Abstract
With over 58 million cases and 6 million deaths by August 2022, the Coronavirus disease 2019 (COVID-19), causing severe acute respiratory syndrome coronavirus 2 (SARs-CoV-2), has had an insurmountable impact on the world’s population. This is one of the worst health crises since 1918’s influenza pandemic. There are four subvariants of Omicron; BA.1, BA.1.1, BA.2 and BA.3. As a result of new mutations in its spike protein, most of which occur in its receptor binding site, the Omicron variant appears to be more transmissible and less resistant to vaccination and antibody response. Understanding Omicron’s virology and mutations is essential to developing diagnostic and therapeutic methods. A thorough assessment of control measures, as well as timely adjustment of control measures, requires addressing such issues as re-infection risk, vaccine response, booster vaccine doses, and the increased rate of Omicron infections. This review article aims to look at the current information about the different types of SARs-CoV-2, focusing on the new subtype BA.2.75.
Introduction
SARS-CoV-2, which first emerged in the Chinese city of Wuhan, is infectious in humans and has spread quickly through intimate contact with other people or the release of respiratory secretions (ie, coughing or sneezing) from infected individuals. On March 12, 2020, the World Health Organization (WHO) Director-General proclaimed the COVID-19 outbreak “a pandemic” due to the rising infection rate in China.Citation1,Citation2 According to statistics, the enormous SARs-CoV-2 genome will produce single-point mutations daily due to the pandemic’s scope.Citation3 Thousands of distinct mutations have been identified, and roughly a year after the outbreak began, strains with several mutations, mainly in the spike (S) gene, started to appear.Citation4 These are the main variants of concern (VOCs).Citation5 As a result, multiple waves occurred: The first wave (Alpha), the second wave (Delta), and the third wave (Omicron). Although Beta and Gamma caused regional outbreaks in southern Africa and South America, they did not spread globally.Citation6 In November 2021, the Omicron variant was discovered in Botswana. It was reported from South Africa on November 24, 2021, and on November 26, 2021, it was classified as a VOC.Citation7
Since the beginning of SARS-CoV-2, more than 2.2 million virus sequences have been generated and shared in online databases like GISAID. These genome sequences enable researchers to track, analyze and detect possible mutational variants.Citation8
In addition to other proteins like NSP12 and NSP14 that are necessary for viral replication, Omicron contains a significant number of mutations that have previously been reported in other VOCs, including at least 32 mutations in the spike protein alone in contrast to the 16 mutations in the delta variant, which was already extremely contagious. The Omicron variant is more transmissible than other variants and the original SARS-COV-2. After that, Omicron sub-variants were identified in sequence. BA.1 was first discovered, followed by BA.2 sub-variant, then BA.4, and finally BA.5.Citation9 Close epidemiological monitoring of newly emerging variants and lineages is also advised in the event of an increase in severe disease outcomes, such as an increase in hospitalization or ICU admissions. Evaluation of the efficacy of vaccines and antibody-based therapies against these new variants is also required. Also, the design and development of next-generation vaccines which are more effective and newer monoclonal antibodies to halt the spread of the continuously evolving and emerging newer SARS-CoV-2 variants and lineages.Citation10
An increasing prevalence of BA.2.75 Omicron sub-variant in India and other countries like the UK, Canada, the US, Australia, and Japan might be behind the current COVID-19 surge. The (WHO) and experts have emphasized that countries should raise concerns about this new sub-variant because it has many spike mutations, manifests rapid growth, and has an extensive geographical distribution. In addition, BA.2.75 may have a crucial role in evading vaccine-induced immunity.Citation11–14
Each Omicron sub-variant has specific characteristics. This study aims to describe each sub-variant in terms of data and country of discovery, transmissibility, spike mutations of interest, hospitalization rate, effect of vaccination, most significant symptoms reported, and diagnosis. In addition, we will focus on the new BA.2.75 sub-variant.
