Abstract
Background
Endophthalmitis caused by Mycobacterium fortuitum as a complication of cataract surgery is rare in China and globally. This study aimed to report the clinical features, surgical treatment strategies, antibiotic susceptibilities and treatment outcomes in patients with endophthalmitis caused by Mycobacterium fortuitum.
Patients and methods
A case series of 15 patients (15 eyes) with post-cataract endophthalmitis caused by Mycobacterium fortuitum treated at the Ophthalmology Clinic of Shengjing Hospital between June 2008 and June 2017 was reviewed retrospectively. Information about Mycobacterium fortuitum culture results, clinical features, surgical procedures, and final visual acuity were obtained.
Results
The vitreous samples were all positive. These eyes underwent total capsulectomy and intraocular lens explantation and vitrectomy combined with intravitreal and intravenous injections of antibiotics. Finally, 14 eyes had controlled inflammation and retained eyeballs. One eye had panophthalmitis and enucleation of the eyeball. Presenting visual acuity ranged from counting fingers to no light perception. Final visual acuity was better than 20/400 in 4 of 15 eyes (26.67%), 20/400 to hand motions in 7 of 15 eyes (46.67%), and light perception to no light perception in 4 of 15 eyes (26.67%) at 6-month follow-up visit.
Conclusion
Mycobacterium fortuitum might be an etiologic agent in postoperative endophthalmitis. The Mycobacterium fortuitum endophthalmitis might be treated with early vitrectomy and targeted antibiotic therapy approach.
Introduction
Endophthalmitis is a severe intraocular infection involving uveitis and suppurative inflammation of the retina.Citation1 The development of postoperative endophthalmitis after intraocular surgery, including cataract surgery, is a rare but debilitating complication.Citation2 The nontuberculous mycobacterial infections in periocular region are rare and usually caused by the organisms, such as Mycobacterium chelonae and Mycobacterium fortuitum.Citation3 Endophthalmitis caused by Mycobacterium fortuitum as a complication of cataract surgery is rare in China and globally.Citation4,Citation5 M. fortuitum may be acquired from the natural environment, particularly from soil, dust and bio-films in tap water.Citation6–Citation8 M. fortuitum is able to infect the eye, resulting in a number of ocular infections, including conjunctivitis, keratitis and endophthalmitis.Citation9,Citation10 However, the treatment of the M. fortuitum infections could be difficult because of the multi-drug resistance.Citation11 The treatment usually involves the surgical debridement with the removal of the infected foreign body and prolonged the course of the antibiotics, such as the clarithromycin, doxycycline, amikacin and ciprofloxacin.Citation11 Therefore, the investigation for the M. fortuitum infection is critical for the treatment of the endophthalmitis in clinic. The microbiology, clinical features, surgical strategies, and outcomes were presented and evaluated in this retrospective study.
Patients and methods
Patients
The medical records of all patients treated for endophthalmitis caused by M. fortuitum post the cataract surgery at Shengjing Hospital, Shenyang, China between June 2008 and June 2017 were reviewed. The clinical data collected and reviewed included demographic information, past medical history, presenting signs and symptoms, duration of symptoms before diagnosis of endophthalmitis, time between cataract surgery and diagnosis of endophthalmitis, organisms, treatment, and final visual acuity.
All procedures involving human participants were in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of the Department of Ophthalmology of Shengjing Hospital, Shenyang, China.
Surgical method
Fifteen patients underwent cataract removal without complications by phacoemulsification with implantation of a posterior chamber intraocular lens (IOL) in the capsular bag of one eye. Approximately 2or 3weeks later, the patients experienced worsening vision, redness, sudden pain and photophobia in the operated eyes and were referred to our institution. The patients had no serious medical or ocular history and they were HIV negative.
As post-cataract endophthalmitis was suspected, the patients underwent total capsulectomy and IOL explantation and vitrectomy combined with intravitreal injection of 1 mg/0.1 mL vancomycin, 2.25 mg/0.1 mLceftazidime, and 0.2 mg/0.1 mL of dexamethasone. Meanwhile, anterior chamber irrigation was performed for empyema of the anterior chamber during the operation. Patients underwent surgery approximately 1–5 days from the first eye complaint.
