Abstract
Influenza virus is a pathogen that causes morbidity and mortality worldwide. Whereas vaccination is important for prevention of disease, given its limitations, antiviral therapy is at the forefront of treatment and also plays a role in prevention. Currently, two classes of antiviral medications, the adamantanes and the neuraminidase inhibitors, are approved for treatment. Given the resistance patterns of circulating influenza, adamantanes are not recommended. Within the US, two neuraminidase inhibitors are currently approved for both treatment and prevention, while worldwide there are four available. In this review, we will briefly discuss the epidemiology and pathology of influenza and then discuss neuraminidase inhibitors: their mechanism of action, resistance, development, and future applications.
Introduction
Influenza viruses are ribonucleic acid (RNA) viruses in the family Orthomyxoviridae. There are three subtypes, influenza A, B, and C, with the majority of human infections caused by subtypes A and B. These viruses are responsible for seasonal influenza, causing yearly epidemics in addition to more sporadic, but potentially devastating, pandemics. From the 1970s through 2007, the annual deaths attributable to influenza have ranged from 3,000 to 50,000 in the US.Citation1 This is likely an underestimate, as many persons who die from influenza may die secondary to complications such as bacterial superinfections or cardiovascular events, in addition to a direct result of the virus itself. The majority of those with more severe illness are the elderly, the very young, those with comorbid conditions, and the immunocompromised.Citation2 Influenza causes fevers, chills, myalgias, and upper respiratory symptoms. When severe, it can cause lower respiratory tract infections and can lead to acute respiratory distress syndrome (ARDS). As a result of the high attack rate, extensive resources and health care expenditures are dedicated yearly to the detection, prevention, and treatment of influenza.
Influenza genes and life cycle
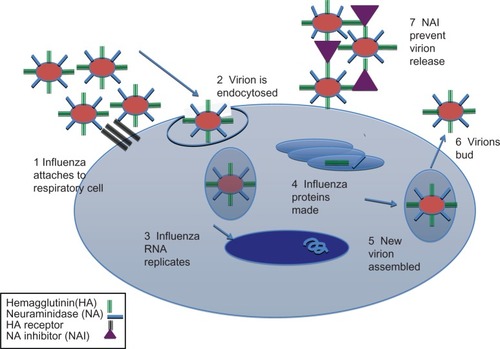
Influenza A is a negative sense RNA virus with a low fidelity RNA polymerase. It contains eight gene segments that encode eleven proteins, including hemagglutinin (HA) and neuraminidase (NA) glycoproteins. The influenza A virus uses HA to attach to sialic acid residues on host cells, which then initiates the infection. Once cells are infected, there are direct necrotic effects on the respiratory cell as the virus begins to use the host cell machinery for replication and turns off host cell RNA transcription and translation.Citation3 NA is responsible for virion release and propagation of infection through cleaving sialic acid residues on host cells. Currently, there are 17 known types of HA, with the majority of human disease caused by H1 and H3 and with occasional cases of infection caused by H5, H7, or H9 viruses. There are ten kinds of NA, with N1, N2, and N9 currently circulating in humans. Influenza B is derived from two lineages – the Victoria and Yamagata strains – named for the place of discovery. Influenza B is not responsible for pandemics because it does not have an animal reservoir.
Each year, influenza develops mutations within these genes leading to antigenic drift. When new HA or NA subtypes are introduced via mixing, or within other species (avian or swine), a new subtype is created–this is called antigenic shift and is responsible for pandemics.Citation4 As influenza evolves within populations, this may also lead to antigenic shift. For example, in the current H7N9 outbreak, evolution within the human host could lead to easier transmission between individuals.Citation5 In the twenty-first century, there has been one pandemic: the 2009 swine H1N1 strain.
In the replication cycle (), influenza first attaches to the host cell by HA, after which the virus is taken into the cell by an endosome. Then the viral RNA replicates and undergoes translation, host genes are suppressed (especially those responsible for immunity), and new virions bud from the surface of the host cell and are released to infect other cells in the host.
Influenza prevention
Current prevention strategies include both vaccination and prophylaxis with antivirals. In the event of novel influenza viruses (such as the current circulating H7N9) or the potential for a new pandemic strain, development of an effective vaccine may be too slow to be effective against spread of infection. Additionally, for some patients who are immunocompromised, vaccination, while beneficial, may not be entirely protective.Citation6 This is also true for the elderly and infants, who do not mount as aggressive an immune response to vaccination and who are at increased risk for more severe disease. Therefore, other preventive measures and treatment must be effective, widely available, and well tolerated.
Vaccination currently targets the HA glycoprotein. Vaccines are designed to match major HA epitopes within the predicted circulating strains of influenza. Given that these epitope sequences may change yearly, vaccination is only effective for the current circulating strains. In years where the predicted strains do not match the actual circulating strains, or during a pandemic where the HA is novel, vaccination may not be as effective or readily available. Other targets for vaccination are currently being examined, including some sites within the HA that are highly conserved and would therefore lead to the creation of antibodies that can neutralize HA from a wide variety of subtypes.Citation7 The matrix (M) protein, which affects virion packaging and release, is highly conserved within influenza subtypes and is therefore an attractive target for future influenza vaccine development. Because it would introduce only T cell immunity, it would likely not replace current antibody-inducing vaccines.Citation8
Epidemiology
During the 2012–2013 influenza season in the US, influenza B (>60% Yamagata, >30% Victoria lineages) and influenza A (H3N2 and 2009 H1N1) strains were the major causes of infection.Citation9 According to the US Centers for Disease Control and Prevention (CDC), over 12,000 patients were hospitalized with laboratory-confirmed influenza during 2012–2013.Citation10 That represents approximately only 9% of all cases/hospitalizations within the US, as these numbers are derived from only 15 states. Thus, the estimate for the 2012–2013 season of hospitalized patients is closer to 137,000.Citation10 Of the samples tested by CDC for the entire season, only two H1N1 and two H3N2 samples demonstrated resistance to the neuraminidase inhibitors (NAIs) oseltamivir and zanamivir.Citation10 In addition, from January to September of 2012, there were approximately 307 human influenza cases with a swine variant H3N2 (H3N2v) in the US; this strain did not demonstrate sustained transmission among humans, and the majority of affected persons had prolonged exposure to pigs.Citation10
Within the US Department of Veterans Affairs (VA) population, 27,972 respiratory samples were tested during the 2012–2013 influenza season; of these, 5,110 (18%) were positive: 76% for influenza A and 23% for influenza B. Of these, 261strains (H3N2, H1N1, and B) underwent NA gene sequencing, and none were found to have NAI resistance mutations (Mark Holodniy, personal observation 2013).
