Abstract
Liposomal amphotericin B is a “true” liposomal formulation of amphotericin B with greatly reduced nephrotoxicity and minimal infusion-related toxicity. This broad spectrum polyene is well tolerated and effective against most invasive fungal infections. In view of the current limitations on diagnostic capability of invasive fungal infections, most clinicians are often compelled to use antifungal drugs in an empiric manner; liposomal amphotericin B continues to play an important role in the empiric management of invasive fungal infections, despite the recent availability of several other drugs in the azole and echinocandin classes.
Introduction
Invasive fungal infections (IFIs) have become a leading cause of morbidity and mortality among immunocompromised patients.Citation1 The incidence of IFIs in these patient populations has increased dramatically over the past three decades. The most common fungal pathogens include Candida albicans and Aspergillus fumigatus and cryptococcus. However, uncommon pathogens such as non-albicans Candida spp, opportunistic yeast-like fungi (eg, Trichosporon and Rhodotorula spp), non-fumigatus Aspergillus spp, Mucorales and hyaline molds (eg, Fusarium and Scedosporium spp) are now emerging as not-so-uncommon opportunistic pathogens.Citation2,Citation3 Etiologic identification of fungal pathogens is frequently difficult, particularly in compromised hosts, since reliable, noninvasive diagnostic tests are presently not available; such situations often compel the clinician to use drugs in an empiric fashion. However, the suspected fungal pathogens are often less susceptible to many antifungal agents including the “broadly-active” amphotericin B (AmB).Citation4–Citation8 Thus, the choice of appropriate agents for empirical antifungal therapy has become a challenge; in the context of recently available, noninvasive diagnostic tests and newer antifungal drugs, the role of amphotericin B as a drug for empiric therapy has become less clear. This review will provide an overview of liposomal amphotericin B (L-AmB) and focus on efficacy studies as well as the safety and tolerability of this drug for the empiric treatment of IFIs.
Management of IFIs in the immunocompromised host
Multiple factors have contributed to the new epidemiologic trends of IFIs, notably a growing number of immunocompromised states (ie, cancer, hematologic stem cell and solid organ transplantation, major surgeries, acquired immune deficiency syndrome, the elderly, etc), the advent of potent immunosuppressant drugs and their widespread use, and the use of antifungal prophylaxis.Citation9–Citation12
In contrast to most bacterial infections, the diagnosis of IFIs is challenging. Delay in diagnosis leads to delayed initiation of appropriate antifungal therapy and, hence, increased mortality. In this setting, early and definitive diagnosis is critical in the management of IFIs. However, clinical presentation of IFIs is often nonspecific; moreover, signs and symptoms could be absent in the early stages of the disease. Fever without signs of localized infection is the most common clinical presentation.Citation13 Fever is of particular concern in severely immunosuppressed patients such as those with profound and prolonged neutropenia following chemotherapy for cancer. Radiographic signs and laboratory tests such as galactomannan and 1,3-beta-D-glucan are used as surrogate markers for the diagnosis and management of IFIs.Citation14,Citation15
Prompt initiation of appropriate antifungal therapy of IFIs is crucial for optimal outcome. Current strategies for the management of IFIs include prophylactic, empiric, preemptive, and targeted therapyCitation15,Citation16 (). Prophylactic strategy includes administration of a narrow- or broadspectrum antifungal drug (active against yeasts or yeasts and molds) to high-risk patient population before the onset of signs/symptoms of infection. Empirical antifungal therapy is often initiated when a microbiological diagnosis of IFI is unavailable in high-risk presently neutropenic patients presenting with persistent or recurring fevers despite 4–7 days of appropriate antibiotic therapy (duration of neutropenia expected to be more than 7 days).
Figure 1 Current strategies for the management of IFI in high-risk patients.
Notes: *High-resolution computed tomography scan of the lungs showing new ≥1 cm single or multiple nodules with or without halo sign, lobar consolidation, wedge-shaped consolidative infarct; **classic example: patients with proglonged and profound neutropenia after intense chemotherapy for hematologic malignancy.
Abbreviations: GM, serum Galactomannan; IFI, invasive fungal infection; PCR, polymerase chain reaction.
