Abstract
Introduction
Understanding factors affecting the time to recovery from acute mania is critical in the management of manic syndromes. The aim of this study was to determine the effect of HIV infection on time to recovery from acute mania.
Methods
We performed a retrospective study in which medical charts of individuals who were treated for acute mania were reviewed. Survival analysis with Cox regression models were used to compare time to recovery from an acute manic episode between human immunodeficiency virus (HIV)-positive individuals and HIV-negative individuals.
Results
Median survival time was one week for HIV-positive individuals and more than four weeks for HIV-negative individuals (χ2 = 18.4, P value = 0.000). HIV infection was the only marginally significant independent predictor of survival probability on the acute admission ward (hazards ratio 2.87, P = 0.06).
Conclusion
Acute mania in HIV-infected persons responds faster to psychotropic drugs compared with that in HIV-negative persons.
Introduction
In the past five years, an increasing body of evidence has accumulated describing the mental health problems of persons living with immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) in Uganda.Citation1–Citation5 These problems may be pre-existing mental illnesses in an individual who becomes secondarily infected with HIV or they may develop because of the direct or indirect effects of the HIV virus on the brain.Citation6 For example, we have previously described the clinical presentation of individuals with acute mania and HIV infection.Citation7 Our research has shown that such individuals could have HIV-related secondary mania or bipolar disorder mania. HIV-positive individuals with bipolar disorder mania had more cognitive impairment, more immune suppression, more severe respiratory tract infections, and more current use of antituberculosis therapy compared with individuals with HIV-related secondary mania.Citation7
Hospital data consistently show that bipolar disorder is the most common mental disorder seen at Butabika Hospital, Uganda’s only psychiatric hospital, accounting for 30%–35% of all first psychiatric hospitalizations annually. The prevalence of HIV infection among individuals with a first psychiatric hospitalization for severe mental disorder is estimated at 18%, which is three times the rate in the general population.Citation8 The literature on treatment outcomes of HIV-positive individuals with severe mental illness, such as bipolar disorder, is limited in low-resource settings like Uganda.
In the context of HIV/AIDS, descriptive and treatment studies of acute mania in HIV-infected persons is lacking in developing countries. In developed countries, comprehensive reviews of the literature have provided compelling evidence that both typical and atypical antipsychotics are effective in the treatment of manic episodes in mentally ill, HIV-infected individuals.Citation9–Citation11 However, the literature on the effect of HIV infection in response to these treatments is limited. No study has compared the recovery time of HIV-positive individuals with acute mania with that of HIV-negative individuals with acute mania. Studies that we have performed comparing the clinical presentation of bipolar disorder mania versus that of HIV-related mania provided us with an opportunity to investigate the effect of HIV infection on time to recovery from an acute manic episode retrospectively. From our previous crosssectional studies, we had noted a quicker response to psychotropic drugs among HIV-positive individuals compared with HIV-negative individuals with an acute manic episode.Citation12
The aim of this study was to explore this finding further, using a survival analysis technique, and investigate its clinical implications in the care of HIV-positive individuals in Uganda and other low-resource settings. We hypothesized that individuals with HIV infection would have a shorter time to recovery from an acute manic episode compared with those without HIV infection.
Material and methods
A random subsample of 60 medical charts were obtained from a sample of 155 medical charts of patients who, in 2004–2006, had participated in a previous study that described the clinical presentation of bipolar disorder mania in Butabika hospital.Citation7 To obtain a random sample, we made a list of inpatient identification numbers for patients who had participated in the previous study. Unique numbers 1–155 were assigned to each inpatient number. Pieces of paper labeled with these unique numbers were placed in a box and on each day of data collection, research assistants randomly picked 10 pieces of paper. The inpatient number corresponding with the number on the piece of paper was then used to trace the medical chart from the medical records office. Research assistants reviewed the medical charts and extracted data on variables of interest in this study. Medical charts that had incomplete data on variables of interest were excluded from the study. This process was repeated until we obtained a subsample of 60 medical charts.
These medical charts belonged to individuals aged 18 years and older, with a first episode of acute mania and without a history of substance or alcohol dependence. In addition, these study participants had not met the Diagnostic and Statistical Manual for Mental Disorders, Fourth edition (DSM-IV) criteriaCitation13 for delirium or a substance use disorder, and were not in the puerperium period. They had to have a laboratory record of their HIV serostatus, and a record of the dates of admission and discharge from the acute admission ward. In addition, study participants had to have sufficient data on other explanatory variables of interest including gender, age, years of education, source of referral, and treatment combination (whether patient was treated with an antipsychotic alone or in combination with a mood stabilizer or other drug).
The outcome of interest was time from psychotropic drug initiation (on the date of admission) to discharge from the acute admission ward. The decision to discharge a patient is made during major ward rounds that are conducted twice a week. The psychiatrist in charge of an acute admission ward, together with other members of the psychiatric team, carry out assessments based on DSM-IV criteria and make a decision as to whether a patient is fit for discharge or not. For acute mania, the decision to discharge an individual who was admitted with acute mania is based on the absence of all DSM-IV criteria for manic symptoms that were present at the time of admission. In this study, the “failure event” was considered as being discharge within four weeks of the date of admission. The Butabika Hospital Research Committee approved the study.
