Abstract
Background
Hepatitis E virus (HEV) is an emerging infectious agent that causes acute hepatitis in developing and developed countries. Diagnosis of HEV infection has not been routinely done in Egyptian hospitals, and clinicians do not prescribe ribavirin (RBV) for acute hepatitis cases of unknown etiology (AHUE). We aimed to screen patients with AHUE for the presence of HEV markers and to determine the complications associated with HEV infection.
Patients and Methods
HEV markers (anti-HEV IgM, anti-HEV IgG, and HEV RNA) were assessed in patients with AHUE (n=300) admitted to Assiut University Hospitals. RT-qPCR was used to detect the viral load and sequencing analysis was carried out to determine the genotype of the detected viruses. Phylogenetic tree was constructed to evaluate the genetic relatedness between the isolates. Laboratory parameters and the outcomes of infection were determined.
Results
Acute HEV infection (AHE) was detected in 30 out of 300 (10%) of AHUE patients. Anti-HEV IgM, HEV RNA, and anti-HEV IgG were reported in 83%, 50%, and 43% of the samples, respectively. HEV RNA load ranged from 5×102 IU/mL to 1.1×104 IU/mL. Sequencing of the isolated viruses revealed that five viruses belong to HEV-1 and one isolate belongs to HEV-3 with high homology to the virus recently isolated from the cow and goat milk in the Egyptian villages. Although previous reports showed that attenuated HEV isolates were circulating in Egypt, four out of 30 patients (13%) developed coagulopathy and hepatic encephalopathy and died due to fulminant hepatic failure (FHF) within 3–6 weeks of hospitalization. Age, malignancy, and a history of pre-existing liver diseases were a risky factor for FHF development.
Conclusion
AHE is common in Upper Egypt. Older patients with malignancy and/or a history of liver diseases are risky. HEV diagnosis and treatment become pivotal in Egyptian hospitals to reduce the fatality rate and they should start urgently and promptly.
Introduction
Hepatitis E virus (HEV) causes about 20 million infections and 70,000 deaths per year.Citation1 HEV belongs to the Hepeviridae family and at least five genotypes are known as human pathogens.Citation2 HEV-1 and HEV-2 are associated with waterborne infection in developing countries.Citation3 Vertical transmission of HEV from mother to fetus is documented and the complications are mainly associated with HEV-1.Citation4 HEV-3, HEV-4, and HEV-7 are zoonotic, they are associated with foodborne and blood transfusion infections.Citation5–Citation9
The genome of HEV includes three open reading frames (ORFs). ORF1 encodes the essential enzymes required for viral replication. ORF2 encodes the structural capsid protein. ORF3 is involved in virion morphogenesis and egress from the infected cells.Citation1,Citation9
Most HEV infected patients are asymptomatic.Citation10 The symptoms of AHE are indistinguishable from the symptoms of other acute viral hepatitis (AVH) causes. AHE is a mostly self-limiting disease, however, progress to fulminant hepatic failure (FHF) was recorded in several studies.Citation11,Citation12 Also, HEV causes chronic infection especially in immunocompromised patients such as HIV infected, leukemic and organ transplant patients.Citation13,Citation14 Ribavirin (RBV) is used off-label in the treatment of severe acute and chronic HEV infections.Citation15,Citation16
The incubation period for HEV is about 15 to 60 days. Anti-HEV IgM starts to appear first alongside the development of clinical symptoms and elevation of liver transaminases, followed by the appearance of anti-HEV IgG. HEV RNA is detectable in the blood and stool within 3-week post infection.Citation17 The diagnosis of HEV infection is based on the detection of HEV RNA (gold standard), and anti-HEV antibodies (IgM and/or IgG).Citation17–Citation19 However, the serological markers could be misleading as IgM could stay positives for 6 months after the onset of symptoms.Citation20
The seroprevalence of anti-HEV IgG in Egyptians is among the highest worldwide, reaching up to 84%.Citation21,Citation22 Moreover, an outbreak of HEV was previously reported in rural communities of the Assiut governorate.Citation23 However, HEV infection is a neglected disease in Egypt. HEV diagnosis is not routinely enrolled in the diagnosis of suspected hepatitis cases in Egyptian Hospitals. Consequently, RBV is not prescribed by physicians in AHUE.
Herein, we screened the suspected hepatitis cases admitted to Assiut University hospitals for HEV markers. Ten percent of the samples were reactive to HEV markers. Importantly, we recorded four patients who developed FHF and died due to hepatic encephalopathy and severe liver decompensation as a consequence of AHE.
Patients and Methods
Patient Samples
Patients enrolled in this study were admitted to Assiut University Hospital, Assiut Fever Hospital, and AL-Rajhi Liver hospital, Egypt during the period from September 2016 to December 2018. The enrolled patients had one or more of the clinical symptoms of acute hepatitis including fever, jaundice, dark urine, pale stool, and a tender liver. Blood samples were collected from those patients and screened for the following, liver function tests (LFTs) including liver transaminases (alanine transaminase (ALT) and aspartate transaminase (AST), alkaline phosphatase (ALP) and bilirubin). Also, these samples were screened for routine viral hepatitis markers (as described below) and autoimmune hepatitis disease. Ultrasound-abdomen was done to exclude hepatic cell failure (portal hypertension, ascites). Patients with liver disease of known etiology (for example, HBV, HCV, autoimmune hepatitis, Drug-induced liver injury (DILI), and biliary diseases (diagnosed by radiology imaging) were not included in this study. A complete medical history, including possible routes and risks of hepatitis exposure, was filled for each patient. All participants provided written informed consent, and the protocol of HEV detection in the blood samples of AHUE was approved by the Institutional Review Board (IRB no 17200190) at the Faculty of Medicine, Assiut University, Egypt, in accordance with the provisions of the Declaration of Helsinki.
