Abstract
Background
Large segments of the hypertensive population in the world are either untreated or inadequately treated. The incidence of heart failure and mortality from cardiovascular complications of hypertension is high among patients with uncontrolled blood pressure (BP). But BP control status of hypertensive patients has not been investigated in the study area. The study aimed to assess BP control status and determinant factors among adult hypertensive patients on antihypertensive medication attending outpatient follow-up at University of Gondar Referral Hospital, northwest Ethiopia.
Methods
An institution-based retrospective follow-up study was conducted from September 2015 to April 2016. Data were collected using a structured and pretested questionnaire adopted from the World Health Organization STEPwise approach. BP records of 6 months were used, and patients were classified as having controlled BP if their BP readings were <140/90 mmHg for all adults ≥18 years of age and <150/90 mmHg for adults aged ≥60 years. A generalized estimating equation was fitted, and the odds ratio with a 95% confidence level was used to determine the effect of covariates on BP control status.
Results
Among 395 participants, 50.4% (95% CI: 45–55) of them controlled their BP in the last 6 months of the survey. Physical activity (adjusted odds ratio [AOR]=1.95, 95% CI: 1.41–2.68), duration on antihypertensive drugs of 2–4 years (AOR=1.70, 95% CI: 1.13–2.56) and 5 years or more (AOR=1.96, 95% CI: 1.32–2.92), and high adherence (AOR=2.18, 95% CI: 1.14–4.15) to antihypertensive drugs were positively associated with BP control, while salt intake (AOR=0.67, 95% CI: 0.49–0.93), overweight (AOR=0.50, 95% CI: 0.36–0.68), and obesity (AOR=0.56, 95% CI: 0.36–0.87) were inversely associated with BP control.
Conclusion
In this study, only half of the hypertensive patients controlled their BP. Thus, health care providers need to be made aware about the importance of counseling hypertensive patients on drug adherence, moderate physical activity, and salt restriction to improve BP control.
Introduction
Hypertension (HTN) is a condition where systolic blood pressure (SBP) is ≥140 mmHg or diastolic blood pressure (DBP) is ≥90 mmHg.Citation1 HTN disproportionately affects populations in low- and middle-income countries where health systems are weak. As it rarely causes symptoms in the early stages, many people go undiagnosed. Those who are diagnosed may not have access to treatment and may not be able to successfully control their illness over the long-term. Significant health and economic gains are attached to early detection, adequate treatment, and good control of HTN.Citation2
The global prevalence of raised BP in adults aged 18 years and above was around 22% in 2014.Citation3 In Sub-Saharan Africa, an estimated 74.7 million individuals are hypertensive, and by the year 2025, the number of hypertensive individuals is projected to increase by 68% to 125.5 million individuals.Citation4
HTN doubles the risk of cardiovascular diseases, such as coronary heart diseases, congestive heart failure, stroke, renal failure, and peripheral arterial diseases.Citation1 Globally, cardiovascular disease accounts for ~17 million deaths a year, nearly one-third of the total deaths. Of these, complications of HTN account for 9.4 million deaths and 7% of the disease burden worldwide every year. HTN is responsible for at least 45% of the deaths due to heart disease and 51% of deaths due to stroke. There is strong scientific evidence on the health benefits of lowering BP through behavioral and pharmacological interventions.Citation5
The incidence of heart failure and mortality from cardiovascular complications of HTN is high among patients with uncontrolled BP.Citation6 In some age groups, the risk of cardiovascular disease doubles for each increase of 20 mmHg in SBP and 10 mmHg in DBP starting from 115/75 mmHg. Treating SBP and DBP until they are less than 140/90 mmHg is associated with a reduction in cardiovascular complications.Citation7
The control of high BP is critical in managing hypertensive patients. Although antihypertensive therapy clearly reduces the risks of cardiovascular and renal diseases, large segments of the hypertensive people are either untreated or inadequately treated.Citation1 Worldwide, the detection, treatment, and control of HTN are inadequate.Citation3
According to the World Health Organization (WHO), approximately one billion persons are living with uncontrolled HTN worldwide.Citation5 Many studies in different parts of the world show that uncontrolled BP is a common phenomenon among hypertensive patients on treatment.Citation8–Citation11 Thus, BP was controlled for only less than 50% of the hypertensive patients in Japan,Citation12 31.7% in Turkey,Citation13 and 48.3% in Malaysia.Citation14 Controlling BP is a difficult experience in Africa too; BP control was accomplished for only 47.7% of the hypertensive patients on follow-up in Tanzania,Citation15 35.9% in Uganda,Citation16 32.8% in Zimbabwe,Citation17 33.4% in Kenya,Citation18 and 40.1% in Addis Ababa, Ethiopia.Citation9
