, April 2011
Fitted final regression model for prediction of refusal of PIHT in OPDs
As shown in , to fit final regression model that best predicts refusal of PIHT in OPDs, this study adjusted all blocks of analysis; HBM constructs, the modifying contexts, and past behaviors related to HIV transmission or testing. Self efficacy, perceived explicitness of opt-out right, residence in Jimma zone rural, and small towns showed statistically significant protective effect on refusal of PIHT. On the other hand, perceived unpreparedness and report of recent testing showed aggravating effect on refusal of PIHT. This fitted final model explained 62.2% (r2) variance of refusal of PIHT in OPDs with goodness of fit to the model (χ2/df) of 19.58/8 = 2.48. This ratio score observed to be between 0 and 3 shows the goodness of fit to the model in predicting PIHT refusal at indicated variance.
Table 7 Regression effects of fitted final prediction model of refusal of PIHT among clients in Jimma town adult outpatient departments, Oromia region, April 2011 (N = 276)
ROC curve for fitted final regression model for refusal of PIHT
As shown in , the ROC curve for fitted final prediction model showed statistically significant sensitivity and specificity of refusal of PIHT, with curve area (95% CI) = 0.91 (0.87–0.95), P < 0.01. This indicates the items used in measuring predictors of refusal of PIHT in OPDs correctly differentiated cases from controls and vice versa on average by 91%.
Discussion
This study estimated the likelihood of refusal of PIHT in OPDs using: (1) HBM; (2) HBM-modifying contexts such as health motivation, psychosocial conditions in the health setting, and sociodemographic factors; (3) past behaviors, including experience of past similar behavior (HIV testing) and sexual behavior. According to HBM, someone with a perceived susceptibility to severe ill-health may feel a need to engage in healthy behavior.Citation37,Citation39 In this study, adjusted effects of HBM, the modifying factors, and past experiences explained 43.6%, 17.4%, and 8.5% variances of refusal of PIHT respectively. The HBM shared 69.8% of the total variances (62.5%) explained by this study. This showed inclusion of modifying contexts and past experiences contributed to prediction of PIHT, and thus using only HBM would not be adequate.
Regarding the direction of prediction, most of the constructs of HBM showed the same direction of effect on healthy behavior (HIV testing in this case) as proposed by the model proponents. Only perceived severity showed inversed direction (refer conceptual framework). Accordingly, perceived susceptibility to HIV/AIDS slightly reduced a client’s likelihood of refusing PIHT, although this observation was insignificant compared with other constructs. Many studies in Ethiopia and other countries also showed similar findings that a client’s perception of high personal or partner susceptibility to HIV risk, and acknowledging risk behaviors, facilitate acceptance of being tested.Citation19,Citation28,Citation50,Citation51
In this study, perceived clinical severity of HIV/AIDS showed an adjusted slight positive effect on refusal of PIHT, even though social severity showed no effect. Also, the weighted dimensions of perceived severity showed no significant effect on refusal. However, it had positive standardized effect with perceived barriers (see ). Similarly, research on the utilization of HCT in America in 2007shows clients’ perceptions of HIV/AIDS facilitates barriers such as the emotional connotations of HIV tests, and fear of stigma negatively influenced HIV testing.Citation26 In addition, a systematic review of many studies that used HBM showed slight power of perceived severity in directly affecting health behavior.Citation37
In this study, perceived clinical and social threat showed no adjusted effect on refusal of PIHT. This is certainly related to effects of perceived susceptibility and severity. In this study, among perceived benefit dimensions only, perception that testing should be made as early as possible showed an adjusted negative effect on refusal of PIHT compared with other constructs of HBM. Studies on accepting HIV testing showed individuals with a high awareness about the benefits of HIV testing and knew that ART can help a person live longer were more likely to be tested than individuals with low awareness.Citation28,Citation52 Even though attitude towards ART and the importance of testing to plan future life showed no adjusted effect on refusal of PIHT, weighted dimensions of perceived benefit showed negative standardized effects with perceived severity and dimensions of perceived barriers to testing (see ). Thus, perhaps predicting HIV testing in terms of perceived benefits of ART is less efficient when it is PIHT than when it is client initiated.