Statistical analysis
Statistical analysis was performed using Stata 10.0 (Stata Corp., College Station, TX).
Bivariate analyses were conducted to identify demographic and clinical variables that were significantly correlated with HIV-positive status at the time of admission. We used Chi-square tests or Fisher’s Exact test for qualitative variables, and independent sample t-tests for continuous variables.
We computed Kaplan-Meier estimates and log-rank Chi-square tests to determine the impact of study variables on survival in the acute admission wards. Study variables that were statistically significantly associated with HIV status and survival at P < 0.05 were entered into a Cox regression model to control for their effect when assessing the effect of HIV infection on time to recovery from an acute manic episode. We used graphical methods and Schoenfeld residuals to assess the proportional hazards assumption.
Results
There were 60 records selected for the study, but eight records did not have laboratory confirmation of HIV status, so were excluded from the data analysis. The majority of the study participants were HIV-positive (65.4%) and female (70%). The mean age was 33.6 (standard deviation [SD] 6.9, range 23–55) years. Sixty percent of the participants had more than eight years of formal education, indicating that they had at least attained secondary education level and above. Physicians and general practitioners had referred 34% of the study sample.
Among HIV-positive individuals, the mean CD4 count was 206 (SD 75.5, range 48–332). None of the HIV-positive individuals had initiated antiretroviral therapy prior to admission. Overall, 39 individuals with acute mania were discharged within four weeks of admission. The study participants had a median time to recovery of 2.35 weeks (mean 2.5, SD 1.59, range 3.5 days–5.0 weeks). Sixty percent of the study participants received monotherapy with one antipsychotic drug, either haloperidol or chlorpromazine. The relationship between the study variables and HIV infection among patients with acute mania is shown in .
Table 1 The relationship between study variables and HIV infection among patients with acute mania
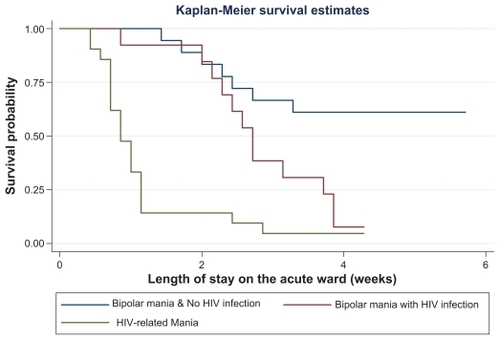
and show the Kaplan-Meier estimates of the survival distribution of time to discharge by HIV status and by mania status, respectively. Median survival time was one week for HIV-positive individuals and more than four weeks among HIV-negative individuals. These differences were statistically significant by the log-rank tests (χ2 = 18.4, P = 0.000 and χ2 = 33.6, P = 0.000, respectively). Individuals with HIV-related mania had the shortest median survival time of six days. Males had a median survival time of 3.7 weeks, whereas females had a survival time that averaged two weeks (log-rank test χ2 = 4.97, P = 0.03). Individuals over 30 years of age had a median survival time of 1.1 weeks whereas younger individuals had a survival time that averaged 2.7 weeks (log-rank test χ2 = 7.25, P = 0.007). Individuals referred from general hospitals and clinics had a median survival of one week while those brought by relatives had a median survival time of 3.1 weeks (log-rank test χ2 = 7.11, P = 0.03). Individuals who had monotherapy with one antipsychotic drug had a median survival of one week, whereas those who had combination therapy with two antipsychotics or an antipsychotic and a mood stabilizer had a median survival time of 3.3 weeks (log-rank test χ2 = 11.5, P = 0.001).
Figure 1 Kaplan-Meier estimates of the distribution of time until discharge from the admission wards (by HIV status) among individuals admitted with an acute episode of mania.
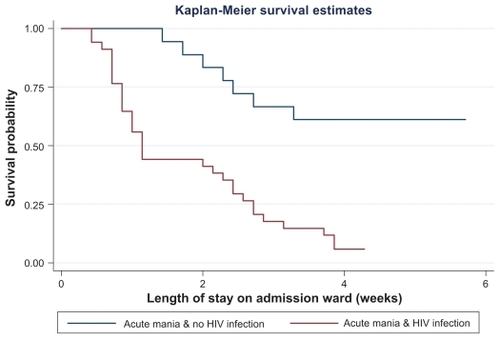
Figure 2 Kaplan-Meier estimates of the distribution of time until discharge from the admission wards (by mania status) among individuals admitted with an acute episode of mania.
Abbreviation: HIV, human immunodeficiency virus.
shows the Cox proportional hazard models for covariates with rate of discharge from acute admission wards. After controlling for study variables that were associated with both HIV and survival probability on the admission wards, HIV infection remained the only marginally significant independent predictor of survival probability on the acute admission wards (P = 0.06).