Epidemiology
Covid-19 so Far
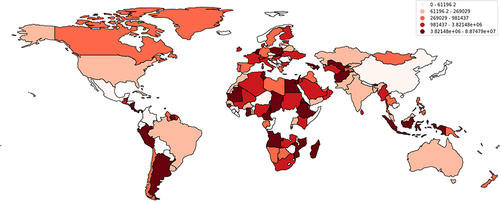
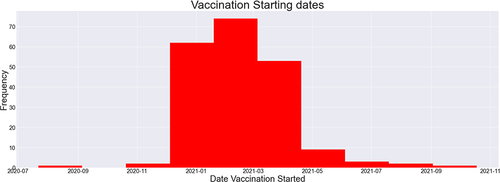
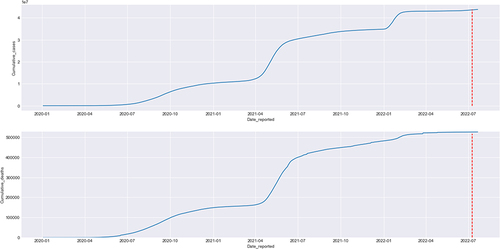
According to data reported by the WHO, a cumulative total of 88,747,875 cases have been reported in the USA alone, with a cumulative total of 1,015,093 deaths in the past years (). Multiple measures have been monitored by the WHO, including mask policies, travelling restrictions, social distancing, and, most importantly, vaccinations. Vaccinations started in July 2020 in China and have been made available worldwide since then ().Citation2,Citation15
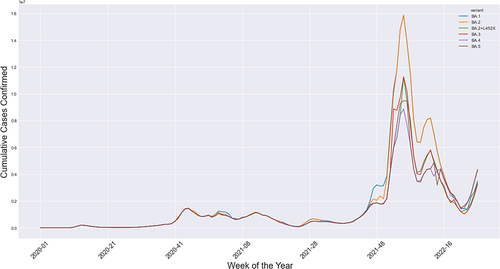
Omicron Sub-Variants
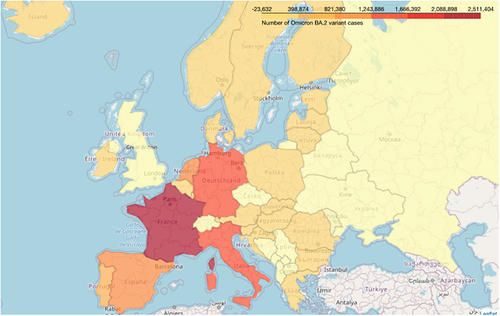
Omicron’s four sub-lineages are considered variants of concern: BA.1, BA.2, BA.4, and BA.5. BA.2.75 is the new emerging variant. In the United States, the dominant omicron sub-variant is BA.2.12.1; in South Africa, the dominant is BA.4 and BA. 5.Citation8 The Omicron sub-lineages (BA.1, BA.2, and BA.3) nearly appeared at the same time and location. However, BA.1 was dominant in infectivity and spread, ousting the Delta variant in late 2021. The BA.2 variant replaced it in March 2022 and peaked in April 2022. BA.3 was the least lineage in both infectivity and spread due to having no unique mutations in its spike proteins compared with BA.1 and BA.2 lineagesCitation16,Citation17 ().
Figure 5 The cumulative number of cases confirmed in Europe as reported by ECDC from January 2020 up to July 2022.
Immune Reaction of Omicron Sub-Variant
The Omicron variant is distinguished by 26–32 spike protein mutations, many of which are found within the receptor binding region. In addition, Omicron possesses mutations beyond the spike protein, three deletions, and one insertion in the spike protein.Citation18 Work on previous VOC has shown that such variants may be substantially different antigenically, and many of the changes are either known or projected to contribute to the escape from neutralizing antibodies.Citation19 A preprint paper found increased immune escape of the Omicron variant.Citation20
The risk of reinfection by the Omicron sub-variants is considered a question of great importance. It depends on the ability of the new sub-variants to escape the immune system. According to laboratory research, the convalescent serum seems to have a diminished neutralizing effect on the Beta and Delta variants of the virus in vitro compared to the wild-type virus.Citation18 However, this does not necessarily translate into immunological escape at the population level.Citation19,Citation21,Citation22
Clinical Presentation and Severity
The severity of the Omicron variant seems to be less than the delta variant, even though they have similar clinical manifestations.Citation23 According to preliminary evidence, Omicron may produce relatively mild sickness, with some patients developing severe illness, requiring hospitalization, and dying due to the infection caused by this variant.Citation7,Citation23 The hospitalization rate increased with all Omicron sub-variants.Citation24 Although there was little increase in hospitalization and death rates in South Africa, outside of it, there was a significant increase in both.Citation25 The most frequent complaints of patients are fever, cough, exhaustion, and loss of taste and/or smell. Other symptoms include pharyngitis, headaches, skin rashes, discolored fingers and toes, red or itchy eyes, stomach cramps, and diarrhea are frequently seen with Omicron. It may also result in serious symptoms like dizziness, shortness of breath, chest discomfort, difficulty moving, and difficulty breathing. Respiratory symptoms include cough, scratchy throat, shortness of breath, and pneumonia may also be seen.Citation26
