Abstract
Healthcare workers (HCWs) are highly at risk for tuberculosis (TB) exposure, particularly those in high TB burden countries. Inoculation TB secondary to needlestick injury is uncommon but can occur in HCWs. Herein, we report an unusual case of primary multidrug‐resistant tuberculosis (MDR-TB) in a surgeon secondary to a needlestick injury while performing thoracentesis on a TB patient, and the surgeon recovered and returned to work after 22 months of anti-TB treatment. We searched the PubMed database and identified 19 cases of inoculation TB secondary to sharp injury in HCWs including the present case. Those cases highlight that primary inoculation of TB even MDR-TB infection should not be neglected in patients suffered needlestick injury when the sharp instrument suspected or confirmed contaminated with TB. In this situation, if the HCWs need for additional protection or prophylactic anti-TB is worthy of further study.
Introduction
China is one of 30 high TB burden countries for both tuberculosis (TB) and multidrug‐resistant tuberculosis (MDR-TB).Citation1 HCWs have a high risk of contracting Mycobacterium tuberculosis (Mtb) infection, and a previous study revealed that HCWs have higher rates of latent and active TB than the general population in China.Citation2,Citation3 Hence, the TB epidemic in HCWs is an important public health problem in China. Inoculation TB secondary to needlestick injury is uncommon but can occur in HCWs and could not be neglected.
We present the following case as a warning and to suggest an effective approach for proper management. A 35-year-old male surgeon presented with a right thumb skin lesion after accidentally pricking his right thumb while performing thoracentesis. Thereafter, the surgeon had soft-tissue and tenosynovial TB in the right thumb, right axillary lymphadenopathies, and tuberculous pleurisy. Susceptibility of the skin lesion culture was demonstrated against isoniazid and rifampicin. After 22-month anti-MDR-TB treatment, he returned to work afterward and regained normal thumb function.
Case Presentation
A 35-year-old male previously healthy surgeon sustained a needlestick injury while performing thoracentesis on a patient with smear-positive pulmonary tuberculosis (PTB) and was suspected of tuberculous pleurisy on November 9, 2012. The source patient was admitted to the local hospital because of respiratory failure, because his sputum detected acid-fast bacilli quickly, PTB was considered and was treated with isoniazid, rifampicin, ethambutol, and pyrazinamide. But his condition deteriorated rapidly and had acute hemopneumothorax. The surgeon in our study gave him an emergency chest puncture and drainage, and he collected the pleural effusion for tuberculosis culture. But he unfortunately sustained a needlestick injury while performing thoracentesis. He immediately disinfected the wound with povidone–iodine and washed it with water and soap. The source patient died the next day because of respiratory failure, it was less than a week before he was admitted to the hospital. Mtb were found in the source patient’s hydrothorax culture; however, a susceptibility test was not performed. The surgeon had no history of TB infection or any other health problems. He was vaccinated with Bacillus Calmette–Guérin during childhood. The injury healed normally; however, after 3 weeks, redness, edema erythematous papule, and pain in his thumb at the previously injured site occurred, and then, the papule enlarged and subsequently resulted in abscess formation, which was drained using a needle, Ziehl–Neelsen stain, detecting acid-fast bacilli (AFB). The diagnosis of primary inoculation cutaneous TB was made based on the positive result of Ziehl–Neelsen staining and the source patient’s hydrothorax culture. Then, he was treated with isoniazid, rifampicin, ethambutol, and pyrazinamide. After 10 days of treatment, the patient had a mild fever with chest tightness and noted multiple enlarged lymph nodes (LN) in his right axillary region. Then, he was transferred to our hospital.
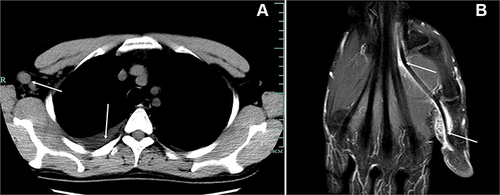
Physical examination revealed an indurated erythematous plaque at the middle of the thumb, a few clear liquids can be observed when pressed (), and tender multiple right axillary LN. Mild movement limitation of the affected finger’s mobility was caused by the presence of a lesion. Laboratory testing revealed an elevated C-reactive protein level and a white blood cell count of 21.6 mg/L and 8800 cells/μL, respectively, with 76.7% neutrophils. Human immunodeficiency virus (HIV) types 1/2 and hepatitis viral panels were negative. A chest computed tomography (CT) scan showed multiple enlarged LN in the right axilla and right pleural effusion (white arrows) (). Magnetic resonance imaging (MRI) of the right hand (conducted 50 days after the needlestick) showed tenosynovitis involvement of the entire flexor tendon of the thumb (). The patient underwent thoracic puncture and drainage in our hospital, the pleural effusion was exudative, and the pleural fluid protein was 37.83 g/L. However, acid-fast staining of the pleural fluid was negative, and the general bacterial culture and TB culture were negative.