Table 2 Cox proportional hazard regression models
Discussion
HIV infection emerged as the only marginally significant independent predictor of survival time on the acute admission ward for individuals admitted with acute mania. Individuals with HIV-related mania had the shortest stay on the acute admission ward compared with those with bipolar mania regardless of HIV status. These findings strengthen previous theories that mania secondary to the pathophysiologic effects of the HIV virus on the brain may be different from bipolar mania in HIV-negative individuals.Citation14,Citation15 HIV-related mania appears to be more responsive to psychotropic drugs than mania in HIV-negative individuals. Previous studies have shown that HIV-related mania is responsive to both typical and atypical antipsychotics,Citation16 –Citation18 benzodiazepines such as clonazepam,Citation19 and electroconvulsive therapy.Citation20 However, none of these studies compared responses to these psychotropic drugs between HIV-positive and HIV-negative individuals.
There are several limitations to our study. First, the study sample is small and thus may not have sufficient power to detect significant findings. Second, generalization of the findings to other HIV-positive populations is limited because this was a hospital-based study. Third, we could not control for nonadherence, critically ill status, or poor access to care. Finally, we did not have information on prior treatments given before referral to the psychiatric hospital that may have affected outcomes in this study.
Within the context of these limitations, this study points out important clinical implications for the care of HIV-positive individuals in Uganda. The rapid response to psychotropic drugs indicates that if prompt diagnosis of HIV-related manic symptoms is made, then treatment can be given in general medical settings. This will prevent affected individuals from progressing to severe manic states that may disrupt compliance with their treatment regimens. However, such evaluations can only be realized if providers of HIV care have adequate mental health communication skills. Comanagement of mental health problems should be an integrative part of HIV treatment and prevention programs.
We conclude that acute mania in HIV-infected persons responds faster to psychotropic drugs compared with responses in HIV-negative persons. Further prospective studies of treatment of mental health problems in HIV-infected persons should be pursued aggressively to inform the holistic management of HIV-positive individuals in Uganda.
Disclosure
The authors report no conflict of interest in this work.
References
- SacktorNCWongMNakasujjaNThe International HIV Dementia Scale: A new, rapid screening test for HIV dementiaAIDS2005191367137416103767
- WongMHRobertsonKNakasujjaNFrequency of and risk factors for HIV dementia in an HIV clinic in sub-Saharan AfricaNeurology200768535035517261681
- MusisiSKinyandaEPsychiatric problems of HIV/AIDS and their management in Africa Makerere UniversityKampalaFountain Publishers2009
- MusisiSKinyandaEEmotional and behavioral disorders in HIV seropositive adolescents in urban UgandaEast Afr Med J2009861162419530544
- Nakimuli-MpunguEMusisiSKiwuwa MpunguSKatabiraEEarly-onset versus late-onset HIV-related secondary mania in UgandaPsychosomatics200849653053419122130
- CruessDGEvansDLRepettoMJGettesDDouglasSDPetittoJMPrevalence, diagnosis, and pharmacological treatment of mood disorders in HIV diseaseBiol Psychiatry200354330731612893106
- Nakimuli-MpunguEMusisiSMpunguSKKatabiraEClinical presentation of bipolar mania in HIV-positive patients in UgandaPsychosomatics200950432533019687171
- MalingSGrosskurthHMusisiSOnenTHIV infection among firsttime admission patients with severe mental illness at Butabika and Mulago HospitalsProceedings from the Makerere University Faculty of Medicine, First Annual Scientific ConferenceNov 24–26 2005Entebbe, Uganda
- RepettoMJPetittoJMPsychopharmacology in HIV-infected patientsPsychosom Med200870558559218519881
- VlassovaNAngelinoAFTreismanGJUpdate on mental health issues in patients with HIV infectionCurr Infect Dis Rep200911216316919239808
- AngelinoAFTreismanGJManagement of psychiatric disorders in patients infected with human immunodeficiency virusClin Infect Dis200133684785611512090
- Nakimuli-MpunguEMusisiSMpunguSKKatabiraEPrimary mania versus HIV-related secondary mania in UgandaAm J Psychiatry2006163813491354 quiz 148016877646
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders4th Ed International VersionWashington, DCAmerican Psychiatric Association1995
- LyketsosCGSchwartzJFishmanMTreismanGAIDS maniaJ Neuropsychiatry Clin Neurosci1997922772799144109
- TreismanGFishmanMSchwartzJHuttonHLyketsosCMood disorders in HIV infectionDepress Anxiety1998741781879706455
- SinghANGolledgeHCatalanJTreatment of HIV-related psychotic disorders with risperidone: A series of 21 casesJ Psychosom Res19974254894939194023
- EllenSRJuddFKMijchAMCockramASecondary mania in patients with HIV infectionAust N Z J Psychiatry199933335336010442791
- MijchAMJuddFKLyketsosCGEllenSCockramASecondary mania in patients with HIV infection: Are antiretrovirals protective?J Neuropsychiatry Clin Neurosci199911447548010570761
- BudmanCLVandersallTAClonazepam treatment of acute mania in an AIDS patientJ Clin Psychiatry19905152122335499
- FerrandoSJNimsCHIV-associated mania treated with electroconvulsive therapy and highly active antiretroviral therapyPsychosomatics200647217017416508032