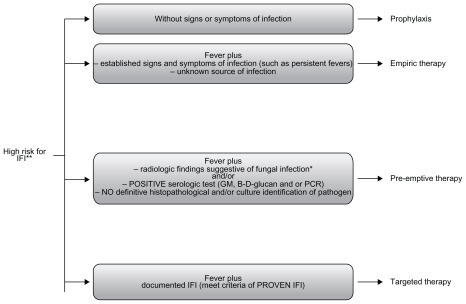
Pre-emptive therapy is initiated when suggestive but nonspecific radiographic signs are present and/or laboratory tests are suggestive of IFIs, without microbiological or histopathological confirmation of IFI. Targeted therapy is initiated when there is microbiologically and/or histologically proven IFI.Citation15,Citation16
Antifungal drugs
There are three main classes of systemic antifungal drugs available for the treatment of IFIs: polyenes, azoles, and echinocandins. Azoles deplete ergosterol and compromise fungal cell-wall integrity by dose-dependent inhibition of cytochrome-P450-dependent 14α-demethylase.Citation17 Currently available systemic azoles include fluconazole, itraconazole, voriconazole, and posaconazole. Echinocandins are compounds that disrupt cell-wall synthesis by inhibiting the synthesis of 1,3-beta-D-glucan, which is a critical component of most fungal cell walls.Citation18 Echinocandins include caspofungin, anidulafungin, and micafungin. Azoles and echinocandins are relatively safe and well tolerated.Citation18,Citation19
The polyenes include conventional amphotericin B (AmB-D) and lipid formulations of amphotericin B (amphotericin B lipid complex [ABLC], L-AmB, and amphotericin B colloidal dispersion [ABCD] formulations).Citation20 AmB-D binds with sterols, principally ergosterol in the fungal cell membrane. This binding is followed by increased leakage of intracellular ions out of the fungal cells resulting in osmotic disruption with increased membrane permeability and, ultimately, cell death. Polyenes also interfere with membrane-associated oxidative enzyme function, which is also lethal for the cell.Citation20
Lipid formulations of amphotericin B were developed to decrease toxicity and improve the tolerability profile of AmB-D. Lipid formulations of amphotericin B have different structures. ABLC has a ribbon-like structure, ABCD is composed of disc-like structures, and L-AmB forms small uniform spherical lipid vesicles or liposomes containing amphotericin B.Citation21 The three formulations produce tissue amphotericin B concentrations ranging from 90% lower than, to 500% higher than the serum levels seen with AmB-D. Most consistently, reduced concentrations are seen in the kidney, thus accounting for the markedly lower nephrotoxicity. The doses of lipid forms of amphotericin B are higher than that of amphotericin B deoxycholate; such high but equipotent doses are better tolerated and there is also a clear reduction in the frequency and severity of nephrotoxicity.
Spectrum of activity: amphotericin B
Despite the differences in the structures of lipid formulations and AmB-D, their spectrum of activity is comparable.Citation22 Amphotericin B is active against clinically relevant yeasts such as most Candida spp and Cryptococcus neoformans and molds, including most Aspergillus spp and Mucorales. AmB is also active against Histoplasma spp, Paracoccidiodes spp, Blastomyces spp, and Coccidioides spp.Citation20
Several Candida species such as Candida lusitaniae, Candida guilliermondii, and Candida rugosa may be resistant to AmB.Citation23–Citation25 Also, Trichosporon spp, an infrequent cause of catheter-related fungemia, are resistant to AmB.Citation26,Citation27
Non-fumigatus Aspergillus spp, in particular Aspergillus terreus, Aspergillus flavus and Aspergillus nidulans, have demonstrated clinical resistance to AmB.Citation28–Citation30 Similarly, Aspergillus ustus is an uncommon clinical species that may have decreased susceptibility to AmB.Citation31–Citation33 However, Aspergillus lentulus, a recently described Aspergillus species, has demonstrated variable in vitro susceptibility to AmB.Citation34,Citation35 AmB has limited activity against Fusarium spp (especially Fusarium solani), although it has better activity as compared with other agents such as the older azoles (eg, Itraconazole) and echinocandins.Citation8,Citation36,Citation37 Mucorales are susceptible to AmB – the drug has been the drug of choice for the treatment of mucormycosis; however, clinical