Abstract
Background
Stenotrophomonas maltophilia (S. maltophilia) is a pathogen causing opportunistic and nosocomial infections that are invasive and fatal, especially in hospitalized and immunocompromised patients. However, community-acquired S. maltophilia is rarely reported in children with normal immunity. S. maltophilia is a multi-drug-resistant bacterium, and the preferred drug is trimethoprim/sulfamethoxazole (TMP/SMX), which has greater side effects in children.
Case Presentation
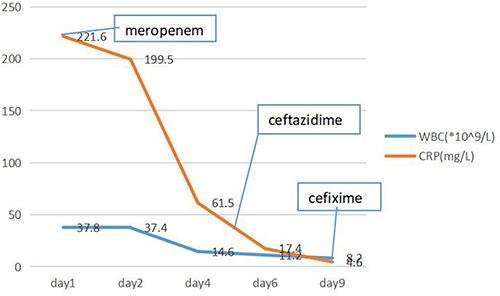
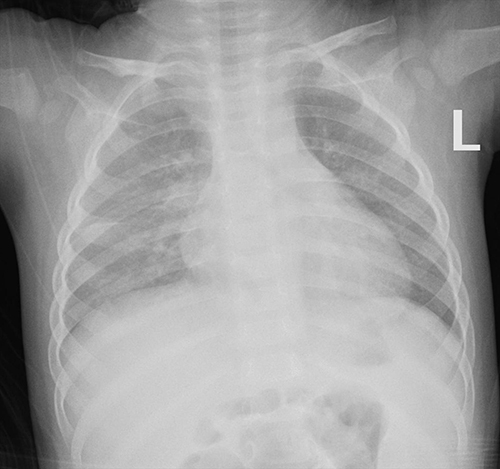
Herein, we reported the case of a child with clinical manifestations of fever, high C-reactive protein (CRP) and white blood cells, and severe pneumonia. The blood culture yielded S. maltophilia. The initial treatment regimen was meropenem IV, which was subsequently changed to ceftazidime IV, and finally to oral cefixime, which has less side effects in children. The child recovered completely. At the 1-month follow-up, anteroposterior chest X-ray was normal, and the child was in good general health.
Conclusion
Although community-acquired S. maltophilia infection in children is rare, it can occur. The doctor encountered such a child in clinical work. This child has a normal immune system, his disease comes from a community infection and has lobar pneumonia located in the lower lung area. At the same time, the child’s white blood cells and CRP values are high, the doctor should be concerned that the child may have S. maltophilia infection. When treating patients, doctors can try to use drugs empirically, such as ceftazidime, instead of using ciprofloxacin, SMZ and other drugs that have relatively large side effects in children. It is worth mentioning that doctors also need to adjust the medication in a timely manner according to the efficacy evaluation and drug sensitivity of the children after the medication, so as to minimize the drug resistance of community-acquired infections. This will prevent the misuse of Meropenem, which has been given in a community patient and that too in a child. Its important to prevent this malpractise.
Introduction
Stenotrophomonas maltophilia (S. maltophilia) is an aerobic, non-fermentative, Gram-negative bacillusCitation1 that is widely found in the environment and can be isolated from sediments, plant rhizosphere,Citation2 food, plastic surfaces of indwelling medical devices and contaminated water.Citation3 In immunocompromised patients, the bacterium can cause opportunistic infections. Among nosocomial infections of non-fermentative pathogens, S. maltophilia is most commonly isolated after Pseudomonas aeruginosa and Acinetobacter.Citation3 However, community-acquired infections of S. maltophilia is very rare in children. S. maltophilia is one of the environmental global emerging multiple-drug-resistant organisms (MDROS).Citation4 The preferred drug for treatment is trimethoprim/sulfamethoxazole (TMP/SMX), but its resistance rate is gradually increasing.Citation4 So it is very difficult to treat the diseases caused by this bacterium. Herein, we reported a spontaneous community-acquired infection of S. maltophilia in a child who was successfully treated with meropenem and ceftazidime. We also conducted a review of relevant literature on community-acquired S. maltophilia in children over the last decade (2012–2022).