Routine Laboratory Diagnosis of Acute Viral Hepatitis (AVH) in Assiut Hospitals
Screening for AVH (HAV, HBV, HCV, CMV, and EBV) was done according to the protocol of Assiut University hospitals. Screening for HAV was performed using a rapid test for anti-HAV immunoglobulin M (IgM) (CTK Biotech, San Diego, CA, USA). HBV diagnosis is based on the detection of HBsAg (ACON laboratories, Inc., USA), anti-HBV core IgM (IND Diagnostic, Delta, Canada) and HBV DNA. Screening for HCV was done for anti-HCV IgG using the fourth-generation HCV Tri-Dot test control (Atlas Link, USA) and detection of HCV RNA by qPCR. CMV was performed using anti-CMV-IgM (MyBioSource, Inc. San Diego, USA) and screening of EBV was done by the monospot test. The diagnosis of HEV infection is not routinely done in Assiut hospitals.
Diagnosis of Autoimmune Hepatitis
The diagnosis was based on a clinical history, expected symptoms of an underlying autoimmune etiology and laboratory diagnosis. Laboratory diagnosis includes the detection of antinuclear antibodies (ANA) using ANA Screen IgG ELISA kit (Diagnostic Automation/Cortez Diagnostics INC. Woodland Hills, California, USA), anti-smooth muscle antibodies (ASMA) using ASMA ELISA Kit (MyBioSource, USA), and total human IgG (Thermo Fischer Scientific, USA).
HEV Serology Assays
Anti-HEV IgM and anti-HEV IgG were tested in the patients’ plasma samples using Wantai ELISA kit (Wantai Biologic Pharmacy Enterprise, Beijing, China) according to the manufacturer’s instructions. We included samples collected from healthy Egyptian subjects besides the negative control (NC) provided in the kit, to calculate the cut off (C.O).
HEV RNA Detection and Sequencing of the Isolated Viruses
Viral RNA was extracted from the plasma using QIAamp Viral RNA Mini Kit (Qiagen, Germany) according to the manufacturer’s instructions. HEV RNA was detected and quantified by qPCR using primers targeting HEV ORF2/3 region as described previously.Citation24–Citation27 For sequencing and classification of the isolated viruses, nested PCR was done using primers targeting HEV ORF2 as previously described.Citation24,Citation26,Citation28 The amplified products were sequenced (Macrogen, South Korea). The resulting sequences were analyzed using Bioedit and aligned using Muscle align alongside HEV references downloaded from NCBI GenBank. A phylogenetic tree was constructed using the MEGAX program and a maximum likelihood analysis to determine the genotype and subtype of the isolated viruses according to the classification of Smith et al.Citation2
Statistics
Statistical analyses were performed using the GraphPad Prism software 6 (GraphPad Software, La Jolla, USA). Results are expressed as mean ± SEM, median with interquartile range unless otherwise specified. P value is calculated by the student’s unpaired two-tailed t-test. P < 0.05 was considered significant.
Result
Screening of HEV Markers in AHUE
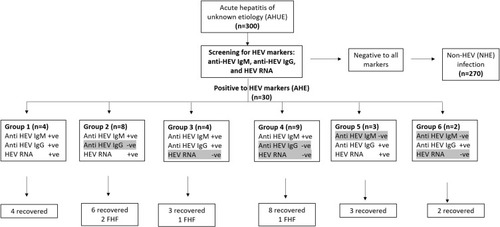
Three hundred (n=300) acute hepatitis cases were screened for HEV markers. The cases were negative for other viral hepatitis causes (HAV, HBV, HCV, CMV, and EBV) and autoimmune hepatitis markers. In addition, medical history excluded the possibility of DILI or alcohol-induced liver injury (). Thirty out of 300 (10%) of the patients were diagnosed with AHE, while 270 samples were tested negative to HEV markers (90%). Twenty-five out of 30 samples were tested positive for anti-HEV IgM (83.33%), HEV RNA was detectable in 15 samples (50%). Anti-HEV IgG was detectable in 43.3% (13/30) of the samples. Two HEV markers were recorded in 15 out of 30 samples (50%), one marker was detectable in 11 samples (36.7%) and the three markers were detectable in 4 samples (13.3%) ().
Figure 1 Schematic flow of the study design. Acute hepatitis symptomatic patients admitted to Assiut University hospitals were assessed for LFTs including liver transaminases and bilirubin. Patients with abnormal LFTs were screened for routine viral hepatitis markers (HAV, HBV, HCV, CMV, and EBV), autoimmune hepatitis markers. Medical history for the patients excluded the possibility of DILI or alcohol-induced liver injury. Samples tested negative to the previously mentioned markers were screened for HEV markers. Patients with liver disease of known etiology (for example HBV, HCV, autoimmune hepatitis, and DILI were not included in this study.