Microbiological examination
Vitreous aspirate was also sent for microbiological examination and culture. The postoperative regimen included topical administration of TobraDex eye drops (Alcon, Fort Worth, TX, USA) every 2 hrs. Four days after the operation, microbial culture identified rapidly growing bacteria by acid-fast and Gram stain that were suspected to be M. fortuitum. The treatment regimen was then switched to intravenous injections of 0.4 g moxifloxacin daily for 1week. Finally, intraocular inflammation subsided 2weeks after the operation.
Results
Basic characteristics of patients
All 15 eyes of these post-operative patients were diagnosed with culture-proven endophthalmitis caused by M. fortuitum. Among them, eight (53.33%) were female and seven (46.67%) were male. Among them, nine cases (60%) were right eyes and six cases (40%) were left eyes. The median age was 61 (ranging from 46 to 84) years. Pertinent systemic medical problems included hypertension in six patients and diabetes mellitus in seven patients. All patients (100%) developed acute-onset endophthalmitis (median 17 days, ranging from 2 to 3 weeks). The characteristics aere listed in .
Table 1 Characteristics of the patients
Clinical features
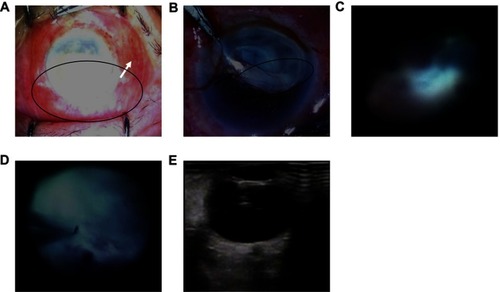
Slit-lamp bio-microscopic examination of the operated eyes identified conjunctival congestion, corneal edema, severe anterior chamber inflammation, and hypopyon (). The posterior chamber IOL was accurately positioned, though a yellowish-white purulent fibrin membrane was present in front of the IOL (). The vitreous and fundus had a yellow and white purulent exudate (). Ocular ultrasonography identified gray flocculent opacities in the vitreous and dense retro-lental opacities in the operated eyes, indicative of endophthalmitis ().
Figure 1 Clinical features of mycobacterium fortuitum endophthalmitis. (A) Biomicroscopic examination identified conjunctival congestion (represented by the white arrow) and a distorted pupil obscured by hypopyon (the pupillary margin hidden in the circle). (B) Biomicroscopic examination identified a severe fibrinous reaction (the fibrinous tissues in the circle) and hypopyon in front of the intraocular lens (represented by the black arrow). (C and D) The vitreous and fundus have a yellow and white purulent exudate. (E) A B-scan ocular ultrasound identified vitreous opacification.
Culture findings
The vitreous samples were all positive for microbes. Microscopic examination, as well as the results of the acid-fast and Gram stain studies were consistent with M. fortuitum (–). The patients underwent detailed systemic examination for occult mycobacterial infections. The clinical examinations, including Mantoux tests, computed tomography of the chest and abdomen, and serum Quantiferon gold test results were all normal. The results of the testing thus ruled out M. tuberculosis.
Figure 2 Diagnosis of Mycobacterium fortuitum endophthalmitis. (A) Microscopic examination of the anterior chamber fibrin membrane sample isolated after vitrectomy. (B) Gram stain of the anterior chamber fibrin membrane sample isolated after vitrectomy. (C) Acid-fast stain of the anterior chamber fibrin membrane sample detected acid-fast bacilli (red stain) that were identified as Mycobacterium fortuitum.

M. fortuitum is an infrequent human pathogen and rare presents in the endophthalmitis post the cataract surgery. Unlike the common pathogenic Mycobacteria, the M. fortuitum grows well on the routine bacteriologic media, such as the MacConkey agar, blood agar, as well as on the Lowenstein Jensen medium at temperatures ranging from 25°C to 40°C, even less than 1week. Meanwhile, the formed colonies demonstrated as the smooth, rough in this study.