Case Report
A 1-year-old female infant of Han ethnicity was admitted to the Department of Pediatrics, ShaoXing KeQiao Women and Children’s hospital in ShaoXing, China, due to occasional cough for four days and intermittent fever for two days. During the Spring Festival, she visited her rural hometown for more than half a month where the environment was poor. She developed cough on the 2nd day after returning to live in the city. During this period, she only had poor appetite. The child had no other medical problems. She had no previous history of any underlying disease and preterm birth. Upon admission to the hospital, all of her vital signs were normal. However, palpable wet rales were heard in both lungs. Anteroposterior chest Xray showed pneumonia on the right side (). Laboratory results showed white blood cells 37.8*10^9 g/L, with 73.6% neutrophils, elevated CRP 221.6 mg/L (normal value 8 mg/L), but low blood oxygen saturation around 89%. The patient was given meropenem 0.18 g q8h IV and symptomatic supportive therapy such as oxygen. The temperature of the patient fluctuated between 36.0 and 37.4°C after admission. On the first day during hospitalization, the patient’s first blood is put into a blood culture bottle, and the culture bottle is put into an automatic bacterial culture system instrument, which automatically detects the presence of bacteria. The physicians in the laboratory then transfer the culture onto Columbia blood agar plates (which include: peptone, animal tissue extract, yeast extract, agar powder, nutritional supplements, and purified water) and place it at 35°C-37°C. The bacteria reappeared after 48 hours of incubation in an incubator. The petri dish was then placed in an automatic microbial identification and drug sensitivity analyzer, which was finally identified as S. maltophilia. Since the drug susceptibility data of S. maltophilia was not included in the bacterial library of the automatic microbial identification and drug susceptibility analyzer in our hospital, the drug susceptibility results could not be obtained automatically. On day 5, the laboratory doctor performed the drug susceptibility test on the cultured bacteria by Kirby-bauer test, and the drug susceptibility results of ceftazidime, levofloxacin, minocycline and TMP/SMX are sensitivity, and the drug susceptibility results of meropenem and cefixime were intermediate. Subsequently, the treatment was changed to ceftazidime 0.45 g bid IV. About 10 days after starting treatment (ceftazidime IV), the patient’s cough improved, lung rales were significantly decreased, repeat blood culture was negative, and repeat chest X-ray showed significant improvement. Thereafter, she was discharged and continued with oral common cefixime 25 mg bid for a 1-week. During the follow-up at one month after discharge, the child’s symptoms were completely relieved () and her chest X-ray showed a marked improvement over the previous X-ray. ().