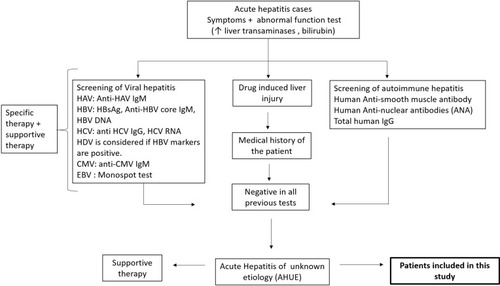
Figure 2 Assessment of HEV markers in AHUE and the outcomes of infection. AHUE (n=300) were screened for HEV markers (anti-HEV IgM, anti-HEV IgG, and HEV RNA). 30 samples were reactive to HEV markers. Four samples were positive to the tested HEV markers (Group 1), 3 samples were positive to anti-HEV IgG and HEV RNA (Group 5) and 2 samples tested positive for anti-HEV IgG (group 6). All the previous patients (Group 1, 5 and 6) recovered without complications. 8 samples were positive to anti-HEV IgM and HEV RNA, and negative for anti-HEV IgG (Group 2), 4 samples tested positive to anti-HEV IgM and anti-HEV IgG, and negative for HEV RNA (Group 3), and 9 samples were tested positive for anti-HEV IgM (Group 4). The previous patients (Group 2, 3, 4, n= 21), 17 patients recovered without complications and 4 patients progressed to FHF. Groups 4 and 6 were also positive for HEV Ag.
Demographic and Laboratory Characterization of AHE Patients
Among 30 AHE patients, 16 patients were male (53%) and 14 patients were female (47%). No statistically significant differences were found between AHE patients and non-HEV infected (NHE) patients with regard to age and sex. The median (interquartile range, IQR) of ALT and AST enzymes in AHE patients were 454 U/l and 357 U/l, respectively, which were significantly higher than the median of these enzymes in NHE patients. While the levels of ALP and bilirubin were comparable in AHE and NHE patients. The median with IQR of the R-value (expressed as (ALT/upper limit normal (ULN) of ALT)/(ALP/ULN of ALP)) was 5.36 in AHE patients, which was significantly higher than in NHE patient (R-value =1.89) ().
Table 1 Demographic and Laboratory of AHE and NHE Infected Patients
Description of the AHE Patients Who Developed Fulminant Hepatic Failure (FHF)
Four cases out of 30 (13%) of AHE patients developed severe decompensated liver and FHF (). FHF patients developed ascites, coagulopathy (INR ≥1.5) and hepatic encephalopathy within 2–3 weeks of the jaundice onset. They died within 3–6 weeks of hospitalization. FHF patients were 3 males (75%) and 1 female (25%), they were older age (age ≥ 60). All FHF patients were living in rural communities and two of them had a history of previous liver disorders. The first patient (patient #1) had admitted to ICU 1 year ago before a recent diagnosis with HEV due to septic shock that required long-standing hospitalization and complicated with liver dysfunction. The second patient (patient #2) had a history of hospital admission due to acute HAV infection few months before the recent diagnosis with HEV. Anti-HEV IgM was detectable in the four cases (100%), HEV RNA was detectable in 2 patients (50%) and anti-HEV IgG was detectable in 1 patient (25%). HEV RNA load was 1.1x104 IU/mL and 2.7x103 IU/mL in patient #1 and patient #2, respectively. The third patient had acute leukemia, and the fourth patient was older (76 years) than the other patients ().
Table 2 Baseline Characteristics of Patients Developed Fulminant Hepatic Failure (FHF)
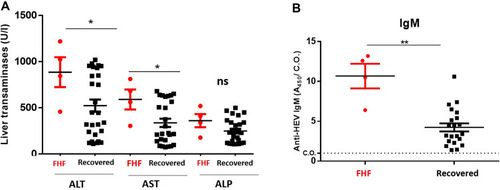
Comparison of FHF Patients with Patients with Self-Limited AHE Patients (Recovered Patients)
Out of 30 AHE patients, 4 cases (13%) developed FHF and 26 cases (87%) had not developed the complications (ie coagulopathy and encephalopathy) and they recovered completely with supportive therapies (). FHF patients were older (median age 69 years) than self-limited AHE patients (median age 51 years). There is no statistical difference between the two groups in terms of sex. The median (with IQR) level of ALT, AST, and bilirubin were significantly higher in FHF patients than self-limited AHE patients. Similarly, the ALP level was higher in FHF cases than in self-limited AHE patients (, ). Anti-HEV IgM was recorded in the FHF cases (4/4, 100%), while this marker was detectable in 80.7% (21/26 cases) of self-limited AHE patients. The level of anti-HEV IgM (as determined by A450/C.O.) was significantly higher in FHF patients than recovered patients (). While anti-HEV IgG was detectable in 12 out of 26 AHE patients (46%) and in 1 out of 4 FHF patients (25%). The mean HEV load was slightly higher in FHF patients (6.8x 103 IU/mL) than self-limited AHE patients (2.76x 103 IU/mL). The previous history of pre-existing liver disease was found to be significantly associated with FHF and the duration of hospitalization was longer for FHF patients. All FHF patients and most self-limited AHE (69%) were living in rural communities ().
Table 3 Comparison of Characteristics of FHF Patients and Acute Self-Limited HEV Patients
Figure 3 Comparison of LFTs and HEV markers in FHF patients and self-limited AHE patients. FHF patients (n=4) and self-limited AHE patients (n=26) were assessed for LFTs and HEV markers. (A) The LFTs (ALT, AST, and ALP) were measured in FHF patients and self-limited AHE patients. (B) The absorbance of anti-HEV IgM (A450/C.O.) was compared in FHF patients and self-limited AHE patients. *, ** means p<0.05 and p≤ 0.01, respectively as determined by two-tailed student’s t test.