response has been variable and the overall mortality of patients with mucormycosis has remained high, particularly in patients with persistent immunosuppression or poor source control. A newer azole, posaconazole is active against most Mucorales and appears to be promising for the treatment of this disease.Citation8,Citation38 Isavuconazole, a more recent broad-spectrum azole, available in oral and parenteral forms, is under clinical investigation. Scedosporium spp are intrinsically resistant to AmB. While Scedosporium apiospermum is susceptible to itraconazole, voriconazole, and posaconazole, Scedosporium prolificans is considered resistant to all available antifungal agents.Citation39,Citation40 Limited data are available to support the optimal antifungal therapy against Acremonium spp. Clinically relevant species of Acremonium, Alternaria, Cladosporium and Exophiala have demonstrated high minimal inhibitory concentrations for AmB.Citation41
Safety and tolerance: L-AmB
Conventional amphotericin B (AmB-deoxycholate [AmB-D]) was considered the gold standard of antifungal treatment for many decades. Infusion-related reactions and dose-dependent nephrotoxicity are major limitations of this drug.Citation21 Indeed, these side effects are associated with increased morbidity in immunocompromised patients.Citation42 Other toxicities reported with the use of AmB-D include local thrombophlebitis, nausea and vomiting, and anemia. Less frequently, hepatotoxicity (ie, transient elevation of transaminase levels and acute liver failure) has been associated with the use of AmB-D.Citation42
In general, all lipid formulations of AmB have been associated with reduced nephrotoxicity compared with AmB- D.Citation21,Citation43,Citation44 White et al reported a randomized, double- blind multicenter superiority trial in which ABCD (4 mg/kg/d) was compared with AmB-D (0.8 mg/kg/d) for the empiric management of febrile neutropenia.Citation43 Therapeutic response was similar (43%–50%), but renal dysfunction was less likely to develop and occurred later in ABCD recipients (P < 0.001 for both parameters). Infusion-related hypoxia and chills were more common in ABCD recipients than AmB-D recipients (P = 0.013 and P = 0.018, respectively). In clinical practice, in view of its frequent infusion-related intolerability, ABCD is not favored.
In a randomized, double-blind comparative study, Wingard et al evaluated the safety of L-AmB versus ABLC in the empirical treatment of febrile neutropenia.Citation45 In this study, L-AmB at a dose of 3 or 5 mg/kg/d was associated with significantly fewer infusion-related reactions and other toxicities (ie, nausea, vomiting) when compared to ABLC at a dose of 5 mg/kg/d. There was nonsignificant difference in the rates of hepatotoxicity, hypokalemia, and anemia between patients receiving either ABLC or L-AmB. Since the publication of Wingard et al’s study, it has been widely believed that L-AmB is less nephrotoxic than ABLC. However, in a recently published study, Safdar et al conducted a metaanalysis to evaluate nephrotoxicity associated with ABLC and L-AmB.Citation46 After adjusting for heterogeneity across the studies included in the meta-analysis, the authors found that the nephrotoxicity was similar for ABLC and L-AmB in patients receiving either drug as antifungal therapy or prophylaxis.
While all three lipid formulations of AmB exhibit reduced nephrotoxicity compared with AmB-D, L-AmB appears to be the safest in terms of infusion-related reactions. summarizes the current US Food and Drug Administration (FDA)-approved indications for the use of L-AmB and all available antifungal agents.
Table 1 US Food and Drug Administration-approved indication of antifungal agents for the management of IFIs
Empirical therapy: liposomal amphotericin B (L-AmB)
The strategy of empirical antifungal therapy has been systemically evaluated only in the setting of antibiotic-refractory fever in patients with chemotherapy-induced neutropenia. summarizes the clinical trials of L-AmB in the empiric management of fever in neutropenic patients.