In addition to the current seasonal strains, there have been sporadic human cases of avian H5N1 influenza, and most recently, an H7N9 outbreak in the People’s Republic of China. H5N1 is a highly pathogenic avian influenza that causes high mortality in birdsCitation11 and has a case fatality rate of approximately 60% in humans.Citation12 Fortunately, H5N1 has not yet developed the ability for efficient person-to-person transmission. Human infection with H7N9 was first recognized in Eastern ChinaCitation13 and has recently caused significant morbidity. As of June 1, 2013, 131 patients were documented to have H7N9 infection, with the majority of patients developing severe pneumonia.Citation13–Citation15 The Chinese Center for Disease Control and Prevention has instituted the Chinese National Influenza-Like Illness Surveillance Network, which as of April 28, 2013 had collected 20,739 samples and tested them for H7N9.Citation16 Among those, six were positive for H7N9.Citation16 The majority of patients were male, and the time from onset of symptoms to presentation was around 13 days.Citation17 At the time of this writing, there have been 32 deaths attributed to H7N9.Citation13,Citation18 No cases of H7N9 human-to-human transmission have been documented, although there have been over a thousand close contacts tested.Citation17 Some patients reported exposure to poultry markets, and in Shanghai some birds tested positive for H7N9.Citation19
Current antiviral medications
There are two classes of drugs used to treat influenza: adamantanes and NAIs. The adamantanes are only effective against influenza A viruses, as they inhibit the M2 protein, which is not coded by influenza B. Adamantanes prevent hydrogen ion influx and prevent the virus from uncoating.Citation20 There are two drugs that are licensed (amantadine and rimantadine), but given the high degree of resistance among influenza A strains to these drugs, they are not approved for use and are ineffective against influenza B (which lacks the M2 protein).Citation4,Citation21–Citation24 In the US, there are currently two licensed NAIs – oseltamivir (Tamiflu™; Genentech Inc, South San Francisco, CA, USA) and zanamivir (Relenza™; GlaxoSmithKline, Research Triangle Park, NC, USA). In addition, laninamivir (Inavir®; Daiichi Sankyo, Tokyo, Japan), which is currently licensed in Japan, is undergoing study in the US.Citation25 Peramivir, which is licensed in Japan (Rapiacta®; Shionogi, Tokyo, Japan) and South Korea (PeramiFlu®; Green Cross, Yongin-Si, South Korea) has also been studied in the US, but is not currently approved. There are other promising targets. The influenza RNA polymerase has multiple sites of enzymatic activity; these could be exploited for future drug development.Citation26–Citation28 Additionally, the nucleoprotein (NP), which among other functions wraps the influenza RNA molecules into viral particles, could also be exploited for prevention; drugs using this strategy are currently being investigated.Citation26 Other potential targets include the nonstructural proteins (NS1 and NS2) that suppress the host immune response.Citation26
Neuraminidase glycoprotein and inhibition
The NA protein is a homotetrameric glycoprotein with a stalk region and an enzymatically active head.Citation29 The NA active site cleaves sialic acid at the glycosidic bond on the host cell as well as in respiratory mucus, leading to spread of the virus.Citation30 NAIs act to prevent viral progeny from being released and thus slow the spread of infection.Citation31
The NA active site is highly conserved across both influenza A and BCitation32 and has many charged amino acids that act to bind the sialic acid residues.Citation28,Citation32–Citation34 The majority of these bonds are either hydrogen bonds or charge-charge interactions.Citation34 The degree of polarity within the active site has an impact on the oral bioavailability of NAIs, because NAIs that have a polar side chain, such as zanamivir, are not orally bioavailable.Citation34 The active site contains eight functional residues in addition to eleven framework residues.Citation30,Citation32 Within the different NA subtypes, there are further differences and similarities, and thus they have been grouped into two families: group 1 contains subtypes NA1, NA4, NA5, and NA8; group 2 contains NA2, NA3, NA6, NA7, and NA9.Citation35 Most NAs within group 1 contain a region (the “150 loop/cavity”) that rearranges when bound by a drug or sialic acid to open a cavity that could be exploited for development of new agents.Citation26,Citation33 Influenza B NA appears to have segregated from influenza A relatively early in its evolution into group II and thus is distinct from influenza A NA groups.Citation36
In general, rearrangements necessary for binding of NAIs to influenza B-NA require greater conformational changes than those for influenza A-NA, and this may play a role in the generally better efficacy of NAIs in the treatment of influenza A compared with influenza B.Citation34 It has also been observed that some mutations leading to substitutions within the NA active site that cause oseltamivir resistance, are only active for group 1 NA.Citation33
Current neuraminidase inhibitors
As mentioned previously, there are two NAIs currently licensed in the US and two other NAIs that are licensed in Japan; we will discuss them individually in more depth.