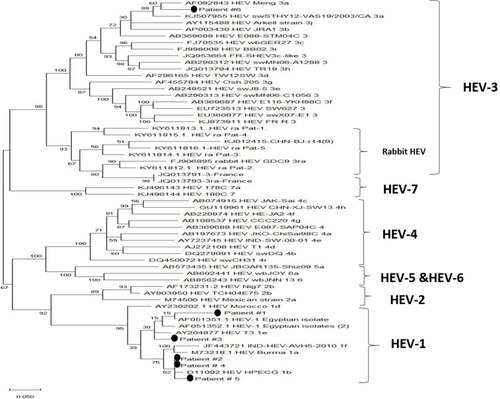
Characterization of the Isolated Viruses from FHF and Self-Limited AHE Patients
HEV RNA was detectable in two cases (2/4, 50%) of FHF patients, the HEV RNA load was 1.1x104 IU/mL and 2.7x103 IU/mL in the two cases, respectively. HEV RNA was also detectable in 50% of recovered patients (13/26 cases). The HEV load in self-limited AHE patients ranged from 5x102 IU/mL to 9.45x103 IU/mL. Sequencing of the isolated viruses was possible in six cases (2 FHF, 4 self-limited AHE patients). Phylogenetic analysis revealed that the isolated viruses from FHF belong to HEV-1, one virus (patient #1) showed a homology to the previous HEV isolate from Egypt (accession number AF51351.1) and the other isolate (patient #2) subclassed to 1b. Similarly, two viruses isolated from self-limited AHE patients (patient #4 and patient #5) belonged to HEV-1 subclass 1b, one virus (patient #3) subdivided the cluster of 1e, and the last isolate (patient #6) subdivided to HEV-3 subtype 3a ().
Figure 4 Phylogenetic analysis of the isolated viruses. A maximum-likelihood phylogenetic tree was constructed using various HEV reference sequences with 1000 bootstrap replicas. GenBank accession numbers are shown for each HEV reference strain used in the phylogenetic analysis. The isolated viruses from the patients were remarked it by putting a circle beside them.
Discussion
Viral hepatitis infections, including HEV, are endemic in many developing countries.Citation29–Citation31 HEV infection was reported as highly endemic in rural Egyptian communities.Citation22 Stoszek et al conducted a prospective cohort study on the villagers in two Egyptian rural communities, 919 villagers were initially anti-HEV IgG negative, after about 10 months 3.7% of the villagers showed reactivity to anti-HEV IgG giving an estimated anti-HEV incidence of 41.6/1000 person-years.Citation21 Also, the reported seroprevalence of HEV among the Egyptian pregnant women was up to 84%, most of the tested women were asymptomatic or had subclinical infection suggesting that these women had prior HEV exposures at the childbearing age.Citation21 In Egypt, HEV caused 13–42% of acute viral hepatitis (AVH) cases.Citation32–Citation34 In the Assiut governate, there was an outbreak of HEV infection in one village (Kom EL Mansoura), where symptomatic HEV cases (n=14) and asymptomatic HEV infections in their family members and contacts (14 cases) were seroconverted to anti-HEV IgM.Citation23 Although the previously mentioned reports, HEV infection is still a neglected disease in Egypt. HEV diagnosis is not routinely done in the screening of AVH cases and/or AHUE in Egyptian hospitals. Besides, HEV research is limited in Egypt and only limited sequences of HEV were characterized. The cause for this neglect despite the previous alerts could be attributed to several reasons: a) Earlier studies done on HEV in Egypt during the period 2000–2006 revealed that HEV infection was self-limiting disease and most AHE cases were asymptomatic or had subclinical infection.Citation21,Citation22 b) One large prospective was done in two governates in Egypt during the period 2006–2008 concluded that HEV-associated AVH is relatively uncommon and an attenuated HEV-1 strain was circulating in Egypt which explained the low mortality rate associated with HEV infection.Citation35 c) Due to the financial limitation in developing countries, most of the available funding sources in Egypt were directed to study other highly endemic hepatotropic viruses such as HCV and HBV.
The research on HEV has been increased globally in the past decade. Therefore, the understanding of HEV ecology has been changed, from a waterborne pathogen causing acute infection in developing countries to a global pathogen causing acute, chronic and extrahepatic manifestations with a possible zoonotic origin.Citation3,Citation36–Citation38 Moreover, HEV infection was underestimated due to the lack of sensitive assay for HEV diagnosis. With the improvement in the sensitivity and specificity of the serological and molecular tools, the diagnosis of HEV has become more reliable and the number of HEV infected cases become accurately estimated.Citation18
In this study, we aimed to investigate HEV prevalence in AHUE (HEV diagnosis is not done in Egyptian hospitals). The LFTs showed an elevation in liver enzymes and bilirubin. Routine laboratory analysis excluded the viral hepatotropic agents such as HAV, HBV, HCV, CMV, and EBV. Also, these samples were tested negative for autoimmune hepatitis markers and the medical history excluded the possibility of DILI. We screened these samples for HEV markers; 10% (30/300) of these samples were showed reactivity to HEV markers and diagnosed with AHE infection according to the guidelines of EASL.Citation17 There was no statistical difference between AHE patients and NHE patients in terms of age and sex. Similar findings were reported in previous studies conducted on Egyptian cohorts in the same geographical area.Citation34,Citation39 In this study, the level of liver transaminases and the ratio of ALT/ALP (R-value) were significantly higher in AHE patients than NHE patients. Similarly, Wallace et al reported that the maximum ALT and ALT/ALP ratio could discriminate between AHE infection and other, nonviral causes of liver dysfunction such as DILI, common bile duct stones, decompensated chronic liver disease, alcoholic liver disease, non-HEV viral hepatitis, autoimmune hepatitis, hepatitis of uncertain cause, ischemic hepatitis, etc. Also, Wallace et al recommended that patients with ALT higher than or equal to 300 IU/l should be tested for HEV and they reported that ALT/ALP ratio (R-value) was higher in AHE infection than other causes of liver dysfunction.Citation40