Country and Date of Detection
BA.2.75
The new omicron sub-variant BA.2.75 was first detected in early June in India and identified as a variant of concern by the WHO on July 7, 2022,Citation27 At least 23 samples of the BA.2.75 variant in India have been recorded in Karnataka, Maharashtra, and Jammu & Kashmir. About 37 samples have been detected in Australia, Canada, Germany, and New Zealand.Citation28 There are two cases of BA.2.75 in the United States, the first of which was identified on June 14, but both have not been officially confirmed.Citation29 It has then spread to more than ten countries, including the UK and Japan.Citation30
BA.1
According to the Phylogenetic tree analysis, Omicron independently evolved from the previous SARS Cov-2 variants as Alpha, Beta, Gamma, and Delta.Citation31 Although the Omicron variant was initially reported in November 2021 in South Africa, the first confirmed case was in the Netherlands.Citation32,Citation33 BA1.1 emerged in late 2021 and rapidly became predominant in early 2022.Citation34
BA.2
BA.2 has been detected in at least 67 countries, and the most dominant variant is in the Philippines, India, and Denmark.Citation35
BA.4 and BA.5 variants accounted for more than 50% of sequenced cases in South AfricaCitation36 ().
Table 1 Summarize the Characteristics of Each Omicron Sub-Variant
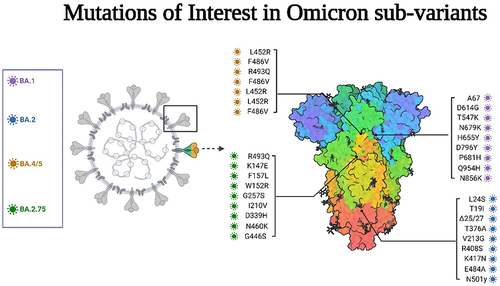
Mutations of Interest and Sequencing of Omicron Sub-Variants
BA.2.75
The scientific director of WHO, Soumya Swaminathan, published a video about this sub-variant saying, “There are still limited sequences available to analyze, but this sub-variant seems to have a few mutations on the receptor binding domain of the spike protein”.Citation37
This sub-variant shows a high number of mutations in genome sequences, mainly in the spike proteins of the virus with a high weakly growth with possible mutations at S: K147E, S: F157L, S: W152R, S: G257S, S.I210V, S: D339H, S: N460K, S: G446S and S: R493Q. The most concerning are G446S and R493Q. The G446S mutation can potentially affect immune evasion and ACE2 binding. Given the available evidence, it is possible that, although this mutation may reduce the binding effect of the sub-variant, it may also lead to considerable immunological escape. This suggests that reinfections and breakthrough infections may be driving the spread of BA.2.75. This may explain the increasing number of cases in India.Citation38,Citation39 BA.2.75 has been dominant in many regions worldwide lately, acquiring more rise in its alpha helices’ number than BA.2, which enables it to escape immunity.Citation40,Citation41
Another hypothesis is that a unique characteristic is acquired from APOBEC-induced mutations, which lead to the loss of 2 CPG dinucleotides, and the gain of 4 new ones in the Omicron BA.2 variant, thus escaping the zinc finger antiviral protein in lung cells.Citation42 Another finding is that there is a high expression of transmembrane serine protease 2, which is generally involved in regulating cellular signaling in the plasma membrane and extracellular matrix. These molecules were found to be dominant in various cancers.Citation43
According to the available online data in genome trackers platforms, the number of mutations in the BA.2.75 spike protein is more than those in the BA.4/5, making it highly contagious and resistant to neutralization compared with other omicron variants.Citation27,Citation29 However, researchers are still tracking its possible mutations.