Zanamivir
Zanamivir was the first NAI to be developedCitation37 and was licensed in 1999. It exhibits higher affinity to the NA binding site than does the native sialic acid.Citation21 Given its polarity, it is not well absorbed and is thus delivered as an inhaled agent.Citation21,Citation31 After inhalation, 15% of the drug deposits within the lower respiratory tract.Citation31 Therefore, it can precipitate bronchospasm in patients with pulmonary disease and cannot be used in patients who require mechanical ventilation.Citation31 It is also available in an intravenous (IV) form for compassionate use and is currently undergoing clinical trials to determine optimal dosing.Citation28 For influenza treatment, a 10 mg dose is inhaled twice daily (approved for patients older than 7 years) for 5 days, whereas prophylaxis is given once daily for 10 days (although it can be administered for up to 28 days) in patients older than 5 years of age.Citation28,Citation38 Zanamivir also appears to have higher activity against influenza B and H1N1 strains than oseltamivir, but slightly lower activity against H3N2 compared with oseltamivir.Citation28 It remains active against influenza strains that contain the H275Y (or H274Y) neuraminidase mutation.Citation31 The H275Y mutation is associated with resistance to oseltamivir and peramivir; however, zanamivir, given its more closely retained homology to the natural substrate, is unaffected.Citation4 In immunocompetent patients, no resistance to zanamivir therapy has been demonstrated, though the N294S (N295S) neuraminidase mutation causes decreased sensitivity to zanamivir.Citation21
Oseltamivir
Oseltamivir was developed based on the structure of the active site of zanamivir and is administered as a prodrug that is converted by the liver into its active form.Citation39 Like zanamivir, it is licensed in the US for both treatment and prophylaxis.Citation28 Unlike zanamivir, treatment and prophylaxis dosages are based both on weight and renal function. It has been approved for children as young as 1 year. It is relatively well tolerated, with the most common side effect being gastrointestinal upset, which is mitigated by ingestion along with food; however, there have been reports of neurological side effects in children, noted mostly in Japan.Citation22,Citation40 It is also available for intravenous administration in patients who cannot tolerate oral dosing.Citation28 Resistance to oseltamivir has been documented in patients who have been treated with the drug, but it also has been found in patients without exposure to NA inhibitors.Citation21
Peramivir
Peramivir is offered only as an intravenous formulation because of its low oral bioavailability.Citation28,Citation33 In initial clinical trials, oral peramivir efficacy was no better than placebo, as its absorption was low.Citation33 However, it achieves very high concentrations in the bloodstream.Citation41 It has a slightly lower activity against influenza than either zanamivir or oseltamivir.Citation31 The half-maximal inhibitory concentration (IC50) for influenza B is higher than that for influenza A, but is lower than that for both oseltamivir and zanamivir.Citation42 In addition to gastrointestinal side effects, peramivir has been linked to neutropenia and occasionally to electrocardiographic (ECG) abnormalities.Citation31 It is delivered at 600 mg intravenously twice daily for 5 days in adults, and by weight-based dosing for pediatric patients.Citation28 Like oseltamivir, peramivir resistance is mediated by the H275Y NA mutation.Citation31
Laninamivir
Laninamivir is another inhaled NAI, but is currently licensed only in Japan.Citation28,Citation31 It is a prodrug, like oseltamivir, and is converted to the active form in the respiratory tract.Citation43 It requires only one dose because of its long half-life and is highly concentrated within tissues.Citation28 It is very active against both influenza A and B and has good activity against strains that contain the H275Y NA mutation.Citation28
Mutations in neuraminidase associated with NAI resistance
Numerous excellent reviews have discussed NAI resistance.Citation4,Citation21,Citation28,Citation44,Citation45 NAI resistance is mediated by mutations that change the conformation of the NA active site leading to decreased binding of the NAI to the NA, or by changes in amino acids that change the contact/interaction with the drug.Citation28 Depending on the drug-NA interaction, different changes can lead to different drug susceptibility or resistance. Though ideally the NAI should be as similar to the natural substrate as possible, some differences are needed to ensure that the drug is absorbed and retained.Citation26 In general, the majority of resistance has been seen with oseltamivir; relatively few strains have been found to have zanamivir resistance.Citation44 This may be because zanamivir is more closely related to the natural substrate; however, oseltamivir is also used much more frequently.Citation44 No laninamivir-resistant strains have yet been described.Citation28 Please see for a partial list of resistance mutations.
Table 1 Neuraminidase inhibitor resistance mutations
As an example of the mechanism whereby resistance develops, when oseltamivir binds to the NA target, the NA undergoes a conformational change.Citation21,Citation28 The H274Y (H275Y) and N294S mutations lead to decreased affinity for oseltamivir because they prevent some of the conformational changes from taking place, whereas the R292K lowers affinity for the drug.Citation28,Citation46 However, only in N1 is the H274Y mutation significant, whereas the other two mutations are important for N2 viruses.Citation21,Citation47 H274Y is not located in the active site; however, it causes repositioning in a side chain and decreased binding to oseltamivir and greater binding to sialic acid.Citation26 H274Y does not interfere with binding to zanamivir.Citation26 Also, although oseltamivir binding is inhibited, it appears that sialic acid binding also occurs at a decreased rate compared with the wild-type virus; however, there are compensatory mutations such as R222Q and D344N that allow increased binding of sialic acid.Citation26,Citation48,Citation49 The mutations E119V and R292K also confer resistance to oseltamivir: the E119 mutations via decreasing side chain interaction with the drug; and R292 by inhibiting the rotation of the E276 residue.Citation50 Additionally, R292K decreases affinity to the drug because of decreased interaction with the carboxylate group.Citation50 It could be inferred that other NA subtypes with H274Y mutation (group 1) would be resistant to oseltamivir and that those within group 2 with the E119V and R292K mutations would be resistant as well. The I222V mutation has also been shown to decrease susceptibility to oseltamivir within N1 influenza strains in vitro and appears to have an added effect when paired with H274Y.Citation4,Citation21,Citation51 The McKimm-Breschkin articleCitation21 offers a useful summary of the mechanisms of resistance to NAIs that includes a discussion of structural issues.
Zanamivir and laninamivir are the drugs most similar to the natural target, and therefore resistance is seen less frequently, although it does occur.Citation21,Citation52 It is expected that resistance to these two drugs would cause more harm to the virus as it would lead to greater changes and potentially decreased fitness.Citation21 Peramivir has similarities to both oseltamivir and zanamivir, and thus many of the mutations that confer resistance to either of these drugs lead to cross-resistance with peramivir.Citation21
The N294S mutation leads to decreased susceptibility to both zanamivir and oseltamivir and is seen primarily in N1 subtypes.Citation21 I223R and K mutations can cause resistance to zanamivir.Citation4,Citation53,Citation54 The I222 mutations (I222V, I222R, and I222T) have been seen across N subtypes (and also within influenza B) and result primarily in decreased susceptibility to oseltamivir.Citation21 E119 mutants (E119V, E119I in vivo, E119A/D/G in vitro) can cause decreased susceptibility to different NAIs depending on the substitutionCitation21, and viral fitness can increase when accompanied by the I222V mutation, as demonstrated in H3N2 isolates.Citation55
The majority of mutations to NAIs are caused by mutations within the NA gene itself. Changes to the HA gene and product can also lead to decreased susceptibility to NAIs. These changes in turn decrease the need for NA activity.Citation28,Citation31
Transmission and the effect of NAI resistance