Table 2 Summary of clinical trials comparing efficacy and safety of liposomal amphotericin B with other antifungal agents for empirical antifungal therapy in patients with neutropenia
In a randomized trial by Walsh et al, L-AmB was as effective as AmB-D for the empirical therapy of fever in adult and pediatric neutropenic patients.Citation47 In this study, 687 patients were randomized to empirical treatment with L-AmB at a dose of 3.0 mg/kg/d or AmB-D at 0.6 mg/kg/d.Citation47 Rates of successful treatment were similar (50.1% for patients receiving L-AmB and 49.4% for those receiving AmB-D.) Rates of survival were also similar (93% for L-AmB and 90% for AmB-D). Significantly, the use of L-AmB was associated with fewer proven breakthrough IFIs (11 patients [3.2%]) compared to patients receiving AmB-D (27 patients [7.8%], P = 0.009).
As previously discussed, Wingard et al conducted a randomized, double-blind comparative study of L-AmB (3–5 mg/kg/d) versus ABLC (5 mg/kg/d) in the empirical treatment of febrile neutropenia.Citation45 Among 244 patients included, actual response rates were 40% (3 mg/kg/d) and 42% (5 mg/kg/d) for L-AmB, and 33% for ABLC. While the primary endpoint in this study was the incidence of infusion-related reactions, the authors found no significant differences in successful response and survival in both adult and pediatric patients.Citation45
With the introduction of new classes of antifungal agents, the efficacy of L-AmB for empirical therapy has been compared with that of caspofunginCitation48–Citation50 and voriconazole.Citation51 Many prospective, randomized, multicenter comparative trials evaluating echinocandins have been publishedCitation48,Citation49,Citation51 (). In these studies, efficacy assessment was based on a composite endpoint consisting of five criteria: (1) successful treatment of any baseline fungal infection, (2) absence of any breakthrough fungal infection during therapy or within 7 days after the completion of therapy, (3) survival for 7 days after the completion of therapy, (4) no premature discontinuation of study therapy because of drug-related toxicity or lack of efficacy, and (5) resolution of fever during neutropenia. Treatment was considered successful if all five criteria were met.Citation47
In a randomized, double-blind multicenter trial of 1095 patients with persistent fever and neutropenia, Walsh et al showed that caspofungin was as effective as L-AmB.Citation48 The overall success rates were 33.9% for caspofungin and 33.7% for L-AmB (95.2% confidence interval: −5.6 to 6.0) caspofungin improved survival (92.6% and 89.2% for caspofungin and L-AmB, respectively; P = 0.05) and response rates in patients with IFIs (51.9% vs 25.9%; P = 0.04). Breakthrough fungal infections were similar in the two groups. Also resolution of fever during the period of neutropenia was comparable. Fewer patients in the caspofungin group encountered nephrotoxicity and there were fewer infusion-related events or premature discontinuations of therapy. The authors concluded caspofungin to be as effective as L-AmB.
More recently, Maertens et al reported the results of a randomized, double-blind multicenter trial comparing empirical therapy with caspofungin versus L-AmB in pediatric patients.Citation49 In this study, patients were randomized to receive caspofungin (70 mg loading dose on day 1 followed by 50 mg/d) or L-AmB (3 mg/kg/d). Although the main endpoint of this study was safety, clinical efficacy was also evaluated. Overall success rates were similar across treatment groups (46.4% and 32% for caspofungin and L-AmB, respectively).
Walsh et al conducted a randomized, nonblinded multicenter trial among febrile neutropenic patients comparing empirical antifungal therapy with L-AmB versus voriconazole. Citation51 In this study, voriconazole failed to meet the prespecified criteria for noninferiority to L-AmB. A total of 837 patients (415 assigned to voriconazole and 422 to L-AmB) were evaluated for success of treatment. Based upon prespecified criteria, voriconazole was inferior to L-AmB with overall success rates of 26% with voriconazole and 30.6% with L-AmB (95% confidence interval: −10.6 to 1.6). Importantly, however, documented breakthrough IFIs occurred less frequently among voriconazole recipients – eight patients (1.9%) in the voriconazole group versus 21 patients (5%) in the L-AmB group (P = 0.02). After stratifying for risk, overall success rates were 32% and 30% for high-risk patients receiving voriconazole and L-AmB, respectively. The authors concluded that voriconazole is a suitable alternative to L-AmB for empiric antifungal therapy in patients with neutropenia and persistent fever.