Many socioeconomic, behavioral, and clinical factors affect BP control. Thus, BP is less likely to be controlled among unmarried,Citation19 male,Citation20 elderly,Citation18 less educated,Citation14 low-income,Citation17 rural,Citation9 and unemployedCitation17 patients. Smoking,Citation13,Citation17 salt addition habit in meal,Citation9 and alcohol drinkingCitation17 are associated with poor BP control, whereas vegetable consumption habitCitation21 and moderate physical activityCitation22,Citation23 are important behaviors to control BP. Having other comorbidities, like diabetes mellitus (DM) or renal diseases,Citation12–Citation14 low adherence to anti-hypertensive treatments,Citation9,Citation15,Citation20,Citation24 obesity/overweight,Citation13,Citation15,Citation17 being on multidrug regimen,Citation14,Citation18,Citation20 and lack of information on complications of HTN are also other factors associated with poor BP control.
HTN has become an important chronic noncommunicable disease with increasing trends in developing countries, and uncontrolled BP will result in life-threatening complications. So, knowing the BP control status of hypertensive patients is very important for policy makers and clinicians responsible for designing appropriate strategies for a better management of hypertensive patients. Therefore, this study aimed to assess BP control status and associated factors among adult hypertensive patients on outpatient follow-up at University of Gondar Referral Hospital (UOGRH), northwest Ethiopia, 2016.
Methods
Study setting and design
A 6-month institution-based retrospective follow-up study was conducted from September 2015 to April 2016 at UOGRH Chronic Illness Clinic. UOGRH is a teaching hospital located in Gondar town, North Gondar Administrative Zone, Amhara National Regional State, 727 km from Addis Ababa, the capital of Ethiopia. UOGRH provides service for about more than five million people in North Gondar Zone and the neighboring zones, West Gojjam and south Tigray.
Sample size and sampling procedure
All adult hypertensive patients who were on outpatient follow-up for at least 6 months and had at least one documented BP measurement result were eligible for the study. Then, all 403 patients who came for follow-up during the data collection period were included in the study.
Data collection instrument and procedure
A structured interviewer-administered questionnaire adopted from the WHO STEPwise approach for chronic disease risk factor surveillanceCitation25 was used to collect data. The questionnaire was first prepared in English and translated into the local language (Amharic) and finally back to English to maintain consistency. A pretest was conducted on 10% of the sample size out of the study area before the actual data collection. Data collectors and supervisors were trained for 2 days. Two health officer supervisors and three graduate nurses data collectors were recruited for data collection. The process was closely monitored by the principal investigator and supervisors throughout the data collection period. Filled copies were checked daily for completeness of information, and problems were immediately communicated to data collectors.
Assessment of BP control status
BP recordings in the charts of adult hypertensive patients for the last 6 months were reviewed. The last BP was measured by the data collectors using a standard mercury sphygmomanometer BP cuff with the appropriate cuff size that covered two-thirds of the upper arm, while the patient was in a sitting position, had rested for at least 5 minutes, and consumed no cigarettes or caffeine 30 minutes before the measurement. Two consecutive measurements were taken in a minimum interval of 5 minutes, and the mean was recorded. Patients were classified as having controlled BP at each visit with BP readings <140/90 mmHg for all adults ≥18 years old, and <150/90 for adults aged ≥60 years.Citation26 Then, the BP recordings at each visit were used as dependent variable, but the prevalence of controlled BP was determined by the average BP recordings across the 6 months.
Assessment of adherence to antihypertensive treatment
Adherence to antihypertensive drugs was measured by the four-item Morisky–Green–Levine Scale, which measures both deliberate and unintended adherence grounded on forgetfulness, carelessness, stopping medication when feeling better, and stopping medication when feeling worse. The response categories were either “yes” or “no” for each item. On the whole, 0 point was allocated to a “yes” response and 1 point to a “no” response. The total score ranged from 0 (nonadherent) to 4 (adherent). Then patients were categorized as having high (score=4), medium (score=2–3), and low adherence (score ≤1).