In general, influenza is highly infectious and is transmitted via aerosolized respiratory secretions and large droplets and has an incubation period of 1 to 4 days.Citation2 Persons who are immunocompromised can shed virus for several weeks.Citation56,Citation57
For the 2012–2013 season, oseltamivir resistance within the US was reported to be approximately 1% for H3N2 and 0% for 2009 H1N1 and influenza B strains in circulation.Citation10 However, in 2008–2009, H1N1 oseltamivir resistance had been quite high and widespread in the US, Europe, and other countries.Citation44,Citation58,Citation59 This was not the case in 2009 pandemic H1N1. Additionally, it was once thought that oseltamivir resistance mediated by the H274Y/H275Y mutation led to the decreased viral fitness and transmissibility previously seen in in vitro phenotypic models. This was true from 1999 through 2006. However, during the 2007 season, H1N1 containing the H274Y mutation increased and eventually became the dominant strain in circulation.Citation47,Citation60 What was even more alarming was that resistance in these strains arose without any drug pressure or exposure, suggesting that mutated strain was more fit than the nonresistant strains.Citation47 It has been shown that decreased viral fitness associated with H274Y is mediated by V234M and R22Q NA mutations.Citation49 However, many H274Y strains have unimpaired transmission.Citation61 Within the H3N2 strains, the majority of resistance is mediated by E119V and R292K NA mutations; to date, these appear to result in decreased viral fitness and require higher titers in experimental models to cause infection in ferrets.Citation47
During the 2009 pandemic, the novel H1N1 virus demonstrated susceptibility to oseltamivir. NAI-resistant strains were reported, the majority of those strains were found in immunocompromised hosts and were thought to have arisen secondarily to increased exposure to oseltamivir and prolonged shedding. Studies demonstrated that transmission of oseltamivir-resistant strains may be slightly less efficient than that of the wild-type virus, but resistant strain viral titers tend to be comparable to that of the wild-type virus in vitro.Citation47 As discussed in Govorkova’s excellent reviewCitation62, in some animal models, transmissibility of resistant strains is comparable to that in the wild type, though this is somewhat controversial as other studies have found less efficient transmission of resistant strains.Citation63
For avian H5N1, experimental models have shown that mutations like H274Y and N294S within NA can lead to decreased enzymatic function, but viral fitness appears to be similar to that of wild-type influenza, which is of concern given the high pathogenicity in humans of this avian influenza subtype.Citation47 For the emergent H7N9 subtype, there has not been documentation of transmission between persons.Citation21 However, NAI resistance appears to arise relatively quickly following treatment with oseltamivir.Citation64 The NA gene resistance mutation was documented as R292L and was associated with patients who deteriorated quickly, maintained high viral loads, and required extracorporeal membrane oxygenation (ECMO) support.Citation64
Diagnosis of NAI-resistant influenza mutants
Despite knowledge of mutations associated with resistance to NAIs, there are currently no rapid diagnostics available for clinical laboratories for the detection of strains; the majority of resistance testing is performed at surveillance laboratories. The two main types of diagnostic tests include genotypic and phenotypic assays.
Phenotypic assays rely on culture and are sometimes inaccurate. The sialic acid structures within the cell types used do not bind HA uniformly; some have even lower HA binding in the presence of NAIs, which decreases the utility of NA activity as a measure of antiviral activity.Citation4,Citation47 Therefore, other phenotypic assays that measure NAI enzyme inhibitory activity are more accurate.Citation65 However, though NAI inhibition may be measured accurately, it does not necessarily correlate with viral replication. Currently, most of these tests utilize either chemiluminescent or fluorescent read-out, and both require that the virus be cultured first.Citation4 Chemiluminescent assay is less expensive but requires a higher viral titer for improved accuracy, whereas the fluorescent assay is generally thought to be more accurate.Citation65 Although there are some limitations to phenotypic assays, they are able to detect the effect of both known and unknown resistance mutations and provide a sensitivity profile for the antiviral drug because they measure inhibitory concentration of the drug.Citation65,Citation66 Kits are commercially available and contain reagents, but still require culture of the virus.Citation67 Finally, some studies have combined phenotypic assays with sequencing.Citation68
Genotypic resistance testing is rapid and can be done without viral culture. Current methodologies used for analyzing the influenza NA gene include the polymerase chain reaction (PCR) with Sanger sequencing, next generation sequencing (NGS), real-time PCR (RT PCR), probe hybridization technologies, and single nucleotide polymorphism analysis, among others.Citation4,Citation65 The disadvantages include cost (although the methodologies mentioned are significantly less expensive than phenotypic assays) and the potential that genotypic resistance does not always correlate with phenotypic resistance.Citation65 PCR and population sequencing are used most frequently, although they can be time consuming depending on whether population-based sequencing or clonal analysis is performed. Given that novel mutations can be discovered through whole gene sequencing, assays using PCR with sequencing are attractive applications.Citation65 RT PCR is faster and is used in clinical laboratories for diagnosis of influenza as well as for subtyping. Detection of resistance mutations can be done utilizing a number of methods, such as allele-specific PCR for specific single nucleotide polymorphisms or probe hybridization.Citation65,Citation69,Citation70
NGS analysis of influenza sequences has generally been performed using pyrosequencing.Citation65,Citation71 We have utilized another NGS technique using targeted resequencing to demonstrate low frequency mutations associated with NAI resistance.Citation72 In our study, we sequenced the NA gene from nine clinical samples and were able to detect oseltamivir resistance (H275Y) at 0.18% in one of the nine clinical samples.Citation72 Presently, it is unclear what the clinical significance of low-level frequency mutants may be.
Combination therapy
Given that there are currently only two NAIs licensed in the US, and that there is increasing concern for resistance, the use of combination therapy is promising as it raises the potential of decreasing emerging resistance and increasing efficacy of therapy.Citation73,Citation74 In addition, combination therapy may help in instances in which treatment is started later or in hosts with compromised immune systems.Citation75 Some initial combinations that have been evaluated have been combinations of NAIs themselves, whereas others have investigated combinations of novel NAIs and novel therapies.Citation76,Citation77
In a placebo-controlled study, patients presenting with influenza during the 2008–2009 influenza season were randomized to receive oseltamivir monotherapy with an inhaled placebo (176 patients), oseltamivir/zanamivir combination therapy (192 patients), or a zanamivir plus an oral placebo pill (173 patients).Citation78 The outcome was defined as influenza viral copy number at 48 hours after treatment. The dual therapy was associated with higher viral copy numbers than oseltamivir monotherapy, potentially because zanamivir caused decreased oseltamivir binding.Citation78 In another small study, dual therapy with oseltamivir and zanamivir was compared to oseltamivir alone during the 2009 pandemic; there did not appear to be a difference in efficacy as measured by influenza viral load and symptoms (though the study was underpowered, with only 24 patients).Citation79
Other therapies that have been considered for combination therapy include the NAIs plus adamantanes and ribavirin. Ribavirin is an RNA polymerase inhibitor and is more commonly used for the treatment of respiratory syncytial virus and hepatitis C virus infections. It is available for inhalation therapy, as tablets for oral administration, and, outside the US, intravenously. However, it is teratogenic, can cause hemolytic anemia, neutropenia, and thrombocytopenia, and for those reasons carries a black box warning.