Visual and anatomical outcomes
Fourteen eyes had controlled inflammation and retained the eyeballs. Secondary IOL implantation was not performed in the late stage for these 14 eyes. One eye had panophthalmitis and required enucleation of the eyeball. Presenting visual acuity ranged from counting fingers to no light perception and final visual acuity ranged from 20/400 to no light perception. Final visual acuity was better than 20/400 in four of 15 eyes (26.67%), 20/400 to hand motions in seven of 15 eyes (46.67%), and light perception to no light perception in four of 15 eyes (26.67%). No further complications such as retinal detachment, bullous keratopathy, or glaucoma were recorded during the follow-up period.
Discussion
M. fortuitum is an infrequent human pathogen.Citation12–Citation14 In culture, it may be detected within 7days along with other rapidly growing nontuberculous mycobacteria, including M. abscessus and M. chelonae.Citation15–Citation17 In our hospital, 15 of 330 cases of endophthalmitis between June 2008 and June 2017 were M. fortuitum infections; other pathogens included Staphylococcus aureus, Staphylococcus epidermidis, fungi, and Pseudomonas aeruginosa.
While mycobacterial infections are common following refractive surgeries, they are rare following cataract surgery. The diagnosis is typically confirmed by a histological culture. In this study, pertinent systemic medical problems included hypertension in six patients and diabetes mellitus in seven patients. We looked for risk factors for M. fortuitum species, including age, gender, chronic obstructive pulmonary disease,Citation18 diabetes, end-stage renal disease,Citation19 collagen vascular disease, cancer, HIV,Citation20 and transplantation.Citation21 The previous studyCitation22 also demonstrated that endophthalmitis caused by M. fortuitumis usually present in chronically immuno-compromised patients.
In this study, we found that the M. fortuitum grew well on the MacConkey agar, blood agar and the Lowenstein Jensen medium, with faster growth. Meanwhile, the formed colonies were smooth and rough in this study. These characteristics of our isolated M. fortuitum are consistent with the previous study described.Citation23 The previous studyCitation24 also reported that the isolated M. fortuitum from patients was proven to be sensitive to the third generation fluoroquinolones (levofloxacin). However, the present study has not evaluated the sensitivity of isolated M. fortuitum to the drugs.
Endophthalmitis following phacoemulsification is a severe postoperative complication. Upon diagnosis of endophthalmitis, treatment should be initiated immediately and involve intravitreal injections of antibiotics and vitrectomy. Vitrectomy was an effective and efficient procedure for abscess drainage. Vitrectomy can remove intravitreal inflammatory lesions, bacteria and toxins, and reduce the damage caused by toxic substances on retinal function. It may also rescue vitreous transparency and reduce or avoid tractional retinal detachment.Citation25 Intravitreous injection delivers antibiotics directly to the infected lesion, and combined with vitrectomy, greatly improves the cure rate of endophthalmitis. At present, intravitreal injection of steroids in the setting of endophthalmitis is controversial. Some investigators report that steroid application during antibiotic therapy protects the intraocular tissue during acute bacterial endophthalmitis, and that intravitreal injection of dexamethasone is likely to cause intraocular toxicity.Citation26 In this study, we found that intravitreal injection of steroids inhibited M. fortuitum endophthalmitis and improved the patient’s vision.
Concurrent intravitreal vancomycin and low-dose (200 μg) moxifloxacin are recommended for patients with infectious endophthalmitis caused by M. fortuitum. According to the experimental and clinical observation, most clinicians believe that injection of vancomycin and moxifloxacin into the vitreous cavity is safe and dose not lead to retinal toxicity. Despite prompt treatment, the visual sequelae of endophthalmitis caused by M. fortuitum are significant and outcomes are poor. In the current series, only four (26.67%) of our patients had visual acuity of 20/400 or better at the 6-month follow-up visit. One patient (6.67%) had panophthalmitis and required removal of the eyeball.