Assessment of physical activity and other behavioral factors
Work or sports that involves moderate-intensity activity that causes small increases in breathing or heart rate, such as brisk walking, carrying light loads, cycling, swimming, volley ball, dancing, gardening, and house working for at least 10 minutes continuously per day, was considered as moderate physical activities.
A participant who smoked at least one cigarette per day at the time of the study was considered as smoker. Male patients who drank more than 2 units of alcohol/day and female patients who drank more than 1 unit of alcohol/day were considered as alcohol consumer.
Fruit and vegetable eating habits of patients were assessed and categorized by dividing the number of days they ate per week into three groups: those who ate for less than 1 day/week (none), 1–3 days/week, and 4–7 days/week.
Assessment of wealth index and knowledge
Household wealth index was determined using Principal Component Analysis (PCA) by considering household assets, such as quantity of cereal products, house, livestock, and agricultural land ownership.Citation27 First, variables were coded between 0 and 1; then variables were entered and analyzed using PCA, and those variables with a communality value of greater than 0.5 were used to produce factor scores. Finally, factor scores were summed and ranked into “poor”, “medium”, and “rich” categories. Knowledge about HTN and its complications was assessed using eight-item questions; also, PCA was used to rank patients knowledge into “poor”, “medium”, and “good”.
Body mass index (BMI) and waist circumference (WC) measurements
Weight was measured with participants standing bare foot, wearing light clothing, and was recorded to the nearest 0.1 kg. Height was measured with participants standing upright with the head in Frankfort plane and was recorded to the nearest 0.5 cm. Then, BMI was calculated by dividing weight in kg to height in m2, and patients were categorized into underweight (BMI <18.5), normal (BMI 18.5–24.9), overweight (BMI 25–29.9), and obese (BMI ≥30).Citation28
WC was measured with the subject in a standing position using a nonelastic plastic tape midway between the lower rib margin and the iliac crest to the nearest 1 mm. One layer of clothing was accepted. Based on WC measurements, patients were classified into three health risk categories in accordance with cutoffs recommended by WHO: low risk (men, WC=93.9 cm or less; women, WC=79.9 cm or less); increased risk (men, WC=94.0–101.9 cm; women, WC=80.0–87.9 cm); and high risk (men, WC=102.0 cm or more; women, WC=88.0 cm or more).Citation29
Data processing and analysis
After checking for consistency and completeness, the collected data were entered into EPI-INFO version 3.5.3 and then exported to STATA 12 for analysis. Descriptive and summary statistics were carried out. The generalized estimating equation was fitted with logit link function and binomial family and working correlation structures (independent, exchangeable, unstructured, and autoregressive) were compared for the smallest standard error difference of robust and model-based standard error. Then, the exchangeable correlation structure showed the smallest standard error difference, and was selected for this study to handle the within correlation.
Both crude odds ratio and adjusted odds ratio (AOR) with the corresponding 95% CI were calculated to determine the strength of association between dependent and independent variables. Variables with a p-value ≤0.2 in the bivariable analysis were fitted into the multivariable analysis and variables with a p-value of <0.05 were considered as statistically significant.
Ethical approval and consent to participate
Ethical clearance was obtained from the Institute of Public Health Ethical Review Board, University of Gondar (Ref. No. IPH/2880/2016). Permission letter was obtained from the Hospital’s clinical director and Department of Internal Medicine to conduct the study. Informed verbal consent was obtained from the respondents, and Institute of Public Health Ethical Review Board, University of Gondar, approved the verbal consent process. The right of participants to withdraw from the study at any time was secured. Personal Identifying information was not recorded on the questionnaire, and all information obtained by face-to-face interview as well as from the patients chart was kept confidential.
Results
A total of 403 patients were included in the study of whom 395 responded, a response rate of 98%.
Sociodemographic characteristics of respondents
Of the 395 participants, 244 (61.8%) were females, and the median age of the respondents was 57 years with an IQR of 16 years. Three hundred sixty (91.1%) of the respondents were from Amhara ethnic group and 361 (91.4%) were orthodox Christians. Out of the total respondents, 242 (61.3%) were married, 179 (45.3%) had no formal education, 315 (79.7%) were urban dwellers, and 142 (46%) lay in the rich class wealth index ().