In an in vitro study, Hoopes et al looked at a mathematical and experimental model of emerging resistance with triple combination antiviral drug therapy (TCAD).Citation80 Using oseltamivir, amantadine, and ribavirin, and serial passaging of influenza virus in culture, resistance emerged rapidly when single agents were used. Those authors also demonstrated that although resistance mutations to oseltamivir did occur in the TCAD-treated cells, overall there was a very high barrier to resistance given that multiple mutations were needed to overcome treatment efficacy of the combination, and that in combination amantadine remained active, likely secondary to the effect of ribavirin. Nguyen et al looked at TCAD with amantadine, oseltamivir, and ribavirin using a murine influenza infection model and found that there was a greater than 90% survival in mice treated with TCAD compared with monotherapy (0% amantadine, 20% oseltamivir, 0% ribavirin alone) or dual therapy (50% oseltamivir/amantadine, 60% oseltamivir/ribavirin).Citation75
Kim et al looked at the efficacy of TCAD therapy in critically ill influenza patients admitted to their hospital in Korea using a retrospective analysis.Citation81 One hundred twenty-seven patients were studied, of whom 24 received TCAD and the others received oseltamivir alone. At 14 days, there was a statistically significant trend toward survival in the TCAD group, with 17% mortality for TCAD versus 35% for oseltamivir alone. However, there was no significant difference in survival at 90 days.
Within the US, two clinical trials have been completed that compared TCAD to oseltamivir. Both studies (NCT0867139 and NCT0979251)Citation82,Citation83 looked at TCAD versus oseltamivir monotherapy in immunocompromised hosts. Seo et al published their results of two investigations (Trial NCT0867139)Citation84,Citation86: one on the pharmacokinetics in healthy individuals and another looking at efficacy within immunocompromised hosts. There were two substudies for the TCAD therapy in immunocompromised hosts; one randomized patients older than 7 years to TCAD (oseltamivir, amantadine, ribavirin) or oseltamivir alone, and the other substudy was open label for patients who had more severe disease and who were excluded from randomization. All patients had either undergone chemotherapy or hematopoietic stem cell transplant within the last 2 years and needed to have a positive test for influenza. Three patients were randomized and four participated in the open label study. Given lack of funding, the trial was stopped early. The patients receiving TCAD did demonstrate a decrease in viral load, although one patient progressed to ARDS. A third study, NCT1227967, is examining the efficacy and safety of TCAD and is currently recruiting patients.Citation85
Future neuraminidase inhibitor development
Given the limitations of current drug therapy (for instance, modality of administration and resistance), new therapeutics are needed. In addition to NAIs, other agents are being investigated that have other viral targets, as well as recent studies of other combination therapies.Citation26,Citation28 Quantitative structural relationship models have been used to model new potential NAIs.Citation34
Zanamivir analogs, including laninamivir, have been synthesized.Citation87 With the discovery of the 150 loop/cavity, other compounds are currently being evaluated that would lead to tighter binding of the NA and thus to greater efficacy.Citation33 Given that NA exists on the surface of virions in tetramers, there is increasing interest in finding compounds that would link multiple NAs on the surface of virions, ie, multivalent preparations that may exhibit greater binding affinity and potentially improved pharmacokinetics, in addition to increased potency.Citation33 There has also been interest in developing derivatives of peramivir.Citation33 In addition, benzoic acid is a relatively inexpensive chemical compound that could be utilized for future NAI synthesis.Citation88 Because current NAIs are expensive to produce and require long manufacturing times, synthesis of lower cost benzoic acid derivatives having anti-influenza activity could be quite useful in pandemics.Citation33
NA binds to its substrate by ionic bonds, but recently Kim et al have demonstrated transient covalent bonding.Citation89 This finding may also lead to new drug development. The group has been investigating 2,3 difluorosialic acid compounds as potential therapeutics; these compounds are attractive because they have relatively high affinity and slow dissociation from the NA, leading to very long half lives and prolonged inactivation of NA.Citation89 In their review, Chamni and De-Eknamkul discuss the current patents and the chemical structures of NAIs.Citation90 Additionally, other compounds that interfere with the influenza binding of sialic acid residues, such as DAS181 which cleaves sialic acid residues on host cells, preventing binding by NA, are in clinical trial.Citation91 Other compounds like favipiravir (T-705) are also being developed and have applications for viral infections beyond influenza.Citation27,Citation92,Citation93 In the future, medications such as these, in addition to newer NAIs, will be increasingly important as influenza resistance to current therapies increases.
Guidelines for prophylaxis
Several guidelines have been developed establishing who should receive zanamivir or oseltamivir for influenza prophylaxis. Jackson et al offer a systematic review that details studies looking at the efficacy of prophylaxis, either postexposure or seasonal and outbreak prevention.Citation94 Generally, the adamantanes are not recommended, given the high level of established resistance among influenza strains, but doses of 100 mg orally twice daily can be used if the strain is thought to be susceptible.Citation31 For close household contacts of persons with influenza who have not received the vaccine and who have comorbidities that could lead to complications if they were to become infected, either zanamivir or oseltamivir is effective.Citation95 Other persons who should receive prophylaxis include health care workers who had not practiced proper precautions, and persons who live in nursing homes or other long-term care facilities.
In general, dosing for children is weight based. For household or other close contact postexposure prophylaxis within the US, oseltamivir is approved for adults and children older than 13 years and is dosed at 75 mg orally twice daily for 10 days. Zanamivir is approved for prophylaxis in adults and children older than 5 years, and is dosed at 10 mg inhaled daily for 10 days. Laninamivir has only been licensed for treatment at this time, although given its long half-life it has potential for influenza prophylaxis.Citation28 Patients who receive postexposure prophylaxis should also be vaccinated.Citation95
For persons at risk for influenza complications, such as long-term care facility residents or persons who cannot receive influenza vaccination, prophylaxis is approved for duration of up to 6 weeks, generally during the time of potential exposure.Citation2,Citation95,Citation96 Long-term administration is safe and relatively well tolerated in adults, and in a recent open label study has been found to be safe for long durations in children.Citation97 However, although safe and well tolerated with proven efficacyCitation2, long-term prophylaxis does raise the concern for promotion of NAI resistance.Citation98 In general, prophylaxis with oseltamivir is approximately 68% to 90% effective, and zanamivir is approximately 68% to 80% effective in preventing influenza infection.Citation31,Citation99
Conclusion
In summary, influenza is a respiratory pathogen that causes significant morbidity and mortality globally. There have been four pandemics in the last 100 years, and the threat of a new pandemic is ever present. Vaccination remains the most important cornerstone of prevention. However, depending on vaccination rates, vaccine effectiveness (based on vaccine composition and the population vaccinated), the amount of protection afforded varies considerably. Therefore, antiviral medications such as the NAIs are increasingly important both for treatment and for prophylaxis of vulnerable populations.