Though clients may recognize the benefit of early testing, they may face barriers to undergo testing when initiated by providers. For example, perceived unpreparedness to undergo testing was the main predictor facilitating refusal of PIHT. According to the stages of change (transtheoretical) model, preparation is an important step in motivating people to plan specific actions that help them adopt healthy behaviors following appreciation of one’s risk and benefit of the action.Citation37,Citation39 Similarly, studies in Ethiopia and other African countries showed that not being emotionally prepared, getting tested after current illness is improved, and a need to consult with their spouses before being tested were common reasons to refuse testing.Citation19,Citation20,Citation22,Citation53 Some other studies showed that those individuals who talk to others about HIV/AIDS and have open discussion about HIV/STI with partners (access to cues to testing) were more prepared to be tested.Citation30,Citation52 In this study, cues to HIV testing showed significant reduction in dimensions of perceived barriers to HIV testing. According to behavior change theories, cues to action is regarded as a strategy to increase readiness.Citation37–Citation39
In this study disagreement over disclosure of HIV positive test results showed a negative effect on refusal of PIHT when adjusted with other HM constructs. However, studies showed that a higher concern for nondisclosure and an interest in keeping confidentiality was associated with refusal of testing. These studies simultaneously indicated that a client’s perception of how confidentiality is handled may influence their willingness to be tested.Citation1,Citation26,Citation28 This perhaps indicates that the relationship between non-disclosure concern and refusal of PIHT is modified by the extent to which preferred condition to undergo testing is met for clients; for example, testing when a closely known person is around. Perhaps for many clients who had visited the study facilities from places other than the study town, were more comfortable to undergo testing. Clients self efficacy to live with HIV was observed as one of the predictors to reduce refusal of PIHT. According to HBM, people will engage in healthy behavior if they are confident in being able to successfully undertake and cope with it. It works by reducing perceived barriers and improving positive effect of perceived benefits.Citation37–Citation39 Likewise self efficacy in this study showed statistically significant positive relationship with perceived benefits and negative relationship with perceived barriers of testing (see ).
In this study, none of the potential behaviors that expose a person to HIV/AIDS predicted HIV testing. Similarly, a study in Southern African countries on HIV testing showed HIV risk factors like multiple partners and lack of condom use were not associated with intention to be tested for HIV.Citation52 This is also supported by the concept of HBM that perceiving susceptibility is better than real susceptibility in facilitating preventive health behavior. This study found self reported ever and/or recent experience of HIV testing to be one predictor to facilitate refusal of PIHT. Similarly, many studies on routine testing showed prior testing, and several times, negative results were among common reasons for declining testing.Citation20,Citation22,Citation50,Citation51 In this study, clients’ psychosocial contexts during interaction with providers determined testing in OPDs. Obedience to provider, perception that providers selectivity initiate only when they suspect clients for HIV, and explicitness of opt-out right protected from refusing PIHT. Similarly, a survey in Botswana regarding routine optout testing shows even though the majority of respondents reported that routine testing was beneficial, about 68% felt that they could not refuse a test offered by their provider.Citation1 There is also a psychological tendency to obey health providers because of the high social status they assume. Thus, clients intentionally or unintentionally may not really opt-out of PIHT.Citation54
Regarding the sociodemographic characteristics of clients and testing, in this study, being a small town and rural resident in Jimma zone were found to reduce likelihood of refusing PIHT, while none of the other sociodemographic variables had an adjusted effect on refusal of PIHT. A study conducted in Uganda hospitals showed no signif icant demographic differences between patients who declined and accepted testing.Citation22 Even though there may be a risk of ecological error, the potential reason for higher significant acceptance among rural residents compared with Jimma town residents may be related to the reduced barriers of feeling discomfort, as rural residents had a significantly lower mean of unmet preferred conditions of testing [mean difference (MD) (95% CI) = −0.36 (−0.52 to −0.17), P < 0.01], and small towns had a statistically significant higher mean of health motivation than Jimma town residents [MD (95% CI) = 0.47 (0.18–0.76), P < 0.01].