Table 1 Sociodemographic characteristics of adult hypertensive patients on outpatient follow-up at UOGRH, Gondar, northwest Ethiopia, 2016 (n=395)
Behavioral/lifestyle characteristics of respondents
Out of the 395 participants, only three (0.8%) were current smokers and nine (2.3%) were drinking alcohol at the moment. The majority, 226 (57.2%), of the respondents did not eat fruit and 219 (55.4%) ate vegetables 1–3 days/week. Slightly over half (51.4%) of the participants had moderate physical activity on most days of the week. Two hundred thirty-three (59%) of the respondents were using vegetable oil for their usual meal preparation, and 109 (27.6%) used additional salt in their meals ().
Table 2 Behavioral characteristics of adult hypertensive patients on outpatient follow-up at UOGRH, Gondar, northwest Ethiopia, 2016 (n=395)
Clinical characteristics of respondents
Of the total participants, 187 (47.3%) were in the normal BMI range, followed by 129 (32.7%) in the overweight range, and 52 (13.2%) in the obese range. Seventy-four (18.7%) of the participants had a family history of HTN, while 107 (27.1%) had DM and 81 (20.5%) had other complications (cardiac diseases 8.9%, chronic kidney diseases 7.1%, asthma 4.3%, and others 2.6%). Slightly over half (50.6%) of the respondents were on a single antihypertensive drug, whereas the majority (68.9%) were highly adherent to their treatment, and 180 (45.6%) of the participants were on antihypertensive treatment for 5 and more years ().
Table 3 Clinical characteristics of adult hypertensive patients on outpatient follow-up at UOGRH, Gondar, northwest Ethiopia, 2016 (n=395)
Proportion of controlled BP
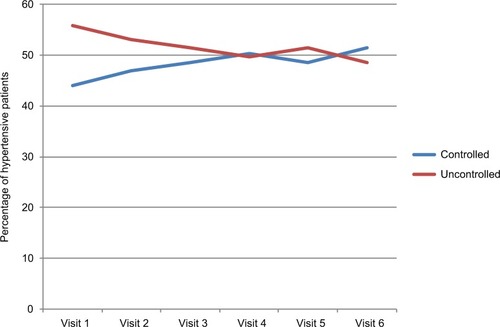
The participants were followed up for an average of 5.8 visits, with a minimum of 3 and a maximum of 6 visits. The mean SBP and DBP readings were 138.38 (±14.06 SD) and 80.73 (±6.26 SD) mmHg, respectively. The overall proportion of controlled BP in the last 6 months was 50.4% (95% CI: 45–55). In the first visit, the BP of 221 (55.9%) patients was uncontrolled, and in the sixth visit, the BP of 51.4% patients was controlled. BP control was relatively low at the first visit, and gradually increased during the consecutive follow-ups ().
Determinant factors of BP control
The generalized estimating equation result showed that moderate physical activity on most days of the week, vegetable consumption habit, duration on antihypertensive treatment, and adherence to antihypertensive drugs were positively associated with controlled BP, whereas salt use and BMI were negatively associated. But factors like age, sex, educational status, wealth index, number of antihypertensive drugs, and presence of comorbidities were not significantly associated with BP control in this study.
Patients who had physical activity on most days of the week were almost two times (AOR=1.95, 95% CI: 1.41–2.68) as likely to have controlled BP compared to patients with no physical activity. Patients who consumed vegetables for 1–3 days/week were two times (AOR=2.24, 95% CI: 1.65–3.06) as likely to have controlled BP compared to patients who did not consume vegetables. Similarly, patients who consumed vegetables for 4–7 days/week were also two times (AOR=2.36, 95% CI: 1.17–4.75) as likely to have controlled BP compared to their counterparts.
The odds of BP control decreased by 33% for hypertensive patients who added salt to their food (AOR=0.67, 95% CI: 0.49–0.93) compared to those who used no salt. At the same time, the odds of BP control decreased by 50% for overweight patients (AOR=0.50, 95% CI: 0.36–0.68) and 44% for obese patients (AOR=0.56, 95% CI: 0.36–0.87) compared to normal or underweight patients.