Although oseltamivir resistance among circulating influenza strains was low during the 2012–2013 influenza season, given the history of natural variants that circulate and can be transmitted with resistance, there remains a pressing need for other antiviral agents that are active against influenza. Zanamivir continues to demonstrate efficacy and low levels of resistance, but its use is limited in patients who have significant respiratory comorbidities. Laninamivir will be a useful addition if approved in the US, as well as other agents that are currently in the very early stages of drug development. The detection of resistance will also need to be streamlined, allowing for better treatment and prophylaxis decisions to be made in real time.
Acknowledgment
This study was funded by intramural funds from the Department of Veterans Affairs. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Departments of Veterans Affairs or the United States Government.
Disclosure
Both authors report no conflicts of interest in this work.
References
- Estimates of deaths associated with seasonal influenza – United States, 1976–2007MMWR Morb Mortal Wkly Rep82720105933105106220134400
- WilliamsJM2009 update in prevention, evaluation, and outpatient treatment of influenzaCurr Med Res Opin4200925481782819207093
- TreanerJJAvian influenzaMandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases7th edPhiladelphiaChurchill Livingstone201022702271
- ChengVCToKKTseHHungIFYuenKYTwo years after pandemic influenza A/2009/H1N1: what have we learned?Clin Microbiol Rev4201225222326322491771
- BaoCJCuiLBZhouMHHongLGaoGFWangHLive-animal markets and influenza A (H7N9) virus infectionN Engl J Med2013368242337233923697471
- BeckCRMcKenzieBCHashimABHarrisRCNguyen-Van-TamJSUniversity of Nottingham Influenza and the ImmunoCompromised (UNIIC) Study GroupInfluenza vaccination for immunocompromised patients: systematic review and meta-analysis by etiologyJ Infect Dis201220681250125922904335
- CortiDVossJGamblinSJA neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutininsScience2011333604485085621798894
- LambeTSpencerAJMullarkeyCET-cell responses in children to internal influenza antigens, 1 year after immunization with pandemic H1N1 influenza vaccine, and response to revaccination with seasonal trivalent-inactivated influenza vaccinePediatr Infect Dis J62012316e86e9122466328
- Centers for Disease Control and Prevention National and Regional Level Outpatient Illness and Viral Surveillance2013 Available from: http://gis.cdc.gov/grasp/fluview/fluportaldashboard.htmlAccessed August 7, 2013
- Centers for Disease Control and Prevention Seasonal Influenza (Flu)Situation update: summary of weekly FluView Available from http://www.cdcgov/flu/weekly/summary.htmAccessed August 7, 2013
- Centers for Disease Control and Prevention Seasonal Influenza (Flu)Highly Pathogenic Avian Influenza A (H5N1) Virus Available from http://www.cdc.gov/flu/avianflu/h5n1-virus.htmAccessed August 7, 2013
- Centers for Disease Control and Prevention Seasonal Influenza (Flu)Highly Pathogenic Avian Influenza A (H5N1) in People Available from http://www.cdc.gov/flu/avianflu/h5n1-people.htmAccessed August 7, 2013
- World Health Organization InfluenzaFrequently Asked Questions on human infection caused by the avian influenza A (H7N9) virus2013 Available from http://www.who.int/influenza/human_animal_interface/faq_H7N9/en/index.htmlAccessed August 7, 2013
- KeYWangYZhangWHuangLChenZDeaths associated with avian influenza A(H7N9) virus in ChinaAnn Intern Med2013159215916023856693
- GaoHNLuHZCaoBClinical findings in 111 cases of influenza A (H7N9) virus infectionN Engl J Med6132013368242277228523697469
- XuCHaversFWangLMonitoring avian influenza A(H7N9) virus through national influenza-like illness surveillance, ChinaEmerg Infect Dis20131981289129223879887
- KeYWangYLiuSHigh severity and fatality of human infections with avian influenza A (H7N9) infection in ChinaClin Infect Dis Epub872013
- GaoRCaoBHuYHuman infection with a novel avian-origin influenza A (H7N9) virusN Engl J Med2013368201888189723577628
- LeeSSWongNSLeungCCExposure to avian influenza H7N9 in farms and wet marketsLancet20133819880181523664058
- TakedaMPekoszAShuckKPintoLHLambRAInfluenza a virus M2 ion channel activity is essential for efficient replication in tissue cultureJ Virol20027631391139911773413
- McKimm-BreschkinJLInfluenza neuraminidase inhibitors: antiviral action and mechanisms of resistanceInfluenza Other Respi Viruses20137Suppl 12536
- SchirmerPHolodniyMOseltamivir for treatment and prophylaxis of influenza infectionExpert Opin Drug Saf20098335737119355841
- DeydeVMXuXBrightRASurveillance of resistance to adamantanes among influenza A(H3N2) and A(H1N1) viruses isolated worldwideThe Journal of Infectious Diseases2007196224925717570112
- BrightRAMedinaMJXuXIncidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concernLancet200536694921175118116198766
- BiotaSafety, tolerability and pharmacokinetic study of multiple doses of CS-8958 Available from: http://clinicaltrials.gov/ct2/results?term=laninamivirAccessed August 7, 2013
- DasKAntivirals targeting influenza A virusJ Med Chem201255146263627722612288
- FurutaYTakahashiKShirakiKT-705 (favipiravir) and related compounds: Novel broad-spectrum inhibitors of RNA viral infectionsAntiviral Res20098239510219428599
- SamsonMPizzornoAAbedYBoivinGInfluenza virus resistance to neuraminidase inhibitorsAntiviral Res201398217418523523943
- VargheseJNLaverWGColmanPMStructure of the influenza virus glycoprotein antigen neuraminidase at 2.9 A resolutionNature1983303591235406843658
- ColmanPMVargheseJNLaverWGStructure of the catalytic and antigenic sites in influenza virus neuraminidaseNature1983303591241446188957
- IsonMGClinical use of approved influenza antivirals: therapy and prophylaxisInfluenza Other Respi Viruses20137Suppl 1713
- BurmeisterWPRuigrokRWCusackSThe 2.2 A resolution crystal structure of influenza B neuraminidase and its complex with sialic acidEMBO J199211149561740114