This study has some limitations. There was reporting bias, particularly when questions were more personalized than when asked in general terms. Regarding the HBM constructs, the regression coefficient was used to see only the relationship between the variables. However, the regression cannot establish the over all structure of the relationship among all constructs at all times.
Conclusion
This study predicted refusal of HIV testing in adult OPDs by 62.5%. HBM alone explained 43.6% of clients’ PIHT decisions. Context modified the prediction ability of HBM. Clients’ psychosocial factors related with HIV/AIDS and testing, personal factors, and perceived contexts in OPDs influenced the decision for provider-initiated HIV testing. Clients with perception of susceptibility to HIV are less likely to refuse PIHT. This indicates the existence of HIV unscreened errors in the community. The provider-initiated testing is a good opportunity to not miss clients on their visit to a health facility. Perceived barriers, particularly unpreparedness for testing best determines refusal of PIHT. Clients’ perceived social severity of HIV/AIDS is associated with increased perception of barriers to undergo PIHT; feeling unprepared for testing and otherwise seeking more comfortable condition to undergo testing. This especially works for clients undergoing testing around their place of residence. On the other hand, exposure to cues to HIV testing (eg, from media and interpersonal discussions) reduces the feeling of unpreparedness and refusal of testing. Increased self efficacy to live with HIV and creating a supportive attitude towards ART, particularly in terms that help clients acknowledge the importance of early testing, reduce perceived barriers and can normalize testing. Clients’ feeling self obedience to providers and providers’ approach in explicitly indicating testing is right based facilitate acceptance of PIHT. without acknowledging the benefits of testing. Providers explicit (more informative) and efficacy-equipped approach of encouraging testing is better than simple initiation. It reduces the sense of mere obedience to the provider, and unhealthy actions that may follow in cases where clients get positive test results without being convinced what to do. In addition, importance of early testing during initiation, continued cues via media, and local discussions on issues of HIV and testing, even outside of the health facilities, are of particular value.
Authors’ contributions
YK conceived and designed the study. ZB, LA, and YK drafted the manuscript. AG and ZB participated in the critical review of the manuscript. All authors gave their final approval of the version of the manuscript submitted for publication.
Acknowledgments
The authors acknowledge Jimma University for funding the study. Furthermore, authors thank clients who responded for the study, the data collectors, and members of staff of the health facilities who organized situations for, and assisted the process of, data collection.
Disclosure
The authors declare that they have no competing interests.
References
- WeiserSHeislerMLeiterKRoutine HIV testing in Botswana: a population-based study on attitudes, practices and human rights concernsPLoS Med200637e26116834458
- WHOInvesting in a comprehensive health sector response to HIV/AIDS – scaling up treatment and accelerating prevention2004
- UNAIDSWHO Global AIDS epidemics update2008/2009
- MawarNSahaSPanditAMahajanUThe third phase of HIV pandemic: social consequences of HIV/AIDS stigma and discrimination and future needsIndian J Med Res2005122647148416517997
- Commission on HIV/AIDS and Governance in AfricaAfrica: the socio-economic impact of HIV/AIDSEconomic commission of Africa Available from: http://www.uneca.org/chga/maputo/socio_eco_impact.pdfAccessed June 22, 2012
- UNAIDS, WHO HIV/AIDS ProgrammeGuidance on provider-initiated testing and counseling in health facilitiesWorld Health Organization52007 Available from: http://whqlibdoc.who.int/publications/2007/9789241595568_eng.pdfAccessed 2008