The odds of BP control were 1.70 times (AOR=1.70, 95% CI: 1.13–2.56) higher for patients who stayed on anti-hypertensive treatment for 2–4 years and 2 times (AOR=1.96, 95% CI: 1.32–2.92) higher for those who stayed for 5 years or more compared to patients with less than 2 years of stay on treatment.
Adherence to antihypertensive drugs was another important variable that showed a significant association with BP control status. Patients who had high adherence to their antihypertensive drugs were two times (AOR=2.18, 95% CI: 1.14–4.15) as likely to have controlled BP as compared to low adherent patients ().
Table 4 Determinant factors of BP control status among adult hypertensive patients on outpatient follow-up at UOGRH, Gondar, northwest Ethiopia, 2016 (n=395)
Discussion
This study revealed that 50.4% of hypertensive patients on outpatient follow-up controlled their BP over the last 6 months. This finding was higher than those of studies conducted in Turkey (31.7%),Citation13 Malaysia (48.3%),Citation14 Tanzania (47.7%),Citation15 Zimbabwe (32.8%),Citation17 Kenya (33.4%),Citation18 Uganda (35.9),Citation16 and similar study in Addis Ababa, Ethiopia (40.1%).Citation9 This difference is probably due to a change in the criteria used to classify hypertensive patients as having uncontrolled and controlled BP. Most of the literatures used JNC7 (which was used as a cutoff point >140/90 for nondiabetic patients and >130/80 for diabetic patients to say uncontrolled BP), and the current study was conducted by using the JNC8 guideline.
On the other hand, the result of this study was lower than those of studies done in Sudan (64%),Citation30 Pakistan (72.3%),Citation31 and this may be attributed to the difference in the study population and the study design.
This study revealed that patients who did moderate physical activity had a greater chance of having controlled BP. This finding is supported by those of studies conducted in People’s Republic of China,Citation8 Canada,Citation22 the US,Citation32 and Ethiopia.Citation9 This may be due to the fact that regular physical activity makes the heart stronger and can pump more blood with less effort. If the heart works less to pump, the force on the arteries decreases, thus lowering BP. Exercise also has an effect on the reduction of systemic vascular resistance, plasma norepinephrine, and renin activities.Citation33
Eating vegetables was found to be a significant factor for BP control among hypertensive patients. This finding was supported by studies conducted in ChileCitation21 and People’s Republic of China.Citation34 This is due to the fact that vegetables are low in cholesterol and saturated fat and high in dietary fiber, potassium, calcium, and magnesium, which result in BP reduction.
Using salt for meal preparation was inversely associated with BP control in the current study. Hence, there was a 33% reduction in the chance of BP control among patients who used salt as compared to patients who did not. The result is consistent with those of other studies conducted in People’s Republic of China,Citation8 Zimbabwe,Citation17 and Addis Ababa, Ethiopia.Citation9 This is due to the fact that salt disrupts the natural sodium balance in the body, causing fluid retention that increases the pressure exerted by the blood against blood vessel walls.
This study revealed that overweight and obese patients have a less chance of controlled BP. Thus, the likelihood of BP control decreased by 50% for overweight patients and 44% for obese patients as compared to normal/underweight patients. Similar findings were reported by studies conducted in People’s Republic of China,Citation8 Iran,Citation11 Spain,Citation35 Zimbabwe,Citation17 Tanzania,Citation15 Sudan,Citation30 and Ethiopia.Citation9 This may be due to obesity inducing a state of chronic volume overload as a result of increased requirements to circulate blood through large and relatively low resistance adipose tissue.Citation36
Coming to duration on antihypertensive treatment, patients with long duration on treatment have better BP control. Though this result is inconsistent with the finding of a study conducted in Addis Ababa, Ethiopia,Citation9 it is supported by a study in Nigeria.Citation10 The possible reason for this finding may be an increase in awareness and adherence to antihypertensive treatment as the patient stays on treatment for longer years.
Adherence, as measured by Morisky–Green–Levine Scale, has shown a significant association with controlled BP. According to this study, patients who are highly adherent to their antihypertensive treatments have a greater chance of controlled BP compared to low adherent patients. Many studies, like those conducted in Nigeria,Citation10 Zimbabwe,Citation17 Tanzania,Citation15 and Addis Ababa, Ethiopia,Citation9 support this finding.