Discussion and Conclusion
The World Health Organization (WHO) lists S. maltophilia as one of the leading drug-resistant pathogens of greatest public health concern in hospitals worldwide.Citation5 The bacterium mainly infects hospitalized and immunocompromised patients, while community-acquired infections are rarely reported. S. maltophilia can easily survive in sink drains, faucets, water, and sponges, etc.Citation4 With the advancements in the detection methods, the reports of community-acquired S. maltophilia infections are gradually increasing, although related reports in children are rare. Herein, we reported a case of community-acquired S. maltophilia infection in a child with normal immunity. Studies have identified that the main routes of transmission of S. maltophilia are through direct contact and aerosol,Citation4 usually causing human respiratory infections, followed by bacteremia. We searched the PubMed database using “Stenotrophomonas maltophilia, children, community acquired” as the keywords, and found only seven case reports of community-acquired infection in children in the past decade (2012–2022).Citation6–9 These seven patients developed meningitis, bacteremia, intervertebral discitis, etc, which was successfully treated with antibiotics (TMP/SMX, levofloxacin, etc.) despite their major side effects (). Our patient had no recent history of hospitalization or previous history of S. maltophilia infection. During the Spring Festival, she visited her rural hometown for more than half a month where the environment was poor, which may be the main source of infection in this child. The child developed severe pneumonia after bacterial infection, which was mainly distributed in the right side of the lung, in accordance with the characteristics of S. maltophilia infection and the findings of Kang et al of bacteria causing pneumonia in patients with normal immunity. Parenchymal abnormalities were more predominately distributed in lower lung zone in immunocompetent patients, and diffusely distributed in immunocompromised patients.Citation10 Arthur et al showed that the incidence of S. maltophilia infection in children in the Intensive Care Unit (ICU) was 0.8–20.3%.Citation11,Citation12 The prevalence of S. maltophilia infection in the general population was about 1.3–1.68% during 2007–2012.Citation13 However, the number of reported cases of community infection in children is very small. Most patients with S. maltophilia infections are immunocompromised and have some comorbidity (eg, COPD, trauma, central venous catheter, prior antibiotic use, malignancy, prior hospitalization, HIV infection, or other immune suppression).Citation4 Among the seven children previously reported, only two patientsCitation7 had an indwelling catheter, and the other children had no associated comorbidities. Our reported case had no previous history of any related disease, so bacterium can also infect immunocompetent children in the community. Chang et al found that S. maltophilia is resistant to most antibiotics (β-lactam antibiotics, cephalosporins, macrolides, aminoglycosides, and carbapenems).Citation13 The mechanisms of its resistance to antibiotics include β-lactamase production, the expression of Qnr genes, and the presence of class 1 integrons and efflux pump.Citation13 The rate of resistance to other historically sensitive drugs (such as ceftazidime, ticacillin-clavulanate and urquinolones) has gradually increased. The current preferred drug is TMP/SMX, but its resistance rateCitation14 has also increased, with frequent adverse effects such as anaphylaxis, renal impairment and myelosuppression.Citation15 Hence, TMP/SMX should be administered with caution to pediatric cases. In the cases we reported, although the two drugs, meropenem and cefixime, were the intermediary of drug susceptibility prompts, the drug was not changed due to the small range of drug options for infants, and the clinical symptoms of the children improved when the drug susceptibility results came out. This is inconsistent with previous reports of innate resistance to carbapenems by S. maltophilia. It may be related to the fact that the bacteria in this article are different from community-acquired sources. More research on this bacteria is needed in the future to understand the this characteristic of bacteria. Hence, doctors can use Carbapenems antibiotics in children with normal immunity who develop a community-acquired infection with the bacterium. If the patient is stable and recovers well, then drugs with fewer side effects (such as ceftazidime) can be selected.
Table 1 Clinical Data of Patients with Stenotrophomonas maltophilia
In summary, although community-acquired S. maltophilia infection in children is rare, it can occur. The doctor encountered such a child in clinical work. This child has a normal immune system, his disease comes from a community infection and has lobar pneumonia located in the lower lung area. At the same time, the child’s white blood cells and CRP values are high, the doctor should be concerned that the child may have S. maltophilia infection. When treating patients, doctors can try to use drugs empirically, such as ceftazidime, instead of using ciprofloxacin, SMZ and other drugs that have relatively large side effects in children. It is worth mentioning that doctors also need to adjust the medication in a timely manner according to the efficacy evaluation and drug sensitivity of the children after the medication, so as to minimize the drug resistance of community-acquired infections. This will prevent the misuse of Meropenem, which has been given in a community patient and that too in a child. Its important to prevent this malpractise.
Abbreviations
TMP/SMX, trimethoprim/sulfamethoxazole; IV, intravenous injection; CRP, C-reactive protein; MDROS, multiple-drug-resistant organisms; WHO, The World Health Organization; ICU, the Intensive Care Unit.
Ethics Approval
Ethical approval for the study was granted by ShaoXing KeQiao Women And Children’s Hospital.