Combined treatment with intravitreal vancomycin and low-dose moxifloxacin may provide a synergistic bactericidal effect and prevent retinal toxicity, though this is not well studied. Further clinical trials in patients with Mycobacterium fortuitum endophthalmitis will be needed to elucidate the effects of intravitreal vancomycin and low-dose moxifloxacin in this setting, the present study indicates that early identification and aggressive intervention with vitrectomy and antibiotics may prevent poor outcomes in these patients.
This study also has a few limitations. Firstly, as a retrospective study, the case data may be imperfectly recorded or retrieved and compiled. Secondarily, data from only a small number of patients were available for the present retrospective study, and so further studies with larger sample sizes, preferably with multi-center involvement, will be important to confirm and extend our conclusions.
Conclusion
This study demonstrated that Mycobacterium fortuitumis was an etiologic agent in postoperative endophthalmitis. In the following investigation, the Mycobacterium fortuitum endophthalmitis might be treated with early vitrectomy and targeted antibiotic therapy approach.
Acknowledgments
We would like to thank Dr Zhijie Zhang for providing microbiological testing and cultures from the Clinical Laboratory, Shengjing Affiliated Hospital, China Medical University. Data were generated by the authors as part of their routine work. The authors were not funded for data collection.
Disclosure
The authors report no conflicts of interest relevant to this article.
References
- Taban M, Behrens A, Newcomb RL, et al. Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol. 2005;123:613–620. doi:10.1001/archopht.123.5.61315883279
- Choi JA, Chung SK. Postoperative endophthalmitis following cataract surgery in Asian. ISRN Ophthalmol. 2011;2011:361–366.doi: 10.5402/2011/917265
- Walang B, Rath S, Sharma S. Nontuberculous mycobacterial infection after frontalis sling surgery using silicone rod. J Ophthalmic Inflamm Infect. 2012;2:219–221. doi:10.1007/s12348-012-0073-y22477624
- Zhang Y, Liu X, Li K, Bai J. Mycobacterium tuberculosis 10-kDa co-chaperonin regulates the expression levels of receptor activator of nuclear factor-kB ligand and osteoprotegerin in human osteoblasts. Exp Ther Med. 2015;9:919–924. doi:10.3892/etm.2014.215325667654
- Palani D, Kulandai LT, Naraharirao MH, Guruswami S, Ramendra B. Application of polymerase chain reaction-based restriction fragment length polymorphism in typing ocular rapid-growing nontuberculous mycobacterial isolates from three patients with postoperative endophthalmitis. Cornea. 2007;26:729–735. doi:10.1097/ICO.0b013e318060ac3a17592326
- Lan N, Kolader ME, Van Dung N, et al. Mycobacterium fortuitum skin infections after subcutaneous injections with Vietnamese traditional medicine: a case report. BMC Infect Dis. 2014;11:550. doi:10.1186/s12879-014-0550-z
- Patel T, Scroggins-Markle L, Kelly B. A dermal piercing complicated by mycobacterium fortuitum. Case Rep Dermatol Med. 2013;2013:149829.doi: 10.1155/2013/149829 24073343
- Han VX, Loke KY, Chan SM. Recurrent Mycobacterium fortuitum insulin injection site abscesses. J Paediatr Child Health. 2018;54:316–318. doi:10.1111/jpc.1378829168906
- Venkateswaran N, Yeaney G, Chung M, Hindman HB. Recurrent nontuberculous mycobacterial endophthalmitis: a diagnostic conundrum. Clin Ophthalmol. 2014;8:837–842. doi:10.2147/OPTH.S5667024833891