BA.1
The classical Omicron variant (B.1.1.529) constitutes 18,261 mutations in its genome (), most of them in the coding region, 97% of the total mutations, and most of these mutational events, 60%, are skewed towards the spike proteins as A67, D614G, T547K, N679K, H655Y, D796Y, P681H, Q954H, and N856K and others.Citation31,Citation33 In addition, BA.1.1 is different from BA.1 in the presence of a single mutation (R346K).Citation27
BA.2
BA.2 sub-lineage genome consists of substitutions and deletions in the Receptor binding site, S2 region, and furin cleavage domain.Citation35 It is characterized by the key S mutations L24S, T19I, Δ25/27, T376A, V213G, and R408S.Citation44 In addition, BA 2 variant exhibits 15 mutations in the receptor binding domain, which includes the mutations in K417N, E484A, and N501y, facilitating its escape from neutralizing antibodies, enhanced by the formation of new salt bridges and hydrogen bonds produced by R49, R498, which are mutated residues in the receptor binding protein with ACE2. This change was triggered by increased alpha helices in the RBP, increasing its susceptibility to several mutations.Citation43
BA.4 and BA.5
Spike mutations of interest are L452R, F486V, and R493Q. The S-proteins of the Omicron variants BA.4 and BA.5 are identical to the variant BA.2 except for 69–70 deletion, F486V, and L452R.Citation17,Citation36 BA.4 and BA.5 each have unique alterations, including L452R and F486V in the viral spike protein, which may affect the virus’s capacity to attach to host cells and evade various immune responses.Citation45 As a result of the high similarity between BA.2 and BA4/5, it was found that many genome sequences classified as BA.2 in public databases are BA.4 or BA.5, thus underestimating the variants’ ongoing global riseCitation25 ().
Transmissibility of the Omicron Sub-Variants (BA.2.75)
The mechanism of transmission of the BA.2.75 sub-variant is still unclear, and there is no evidence of any difference between it and the BA.2 sub-variant. However, the current reports may support the hypothesis that BA.2.75 spreads faster, as the curve of new cases in India has increased since the identification of the BA.2.75 sub-variant.Citation46 The daily cases in India have been less than 3000 for several months, but recently they began to increase and reached 18,000/day, which is 1/100K of the populationCitation38 ().
Clinical Characteristics and Severity of the Omicron Sub-Variants
It is early to say anything about the severity of the new sub-variant, but it seems to be as severe as the BA.2 variant with a higher transmissibility rate. Further investigations are crucially needed. The first cases of the BA.2.75 sub-variant were asymptomatic, and all recovered at home.Citation28,Citation47–49 Further studies are required to investigate the clinical picture and severity of the new sub-variant and compare it with previous variants ().
As a result of the insufficient data reported on the new B.A.2.75 Omicron sub-variant, the evidence of its infectivity, immunity evasion, and severity is still unclear. However, investigations are proceeding to understand the details regarding the BA.2.75 sub-variant to suggest the best effective methods to restrict the upcoming surge.Citation11,Citation49
BA.1 seems to cause a mild form of the disease. The most significant symptoms reported with BA.1 sub-variant are cold and flu-like symptoms with no significant symptoms reported. Infections were more likely to be asymptomatic.Citation50
BA.2 also causes mild illness but is more severe than BA.1. Symptoms with BA.2 subvariant are cough, fatigue, congestion, and runny nose.Citation51 In addition, the impact of BA.2 sub-variant on immunity increased.Citation9 A study by Chen et al 2022. Showed a very low prevalence of neutralizing antibodies against BA.2 sub-variant among the Hong Kong population.Citation52
BA.4 and BA.5 cause more severe disease than BA.1 and BA.2.Citation24 The most reported symptoms with BA.4 and BA.5 sub-variants were severe throat pain and increasing fatigue.Citation53
Clinical Diagnosis
The diagnosis of Omicron cases depends mainly on molecular and immunological testing. The molecular testing includes real-time PCR (RT-qPCR), Next generation sequencing, and rapid molecular detection by LAMP. RT-qPCR can identify Omicron but cannot differentiate between its sub-variants. It identifies Omicron by detecting mutations in the S gene. The focus of the RT-PCR diagnostic kits, which have been approved, is the E, Rd, Rp, and N genesCitation54 (Bazargan et al).
RT-PCR gives positive or negative results. Therefore, positive results may be recommended to undergo further DNA sequencing to identify the new mutation, which leads to variant identification.Citation26
Immunological testing includes testing for antigens or antibodies, but they are not confirmatory. Therefore, the sample is preferably taken from the upper respiratory tract or saliva. Antibodies measured are directed against S or N protein, ie, virus-specific antibodies.Citation26
So as a general approach to diagnosis, we depend on RT-qPCR, and according to the results, we classify patients into A) Suspected: absence of E484K and L452R mutations in the Spike protein.