Figure 1 (A) Physical examination reveals an indurated erythematous plaque on the middle of the right thumb, and a few clear liquids can be observed when pressed. (B) The skin lesion is healed after an anti-tuberculous therapy.
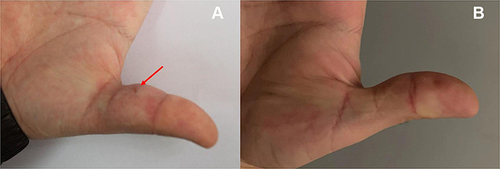
Figure 2 (A)CT scan of the chest shows multiple enlarged lymph nodes in the right axilla and right pleural effusion (white arrows). (B) MRI of the right hand shows an abnormal signal on the palmar side of the first proximal phalangeal bone of the right hand. T2W1 shows high signal intensity. The lesion extends along the tendon sheath of the flexor tendon into the carpal canal.
The puncture fluid from the skin lesion was cultured, and Mtb was observed thereafter. Susceptibility was demonstrated against isoniazid and rifampicin. Therefore, the regimen was changed to moxifloxacin (400 mg daily), amikacin (400 mg daily), pyrazinamide (1500 mg daily), prothionamide (600 mg daily), and aminosalicylate (10 g, daily). However, amikacin was discontinued at 5.5 months because the patient complained of tinnitus and aural fullness, then the remaining drugs were continuously administered for 16 months without any other adverse effects. After 4 weeks of treatment, the finger lesion had disappeared (). Axillary adenopathy disappeared approximately 6 months post-treatment. The surgeon completed recovery by the end of the 22-month course of anti-MDR-TB therapy and returned to work afterward and gained normal thumb functions. The patient was maintained in the 8-year follow-up without any relapse.
Discussion
TB is a known public health problem worldwide, is one of the most important occupational exposure diseases, and is mostly transmitted through inhalation of droplets or dust that contain bacteria from infected patients or materials. Inoculation, another mode of transmission, results from direct inoculation of Mtb into the skin, which can cause cutaneous TB. Primary cutaneous TB infection has been reported through contact routes, such as ear piercing, tattooing, intramuscular injection, acupuncture, and sharp instrument injury.Citation4–7 For example, acupuncture-induced primary inoculation TB has been reported in Korea and China.Citation6,Citation8 Because of the particularity of the work of HCWs, this population is a high-risk group for sharp instrument injury; thus, they are also more likely to suffer direct inoculation of TB. However, the risk of primary inoculation TB in HCWs following a needlestick injury is seldom discussed.
We searched the PubMed database for reports of inoculation TB secondary to a sharp instrument injury in HCWs published as of June 2022 and found cases in English-language articles or abstracts that included clinical details. A total of 19 cases of inoculation TB secondary to sharp injury in HCWs since 1974 were identified,Citation9–25 including the present case (). The mean age was 35.5 (range, 18–55) years, predominantly consisting of 63.2% males (12/19) and 36.8% (7/19) females. Clinicians were more frequently affected (57.9%, 11/19) than other HCWs (laboratory technicians, pathologists, students, and nurses). Six clinicians were injured by sharp instruments during operations involving the lungs and pleura, two cases while performing needle biopsy of neck LN, one by lumber puncture, one while draining the abscess, and one while collecting the lumbar material. The primary lesion sites include fingers (15), palm (2), opisthenar (1), and forearm (1). Left hands (73.7%, 14/19) were the most vulnerable part, as the instrument was generally held with their right hand.
Table 1 Clinical Characteristics of Inoculation TB Secondary to Needlestick Injury in HCWs
Skin lesions of approximately 5–10 mm in diameter usually develop at the site of inoculation within 1–6 weeks post-injury. The pain is slight or not obvious and may be followed by nonhealing ulcers, which may also present as abscesses, papules, verrucous nodules, and chronic ulcers. Involvement of the regional LN takes place approximately 6–8 weeks post-injury. Nine patients (47.4%, 9/19) developed regional LN enlargement, seven developed ipsilateral axillary lymphadenopathies after 3–6 weeks, and one developed epitrocheal adenopathy. However, the skin lesion spontaneously disappeared post-injury in one case, until 8 months later, the patient became aware of lymphadenopathy in the ipsilateral supraclavicular region. In addition to the primary skin lesion and regional LNs, one case had osteomyelitis, four including our case had tenosynovitis, and only one had pleurisy.
