Abstract
Objective
To determine the trends of conjunctival sac bacterial flora isolated from patients prior to cataract surgery.
Subjects and methods
The study comprised 579 patients (579 eyes) who underwent cataract surgery. Specimens were collected by lightly rubbing the inferior palpebral conjunctival sac with a sterile cotton swab 2 weeks before surgery, and then cultured for isolation of bacteria and antimicrobial sensitivity testing. The bacterial isolates and percentage of drug-resistant isolates were compared among age groups and according to whether or not patients had diabetes mellitus, hyperlipidemia, dialysis therapy, oral steroid use, dry eye syndrome, or allergic conjunctivitis.
Results
The bacterial isolation rate was 39.2%. There were 191 strains of Gram-positive cocci, accounting for the majority of all isolates (67.0%), among which methicillin-sensitive coagulase-negative staphylococci was the most frequent (127 strains, 44.5%), followed by methicillin-resistant coagulase-negative staphylococci (37 strains, 12.7%). All 76 Gram-positive bacillary isolates (26.7%) were from the genus Corynebacterium. Among the 16 Gram-negative bacillary isolates (5.9%), the most frequent was Escherichia coli (1.0%). The bacterial isolation rate was higher in patients >60 years old, and was lower in patients with dry eye syndrome, patients under topical treatment for other ocular disorders, and patients with hyperlipidemia. There was no significant difference in bacterial isolation rate with respect to the presence/absence of diabetes mellitus, steroid therapy, dialysis, or a history of allergic conjunctivitis. Methicillin-resistant coagulase-negative staphylococci showed a significantly higher detection rate in diabetic patients than nondiabetic patients (20.3% versus 7.0%, P < 0.05). The percentage of all isolates resistant to levofloxacin, cefmenoxime, and tobramycin was 14.0%, 15.2%, and 17.9%, respectively, with no significant differences among these drugs.
Conclusion
The high bacterial isolation rate in patients >60 years old and the high methicillin-resistant coagulase-negative staphylococci isolation rate in patients with diabetes are important to consider for prevention of perioperative infections.
Introduction
Age-related cataract is responsible for 48% of world blindness, which represents about 18 million people.Citation1 Cataract surgery has become widespread in developed countries thanks to advances in procedures and instruments, and almost all patients achieve recovery of visual acuity as a matter of course after treatment. Further, incidence of endophthalmitis after cataract surgery is decreasing.Citation2 However, if postoperative endophthalmitis occurs, there is a high risk of loss of vision with consequent adverse effects on the patient’s quality of life. At the same time, the responsibility for endophthalmitis is a mental burden for the surgeon.
It has been reported that indigenous bacteria in the conjunctival sac influence the bacterial pathogens causing endophthalmitis after cataract surgery.Citation3 It is likely that conjunctival sac bacterial flora would be altered by factors that affect a patient’s general condition such as diabetes mellitus, corticosteroid use, and aging.Citation4–Citation8 Accordingly, this study was conducted to compare isolates from the conjunctival sac bacterial flora prior to cataract surgery in order to identify differences of isolates and resistance to antimicrobial agents related to patient factors such as the presence/absence of diabetes mellitus, hyperlipidemia, oral steroid therapy, dry eye syndrome requiring topical medication, other ocular conditions except requiring topical antimicrobial agents, and allergic conjunctivitis.
Subjects and methods
The study population comprised 579 patients (579 eyes) who underwent cataract surgery in the Department of Ophthalmology of Saiseikai Kurihashi Hospital during a 3.5-year period from January 2004 to June 2007. The patients were enrolled in a consecutive manner. All patients provided informed consent, this study was conducted in accordance with the Declaration of Helsinki, and only one eye was investigated even in patients with cataracts affecting both eyes. There were 234 men (40.4%) and 345 women (59.6%) who ranged in age from 51 to 100 years (mean ± standard deviation: 71.7 ± 9.5 years).
Two weeks before cataract surgery, specimens for bacteriologic examination were collected from the conjunctival sac, without anesthesia, by lightly rubbing the inferior palpebral conjunctiva with a sterile cotton swab, and were transferred within 1 hour to the clinical laboratory of the hospital for plating on blood agar medium and chocolate agar medium.Citation9,Citation10 Cultures were incubated at 35°C for 24–48 hours. Neither anaerobic nor enrichment cultures were performed. Antimicrobial sensitivity testing of the bacterial isolates was carried out by the microbroth dilution technique in accordance with the Clinical and Laboratory Standards Institute (document M100-S17) using the disc diffusion methodCitation11 and a fully automated microbiology system (RAISUS; Nissui Pharmaceutical Co, Ltd, Tokyo, Japan).