Because of its broad spectrum of activity, rarely documented resistance, and long track record of clinical efficacy, AmB-D has been the standard choice for the empirical treatment in patients with persistent fever and neutropenia for many decades. However, antifungal agents that have become available over the past 15 years are less toxic and are as effective as AmB-D in the empiric treatment of IFIs.Citation45,Citation47–Citation51 Indeed, based on the data discussed, L-AmB and caspofungin have now been approved by the FDA for the empiric antifungal therapy in febrile neutropenic patients.Citation52,Citation53
All echinocandins are safe, well tolerated, and have a similar spectrum of antifungal activity. However, FDA-approved indications of these drugs differ.Citation52,Citation53 Caspofungin is approved for empirical therapy of febrile neutropenia and for the treatment of invasive aspergillosis in patients refractory of or intolerant to other approved drugs.Citation53 Micafungin, however, has been approved for antifungal prophylaxis in stem-cell transplantation. Limited data suggest that the safety and efficacy of caspofungin and micafungin are comparable in the empiric treatment of invasive aspergillosis, but micafungin has not been licensed for this use.Citation54 Similarly, despite the widespread use of voriconazole as empiric therapy and prophylaxis of IFIs, voriconazole is not FDA approved for these indications.Citation55 Posaconazole, based on available data, has been approved for the prophylaxis of invasive Aspergillus and Candida infections in high-risk, severely immunocompromised adult patients.Citation55
In summary, the three lipid formulations of AmB have demonstrated similar efficacy and fewer adverse events compared with conventional amphotericin B deoxycholate. Amphotericin B colloidal dispersion, in view of its unacceptably high frequency of infusion-related toxicities similar to amphotericin B deoxycholate, is no longer favored. L-AmB has fewer infusion-related adverse reactions as compared with ABLC. Both L-AmB and ABLC appear to have similar nephrotoxic potential.
L-AmB has been rigorously evaluated in the empiric treatment of patients with neutropenia and antibiotic-refractory fever. The drug appears safe as well as effective. Besides neutropenic fever, empiric therapy may be required in some nonneutropenic situations as well. For example, allogeneic stem-cell recipients with graft versus host disease may require empiric antifungal therapy in the setting of undiagnosed, nodular pulmonary infiltrates. Although not clinically proven, L-AmB may be an appropriate empiric choice in such situations, particularly in the background of prophylactic use of broad-spectrum azoles. During the last decade, many thought that amphotericin B-deoxycholate and its lipid forms would become obsolete in view of the recently released, less-toxic azoles and echinocandins. That has not turned out to be so. Despite the fact that amphotericin B is an “old” drug, L-AmB plays and will continue to play an important role in the empiric antifungal management of patients at high risk for invasive fungal infections.
Disclosure
The authors report no conflicts of interest in this work.
References
- MohrJJohnsonMCooperTLewisJSOstrosky-ZeichnerLCurrent options in antifungal pharmacotherapyPharmacotherapy200828561464518447660
- MiceliMHDíazJALeeSAEmerging opportunistic yeast infectionsLancet Infect Dis20111114215121272794
- MiceliMHLeeSAEmerging moulds: epidemiological trends and antifungal resistanceMycoses2011546e666e67821672045
- BormanAMPetchRLintonCJPalmerMDBridgePDJohnsonEMCandida nivariensis, an emerging pathogenic fungus with multidrug resistance to antifungal agentsJ Clin Microbiol200846393393818199788
- SnydmanDRShifting patterns in the epidemiology of nosocomial Candida infectionsChest20031235 Suppl500S503S12740235
- PfallerMADiekemaDJGibbsDLResults from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997–2005. An 8.5-year analysis of susceptibilities of Candida species and other yeast species to fluconazole and voriconazole by CLSI standardized disk diffusion testingJ Clin Microbiol20074561735174517442797