In this study, anti-HEV IgM, HEV RNA, and anti-HEV IgG were detectable in 83%, 50%, and 43% of AHE samples. The higher prevalence of anti-HEV IgM over HEV RNA and anti-HEV IgG could be attributed to the time of sample collection, probably these samples were collected from the patients immediately after the onset of symptoms had appeared. During HEV infection, antibodies start to appear around the time of clinical onset, with IgM antibodies appearing first, followed by IgG antibodies. HEV RNA is detected in the blood and stool of the patient around 3 weeks post infection.Citation17
In this study, 4/30 (13%) of AHE patients developed severe outcomes, while 26/30 (87%) of AHE cases were recovered. The level of liver transaminases and anti-HEV IgM were significantly higher in FHF patients than self-limited AHE patients at the acute phase of infection. Our results agreed with Saravanabalaji et al who reported that FHF patients had significantly higher anti-HEV IgM and IgG titers than recovered patients.Citation41 HEV is not a hepatotoxic virus and the liver injury is mainly mediated by an immune response against the virus, this could explain the higher prevalence of anti-HEV antibodies in the blood of FHF patients.Citation42 Future studies could ascertain this point. However, the prevalence of HEV RNA (50%) and the viral load were comparable in FHF patients and self-limited AHE patients. Suzuki et al detected HEV RNA in 17% (3/18) of fulminant hepatitis patients in Japan.Citation43 While Saravanabalaji et al reported that HEV RNA could be detected in 7.14% (1/14) of pregnant FHF patients with fatal outcomes, and the HEV RNA detection rate was higher in recovered patients (46%, 22/47). On the other hand, Kar et al reported that the prevalence and HEV RNA load were significantly higher in FHF pregnant patients than AVH pregnant women, and high HEV load during pregnancy was associated with severe outcomes.Citation44 Since HEV diagnosis is not routinely done in Assiut University Hospitals, we could not get access to the stool samples from HEV infected patients. Previous studies showed that the excretion of HEV particles in the stool is more than the blood of infected patients and in vivo animal models.Citation26,Citation45,Citation46
In this study, 4 out of 30 (13%) AHE patients present as a fulminant hepatic failure (FHF). AHE infection contributed to 5–15% of acute liver failure (ALF) cases in developed counties.Citation47,Citation48 FHF patients were older than self-limited AHE patients. Similarly, previous reports showed that Age is a prognostic marker for AHE outcome and old patients had a higher risk of comorbidity when they were infected with HEV.Citation11,Citation49 Two of the FHF patients had a history of liver diseases. In a parallel line, Péron et al described seven patients with FHF in France, six of them had chronic or preexisting liver disease.Citation11 The mortality rates in our study were 13%, which is higher than the known mortality rate of HEV (0.5% to 4%, and reaching up to 25% in pregnant women).Citation3 Also, all FHF patients in this study died (100%). One explanation of the higher fatality rate in our study is that HEV is a neglected disease in Egypt; therefore, those patients only received supportive measures without specific antiviral therapy, ie RBV. RBV is the drug of choice in the treatment of autochthonous AHE infection and reduces the mortality rate in FHF cases.Citation15
In this study, sequencing was done on six isolated viruses from AHE patients (2 FHF patients and 4 self-limited AHE patients). Phylogenetic analysis revealed that five viruses belong to HEV-1 and one isolate belong to HEV-3. Previous studies showed that HEV-1 is circulating in Egypt.Citation35,Citation50 Recently we reported HEV-3 in the cow and goat milk in Assiut rural communities.Citation28,Citation51,Citation52 Interestingly, this patient (HEV-3 infected) was living in the same village where HEV-3 identified in the cow milk and the diagnosis was done within the same period. The patient reported that he often consumed unpasteurized cow milk and its products. Also, most cases of FHF patients and self-limited AHE cases were living in villages and rural communities. Similarly, the reported risk factors associated with HEV transmission among Egyptians were poor sanitation, contamination of drinking water and residing in rural communities where living nearby and/or contact with animals is very common.Citation21,Citation32–Citation34
One limitation in this study, we screened HEV markers in samples that were tested negative for other hepatotropic viruses, autoimmune markers, and DILI. It is possible that HEV could be present in those excluded groups. Coinfection of HBV/HEV or HCV/HEV is common and could lead to more severe outcomes.Citation53,Citation54 In addition, many ALF cases were HEV related and previously misdiagnosed as DILI.Citation55,Citation56 Moreover, HEV was reported in patients diagnosed with autoimmune hepatitis.Citation57 We believe that the actual prevalence of HEV infection and the mortality rate in Assiut University Hospitals are still underestimated. The estimated prevalence of HEV in our study was lower than the prevalence reported in other countries in the Middle East.Citation58 Also, the assay used in HEV detection could affect the prevalence rate since there is a variation in the performance, sensitivity, and specificity between different serological assays.Citation59,Citation60 Future studies should be done to estimate the actual prevalence of HEV in Egypt.
In conclusion, this study shows that AHE infection is common in Egypt. AHE patients may progress to FHF especially older patients with those with a history of liver diseases. HEV diagnosis and treatment become pivotal in Egyptian hospitals to reduce the fatality rate associated with AHE infection and they should be started urgently and promptly.