B- Probable: detection of Spike protein substitutions K417N, S371L-S373P, and Q493R, or deletion at position 69/70; then to confirm the diagnosis, we perform whole genome sequencing (WGS)Citation55
Expected Response to BA.2.75
Previous recommendations to tackle the COVID‐19 pandemic must be sustained worldwide with recently improvised instructions. These include vaccinations for all individuals, social distancing, mask-wearing, and careful handwashing and quarantining of the BA.2.75 sub-variant positive patients in an alternative area. It is critical to highlight that genome sequencing of all samples could potentially impact the control of disease and evaluate the threat of new waves in the world.Citation11–13 Further surveillance is needed to prevent more dissemination of the BA.2.75 sub-variant.
Vaccination Against BA.2.75
Despite the spread of the new variant in India and other countries, it is early to predict if it is a dominant strain. Still, it shows a rapid growth rate of 16% per day other than BA.2 sub-variants found in most reported cases in India.Citation39,Citation56 Therefore, adding boosting protection against BA.2.75 to vaccines is important to avoid the spike of BA.2.75 and its spread.
Immunity Against BA.4 / BA.5
The COVID-19 vaccines have a mild effect on it, as there were seven folds drop in the neutralizing antibodies produced against both BA.4 and BA.5, compared to BA.1. Booster doses are recommended by the WHO to minimize the mortality and hospitalization rates.Citation60,Citation61
Omicron Variants and Susceptibility to Vaccine
The Existing vaccines targeting the first COVID variant detected in Wuhan, China, showed effectiveness in decreasing the severity of infection.Citation57 However, its effect diminishes over time and appears to be less effective in the new variants of Omicron declared by the Vaccines and Related Biological Products Advisory Committee (VRBPAC) meeting at the Food and Drug Administration (FDA) in late June 2022.Citation58 Therefore, all these issues encouraged the pharmaceutical companies to make Omicron-specific vaccines to face all sub-variants and their modifications. These vaccines will be administered as booster dosesCitation59,Citation60 In addition, vaccines have produced neutralizing antibodies against different omicron variants.Citation61
Omicron BA.1 sub-lineage is more reliable to neutralize antibodies generated from vaccine combination compared to other lineages such as BA.2.12.1 and BA.5, which are less susceptible to neutralization by 2.4 to 5.3 times.Citation61 A study by Tan et al has shown that the BNT16b2 Vaccine reduced infection and hospitalization from omicron subvariants B.1.1529 and B1.617.2 in Singapore with estimated effectiveness of 36.8% and 65.3%, respectively, among children from 5 to 11.Citation62
Currently, the most dominant strain in the US is BA.5, representing 65% of cases in the US from July 3–9. It is Hyper contiguous and five times more resistant to vaccines, especially mRNA vaccines, as Moderna and Pfizer.Citation63 Despite the lower efficacy of vaccines, it still provides protection compared to their absence. Non-vaccinated individuals are five times more likely to get BA5 sub lineage infection and 7.5 times higher to become hospitalized. However, BA.5 is becoming more prevalent over time, and the incidence of BA.1 and BA.2 strains is decreasing.Citation63 Moderna and Pfizer are now updating booster vaccines against BA4 and BA5, Moderna mRNA-123.214. A clinical trial showed that this bivalent vaccine would be effective against both BA4 and BA5, and it is expected to be administered by October.Citation58,Citation59 ECDC released a statement on Omicron sub-variants stating that ECDC has reclassified Omicron sub-lineages BA.4 and BA.5 from variants of interest to variants of concern. The currently observed growth advantage for BA.4 and BA.5 is likely due to their ability to evade immune protection induced by prior infection and/or vaccination, particularly if this has waned over timeCitation9().
Spread and Prevention
Expected Spread of Omicron
According to the CDC’s hospital forecast, daily COVID-19 hospital admissions are likely to increase by July 2022.Citation64 As a result, immunized patients, whether through vaccines or natural immunity, are at risk.
BA.2.75 will likely become a trend in the upcoming weeks. However, it is too early to conclude that this lineage spreads faster or will become the dominant one in the future.