- USAIDThe US Agency for International Development works in partnership with the US President’s Emergency Plan for AIDS Relief http:www.globalhealthfacts.org/topic/map.aspx?ind=53
- MOHUganda national policy guidelines for HIV counselling and testing22005
- BransonBCurrent HIV epidemiology and revised recommendations for HIV testing in health-care settingsPublic Health Rep2007122557958317877304
- WHOPerspective in public healthScaling up HIV testing and counseling in Asia and the pacific. Report of a technical consultation PhnomCambodiaJune 4-6, 2007
- BlakeSJRisky Rhetoric: AIDS and the cultural practices of HIV testingCarbondaleSouthern Illinois University Press2003
- WHO/UNAIDS/UNICEFGlobal AIDS Epidemics2007
- AndersonJEMosherWDChandraAMeasuring HIV risk in the US population aged 15–44: results from Cycle 6 of the National Survey of Family Growth2006377127
- KeineMSBateganyaMWanyenzeRLuleHMayerKSteinMProvider-initiated HIV testing in health care settings: should it include client-centered counselling?SAHARA J20096311511920485851
- WHOTreat 3 million by 2005 “3 by 5 initiatives”. Available from: http://www.who.int/3by5/Accessed June 22, 2012
- JasonOOnsembeEthiopia situation analysis on population, reproductive health and genderUNFPA. CSA. Addis Ababa122005 http:www:unfpa.org/pds/PSA_Guide.pdf
- Federal HIV/AIDS Prevention and Control Office [Ethiopia]Guidelines for HIV counseling and testing in EthiopiaFHAPCO72007
- Centers for Disease Control (CDC)Publicly funded HIV counseling and testing – United States, 1990MMWR Morb Mortal Wkly Rep1991406666696751654500
- FeteneNWFelekeADMissed opportunities for earlier HIV testing and diagnosis at the health facilities of Dessie town, North East EthiopiaBMC Public Health20101036220573215
- MselekuMSmithTHGuidozziFHIV sero positive in pregnant South African women who initially refuse routine antenatal HIV screeningBJOG2005112337037115713157
- MossdorfEStoeckleMVincenzAImpact of a national HIV voluntary counselling and testing (VCT) campaign on VCT in a rural hospital in TanzaniaTrop Med Int Health201015556757320345555
- WanyenzeRKNawavvuCNamaleASAcceptability of routine HIV counselling and testing, and HIV sero prevalence in Ugandan hospitalsBull World Health Organ200886430230918438519
- UNAIDSUniting the world against AIDS2007 Available from: http://data.unaids.org/publications/irc-pub07/jc1248-overviewbrochure_en.pdfAccessed June 22, 2012
- World Health OrganizationTowards universal access: scaling up priority HIV/AIDS interventions in the health sector: progress report2008 Available from: http://www.who.int/hiv/pub/towards_universal_access_report_2008.pdfAccessed May 19, 2009
- WangYLiBZhengJFactors related to female sex workers’ (FSWs) willingness to utilize VCT service: a qualitative study in Jinan city, northern ChinaAIDS Behav200913586687218770027
- ObermeyerCMOsbornMFraming health matters. The utilization of testing and counseling for HIV: a review of the social and behavioral evidenceAm J Public Health200797101762177417761565
- WHO, United Nations Children’s Fund, UNAIDSTowards universal access: scaling up priority HIV/AIDS interventions in the health sectorProgress report2009GenevaWHO2009
- AyenewALeykunAColebundersRDeribewAPredictors of HIV testing among patients with tuberculosis in North West Ethiopia: a case-control studyPLoS One201053e970220300574
- JereneDEndaleALindtjørnBAcceptability of HIV counselling and testing among tuberculosis patients in south EthiopiaBMC Int Health Hum Rights20077417537265
- TasewTFactors affecting acceptance of HIV testing among antenatal care attendees: with emphasis of the role of male partners in Wolaita ZoneEPHA sponsored Master’s Thesis extracts on HIV/AIDS Extract number 9120102131
- RakgoasiSDHIV counselling and testing of pregnant women attending antenatal clinics in BotswanaBotswanaDepartment of Population Studies, University of Botswana2001