- BaddleyJWMoserSAEmerging fungal resistanceClin Lab Med2004243721735vii15325062
- SabatelliFPatelRMannPAIn vitro activities of posaconazole, fluconazole, itraconazole, voriconazole, and amphotericin B against a large collection of clinically important molds and yeastsAntimicrob Agents Chemother20065062009201516723559
- ImhofABalajeeSAFredricksDNEnglundJAMarrKABreakthrough fungal infections in stem cell transplant recipients receiving voriconazoleClin Infect Dis200439574374615356792
- KobayashiKKamiMMurashigeNKishiYFujisakiGMitamuraTBreakthrough zygomycosis during voriconazole treatment for invasive aspergillosisHaematologica20048911ECR4215533847
- MartyFMCosimiLABadenLRBreakthrough zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplantsN Engl J Med2004350995095214985500
- ProcopGWRobertsGDEmerging fungal diseases: the importance of the hostClin Lab Med2004243691719vivii15325061
- AsciogluSRexJHde PauwBDefining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensusClin Infect Dis200234171411731939
- ChandrasekarPInvasive mold infections: recent advances in management approachesLeuk Lymphoma200950570371519337880
- RuhnkeMBohmeABuchheidtDDiagnosis of invasive fungal infections in hematology and oncology – guidelines from the Infectious Diseases Working Party in Haematology and Oncology of the German Society for Haematology and Oncology (AGIHO)Ann Oncol Epub 2011 Sep 23
- FreifeldAGBowEJSepkowitzKAClinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of americaClin Infect Dis2011524e56e9321258094
- GhannoumMARiceLBAntifungal agents: mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistanceClin Microbiol Rev199912450151710515900
- SucherAJChahineEBBalcerHEEchinocandins: the newest class of antifungalsAnn Pharmacother200943101647165719724014
- WalshTJDriscollTMilliganPAPharmacokinetics, safety, and tolerability of voriconazole in immunocompromised childrenAntimicrob Agents Chemother201054104116412320660687
- MoenMDLyseng-WilliamsonKAScottLJLiposomal amphotericin B: a review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infectionsDrugs200969336139219275278
- DupontBOverview of the lipid formulations of amphotericin BJ Antimicrob Chemother200249Suppl 1313611801578
- AnaissieEPaetznickVProffittRAdler-MooreJBodeyGPComparison of the in vitro antifungal activity of free and liposome-encapsulated amphotericin BEur J Clin Microbiol Infect Dis19911086656681748123
- HawkinsJLBaddourLMCandida lusitaniae infections in the era of fluconazole availabilityClin Infect Dis2003362e14e1812522762
- KrcmeryVBarnesAJNon-albicans Candida spp causing fungaemia: pathogenicity and antifungal resistanceJ Hosp Infect200250424326012014897
- ColomboALMeloASCrespo RosasRFOutbreak of Candida rugosa candidemia: an emerging pathogen that may be refractory to amphotericin B therapyDiagn Microbiol Infect Dis200346425325712944016
- Araujo RibeiroMAlastruey-IzquierdoAGomez-LopezARodriguez-TudelaJLCuenca-EstrellaMMolecular identification and susceptibility testing of Trichosporon isolates from a Brazilian hospitalRev Iberoam Micol200825422122519071890
- PfallerMADiekemaDJRare and emerging opportunistic fungal pathogens: concern for resistance beyond Candida albicans and Aspergillus fumigatusJ Clin Microbiol200442104419443115472288
- BaddleyJWPappasPGSmithACMoserSAEpidemiology of Aspergillus terreus at a university hospitalJ Clin Microbiol200341125525552914662934
- IwenPCRuppMELangnasANReedECHinrichsSHInvasive pulmonary aspergillosis due to Aspergillus terreus: 12-year experience and review of the literatureClin Infect Dis1998265109210979597234
- SuttonDASancheSERevankarSGFothergillAWRinaldiMGIn vitro amphotericin B resistance in clinical isolates of Aspergillus terreus, with a head-to-head comparison to voriconazoleJ Clin Microbiol19993772343234510364610
- VerweijPEvan den BerghMFRathPMde PauwBEVossAMeisJFInvasive aspergillosis caused by Aspergillus ustus: case report and reviewJ Clin Microbiol19993751606160910203536