- FengEYeDLiJRecent advances in neuraminidase inhibitor development as anti-influenza drugsChemMedChem2012791527153622807317
- GongJZLiuYXuWFPharmacophore model of influenza neuraminidase inhibitors – a systematic reviewPharmazie2009641062763219947162
- RussellRJHaireLFStevensDJThe structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug designNature20064437107454916915235
- XuJDavisCTChristmanMCEvolutionary history and phylodynamics of influenza A and B neuraminidase (NA) genes inferred from large-scale sequence analysesPloS ONE201277e3866522808012
- von ItzsteinMWuWYKokGBRational design of potent sialidase-based inhibitors of influenza virus replicationNature199336364284184238502295
- GlaxoSmithKlineRelenza: Prescribing information Available from: http://us.gsk.com/products/assets/us_relenza.pdfAccessed August 7, 2013
- KimCULewWWilliamsMAInfluenza neuraminidase inhibitors possessing a novel hydrophobic interaction in the enzyme active site: design, synthesis, and structural analysis of carbocyclic sialic acid analogues with potent anti-influenza activityJ Am Chem Soc1997119468169016526129
- BeckCRSokalRArunachalamNUK Antiviral Effectiveness Review GroupNeuraminidase inhibitors for influenza: a review and public health perspective in the aftermath of the 2009 pandemicInfluenza Other Respi Viruses20137Suppl 11424
- BoltzDAAldridgeJRJrWebsterRGGovorkovaEADrugs in development for influenzaDrugs201070111349136220614944
- ChairatKTarningJWhiteNJPharmacokinetic properties of anti-influenza neuraminidase inhibitorsJ Clin Pharmacol201353211913923436258
- KoyamaKTakahashiMNakaiNPharmacokinetics and disposition of CS-8958, a long-acting prodrug of the novel neuraminidase inhibitor laninamivir in ratsXenobiotica201040320721620146556
- ThorlundKAwadTBoivinGThabaneLSystematic review of influenza resistance to the neuraminidase inhibitorsBMC Infect Dis20111113421592407
- FerrarisOLinaBMutations of neuraminidase implicated in neuraminidase inhibitors resistanceJ ClinVirol20084111319
- EarhartKCElsayedNMSaadMDOseltamivir resistance mutation N294S in human influenza A(H5N1) virus in EgyptJournal of Infection and Public Health200922748020701864
- BaranovichTWebsterRGGovorkovaEAFitness of neuraminidase inhibitor-resistant influenza A virusesCurr Opin Virol1220111657458122440915
- Rameix-WeltiMAMunierSLe GalSNeuraminidase of 2007–2008 influenza A(H1N1) viruses shows increased affinity for sialic acids due to the D344N substitutionAntivir Ther201116459760321685548
- BloomJDGongLIBaltimoreDPermissive secondary mutations enable the evolution of influenza oseltamivir resistanceScience201032859831272127520522774
- VargheseJNSmithPWSollisSLDrug design against a shifting target: a structural basis for resistance to inhibitors in a variant of influenza virus neuraminidaseStructure1998667357469655825
- PizzornoABouhyXAbedYBoivinGGeneration and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitorsJ Infect Dis20112031253121148493
- HurtACLeeRTLeangSKIncreased detection in Australia and Singapore of a novel influenza A(H1N1)2009 variant with reduced oseltamivir and zanamivir sensitivity due to a S247N neuraminidase mutationEuro Surveill20111623 article Id=19884
- NguyenHTFryAMLovelessPARecovery of a multidrug-resistant strain of pandemic influenza A 2009 (H1N1) virus carrying a dual H275Y/I223R mutation from a child after prolonged treatment with oseltamivirClin Infect Dis201051898398420858074
- van der VriesEStelmaFFBoucherCAEmergence of a multidrug-resistant pandemic influenza A (H1N1) virusN Eng J Med201036313811382
- SimonPHolderBPBouhyXThe I222V neuraminidase mutation has a compensatory role in replication of an oseltamivir-resistant influenza virus A/H3N2 E119V mutantJ Clin Microbiol201149271571721106781
- GhedinELaplanteJDePasseJDeep sequencing reveals mixed infection with 2009 pandemic influenza A (H1N1) virus strains and the emergence of oseltamivir resistanceJ Infect Dis2011203216817421288815
- WeinstockDMGubarevaLVZuccottiGProlonged shedding of multidrug-resistant influenza A virus in an immunocompromised patientN Eng J Med20033489867868
- MeijerALackenbyAHungnesOOseltamivir-resistant influenza virus A (H1N1), Europe, 2007–2008 seasonEmerg Infect Dis200915455256019331731
- DharanNJGubarevaLVMeyerJJOseltamivir-Resistance Working GroupOseltamir Infections with oseltamivir-resistant influenza A (H1N1) virus in the United StatesJAMA2009301101034104119255110
- LackenbyAHungnesODudmanSGEmergence of resistance to oseltamivir among influenza A(H1N1) viruses in EuropeEuro Surveill2008135 article Id=8026
- BazMAbedYSimonPEffect of the neuraminidase mutation H274Y conferring resistance to oseltamivir on the replicative capacity and virulence of old and recent human influenza A(H1N1) virusesJ Infect Dis2010201574074520100088
- GovorkovaEAConsequences of resistance: in vitro fitness, in vivo infectivity, and transmissibility of oseltamivir-resistant influenza A virusesInfluenza Other Respi Viruses20137Suppl 15057
- DuanSBoltzDASeilerPCompetitive transmissibility and fitness of oseltamivirsensitive and resistant pandemic influenza H1N1 viruses in ferretsInfluenza Other Respi Viruses20115Suppl 17982
- HuYLuSSongZAssociation between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistanceLancet201338198852273227923726392
- Okomo-AdhiamboMSheuTGGubarevaLVAssays for monitoring susceptibility of influenza viruses to neuraminidase inhibitorsInfluenza Other Respi Viruses20137Suppl 14449
- GubarevaLVWebsterRGHaydenFGDetection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assayAntiviral Res2002531476111684315
- BiosystemsANA-Star Influenza Neuraminidase Inhibitor Resistance Detection Kit Available from: http://www3.appliedbiosystems.com/cms/groups/applied_markets_marketing/documents/generaldocuments/cms_042653.pdfAccessed August 7, 2013