- Centers for Disease Control and Prevention (CDC)Advancing HIV prevention: new strategies for a changing epidemic – United States, 2003MMWR Morb Mortal Wkly Rep20035232933212733863
- DenisonJAO’ReillyKRSchmidGPKennedyCESweatMDHIV voluntary counseling and testing and behavioral risk reduction in developing countries: a meta-analysis, 1990–2005AIDS Behav20081236337318161018
- KabiruCWLukeNIzugbaraCOZuluEMThe correlates of HIV testing and impacts on sexual behavior: evidence from a life history study of young people in Kisumu, KenyaBMC Public Health20101041220624323
- MishraVHongRGovindasamyPMontanaLEvaluating HIV seroprevalence estimates from Ethiopia: further analysis of the 2005 Ethiopia demographic and health surveyCalverton, MDMacro International2008
- KabatoTAssessment of determining factors for acceptance of HIV testing among pregnant women at antenatal care setting in Arbaminch town, Southern EthiopiaEPHA sponsored Master’s Thesis extracts on HIV/AIDS Extract number 9120108393
- GlanzKRimerBKLewisFMHealth Behavior and Health Education: Theory, Research and PracticeSan FranciscoWiley and Sons2002
- GlanzKRimerBKTheory at a Glance: a guide to health promotion practices2nd edNational Cancer Institute, US Department of Health and Human Services2005
- RosenstockIHistorical origins of the health belief modelHealth Educ Monogr197424328335
- AyranciUAIDS knowledge and attitude in Turkish populationBMC Public Health200559516159400
- AIDSCAP/WHO/CAPS instrument Counselors 6 month follow up questionnaire http://www:caps.ucsf.edu/uploads/tools/survey/index.php
- LeiliSElhamSFarkhondehSA population-based survey of HIV/AIDS knowledge and attitudes in general public, Bandar-Abbas, IranPak J Med Sci2008246 Pt 2838844
- World Health Organization (WHO)HIV testing, treatment and prevention: generic tools for operational researchGenevaPopulation Council, WHO2009
- AIDSCAP/WHO/CAPS instrumentHealthy Oakland teens survey on thoughts, opinions, and feelings about health and what you do to stay healthy1994 http://www:caps.ucsf.edu/uploads/tools/survey/index.php
- Saarc J tuberPerception and knowledge about HIV/AIDS among students in a medical college in western NepalSAARC Journal of Tuberculosis, Lung Diseases and HIV/AIDS200921116
- AIDSCAP/WHO/CAPS Counseling and Testing Efficacy Study: Counselling and Testing Baseline Instrument http://www:popcouncil.org/Horizons/ORTookit/.../ssaids.capvct.html
- KakokoDCLugoeWLLieGTVoluntary testing for HIV among a sample of Tanzanian teachers: a search for socio-demographic and socio-psychological correlatesAIDS Care200618655456016831782
- WalkerLComponents of the health belief model and HIV testing decisionsA thesis submitted to the University of North Carolina at Wilmington in partial fulfillment of the requirements for the Degree of Master of ArtsUniversity of North CarolinaWilmington2004
- ObiajuluACKnowledge, Attitude and Practice of Voluntary Counseling and Testing for HIV/AIDS amongst the health professionals in Maphumulo hospital, iLembe district, Kwazulu-natal provinceA research report submitted in partial fulfillment of the requirements for the award of the degree of masters of family medicine of the University of Limpopo http://www:ul.netd.ac.za/bitstream/10386/209/1/Dr%20Obialulu%20final.pdf
- IrwinKLValdiserriROHolmbergSDAcceptability of voluntary HIV antibody testing: a decade of lessons learned as of 1985 to 1995AIDS Behav2009155866872
- ChinazoOBethanyDJosephDRobertDRaminAGalitSRoutine opt-out HIV testing in an urban community health centerAIDS Patient Care STDS200923861962319591606
- MitchellSCockcroftALamotheGAnderssonNEquity in HIV testing: evidence from a cross-sectional study in ten Southern African countriesBMC Int Health Hum Rights2010102320836859
- OsmanNGender differences in the use of youth-friendly VCT services in MozambiqueICASA2003
- BeckerJTsagueLSahaboRTwymanPProvider initiated testing and counseling (PITC) for HIV in resource-limited clinical settings: important questions unansweredPan Afr Med J20093421532713