The variables investigated were the conjunctival sac bacterial isolation rate, details of the bacterial isolates, and percentage of drug-resistant isolates, which were compared among age groups and according to the presence/absence of diabetes mellitus, hyperlipidemia, dialysis therapy, oral steroid use, usage of eye drops excluding antibacterial medicine, dry eye syndrome, or allergic conjunctivitis. Patients with dry eye syndrome were only enrolled in this study if they were receiving treatment with artificial tears or hyaluronic acid eye drops. Patients excluding dry eye syndrome were compared by the existence of usage of eye drops containing preservatives. Among patients with diabetes, the result was compared by the level of hemoglobin A1c.
Preoperative administration with levofloxacin (LVFX) eye drops for 3 days, which was evaluated in a multicenter study sponsored by the Japanese Association for Ocular Infection,Citation12 was employed in this study routinely, and no oral antibacterial medicine was applied before cataract surgery. The patients were also treated routinely with faropenem sodium hydrate (Farom®; Maruho, Tokyo, Japan) at a dose of 600 mg daily for 4 days after cataract surgery.
Statistical analyses were performed using IBM SPSS for Windows (v 14.0; SPSS, Inc, Chicago, IL). The 2 × 2 Chi square test was employed for categorical comparison.
Results
None of the patients in this study contracted endophthalmitis after cataract surgery.
Bacteria were isolated from 227 (39.2%) of the 579 eyes studied. Of these 227 eyes, a single isolate was detected in 179 eyes (78.9%), while there were two isolates in 39 eyes (17.2%), three isolates in eight eyes (3.5%), and four isolates in one eye (0.4%).
In more detail, there were 191 strains of Gram-positive cocci, accounting for 67.0% of all isolates, as well as 127 strains (44.5%) of methicillin-sensitive coagulase-negative staphylococci, 37 strains (12.7%) of methicillin-resistant coagulase-negative staphylococci, eight strains (2.9%) of methicillin-sensitive Staphylococcus aureus, and three strains (1.0%) of methicillin-resistant S. aureus (). Among 76 Gram-positive bacilli isolates (26.7%), all were of the genus Corynebacterium. There was only one Gram-negative coccus isolated (0.4%), which was identified as Moraxella catarrhalis. There were 16 Gram-negative bacillary isolates (5.9%), including three Escherichia coli isolates (1.0%); two isolates (0.7%) each of Pseudomonas aeruginosa, Acinetobacter spp, and nonglucose-fermenting bacteria; and one isolate (0.4%) each of Proteus vulgaris, Proteus mirabilis, Enterobacter aerogenes, Serratia marcescens, Klebsiella oxytoca, and Alcaligenes spp.
Table 1 Bacterial isolates and rates
The bacterial isolation rate was significantly lower for patients aged ≤60 years compared with patients 61–70 years, 71–80 years, and ≥81 years old (P < 0.001; ). The bacterial isolation rate did not differ significantly between diabetics and nondiabetics (). There was also no significant difference in bacterial isolation rate in relation to presence/absence of diabetic retinopathy and hemoglobin A1c level ( and ). No statistically significant differences were noted in relation to the presence/absence of dialysis therapy, oral steroid use, or allergic conjunctivitis (). In relation to whether the patients were using eye drops or not, the bacterial isolation rate was significantly lower (P < 0.001) for the group using eye drops (85/275 eyes, 30.9%) than for the group not using such medication (142/304 eyes, 46.7%). The bacterial isolation rate was significantly lower (P < 0.001) for patients with dry eye syndrome (19/96, 19.8%) than for those without it (208/483, 43.1%). A significantly lower (P < 0.05) bacterial isolation rate was also noted for patients with hyperlipidemia (55/169, 32.5%) than for those without it (172/410, 42.0%).
Table 2 Bacterial detection rate dependent on age
Table 3 Bacterial detection rate dependent on background
Table 4 Bacterial detection rate dependent on hemoglobin A1c level
For methicillin-resistant coagulase-negative staphylococci, the percentage of resistant organisms was significantly greater (P < 0.05) in diabetic patients (13 strains, 20.3%) than in nondiabetic patients (eight strains, 7.0%).
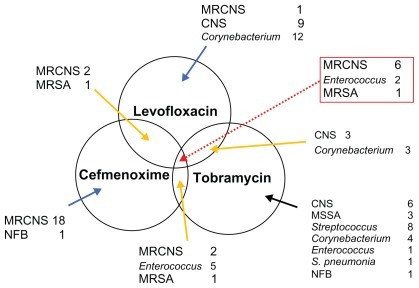
Of the 285 strains isolated, 40 strains (14.0%) were resistant to LVFX. For cefmenoxime, 39 (15.2%) out of 257 strains were resistant, while 42 (17.9%) out of 262 strains were resistant to tobramycin. The percentage of resistant organisms did not differ significantly among these antimicrobial agents. Resistance to all three of these drugs was demonstrated by six methicillin-resistant coagulase-negative staphylococci strains, two enterococcal strains, and one methicillin-resistant S. aureus ().