Consent for Publication
Written informed consent was obtained from the patient’s parents for publication of this case report and any accompanying images. A copy of the written consent is available for review.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
Acknowledgments
This study was partially supported by the Department of Pulmonology, The Children’s Hospital, Zhejiang University School of Medicine.
Additional information
Funding
References
- An SQ, Berg G. Stenotrophomonas maltophilia. Trends Microbiol. 2018;26(7):637–638. doi:10.1016/j.tim.2018.04.006
- Govender R, Amoah ID, Kumari S, et al. Detection of multidrug resistant environmental isolates of acinetobacter and Stenotrophomonas maltophilia: a possible threat for community acquired infections? J Environ Sci Health A. 2021;56:213–225. doi:10.1080/10934529.2020.1865747
- Looney WJ, Narita M, Mühlemann K. Stenotrophomonas maltophilia: an emerging opportunist human pathogen. Lancet Infect Dis. 2009;9:312–323. doi:10.1016/S1473-3099(09)70083-0
- Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev. 2012;25:2–41. doi:10.1128/CMR.00019-11
- Rello J, Kalwaje Eshwara V, Lagunes L, et al. A global priority list of the TOp Ten resistant Microorganisms (TOTEM) study at intensive care: a prioritization exercise based on multi-criteria decision analysis. Eur J Clin Microbiol Infect Dis. 2019;38:319–323. doi:10.1007/s10096-018-3428-y
- Shah A, Singhal T. Stenotrophomonas maltophilia as a Cause of Meningitis in an Infant. Indian J Pediatr. 2021;88:726. doi:10.1007/s12098-021-03800-x
- Büyükcam A, Bıçakcıgil A, Cengiz AB, et al. Stenotrophomonas maltophilia bacteremia in children - A 10-year analysis. Arch Argent Pediatr. 2020;118:e317–e323. doi:10.5546/aap.2020.eng.e317
- Wang G, Xu N, Yang L, et al. Community acquired Stenotrophomonas maltophilia discitis: diagnosis aided by shotgun metagenomic sequencing. Int J Infect Dis. 2019;81:1–3. doi:10.1016/j.ijid.2019.01.032
- Tokatly Latzer I, Paret G, Rubinstein M, et al. Management of Stenotrophomonas maltophilia Infections in Critically Ill Children. Pediatr Infect Dis J. 2018;37:981–986. doi:10.1097/INF.0000000000001959
- Kang YR, Cha YK, Kim JS, et al. Imaging findings of Stenotrophomonas maltophilia pneumonia: emphasis on CT findings between immunocompromised and immunocompetent patients. Acta Radiol. 2020;61:903–909. doi:10.1177/0284185119885117
- Arthur C, Tang X, Romero JR, et al. Stenotrophomonas maltophilia infection among young children in a cardiac intensive care unit: a single institution experience. Pediatr Cardiol. 2015;36:509–515. doi:10.1007/s00246-014-1041-0
- Ning BT, Zhang CM, Liu T, et al. Pathogenic analysis of sputum from ventilator- associated pneumonia in a pediatric intensive care unit. Exp Ther Med. 2013;5:367–371. doi:10.3892/etm.2012.757
- Chang YT, Lin CY, Chen YH, et al. Update on infections caused by Stenotrophomonas maltophilia with particular attention to resistance mechanisms and therapeutic options. Front Microbiol. 2015;6:893. doi:10.3389/fmicb.2015.00893
- Hu LF, Xu XH, Li HR, et al. Surveillance of antimicrobial susceptibility patterns among Stenotrophomonas maltophilia isolated in China during the 10-year period of 2005–2014. J Chemother. 2018;30:25–30. doi:10.1080/1120009X.2017.1378834
- Ho JM, Juurlink DN. Considerations when prescribing trimethoprim-sulfamethoxazole. CMAJ. 2011;183:1851–1858. doi:10.1503/cmaj.111152