Abstract
Erythema nodosum (EN) is a dermatological manifestation, the common etiologies of which are already widely described. Here, we report the case of a patient who presented an EN, where the etiology was found to be a rare diagnosis: syphilis, a sexually transmitted infection with various clinical presentations. A 42-year-old female patient without any medical condition presented with a clinical picture associating a maculopapular rash at first, and later on a well-defined hypodermic lesion, clinically suggestive of an EN, on the right forearm. The etiologic workup ruled out sarcoidosis, which was the first suspected diagnosis. Positive VDRL-TPHA and recovery within 15 days after benzathine benzylpenicillin administration allowed the diagnosis of syphilis to be made on the EN. EN is a rare manifestation of syphilis that should be kept in mind in these times of strong recrudescence of the disease among men who have sex with men in mainland France but also among heterosexuals in Reunion Island.
Introduction
Erythema nodosum (EN) is a painful inflammation of subcutaneous fat tissue. It is the most common type of panniculitis.Citation1 The first cause of EN is idiopathic, but classically the main causative agents are infectious pathogens such as Streptococcus, Yersinia spp, Mycoplasma, Chlamydia, Histoplasma, Coccidioides, and Mycobacterium; inflammatory diseases such as sarcoidosis and enteropathies; pregnancy; oral contraceptive pills; and paraneoplastic syndrome. However, we reported the case of a 42-year-old female living in Reunion Island, with no medical history and receiving no medical treatment, presenting an EN where the etiology was found to be a rare diagnosis: syphilis.
Observation
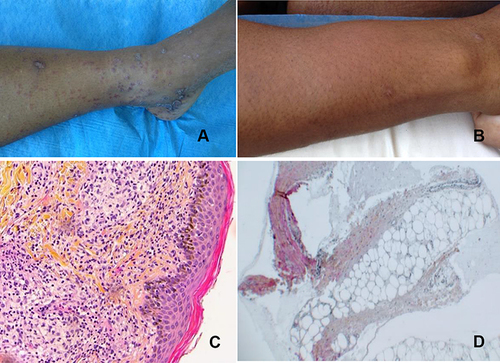
Following three weeks of symptoms, a 42-year-old female presented a persistent and generalised rash, characterised by a pruritic maculopapular rash on the lower limbs (), later extending over the trunk and upper extremities but sparing the palms. She had no fever and no palpable lymph nodes. She also presented a painful inflammatory and well-defined hypodermic lesion on the right forearm () that had developed for 48 hours previously, which was clinically suggestive of an EN. Two skin biopsies were performed on papular lesions (left leg) and on the EN. Awaiting biological and pathological results and suspecting a cutaneous sarcoidosis, dermocorticoids were proposed for the legs. Pathology reported a granulomatous dermatitis with a lichenoid infiltrate in the leg () and confirmed the EN with a septal panniculitis on the arm (). These results supported physicians’ sarcoidosis hypothesis, but no improvement was achieved after dermocorticoids treatment. Before starting a systemic treatment, a blood test diagnosed syphilis (TPHA > 1/1280, VDRL 1/32; Biorad®). Targeted re-interviewing reported a recent divorce and new partners in the last 6 months with unprotected sex. The entire complementary exam presented an elevated CRP (110 mg/L), a polyclonal hypergammaglobulinemia (but no dysimmunity), no other infection (Yersinia, Chlamydia, Mycoplasma, HIV, HBV, HCV, tuberculosis), no other biological dysfunction, normal ECG and no evidence of pulmonary sarcoidosis on a chest CT scan. Given these results, an immunohistochemistry to Treponema pallidum on skin biopsies was requested but came back negative (long-distance transport from Reunion Island to Germany might explain this result for the leg). However, the pathologist reported plasma cells in the leg biopsy, which were highly suggestive of syphilis. The CT scan did not show any signs of visceral syphilis. The patient was treated with an intramuscular injection of benzathine-penicillin G (BPG): 2.4 million units, and complete healing of symptoms occurred within 15 days, confirming the diagnosis of syphilis with EN.Citation2
Discussion
Syphilis is a sexually transmitted infection characterized by an evolution in three stages if untreated.Citation2 Dermatological manifestations occur, particularly in the secondary phase of the disease. However, EN is not described as a classical symptom of this disease, and few cases of EN related to syphilis have been reported ().Citation3–6 If a patient infected with syphilis is undiagnosed and therefore untreated, progression to the tertiary phase with visceral manifestations may occur. Here, despite the negative Treponema immunohistochemistry in the biopsy of the leg, this diagnosis appeared to be a result of syphilis in view of (i) exclusion of frequent causative agents, (ii) presence of plasma cells in the leg biopsy and (iii) regression after BPG.
Table 1 Case Reports of Erythema Nodosum Associated with Syphilis
In a context of resurgence of this infection, mainly among men who have sex with men in developed countries, and also among heterosexuals and women in different parts of the world, it seems primordial to keep in mind this rare differential diagnosis in the presence of an EN.Citation7–10
Ethics and Consent Statement
In accordance with French regulations, this study did not require an Ethics committee nor Comité de Protection des Personnes (article R1121-1, decree n°2017-884 of 9 May 2018 - art.2). No experiments were performed on the patient. Her management relates merely to the rare clinical expression of a pathology and the diagnostic difficulties encountered. The patient gave her written consent for her photos to be published. The patient in this manuscript has given written informed consent for publication of her case details.
Disclosure
The authors report no conflicts of interest for this work.
Acknowledgments
We would like to thank all the team of our STI clinic and our copy editor: Jennifer Sanders.
Additional information
Funding
References
- Chowaniec M, Starba A, Wiland P. Erythema nodosum - review of the literature. Reumatologia. 2016;2:79–82. doi:10.5114/reum.2016.60217
- Janier M, Unemo M, Dupin N, Tiplica GS, Potočnik M, Patel R. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2021;35(3):574–588. doi:10.1111/jdv.16946
- Alinovi A, Lui P, Benoldi D. Syphilis–still a cause of erythema nodosum. Int J Dermatol. 1983;22:310–311. doi:10.1111/j.1365-4362.1983.tb02145.x
- Silber TJ, Kastrinakis M, Taube O. Painful red leg nodules and syphilis: a consideration in patients with erythema nodosum-like illness. Sex Transm Dis. 1987;14:52–53. doi:10.1097/00007435-198701000-00012
- Frishman MP, Smetanin IV. [Case of erythema nodosum in a female patient with secondary recent syphilis]. Vrach Delo. 1975;6:115–116. Russian.
- Guggenheim L. [Erythema nodosum in primary syphilis]. Dermatologica. 1959;118:311–313. German.
- Spiteri G, Unemo M, Mårdh O, Amato-Gauci AJ. The resurgence of syphilis in high-income countries in the 2000s: a focus on Europe. Epidemiol Infect. 2019;147:e143. doi:10.1017/S0950268819000281
- Torrone EA, Miller WC. Congenital and heterosexual syphilis: still part of the problem. Sex Transm Dis. 2018;45:S20–S22. doi:10.1097/OLQ.0000000000000837
- Etienne A, Devos S, Thore E, et al. Increase in early syphilis cases in the young heterosexual population of Reunion Island: surveillance data, 2010–2018. J Eur Acad Dermatol Venereol. 2021;35(9):e573–e575. doi:10.1111/jdv.17294
- Delfosse A, Bouscaren N, Dupin N, et al. High prevalence of syphilis in women, minors and precarious patients: a cross-sectional study in a Reunion Island sexually transmitted infection clinic, 2017–2020. J Eur Acad Dermatol Venereol. 2021;35:2287–2292. doi:10.1111/jdv.17572