Figure 1 Resistance to levofloxacin, cefmenoxime, and tobramycin was shown in six methicillin-resistant coagulase-negative staphylococci strains, two enterococcal strains, and one methicillin-resistant Staphylococcus aureus strain.
Abbreviations: CNS, coagulase-negative staphylococci; MRCNS, methicillin-resistant coagulase-negative staphylococci; MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-sensitive Staphylococcus aureus; NFB, nonglucose-fermenting bacteria.
Discussion
Endophthalmitis after cataract surgery is a severe complication that can occur no matter how strictly the sterility of the operative field is maintained and despite aseptic surgical manipulations/instruments. Risk factors in the surgical procedures and background of the patients are as previously reported, for example, in men, aged patients, and those with capsular rupture, a prior diagnosis of proliferative diabetic retinopathy, and cataract surgery combined with another intraocular surgical procedure on the same day.Citation13,Citation14 Great importance is attached to preventive measures for this complication. Evidence-based prophylactic measures for postcataract surgery endophthalmitis include preoperative instillation of povidone-iodine eye drops as described by Ciulla et alCitation15 and 3-day preoperative sterilization with LVFX eye drops, which was evaluated in a multicenter study sponsored by the Japanese Association for Ocular Infection.Citation12 The pathogens causing endophthalmitis are mainly indigenous bacteria from sites on the ocular surface such as the conjunctival sac, eyelids, and meibomian glands. These microorganisms can be diminished by disinfection, but it is impossible to completely eradicate them even by the strongest disinfection protocol. Microorganisms that are resistant to disinfectants or antimicrobial agents may also be encountered. Although the evidence-based measures that have been demonstrated to be effective for prevention of endophthalmitis after cataract surgery are favorably regarded, it would seem likely that uniform employment of such measures could entail some risk. Therefore, the present study was undertaken to identify significant risk factors.
It is generally agreed that administration of corticosteroids, diabetes mellitus, and old age, which reduce immunity, are associated with a higher bacterial detection rate.Citation4–Citation8 In the present series, however, old age was the only factor associated with a statistically higher bacterial detection rate and no significant difference in bacterial detection was noted in relation to the presence/absence of steroid therapy or diabetes. Furthermore, there was no significant difference in bacterial detection rate among diabetic patients in relation to hemoglobin A1c, diabetic retinopathy, or glycosuria. The reason for this is unclear, but it is possible that these factors have little influence on the microbial flora in the conjunctival sac. Microorganisms isolated from the eye, especially from parts of the ocular surface such as the conjunctiva and cornea, are in direct contact with the external environment and are thought to originate from the palpebral skin influenced by the general condition as well as the meibomian glands and oral indigenous flora. Therefore, these multiple origins could be a reason.
It was found that hyperlipidemia, dry eye syndrome, and use of other topical ocular medication were associated with significantly lower bacterial detection rates. It has been reported that hypercholesterolemia leads to changes in the composition of nasolacrimal duct fluid, so it is possible that such changes may affect the conjunctival sac and its bacterial flora, which are located upstream of the nasolacrimal duct,Citation16 although the precise mechanism is yet to be clarified. Regarding dry eye syndrome, only patients who were using artificial tears or hyaluronic acid eye drops were enrolled, and they showed a lower bacterial detection rate as did the patients using other types of eye drops. Honda et al compared bacterial isolation rates from the conjunctival sac between patients receiving topical medication for glaucoma and those not receiving such medication.Citation10 Bacterial detection rate was 40.3% in the topical medication group, which was significantly lower than the rate of 67.8% in the group without topical medication (P < 0.05, Fisher’s test). These results were similar to the present findings and a washout effect of eye drops may be involved. On the other hand, Hori et al reported that the percentage of LVFX-resistant isolates obtained from the conjunctival sac was higher in patients who had dry eye syndrome compared with healthy subjects.Citation17 They stated that it remains unclear whether fragility of the ocular surface in patients with this syndrome or bacterial contamination of the eyelids and fingers due to application of topical medication is responsible for this finding. Although no such difference in the percentage of LVFX-resistant microorganisms was obtained in the present study (data not shown), this possibility should be kept in mind.