A high index of suspicion is required to make the diagnosis of cutaneous TB at any persistent nonhealing wound or ulcer after an accident or sharp injury, especially when the source patient was proven or suspected of TB infection. Histological and bacteriological examinations are necessary for the diagnosis. Histopathological manifestations of the skin lesion or LN including granulomatous with Langerhans giant cells and caseous necrosis with AFB in necrotic areas support the diagnosis of TB infection. Culture and molecular diagnostic evidence might establish a definite TB diagnosis. Among the 19 patients, 11 had positive results of Mtb culture, and a susceptibility test was performed in all cultures.
Fortunately, all patients, including the present case, recovered with anti-tuberculous therapy (ATT). Ten patients received the surgical adjuvant intervention, nine underwent excision biopsy or surgical debridement of the skin lesion, and one case of tenosynovitis underwent synovectomy besides ATT. Before the present case report, only one report of a laboratory technician who punctured her thumb with a needle containing drug-resistant tuberculous organisms while performing guinea pig inoculation.Citation9 However, to our knowledge, this is the first reported case of inoculation MDR-TB from a patient transmitted to a surgeon by occupational exposure to needlestick injuries, and the patient recovered and returned to work after 22 months of anti-TB treatment. MDR‐TB and rifampicin‐resistant tuberculosis (RR‐TB) are serious problems for global TB control. China is one of the countries with a high MDR‐TB and RR‐TB burden.Citation1 According to the World Health Organization report, in 2019, drug-resistant TB accounted for 14% of global drug-resistant TB cases in China, and 7.1% of the new TB cases and 23.0% of the retreated cases in China were MDR/RR-TB, both exceeding the global average (3.3% and 17.7%, respectively) during the same period.Citation1 The course of ATT in patients with MDR⁃TB is about ≥20 months; however, the treatment effect is not ideal, and the success of treatment and fatality rates are only 54% and 16%, respectively.Citation26 Studies have found that the drug-resistance rate of extrapulmonary TB in China is higher than that of PTB, and the MDR-TB rate of pleural TB is as high as 35.7%.Citation27
As one of the 30 countries with the highest TB burden worldwide, China’s occupational exposure to TB among medical workers is not optimistic, and the infection rate of TB is significantly higher than that of European and American countries and the general population in China.Citation2 With the advent of the HIV epidemic, and the increasing number of MDR-TB cases worldwide and in China, various invasive procedures are unavoidable in treating patients with TB. This case reminds medical staff of the need for additional protection when performing invasive procedures, such as pleural puncture, pleural biopsy, and LN biopsy on patients with suspected or confirmed TB, such as using a puncture needle with a safety device. Furthermore, taking correct preventive and remedial measures after occupational exposure is an effective way to ensure the occupational safety of medical staff. However, no corresponding research has been conducted on how to take correct remedial measures and whether to use preventive drugs for sharp instrument injuries contaminated by Mtb, which is worthy of further discussion. All published cases did not receive prophylactic ATT including the present case. Prophylactic ATT (eg, isoniazid for 6 months) has been recommended after sharp instrument injury with suspected Mtb contamination.Citation15,Citation18,Citation22 We also suggest that the acupuncture prevention process should consider the possibility of TB infection and initiate isoniazid prophylactic treatment when the source of infection is known or suspected TB infection. However, no recognized strategy has been established to prevent TB transmission after a sharp instrument injury exposure, which is worthy of further study.
The needlestick can also serve as a potential mode of transmission of HIV infection, especially in this era of co-existence of TB and HIV infections. Given the increased incidence of MDR-TB and the use of invasive operations to diagnose and treat patients with TB, this report highlights the need for special precautions during invasive manipulation in patients with TB.
Ethics Approval and Informed Consent
Written informed consent to have the case details and any accompanying images published has been provided by the patient. This report was approved by the Ethical Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors would like to thank the patient for his cooperation and for consenting to publication.
Additional information
Funding
References
- World Health Organization. Global Tuberculosis Report 2020. World Health Organization; 2020.