Abbreviations
A, absorbance; Ag, antigen; AHE, acute hepatitis E; AHUE, acute hepatitis of unknown etiology; ALP, alkaline phosphatase; ALT, alanine aminotransferase; ANA, antinuclear antibodies; AVH, acute viral hepatitis; ASMA, anti-smooth muscle antibodies; AST, alanine aminotransferase; CMV, cytomegalovirus; C.O., cut off; DILI, drug-induced liver injury; EBV, Epstein-Barr virus; FHF, fulminant hepatic failure; HAV, hepatitis A virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HEV, hepatitis E virus; ICU, intensive care unit; Ig, immunoglobulin; INR, international normalized ratio; IQR, interquartile range; IU, international unit; LFTs, liver function tests; NC, negative control; NHE, nonhepatitis E; ORF, open reading frame; qPCR, quantitative polymerase chain reaction; RBV, ribavirin; U, unit; ULN, upper limit normal.
Author Details
Current address of Ibrahim M Sayed, Department of Pathology, School of Medicine, University of California, San Diego, La Jolla, California, USA.
Acknowledgments
The authors are grateful to Assiut Medical Research Center and Reproductive Medical Center for providing the space and instruments for doing the analysis.
Disclosure
The authors declare no conflict of interest.
References
- Sayed IM, Vercouter AS, Abdelwahab SF, Vercauteren K, Meuleman P. Is hepatitis E virus an emerging problem in industrialized countries? Hepatology (Baltimore, Md). 2015;62(6):1883–1892. doi:10.1002/hep.27990
- Smith DB, Simmonds P, Izopet J, et al. Proposed reference sequences for hepatitis E virus subtypes. J General Virol. 2016;97(3):537–542. doi:10.1099/jgv.0.000393
- Rein DB, Stevens GA, Theaker J, Wittenborn JS, Wiersma ST. The global burden of hepatitis E virus genotypes 1 and 2 in 2005. Hepatology (Baltimore, Md). 2012;55(4):988–997. doi:10.1002/hep.25505
- Sharma S, Kumar A, Kar P, et al. Risk factors for vertical transmission of hepatitis E virus infection. J Viral Hepat. 2017;24(11):1067–1075. doi:10.1111/jvh.1273028570034
- Pavio N, Doceul V, Bagdassarian E, Johne R. Recent knowledge on hepatitis E virus in Suidae reservoirs and transmission routes to human. Vet Res. 2017;48(1):78. doi:10.1186/s13567-017-0483-929157309
- Abravanel F, Lhomme S, El Costa H, et al. Rabbit Hepatitis E virus infections in humans, France. Emerg Infect Dis. 2017;23(7):1191–1193. doi:10.3201/eid2307.17031828628452
- Colson P, Borentain P, Queyriaux B, et al. Pig liver sausage as a source of hepatitis E virus transmission to humans. J Infect Dis. 2010;202(6):825–834. doi:10.1086/65589820695796
- Lee GH, Tan BH, Teo EC, et al. Chronic infection with camelid hepatitis E virus in a liver transplant recipient who regularly consumes camel meat and milk. Gastroenterology. 2016;150(2):355–357.e353. doi:10.1053/j.gastro.2015.10.04826551551
- Sayed IM, Vercauteren K, Abdelwahab SF, Meuleman P. The emergence of hepatitis E virus in Europe. Future Virology. 2015;10(6):763–778. doi:10.2217/fvl.15.29
- Al-Sadeq DW, Majdalawieh AF. Seroprevalence and incidence of hepatitis E virus among blood donors, a review. 2017;27(5):e1937. doi:10.1002/rmv.1937
- Péron JM, Bureau C, Poirson H, et al. Fulminant liver failure from acute autochthonous hepatitis E in France, description of seven patients with acute hepatitis E and encephalopathy. J Viral Hepat. 2007;14(5):298–303. doi:10.1111/j.1365-2893.2007.00858.x17439518
- Aherfi S, Borentain P, Raissouni F, et al. Liver transplantation for acute liver failure related to autochthonous genotype 3 hepatitis E virus infection. Clinics and Research in Hepatology and Gastroenterology. 2014;38(1):24–31. doi:10.1016/j.clinre.2013.05.01324462173
- Kamar N, Selves J, Mansuy JM, et al. Hepatitis E virus and chronic hepatitis in organ-transplant recipients. N Engl J Med. 2008;358(8):811–817. doi:10.1056/NEJMoa070699218287603
- Kenfak-Foguena A, Schöni-Affolter F, Bürgisser P, et al. Hepatitis E Virus seroprevalence and chronic infections in patients with HIV, Switzerland. Emerg Infect Dis. 2011;17(6):1074–1078. doi:10.3201/eid/1706.10106721749774
- Péron JM, Abravanel F, Guillaume M, et al. Treatment of autochthonous acute hepatitis E with short-term ribavirin, a multicenter retrospective study. Liver Int. 2016;36(3):328–333. doi:10.1111/liv.1291126179015
- Kamar N, Izopet J, Tripon S, et al. Ribavirin for chronic hepatitis E virus infection in transplant recipients. N Engl J Med. 2014;370(12):1111–1120. doi:10.1056/NEJMoa121524624645943