It has been documented that bacteria isolated from the conjunctival sac in healthy persons are usually nonpathogenic, with S. epidermidis being found frequently, which is part of the indigenous skin flora.Citation18 Coagulase-negative staphylococci was the most frequent isolate in the present investigation as well. The isolation rate of methicillin-resistant coagulase-negative staphylococci among coagulase-negative staphylococci was significantly higher in patients with diabetes mellitus than in nondiabetic patients. Possible reasons for this include a compromised immune status due to diabetes, diabetic infections, use of antimicrobial drugs, and opportunistic infections. This also points to the importance of maintaining caution about bacterial drug resistance even if microorganisms are not virulent. Increased drug resistance rates have been pointed out for Corynebacterium spp.Citation19
There is some apprehension regarding an increase of microbial drug resistance due to widespread use of LVFX eye drops. The drug resistance rate increases progressively along with increased use of such eye drops. It is recommended in Japan to administer LVFX eye drops from 3 days before cataract surgery for prevention of postoperative endophthalmitis.Citation15 In the present study, this protocol was followed in all patients, and no oral antibacterial medicine was administered before cataract surgery.
However, indiscriminate use of LVFX could not only lead to masking of resistant microorganisms but could also result in the potential risk of causing an increase in drug resistance. Therefore, attention should be paid to the possible presence of resistant microorganisms especially in elderly patients and patients with dry eye syndrome like those with higher bacterial isolation rates in this study. The same caution should be exercised for diabetic patients since multidrug-resistant isolates with resistance to LVFX, cefmenoxime, and tobramycin were more frequent among diabetics in the present study.
Disclosure
The authors report no conflicts of interest in this work.
References
- ResnikoffSPascoliniDEtya’aleDGlobal data on visual impairment in the year 2002Bull World Health Organ2004821184485115640920
- OshikaTHatanoHKuwayamaYIncidence of endophthalmitis after cataract surgery in JapanActa Ophthalmol Scand200785884885117459028
- SpeakerMGMilchFAShahMKEisnerWKreiswirthBNRole of external bacterial flora in the pathogenesis of acute postoperative endophthalmitisOphthalmology19919856396492062496
- KattanHMFlynnHWJrPflugfelderSCRobertsonCForsterRKNosocomial endophthalmitis survey. Current incidence of infection after intraocular surgeryOphthalmology19919822272382008282
- PhillipsWB2ndTasmanWSPostoperative endophthalmitis in association with diabetes mellitusOphthalmology199410135085188127571
- KurokawaNHayashiKKonishiMYamadaMNodaTMashimaYIncreasing ofloxacin resistance of bacterial flora from conjunctival sac of preoperative ophthalmic patients in JapanJpn J Ophthalmol200246558658912457921
- MillerBEllisPPConjunctival flora in patients receiving immunosuppressive drugsArch Ophthalmol1977951120122014921581
- AllenHFPrevention of postoperative endophthalmitisOphthalmology1978854386389662287
- ToshidaHKogureNInoueNMurakamiATrends in microbial keratitis in JapanEye Contact Lens2007332707317496698
- HondaRToshidaHSutoCEffect of long-term treatment with eye drops for glaucoma on conjunctival bacterial floraInfect Drug Resist2011419119622114511
- Clinical and Laboratory Standards InstitutePerformance Standards for Antimicrobial Susceptibility Testing; Seventeenth Informational Supplement (M100-S17)Wayne, PAClinical and Laboratory Standards Institute2007
- InoueYUsuiMOhashiYShiotaHYamazakiTPreoperative Disinfection Study GroupPreoperative disinfection of the conjunctival sac with antibiotics and iodine compounds: a prospective randomized multicenter studyJpn J Ophthalmol200852315116118661264
- HatchWVCernatGWongDDevenyiRBellCMRisk factors for acute endophthalmitis after cataract surgery: a population-based studyOphthalmology2009116342543019091417
- SteinJDGrossmanDSMundyKMSugarASloanFASevere adverse events after cataract surgery among medicare beneficiariesOphthalmology201111891716172321640382
- CiullaTAStarrMBMasketSBacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based updateOphthalmology20021091132411772573
- MariniRPFoltzCJKerstenDBatchelderMKaserWLiXMicrobiologic, radiographic, and anatomic study of the nasolacrimal duct apparatus in the rabbit (Oryctolagus cuniculus)Lab Anim Sci19964666566629001179
- HoriYMaedaNSakamotoMKohSInoueTTanoYBacteriologic profile of the conjunctiva in the patients with dry eyeAm J Ophthalmol2008146572973418672220
- McNattJAllenSDWilsonLADowellVRJrAnaerobic flora of the normal human conjunctival sacArch Ophthalmol197896814481450678185
- EguchiHKuwaharaTMiyamotoTHigh-level fluoroquinolone resistance in ophthalmic clinical isolates belonging to the species Corynebacterium macginleyiJ Clin Microbiol200846252753218077650