- Wang XN, He TL, Geng MJ, et al. Prevalence of and risk factors for tuberculosis among healthcare workers in Chinese tuberculosis facilities. Infect Dis Poverty. 2018;7:26. doi:10.1186/s40249-018-0407-6
- Guo HY, Zhong QH, Zhou J, et al. Risk of prevalence of latent tuberculosis infection in health care workers-an idiographic meta-analysis from a Chinese perspective. J Thorac Dis. 2021;13:2378–2392. doi:10.21037/jtd-20-1612
- Wong HW, Tay YK, Sim CS. Papular eruption on a tattoo: a case of primary inoculation tuberculosis. Australas J Dermatol. 2005;46:84–87. doi:10.1111/j.1440-0960.2005.00147.x
- Branagan P, Moran B, Fitzgibbon M, et al. Inoculation site leprosy in a tattoo as a paradoxical reaction following tuberculosis treatment. Int J Tuberc Lung Dis. 2016;20:706–708. doi:10.5588/ijtld.15.0236
- Kim JK, Kim TY, Kim DH, et al. Three cases of primary inoculation tuberculosis as a result of illegal acupuncture. Ann Dermatol. 2010;22:341–345. doi:10.5021/ad.2010.22.3.341
- Liu Y, Pan J, Jin K, et al. Analysis of 30 patients with acupuncture-induced primary inoculation tuberculosis. PLoS One. 2014;9:e100377. doi:10.1371/journal.pone.0100377
- Wang J, Zhu MY, Li C, et al. Outbreak of primary inoculation tuberculosis in an acupuncture clinic in southeastern China. Epidemiol Infect. 2015;143:943–948. doi:10.1017/S0950268814002039
- Sahn SA, Pierson DJ. Primary cutaneous inoculation drug-resistant tuberculosis. Am J Med. 1974;57:676–678. doi:10.1016/0002-9343(74)90023-0
- Hooker RP, Eberts TJ, Strickland JA. Primary inoculation tuberculosis. J Hand Surg Am. 1979;4(3):270–273. doi:10.1016/S0363-5023(79)80162-8
- Sharma VK, Kumar B, Radotra BD, et al. Cutaneous inoculation tuberculosis in laboratory personnel. Int J Dermatol. 1990;29:293–294. doi:10.1111/j.1365-4362.1990.tb02566.x
- Kramer F, Sasse SA, Simms JC, et al. Primary cutaneous tuberculosis after a needlestick injury from a patient with AIDS and undiagnosed tuberculosis. Ann Intern Med. 1993;119:594–595. doi:10.7326/0003-4819-119-7_Part_1-199310010-00007
- Genne D, Siegrist HH. Tuberculosis of the thumb following a needlestick injury. Clin Infect Dis. 1998;26(1):210–211. doi:10.1086/517023
- Fnini S, Ouarab M, Rafai M, et al. An uncommon occupational accident: tuberculous tenosynovitis of the extensor tendons of the hand. Chir Main. 1999;18(4):309–312.
- Oymak SF, Gulmez I, Demir R, et al. Transmission of Mycobacterium tuberculosis by accidental needlestick. Respiration. 2000;67:696–697. doi:10.1159/000056304
- Chandramukhi A, Manjunath MV, Veenakumari HB, et al. Tuberculous skin ulcer following needle-prick injury in a health care professional. J Assoc Physicians India. 2005;53:825–826.
- Lipani F, Canta F, Carosella S, et al. Primary soft tissue and tenosynovial tuberculosis after needlestick injury in a surgeon. Infez Med. 2008;16:33–36.
- Tapias L, Tapias-Vargas LF, Tapias-Vargas L. Primary cutaneous inoculation tuberculosis in a healthcare worker as a result of a surgical accident. Int J Dermatol. 2008;47:833–835. doi:10.1111/j.1365-4632.2008.03656.x
- Delli Carri R, Piscozzi P, Massimelli M, et al. A rare case of tubercular tenosynovitis in hospital surgeon as a result of an occupational accident caused by puncture with an infected needle. Prevention aspects and legal-medical evaluation. Med Lav. 2010;101:26–29.
- Harris SH, Khan R, Verma AK, et al. Finger ulceration in a healthcare professional. Ann Afr Med. 2010;9:45–47. doi:10.4103/1596-3519.62626
- Belchior I, Seabra B, Duarte R. Primary inoculation skin tuberculosis by accidental needle stick. BMJ Case Rep. 2011;2011:bcr1120103496. doi:10.1136/bcr.11.2010.3496
- Huang D, Yin H. Primary inoculation tuberculosis after an accidental scalpel injury. Infection. 2013;41:841–844. doi:10.1007/s15010-013-0442-y
- Karoney MJ, Kaumbuki EK, Koech MK, et al. Primary cutaneous tuberculosis in a 27-year-old medical intern from needle-stick injury: a case report. Clin Case Rep. 2015;3(1):39–42. doi:10.1002/ccr3.143
- Soto-Febres F, Ballena-Lopez J, Alva D, et al. Cutaneous inoculation tuberculosis in a healthcare worker: case report and literature review. IDCases. 2020;20:e00788. doi:10.1016/j.idcr.2020.e00788
- Malek AE, Fife CE, Rasmussen JC, et al. Lymphatic dissemination and axillary web syndrome in primary cutaneous tuberculosis secondary to needlestick injury. Open Forum Infect Dis. 2021;8:ofab160. doi:10.1093/ofid/ofab160
- World Health Organization. Global Tuberculosis Report 2018. World Health Organization; 2018.
- Pang Y, An J, Shu W, et al. Epidemiology of extrapulmonary tuberculosis among inpatients, China, 2008-2017. Emerg Infect Dis. 2019;25:457–464. doi:10.3201/eid2503.180572