Prevention of Omicron and Subvariants
Although Omicron is more transmissible than the previous variants, it spreads through the same mechanisms. This primarily happens when a person is exposed to the respiratory fluids carrying the virus, whether, through inhalation of respiratory droplets or their deposition on mucous membranesCitation50 In addition, the CDC continues to track the spread of Omicron and its sub-variants and advises the public on prevention methods.Citation65
The most effective way to stop the increasing number of cases is through vaccination. Vaccines have decreased hospitalization and mortality and are our first line of defense in this pandemic.Citation66 Up-to-date vaccination is achieved when an individual has received every dose in a primary series and the recommended boosters whenever eligible. The age, type of vaccine received, and time since the last dose determine further vaccine recommendations for the individual.Citation67,Citation68 In addition, mRNA-based vaccines have been shown to induce neutralizing immunity against Omicron and are highly recommended for their use as a booster dose.Citation69,Citation70
The CDC has also advised the public to wear a properly fitting mask to protect against the spread of COVID-19, including Omicron and other variants. The mask does not need to be worn outdoors but should be used when sick or are around or caring for someone with COVID. The recommendations also depend on the COVID-19 community level. The CDC has divided it into low, medium, and high. In low levels, a mask is worn based on personal preference and risk level. For those in a medium community level, it is advised to wear one if there is a risk for severe illness, based on what doctors recommend, and when coming in contact with someone at risk for severe disease. If the risk is high, masks should be worn indoors in public, regardless of vaccination and risk of hospitalization.Citation71
People with a high risk of severe illness from COVID-19 are advised to keep 6 feet from others outside or in public. Close contact with sick individuals should be avoided at home, especially when caring for a sick person. It is also crucial to avoid crowds and poorly ventilated areas while keeping homes well-ventilated by opening windows and doors. Handwashing with soap for a minimum of 20 seconds when in public spaces or after coughing or sneezing. A hand sanitizer with at least 60% alcohol concentration may be used as a substitute if soap and water are unavailable. Sneezes and coughs should be covered, and surfaces should be cleaned and disinfected frequently for maximal protection.Citation72
Testing for COVID-19 is recommended before and after travel, when coming in contact with an infected person, or if there are suspected symptoms, including fever, cough, fatigue, sore throat, nasal congestion, headache, or loss of taste/or smell.Citation73
Conclusion
The SARS-CoV-2 virus, which continues to evolve, is unlikely to disappear completely in the near future. COVID-19 is predicted to eventually be dominated by the Omicron variant, which causes milder symptoms than seasonal influenza. COVID-19 has been expected to become endemic due to the appearance of the Omicron subvariants, which cause mild symptoms despite being more contagious. Vaccination has been shown to reduce the risk of long-term COVID-19 infection. Therefore, vaccination advocacy is still necessary in order to protect individuals who are particularly susceptible.
Abbreviations
WHO, World Health Organization; VOC, variant of concern; VRBPAC, Vaccines and Related Biological Products Advisory Committee; FDA, the Food and Drug Administration.
Data Sharing Statement
All data generated during this study are included in this published article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr Mahmoud Tarek Hefnawy reports non-financial support from Zagazig University Faculty of Medicine, during the conduct of the study. The remaining authors declare no competing interests.
Acknowledgments
The Qatar National Library funded the publication of this article.
References
- WHO director-general’s opening remarks at the media briefing on COVID-19; 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19---11-march-2020. Accessed July 24, 2022.
- Mule S, Singh A, Greish K, Sahebkar A, Kesharwani P, Shukla R. Drug repurposing strategies and key challenges for COVID-19 management. J Drug Target. 2022;30(4):413–429. doi:10.1080/1061186X.2021.2013852
- Sender R, Bar-On YM, Gleizer S, et al. The total number and mass of SARS-CoV-2 virions. Proc Natl Acad Sci U S A. 2021;118(25). doi:10.1073/pnas.2024815118
- Khairnar P, Soni M, Handa M, Riadi Y, Kesharwani P, Shukla R. Recent highlights on Omicron as a new SARS-COVID-19 variant: evolution, genetic mutation, and future perspectives. J Drug Target. 2022;30(6):603–613. doi:10.1080/1061186X.2022.2056187
- Zhou B, Thao TTN, Hoffmann D, et al. SARS-CoV-2 spike D614G change enhances replication and transmission. Nature. 2021;592(7852):122–127. doi:10.1038/s41586-021-03361-1
- Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19). Available from: https://pubmed.ncbi.nlm.nih.gov/34033342/. Accessed July 24, 2022.
- Classification of Omicron (B.1.1.529): SARS-CoV-2 variant of concern. Available from: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern. Accessed July 24, 2022.
- O’Toole Á, Pybus OG, Abram ME, Kelly EJ, Rambaut A. Pango lineage designation and assignment using SARS-CoV-2 spike gene nucleotide sequences. BMC Genomics. 2022;23(1):1–13. doi:10.1186/s12864-022-08358-2
- SARS-CoV-2 variants of concern as of 15 July 2022. Available from: https://www.ecdc.europa.eu/en/covid-19/variants-concern. Accessed July 24, 2022.