- IwenPCRuppMEBishopMRDisseminated aspergillosis caused by Aspergillus ustus in a patient following allogeneic peripheral stem cell transplantationJ Clin Microbiol19983612371337179817905
- PanackalAAImhofAHanleyEWMarrKAAspergillus ustus infections among transplant recipientsEmerg Infect Dis200612340340816704776
- BalajeeSAGribskovJLHanleyENickleDMarrKAAspergillus lentulus sp. nov, a new sibling species of A. fumigatusEukaryot Cell20054362563215755924
- BalajeeSAWeaverMImhofAGribskovJMarrKAAspergillus fumigatus variant with decreased susceptibility to multiple antifungalsAntimicrob Agents Chemother20044841197120315047520
- PujolIGuarroJGenéJSalaJIn-vitro antifungal susceptibility of clinical and environmental Fusarium spp strainsJ Antimicrob Chemother19973921631679069536
- DenningDWEchinocandin antifungal drugsLancet200336293901142115114550704
- van BurikJAHareRSSolomonHFCorradoMLKontoyiannisDPPosaconazole is effective as salvage therapy in zygomycosis: a retrospective summary of 91 casesClin Infect Dis2006427e61e6516511748
- Cuenca-EstrellaMRuiz-DíezBMartinez-SuárezJVMonzónARodríguez-TudelaJLComparative in-vitro activity of voriconazole (UK-109,496) and six other antifungal agents against clinical isolates of Scedosporium prolificans and Scedosporium apiospermumJ Antimicrob Chemother199943114915110381115
- WalshTJPeterJMcGoughDAFothergillAWRinaldiMGPizzoPAActivities of amphotericin B and antifungal azoles alone and in combination against Pseudallescheria boydiiAntimicrob Agents Chemother1995396136113647574531
- PerdomoHSuttonDAGarciaDSpectrum of clinically relevant Acremonium species in the United StatesJ Clin Microbiol201149124325621068274
- GallisHADrewRHPickardWWAmphotericin B: 30 years of clinical experienceRev Infect Dis19901223083292184499
- WhiteMHBowdenRASandlerESRandomized, double-blind clinical trial of amphotericin B colloidal dispersion vs amphotericin B in the empirical treatment of fever and neutropeniaClin Infect Dis19982722963029709879
- Ostrosky-ZeichnerLMarrKARexJHCohenSHAmphotericin B: time for a new “gold standard”Clin Infect Dis200337341542512884167
- WingardJRWhiteMHAnaissieERaffalliJGoodmanJArrietaAA randomized, double-blind comparative trial evaluating the safety of liposomal amphotericin B versus amphotericin B lipid complex in the empirical treatment of febrile neutropenia. L Amph/ABLC Collaborative Study GroupClin Infect Dis20003151155116311073745
- SafdarAMaJSalibaFDrug-induced nephrotoxicity caused by amphotericin B lipid complex and liposomal amphotericin B: a review and meta-analysisMedicine (Baltimore)201089423624420616663
- WalshTJFinbergRWArndtCLiposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study GroupN Engl J Med19993401076477110072411
- WalshTJTepplerHDonowitzGRCaspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropeniaN Engl J Med20043511401391140215459300
- MaertensJAMaderoLReillyAFA randomized, double-blind, multicenter study of caspofungin versus liposomal amphotericin B for empiric antifungal therapy in pediatric patients with persistent fever and neutropeniaPediatr Infect Dis J201029541542020431381
- EllisMFramptonCJosephJAn open study of the comparative efficacy and safety of caspofungin and liposomal amphotericin B in treating invasive fungal infections or febrile neutropenia in patients with haematological malignancyJ Med Microbiol200655Pt 101357136517005784
- WalshTJPappasPWinstonDJVoriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent feverN Engl J Med2002346422523411807146
- USA FDA Regulations http://www.fda.gov/drugs/default.htm
- ChenSCSlavinMASorrellTCEchinocandin antifungal drugs in fungal infections: a comparisonDrugs2011711114121175238
- KubiakDWBryarJMMcDonnellAMEvaluation of caspofungin or micafungin as empiric antifungal therapy in adult patients with persistent febrile neutropenia: a retrospective, observational, sequential cohort analysisClin Ther201032463764820435233
- WaknineYFDA approvalsAvelox, Avandaryl, Trileptal Available at: http://www.medscape.com/viewarticle/518278?rssAccessed February 11, 2006 [cited 2011 Oct 24]