- McKimm-BreschkinJTrivediTHampsonANeuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivirAntimicrob Agents Chemother20034772264227212821478
- DuanSBoltzDALiJNovel genotyping and quantitative analysis of neuraminidase inhibitor resistance-associated mutations in influenza a viruses by single-nucleotide polymorphism analysisAntimicrob Agents Chemother201155104718472721730113
- SuzukiYSaitoRSatoIIdentification of oseltamivir resistance among pandemic and seasonal influenza A (H1N1) viruses by an His275Tyr genotyping assay using the cycling probe methodJ Clin Microbio2011491125130
- DeydeVMOkomo-AdhiamboMSheuTGPyrosequencing as a tool to detect molecular markers of resistance to neuraminidase inhibitors in seasonal influenza A virusesAntiviral Res2009811162418835410
- FlahertyPNatsoulisGMuralidharanOUltrasensitive detection of rare mutations using next-generation targeted resequencingNucleic Acids Res2012401e222013163
- PerelsonASRongLHaydenFGCombination antiviral therapy for influenza: predictions from modeling of human infectionsJ Infect Dis2012205111642164522448006
- NguyenJTHoopesJDLeMHTriple combination of amantadine, ribavirin, and oseltamivir is highly active and synergistic against drug resistant influenza virus strains in vitroPLoS ONE201052e933220179772
- NguyenJTSmeeDFBarnardDLEfficacy of combined therapy with amantadine, oseltamivir, and ribavirin in vivo against susceptible and amantadine-resistant influenza A virusesPLoS ONE201271e3100622292088
- SmeeDFHurstBLWongMHEffects of the combination of favipiravir (T-705) and oseltamivir on influenza A virus infections in miceAntimicrob Agents Chemother201054112613319901093
- TarbetEBMaekawaMFurutaYCombinations of favipiravir and peramivir for the treatment of pandemic influenza A/California/04/2009 (H1N1) virus infections in miceAntiviral Res201294110311022429564
- DuvalXvan der WerfSBlanchonTBivir Study GroupEfficacy of oseltamivir-zanamivir combination compared to each monotherapy for seasonal influenza: a randomized placebo-controlled trialPLoS Med2010711e100036221072246
- EscuretVCornuCBoutitieFOseltamivir-zanamivir bitherapy compared to oseltamivir monotherapy in the treatment of pandemic 2009 influenza A(H1N1) virus infectionsAntiviral Res201296213013722909899
- HoopesJDDriebeEMKelleyETriple combination antiviral drug (TCAD) composed of amantadine, oseltamivir, and ribavirin impedes the selection of drug-resistant influenza A virusPLoS ONE2011612e2977822220216
- KimWYYoung SuhGHuhJWKorean Society of Critical Care Medicine H1N1 CollaborativeTriple-combination antiviral drug for pandemic H1N1 influenza virus infection in critically ill patients on mechanical ventilationAntimicrob Agents Chemother201155125703570921968371
- Fred Hutchinson Cancer Research CenterTCAD vs. Monotherapy for Influenza A in Immunocompromised Patients Available from: http://clinicaltrials.gov/show/NCT0867139. NLM identifier: NCT0867139Accessed August 23, 2013
- Adamas Pharmaceuticals, IncOral Triple Combination Antiviral Drug Therapy for Treatment of Influenza A in Immunocompromised Subjects (PO206) Available from: http://clinicaltrials.gov/show/NCT0979251. NLM identifier: NCT0979251Accessed August 23, 2013
- Fred Hutchinson Cancer Research CenterTCAD vs. Monotherapy for Influenza A in Immunocompromised Patients Available from: http://clinicaltrials.gov/show/NCT0867139. NLM Identifier: NCT0867139Accessed August 23, 2013
- National Institute of Allergy and Infectious DiseasesComparing the Efficacy, Safety, and Tolerability of Combination Antivirals (Amantadine, Ribavirin, Oseltamivir) Versus Oseltamivir for the Treatment of Influenza in Adults at Risk for Complications (IRC003) Available from: http://clinicaltrials.gov/ct2/show/NCT1227967. NLM Identifier: NCT1227967Accessed August 23, 2013
- SeoSEnglundJANguyenJTCombination therapy with amantadine, oseltamivir and ribavirin for influenza A infection: safety and pharmacokineticsAntivir Ther201318337738623264438
- YamashitaMTomozawaTKakutaMCS-8958, a prodrug of the new neuraminidase inhibitor R-125489, shows long-acting anti-influenza virus activityAntimicrob Agents Chemother200953118619218955520
- KruegerACXuYKatiWMSynthesis of potent pyrrolidine influenza neuraminidase inhibitorsBioorg Med Chem Lett20081851692169518242993
- KimJHResendeRWennekesTMechanism-based covalent neuraminidase inhibitors with broad-spectrum influenza antiviral activityScience20133406128717523429702
- ChamniSDe-EknamkulWRecent progress and challenges in the discovery of new neuraminidase inhibitorsExpert Opin Ther Pat201323440942323369206
- MossRBHansenCSandersRLA phase II study of DAS181, a novel host directed antiviral for the treatment of influenza infectionJ Infect Dis2012206121844185123045618
- KisoMTakahashiKSakai-TagawaYT-705 (favipiravir) activity against lethal H5N1 influenza A virusesProc Natl Acad Sci U S A2010107288288720080770
- SleemanKMishinVPDeydeVMIn vitro antiviral activity of favipiravir (T-705) against drug-resistant influenza and 2009 A(H1N1) virusesAntimicrob Agents Chemother20105462517252420350949
- JacksonRJCooperKLTappendenPOseltamivir, zanamivir and amantadine in the prevention of influenza: a systematic reviewJ Infect2011621142520950645
- Centers for Disease Control and Prevention Seasonal Influtenza (Flu)Use of Antivirals Available from: http://www.cdc.gov/flu/professionals/antivirals/antiviral-use-influenza.htm#postexposureAccessed August 7, 2013
- HarperSABradleyJSEnglundJAExpert Panel of the INfectious Diseases Society of AmericaSeasonal influenza in adults and children – diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of AmericaClin Infect Dis20094881003103219281331
- ReisingerKShuDCupelliLSafety and tolerability of a 6-week course of oseltamivir prophylaxis for seasonal influenza in childrenInfluenza Other Respi Viruses2013711113
- BazMAbedYPapenburgJEmergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxisN Eng J Med20093612322962297
- MosconaANeuraminidase inhibitors for influenzaN Engl J Med2005353131363137316192481