- Malik JA, Ahmed S, Mir A, et al. The SARS-CoV-2 mutations versus vaccine effectiveness: new opportunities to new challenges. J Infect Public Health. 2022;15(2):228. doi:10.1016/j.jiph.2021.12.014
- CGTN. Could Omicron BA.2.75 sub-variant lead to a new global COVID-19 wave?; 2022. Available from: https://news.cgtn.com/news/2022-07-05/Could-Omicron-BA-2-75-sub-variant-lead-to-A-new-global-COVID-19-wave--1bqoo4JLfwI/index.html. Accessed October 10, 2022.
- World Health Organization. WHO coronavirus (COVID-19) dashboard. Available from: https://covid19.who.int/measures/. Accessed October 20, 2022.
- India Today. WHO monitoring new Omicron sub-variant BA.2.75 detected in countries like India; 2022. Available from: https://www.indiatoday.in/coronavirus-outbreak/story/who-monitoring-new-omicron-sub-variant-ba-2-75-detected-india-covid-cases-1972801-2022-07-07. Accessed October 20, 2022.
- WHO Coronavirus (COVID-19) Dashboard. WHO coronavirus (COVID-19) dashboard with vaccination data. Available from: https://covid19.who.int/. Accessed July 24, 2022.
- Ahmad Malik J, Ahmed S, Shinde M, et al. The impact of COVID-19 on comorbidities: a review of recent updates for combating it. Saudi J Biol Sci. 2022;29(5):3586–3599. doi:10.1016/j.sjbs.2022.02.006
- Desingu PA, Nagarajan K, Dhama K. Emergence of Omicron third lineage BA.3 and its importance. J Med Virol. 2022;94(5):1808. doi:10.1002/jmv.27601
- Mohapatra RK, Kandi V, Sarangi AK, et al. The recently emerged BA.4 and BA.5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic – correspondence. Int J Surg. 2022;103:106698. doi:10.1016/j.ijsu.2022.106698
- Farooqi T, Malik JA, Mulla AH, et al. An overview of SARS-COV-2 epidemiology, mutant variants, vaccines, and management strategies. J Infect Public Health. 2021;14(10):1299. doi:10.1016/j.jiph.2021.08.014
- Liu C, Ginn HM, Dejnirattisai W, et al. Reduced neutralization of SARS-CoV-2 B.1.617 by vaccine and convalescent serum. Cell. 2021;184(16):4220–4236.e13. doi:10.1016/j.cell.2021.06.020
- Pulliam JRC, Govender N, Gottberg A, et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of the Omicron variant in South Africa. medRxiv. 2021;376:eabn4947.
- Planas D, Veyer D, Baidaliuk A, et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021;596(7871):276–280. doi:10.1038/s41586-021-03777-9
- Cele S, Gazy I, Jackson L, et al. Escape of SARS-CoV-2 501Y.V2 from neutralization by convalescent plasma. Nature. 2021;593(7857):142–146. doi:10.1038/s41586-021-03471-w
- CDC. Omicron variant: what you need to know. Available from: https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html. Accessed July 24, 2022.
- Taylor CA, Whitaker M, Anglin O, et al. COVID-19–associated hospitalizations among adults during SARS-CoV-2 delta and omicron variant predominance, by race/ethnicity and vaccination status — COVID-NET, 14 states. MMWR Morb Mortal Wkly Rep. 2022;71(12):466–473. doi:10.15585/mmwr.mm7112e2
- Callaway E. What Omicron’s BA.4 and BA.5 variants mean for the pandemic. Nature. 2022;606(7916):848–849. doi:10.1038/d41586-022-01730-y
- Bazargan M, Elahi R, Esmaeilzadeh A. OMICRON: virology, immunopathogenesis, and laboratory diagnosis. J Gene Med. 2022;24(7). doi:10.1002/jgm.3435
- Yamasoba D, Kimura I, Kosugi Y, et al. Neutralization sensitivity of Omicron BA.2.75 to therapeutic monoclonal antibodies. bioRxiv. 2022;2022. doi:10.1101/2022.07.14.500041
- BA.2.75 — new Covid variant detected in India a mystery, but could ‘have immune-escape property. Available from: https://theprint.in/health/ba-2-75-new-covid-variant-detected-in-india-A-mystery-but-could-have-immune-escape-property/1020578/. Accessed July 23, 2022.