- EASL Clinical Practice Guidelines on hepatitis E virus infection. Journal of Hepatology. 2018;68(6):1256–1271. doi:10.1016/j.jhep.2018.03.00529609832
- Vollmer T, Knabbe C, Dreier J. Comparison of real-time PCR and antigen assays for detection of hepatitis E virus in blood donors. J Clin Microbiol. 2014;52(6):2150–2156. doi:10.1128/JCM.03578-1324740079
- Trémeaux P, Lhomme S, Chapuy-Regaud S, et al. Performance of an antigen assay for diagnosing acute hepatitis E virus genotype 3 infection. J Clin Virol. 2016;79:1–5. doi:10.1016/j.jcv.2016.03.01927038538
- Al-Sadeq DW, Majdalawieh AF, Mesleh AG, Abdalla OM, Nasrallah GK. Laboratory challenges in the diagnosis of hepatitis E virus. J Med Microbiol. 2018;67(4):466–480. doi:10.1099/jmm.0.00070629485390
- Stoszek SK, Abdel-Hamid M, Saleh DA, et al. High prevalence of hepatitis E antibodies in pregnant Egyptian women. Trans R Soc Trop Med Hyg. 2006;100(2):95–101. doi:10.1016/j.trstmh.2004.12.00516257426
- Stoszek SK, Engle RE, Abdel-Hamid M, et al. Hepatitis E antibody seroconversion without disease in highly endemic rural Egyptian communities. Trans R Soc Trop Med Hyg. 2006;100(2):89–94. doi:10.1016/j.trstmh.2005.05.01916257427
- Shata MT, Daef EA, Zaki ME, et al. Protective role of humoral immune responses during an outbreak of hepatitis E in Egypt. Trans R Soc Trop Med Hyg. 2012;106(10):613–618. doi:10.1016/j.trstmh.2012.07.00422938992
- Sayed IM, Foquet L, Verhoye L, et al. Transmission of hepatitis E virus infection to human-liver chimeric FRG mice using patient plasma. Antiviral Res. 2017;141:150–154. doi:10.1016/j.antiviral.2017.02.01128232247
- Sayed IM, Meuleman P. Murine tissues of human liver chimeric mice are not susceptible to Hepatitis E virus genotypes 1 and 3. J Infect Dis. 2017;216(7):919–920. doi:10.1093/infdis/jix42228968853
- Sayed IM, Verhoye L, Cocquerel L, et al. Study of hepatitis E virus infection of genotype 1 and 3 in mice with humanised liver. Gut. 2017;66(5):920–929. doi:10.1136/gutjnl-2015-31110927006186
- Sayed IM, Verhoye L, Montpellier C, et al. Study of hepatitis E virus ORF2 antigen kinetics in human-liver chimeric mice and its impact on HEV diagnosis. J Infect Dis. 2019;220(5):811–819. doi:10.1093/infdis/jiz17131001628
- Sayed IM, Elkhawaga AA, El-Mokhtar MA. Circulation of hepatitis E virus (HEV) and/or HEV-like agent in non-mixed dairy farms could represent a potential source of infection for Egyptian people. Int J Food Microbiol. 2020;317:108479. doi:10.1016/j.ijfoodmicro.2019.10847931874303
- El-Mokhtar MA, Elgendy SG, Eldin AS, et al. Hepatitis C virus affects tuberculosis-specific T cells in HIV-negative patients. Viruses. 2020;12:1. doi:10.3390/v12010101
- Ali ME, El-Badawy O, Afifi NA, et al. Role of T-Helper 9 cells in chronic hepatitis C-infected patients. Viruses. 2018;10:7. doi:10.3390/v10070341
- Hassan EA, Ahmed EH, Nafee AM, El-Gafary N, Hetta HF, El-Mokhtar MA. Regulatory T Cells, IL10 and IL6 in HCV related hepatocellular carcinoma after Transarterial Chemoembolization (TACE). Egypt j Immunol. 2019;26(1):69–78.31332997
- Zakaria S, Fouad R, Shaker O, et al. Changing patterns of acute viral hepatitis at a major urban referral center in Egypt. Clin Infect Dis. 2007;44(4):e30–36. doi:10.1086/51107417243045
- Divizia M, Gabrieli R, Stefanoni ML, et al. HAV and HEV infection in hospitalised hepatitis patients in Alexandria, Egypt. Eur J Epidemiol. 1999;15(7):603–609. doi:10.1023/A:100751403006210543349
- Hasan G, Assiri A, Marzuuk N, et al. Incidence and characteristics of hepatitis E virus infection in children in Assiut, Upper Egypt. J Int Med Res. 2016;44(5):1115–1122. doi:10.1177/030006051665957527688687
- Blackard JT, Rouster SD, Nady S, et al. Genotypic characterization of symptomatic hepatitis E virus (HEV) infections in Egypt. J Clin Virol. 2009;46(2):140–144. doi:10.1016/j.jcv.2009.07.00719651539
- El-Mokhtar MA, Othman ER, Khashbah MY, et al. Evidence of the extrahepatic replication of Hepatitis E virus in human endometrial stromal cells. Pathogens. 2020;9:4. doi:10.3390/pathogens9040295
- Sayed IM, Seddik MI, Gaber MA, Saber SH, Mandour SA, El-Mokhtar MA. Replication of Hepatitis E Virus (HEV) in primary human-derived monocytes and macrophages in vitro. Vaccines (Basel. 2020;8:2.
- El-Mokhtar MA, Seddik MI, Osman A, et al. Hepatitis E virus mediates renal injury via the interaction between the immune cells and renal epithelium. Vaccines (Basel. 2020;8:3.