The findings of this study could be used by physicians who care for hypertensive patients in Ethiopia for an evidence-based management of hypertensive patients. They can also serve as a baseline information for public health policy makers in Ethiopia as well as Sub-Saharan Africa for designing guidelines for better BP control among hypertensive patients, thereby reducing HTN-related morbidity and mortality.
Limitations of the study
Information on lifestyle-related variables and drug adherence were collected by interview, and this may lead to recall bias. Social desirability bias may also occur during collecting some covariates (alcohol, smoking) by the interview technique. These may underestimate the effect of these variables on the dependent variable (biasing the measure of association towards the null). There were some potentially time varying covariates (eg, BMI, physical activity) that were taken at the last visit as we did not have the data during the middle visits. In this study, the prevalence of the outcome (controlled BP) is 50%, and the odds ratio may overestimate the risk in measuring the association.
Conclusion
A significant proportion of the hypertensive people had uncontrolled BP. Lifestyle modifications, like doing physical activity, eating vegetables, and avoiding salt addition on meals, were found as effective nonpharmacologic means of BP control. Duration on antihypertensive treatment and adherence to antihypertensive drugs were positively associated with controlled BP, whereas BMI was inversely associated with controlled BP. Hence, counseling hypertensive patients on drug adherence, the need for vegetable consumption, doing moderate physical activity, and avoiding salt addition habit in meals are recommended to improve BP control.
Data sharing statement
Data will be available upon request from the correspondence authors.
Author contributions
YA wrote the proposal, coordinated the data collection activity, analyzed the data, and drafted the paper. DGL revised the proposal and participated in the data collection and analysis and manuscript writing. ATA revised the proposal and participated in data analysis and manuscript editing. All the authors read and approved the final manuscript.
Acknowledgments
The authors are grateful to supervisors and data collectors. Our appreciation also goes to chronic illness treatment clinic staff of University of Gondar Referral Hospital for their kind support during the data collection. Finally, we would like to thank the study participants without whom the research would not have been completed.
Disclosure
The authors report no conflicts of interest in this work.
References
- KotcherTHypertensive vascular diseaseAthonysFEugeneBDennisKHarrison’s Principles of Internal Medicine217 edNew YorkMcGraw-Hill Companies200815491562
- World Health OrganizationGlobal status report on noncommunicable diseases 2014 Available from: apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdfAccessed April 4, 2018
- World Health OrganizationGlobal status report on noncommunicable diseases2014
- OgahOSRayneBLRecent advances in hypertension in sub-Saharan AfricaHeart201399191390139723708775
- MendisSPuskaPNorrvingBoWorld Health OrganizationGlobal Atlas on Cardiovascular Disease Prevention and Control World Health Organization in Collaboration with the World Heart Federation and the World Stroke OrganizationGenevaWorld Health Organization2011318
- IyerASAhmedMIFilippatosGSUncontrolled hypertension and increased risk for incident heart failure in older adults with hypertension: findings from a propensity-matched prospective population studyJ Am Soc Hypertens201041223120374948
- ChobanianAVBakrisGLBlackHRNational Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating CommitteeThe seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 reportJAMA2003289192560257212748199
- YangLXuXYanJAnalysis on associated factors of uncontrolled hypertension among elderly hypertensive patients in Southern China: a community-based, cross-sectional surveyBMC Public Health20141490325178313
- TesfayeAKumelaKWoldeMBlood pressure control associates and antihypertensive pharmacotherapy patterns in Tikur Anbessa General Specialized Hospital Chronic Care Department, Addis Ababa, EthiopiaAm J Biomed Life Sci2015334148
- IlohGUPOfoeduJNNjokuPUAmadiANGodswill-UkoEUMedication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern NigeriaAfr J Prim Health Care Fam Med201351446452
- RezaeianSAhmadzadehJBlood pressure control in hypertensive patients, Iran: a cross-sectional studyInt J Collab Res Intern Med Public Health201241219521958