- Brown-Elliott BA, Mann LB, Hail D, Whitney C, Wallace RJ. Antimicrobial susceptibility of nontuberculous mycobacteria from eye infections. Cornea. 2012;31:900–906. doi:10.1097/ICO.0b013e31823f8bb922362004
- Chang WJ, Tse DT, Rose RH. Nontuberculous mycobacterials infections. Ophthalmology. 1999;106:86–90. doi:10.1016/S0161-6420(99)90010-69917786
- Chandanwale SS, Gulati I, Baravkar DS, Shinde SP, Mishra N. Multiple lumps in the breast due to Mycobacterium fortuitum. Indian J Tuberc. 2016;63:126–129. doi:10.1016/j.ijtb.2015.07.01627451824
- Hodgson K, Isabel S, McNamara P, Petrich A, Bitnun A. Mycobacterium fortuitum bloodstream infection in a very low birth weight preterm neonate. Pediatr Infect Dis J. 2017;36:800–802. doi:10.1097/INF.000000000000159228333709
- Shah M, Relhan N, Kuriyan AE, et al. Endophthalmitis caused by nontuberculous mycobacterium: clinical features, antimicrobial susceptibilities, and treatment outcomes. Am J Ophthalmol. 2016;168:150–156. doi:10.1016/j.ajo.2016.03.03527048999
- Pang Y, Zheng H, Tan Y, Song Y, Zhao Y. In vitro activity of bedaquiline against nontuberculous mycobacteria in China. Antimicrob Agents Chemother. 2017;61:e02627–16. doi:10.1128/AAC.02627-1628242674
- Lourenco Nogueira C, Simmon KE, Chimara E, et al. Mycobacterium franklinii sp. Nov., a species closely related to members of the Mycobacterium chelonae-Mycobacterium abscessus group. Int J Syst Evol Microbiol. 2015;65:2148–2153. doi:10.1099/ijs.0.00023425858242
- Girgis DO, Karp CL, Miller D. Ocular infections caused by non-tuberculous mycobacteria: update on epidemiology and management. Clin Exp Ophthalmol. 2012;40:467–475. doi:10.1111/j.1442-9071.2011.02679.x21902780
- de Mello KG, Mello FC, Borga L, et al. Clinical and therapeutic features of pulmonary nontuberculous mycobacterial disease, Brazil, 1993–2011. Emerg Infect Dis. 2013;19:393–399. doi:10.3201/eid/1903.12073523745217
- Sangwan J, Lathwal S, Kumar S, Juyal D. Mycobacterium fortuitum peritonitis in a patient on continuous ambulatory peritoneal dialysis (CAPD): a case report. J Clin Diagn Res. 2013;7:2950–2951. doi:10.7860/JCDR/2013/6771.380324551685
- Soto-Arquíñigo L, García-Pareja M, Gotuzzo-Herencia E, Legua-Leiva P, Sánchez-Herrera M. Co-infection by Mycobacterium fortuitum and Mycobacterium tuberculosis in splenic abscesses in a patient with HIV. Rev Peru Med Exp Salud Publica. 2017;34:328–331. doi:10.17843/rpmesp.2017.342.247029177396
- Shah SK, McAnally KJ, Seoane L, et al. Analysis of pulmonary non-tuberculous mycobacterial infections after lung transplantation. Infect Dis. 2016;18:585–591. doi: 10.1111/tid.12546
- Modi D, Pyatetsky D, Edward DP, et al. Mycobacterium haemophilum: a rare cause of endophthalmitis. Retina. 2007;27:1148–1151. doi:10.1097/IAE.0b013e318030e62218040262
- Pulose RM, Joseph J, Narayanan R, Sharma S. Clinical and microbiological profile of non-tuberculous mycobacterial endophthalmitis-experience in a tertiary eye care centre in Southern India. J Ophthalmic Inflamm Infect. 2016;6:27. doi:10.1186/s12348-016-0096-x27439781
- Sharma K, Gautam N, Sharma M, et al. Ocular mycobacteriosis-dual infection of M. tuberculosis complex with M. fortuitum and M. bovis. J Ophthalmic Inflamm Infect. 2017;7:2. doi:10.1186/s12348-016-0121-028091937
- Shen X, Xu G. Vitrectomy for endogenous fungal endophthalmitis. Ocul Immunol Inflamm. 2009;17:148–152. doi:10.1080/0927394080268939619585356
- Goel N. Acute bacterial endophthalmitis following intravitreal dexamethasone implant: a case report and review of literature. Saudi J Ophthalmol. 2017;31:51–54. doi:10.1016/j.sjopt.2016.12.00328337065