- Eldin SS, Seddik I, Daef EA, et al. Risk factors and immune response to hepatitis E viral infection among acute hepatitis patients in Assiut, Egypt. Egypt j Immunol. 2010;17(1):73–86.22053611
- Wallace SJ, Webb GW, Madden RG, et al. Investigation of liver dysfunction, who should we test for hepatitis E? European Journal of Gastroenterology & Hepatology. 2017;29(2):215–220. doi:10.1097/MEG.000000000000078127832041
- Saravanabalaji S, Tripathy AS, Dhoot RR, Chadha MS, Kakrani AL, Arankalle VA. Viral load, antibody titers and recombinant open reading frame 2 protein-induced TH1/TH2 cytokines and cellular immune responses in self-limiting and fulminant hepatitis e. Intervirology. 2009;52(2):78–85. doi:10.1159/00021486219401616
- Pischke S, Hartl J, Pas SD, Lohse AW, Jacobs BC, Van der Eijk AA. Hepatitis E virus, infection beyond the liver? J Hepatol. 2017;66(5):1082–1095. doi:10.1016/j.jhep.2016.11.01627913223
- Suzuki K, Aikawa T, Okamoto H. Fulminant hepatitis E in Japan. N Engl J Med. 2002;347(18):1456. doi:10.1056/NEJM20021031347181912409557
- Kar P, Jilani N, Husain SA, et al. Does hepatitis E viral load and genotypes influence the final outcome of acute liver failure during pregnancy? Am J Gastroenterol. 2008;103(10):2495–2501. doi:10.1111/j.1572-0241.2008.02032.x18785952
- Chalupa P, Vasickova P, Pavlik I, Holub M. Endemic hepatitis E in the Czech Republic. Clin Infect Dis. 2014;58(4):509–516. doi:10.1093/cid/cit78224280093
- Sayed IM, Elkhawaga AA, El-Mokhtar MA. In vivo models for studying Hepatitis E virus infection; Updates and applications. Virus Res. 2019;274:197765. doi:10.1016/j.virusres.2019.19776531563457
- Manka P, Bechmann LP, Coombes JD, et al. Hepatitis E virus infection as a possible cause of acute liver failure in Europe. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2015;13(10):1836–1842.e1832; quiz e1157–1838. doi:10.1016/j.cgh.2015.04.014
- Crossan CL, Simpson KJ, Craig DG, et al. Hepatitis E virus in patients with acute severe liver injury. World J Hepatol. 2014;6(6):426–434. doi:10.4254/wjh.v6.i6.42625018853
- Chau TN, Lai ST, Tse C, et al. Epidemiology and clinical features of sporadic hepatitis E as compared with hepatitis A. Am J Gastroenterol. 2006;101(2):292–296. doi:10.1111/j.1572-0241.2006.00416.x16454833
- Delarocque-Astagneau E, Abravanel F, Moshen A, et al. Epidemiological and virological characteristics of symptomatic acute hepatitis E in Greater Cairo, Egypt. Clin Microbiol Infect. 2012;18(10):982–988. doi:10.1111/j.1469-0691.2011.03727.x22264267
- El-Mokhtar MA, Elkhawaga AA, Sayed IM. Assessment of hepatitis E virus (HEV) in the edible goat products pointed out a risk for human infection in Upper Egypt. Int J Food Microbiol. 2020;330:108784. doi:10.1016/j.ijfoodmicro.2020.10878432659521
- Sayed IM, Hammam ARA. Enhancement of the molecular and serological assessment of Hepatitis E virus in milk samples. 2020;8:8.
- Kumar M, Sharma BC, Sarin SK. Hepatitis E virus as an etiology of acute exacerbation of previously unrecognized asymptomatic patients with hepatitis B virus-related chronic liver disease. J Gastroenterol Hepatol. 2008;23(6):883–887. doi:10.1111/j.1440-1746.2007.05243.x18070014
- López-Fabal MF, Gómez-Garcés JL. [Seroprevalence of hepatitis E virus in patients with hepatitis C and/or infected with HIV]. Revista Espanola De Quimioterapia, Publicacion Oficial De La Sociedad Espanola De Quimioterapia. 2015;28(6):314–316.26621176
- Dalton HR, Fellows HJ, Stableforth W, et al. The role of hepatitis E virus testing in drug-induced liver injury. Aliment Pharmacol Ther. 2007;26(10):1429–1435. doi:10.1111/j.1365-2036.2007.03504.x17850420
- Sayed IM, Vercouter AS, Meuleman P. Hepatitis E virus in acute liver failure, an unusual suspect? Hepatology (Baltimore, Md). 2016;64(6):1837–1839. doi:10.1002/hep.28759
- Llovet LP, Gratacós-Ginés J, Ortiz O, Rodriguez-Tajes S. Higher seroprevalence of hepatitis E virus in autoimmune hepatitis, role of false-positive antibodies. 2020;40(3):558–564. doi:10.1111/liv.14332
- Nasrallah GK, Al Absi ES, Ghandour R, et al. Seroprevalence of hepatitis E virus among blood donors in Qatar (2013-2016). Transfusion. 2017;57(7):1801–1807. doi:10.1111/trf.1411628453178
- Abravanel F, Chapuy-Regaud S, Lhomme S, et al. Performance of two commercial assays for detecting hepatitis E virus RNA in acute or chronic infections. Journal of Clinical Microbiology. 2013;51(6):1913–1916. doi:10.1128/JCM.00661-1323515544
- Aldisi RS, Elsidiq MS, Dargham SR, et al. Performance evaluation of four type-specific commercial assays for detection of herpes simplex virus type 1 antibodies in a Middle East and North Africa population. Journal of Clinical Virology. 2018;103:1–7. doi:10.1016/j.jcv.2018.03.01129597097