- MoriHUkaiHYamamotoHCurrent status of antihypertensive prescription and associated blood pressure control in JapanHypertens Res200629314315116755149
- SeravalleGKoylanNNalbantgilIHYT-hypertension in Turkey: a cross-sectional survey on blood pressure control with calcium channel blockers alone or combined with other antihypertensive drugsHigh Blood Press Cardiovasc Prev201522216517225900022
- CheongATSazlinaSGTongSFAzahASSalmiahSPoor blood pressure control and its associated factors among older people with hypertension: a cross-sectional study in six public primary care clinics in MalaysiaMalays Fam Physician20151011925 eCollection 2015
- MagingaJGuerreroMKohEHypertension control and its correlates among adults attending a hypertension clinic in TanzaniaJ Clin Hypertens (Greenwich)201618320721626279168
- MusinguziGNuwahaFPrevalence, awareness and control of hypertension in UgandaPLoS One201384e6223623614041
- GoverwaTPMasukaNTshimangaMUncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, 2012BMC Res Notes2014770325297796
- MutuaEMGitongaMMMbuthiaBMuiruriNCheptumJJMaingiTLevel of blood pressure control among hypertensive patients on follow-up in a regional referral hospital in Central KenyaPan Afr Med J20141827825489372
- HeJMuntnerPChenJRoccellaEJStreifferRHWheltonPKFactors associated with hypertension control in the general population of the United StatesArch Intern Med200216291051105811996617
- MorgadoMRoloSMacedoAFPereiraLCastelo-BrancoMPredictors of uncontrolled hypertension and antihypertensive medication nonadherenceJ Cardiovasc Dis Res20101419620221264184
- PienoviLLaraMBustosPAmigoHConsumo de frutas, verduras y presión arterial. Un estudio poblacional [Fruit and vegetable intake, and blood pressure. A population research]Arch Latinoam Nutr20156512126 Spanish [with English abstract]26320302
- GhadiehASSaabBEvidence for exercise training in the management of hypertension in adultsCan Fam Physician201561323323925927108
- KayimaJWanyenzeRKKatambaALeontsiniENuwahaFHypertension awareness, treatment and control in Africa: a systematic reviewBMC Cardiovasc Disord2013135423915151
- van de VijverSJOtiSOAgyemangCGomezGBKyobutungiCPrevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi, KenyaJ Hypertens20133151018102423425703
- World Health OrganizationWHO STEPS Instrument (Core and Expanded). The WHO STEPwise approach to noncommunicable disease risk factor surveillance (STEPS) Available from: http://www.who.int/ncds/surveillance/steps/instrument/STEPS_Instrument_V3.2.pdf?ua=1Accessed April 4, 2018
- JamesPAOparilSCarterBL2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)JAMA2014311550752024352797
- AbebeZTarikuAGebeyeEAvailability of adequately iodized in Northwest Ethiopia: a cross-sectional studyArch Public Health2017753328781775
- World Health OrganizationPhysical status: the use and interpretation of anthropometry. Report of a WHO Expert CommitteeWHO Technical Report Series 854 Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.htmlAccessed April 4, 2018
- Patry-ParisienJShieldsMBryanSComparison of waist circumference using the World Health Organization and National Institutes of Health protocolsHealth Rep2012233536023061265
- BabikerFAElkhalifaLAMoukhyerMEAwareness of hypertension and factors associated with uncontrolled hypertension in Sudanese adultsCardiovasc J Afr201324620821224217260
- AlmasAGodilSSLalaniSSamaniZAKhanAHGood knowledge about hypertension is linked to better control of hypertension; a multicentre cross sectional study in Karachi, PakistanBMC Res Notes2012557923095492
- BrownRERiddellMCMacphersonAKCanningKLKukJLThe joint association of physical activity, blood-pressure control, and pharmacologic treatment of hypertension for all-cause mortality riskAm J Hypertens20132681005101023690165
- FagardRHCornelissenVAEffect of exercise on blood pressure control in hypertensive patientsEur J Cardiovasc Prev Rehabil2007141121717301622
- LiGCaiAPMoYJEffects of guideline-based hypertension management in rural areas of Guangdong ProvinceChin Med J (Engl)2015128679980325758276
- Rodríguez PérezMCCabrera de LeónAMorales TorresRMFactors associated with knowledge and control of arterial hypertension in the Canary IslandsRev Esp Cardiol (Engl Ed)201265323424022209706
- JeskyMDHayerMKThomasMDasguptaIDo obese individuals with hypertension have more difficult-to-control blood pressure and end organ damage than their nonobese counterparts?J Clin Hypertens (Greenwich)201517646647225807883