- CDC Fortune. “Centaurus”, new “stealth Omicron” COVID subvariant BA.2.75, found in the U.S. Available from: https://fortune.com/2022/07/07/what-is-centaurus-ba275-new-stealth-omicron-covid-subvariant-cdc/. Accessed July 23, 2022.
- Tableau Public. Tracking BA.2.75 lineage over time. Available from: https://public.tableau.com/app/profile/raj.rajnarayanan/viz/TrackingBA_2_75LineageOverTime/BA_2_75. Accessed July 24, 2022.
- Bansal K, Kumar S. Mutational cascade of SARS-CoV-2 leading to evolution and emergence of omicron variant. Virus Res. 2022;315:198765. doi:10.1016/j.virusres.2022.198765
- Yin W, Xu Y, Xu P, et al. Structures of the Omicron Spike trimer with ACE2 and an anti-Omicron antibody. Science. 2022;375(6584):1048–1053. doi:10.1126/science.abn8863
- Araf Y, Akter F, Zheng C, et al. Omicron variant of SARS‐CoV‐2: genomics, transmissibility, and responses to current COVID‐19 vaccines. J Med Virol. 2022;94(5):1825. doi:10.1002/jmv.27588
- Martins M, Do Nascimento GM, Nooruzzaman M, et al. The Omicron variant BA.1.1 presents a lower pathogenicity than B.1 D614G and Delta variants in a feline model of SARS-CoV-2 infection. bioRxiv. 2022. doi:10.1101/2022.06.15.496220
- Kawaoka Y, Uraki R, Kiso M, et al. Characterization and antiviral susceptibility of SARS-CoV-2 Omicron/BA.2. Res Sq. 2022. doi:10.21203/rs.3.rs-1375091/v1
- Tegally H, Moir M, Everatt J, et al. Emergence of SARS-CoV-2 Omicron lineages BA.4 and BA.5 in South Africa. Nat Med. 2022;28(9):1785–1790. doi:10.1038/s41591-022-01911-2
- Statement on Omicron sublineage BA.2. Available from: https://www.who.int/news/item/22-02-2022-statement-on-omicron-sublineage-ba.2. Accessed July 24, 2022.
- Worldometer. India COVID coronavirus statistics. Available from: https://www.worldometers.info/coronavirus/country/india/. Accessed July 24, 2022.
- Hachmann NP, Miller J, Ventura JD, et al. Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5. N Engl J Med. 2022;387(1):86–88. doi:10.1056/NEJMc2206576
- Kumar S, Karuppanan K, Subramaniam G. Omicron (BA.1) and sub-variants (BA.1.1, BA.2, and BA.3) of SARS-CoV-2 spike infectivity and pathogenicity: a comparative sequence and structural-based computational assessment. J Med Virol. 2022;94(10):4780–4791. doi:10.1002/jmv.27927
- Shaheen N, Mohamed A, Soliman Y, et al. Could the new BA.2.75 sub-variant lead to another COVID-19 wave in the world? – correspondence. Int J Surg. 2022;105:106861. doi:10.1016/j.ijsu.2022.106861
- Jung C, Kmiec D, Koepke L, et al. Omicron: what makes the latest SARS-CoV-2 variant of concern so concerning? J Virol. 2022;96(6). doi:10.1128/jvi.02077-21
- Guo Y, Han J, Zhang Y, et al. SARS-CoV-2 Omicron variant: epidemiological features, biological characteristics, and clinical significance. Front Immunol. 2022;13:2010.
- Evans JP, Zeng C, Qu P, et al. Neutralization of SARS-CoV-2 Omicron sub-lineages BA.1, BA.1.1, and BA.2. Cell Host Microbe. 2022;30(8):1093–1102.e3. doi:10.1016/j.chom.2022.04.014
- Tegally H, Moir M, Everatt J, et al. Continued Emergence and Evolution of Omicron in South Africa: new BA.4 and BA.5 lineages. medRxiv. 2022. doi:10.1101/2022.05.01.22274406
- The Wire Science. Could the new BA.2.75 sub-variant lead to another COVID-19 wave in India? Available from: https://science.thewire.in/the-sciences/ba-2-75-sub-variant-new-covid-19-wave/. Accessed July 24, 2022.
- What we know so far about Omicron’s BA.2.75 sub-variant, spreading 18% more. Available from: https://www.dnaindia.com/health/report-what-we-know-so-far-about-omicron-ba-2-75-sub-variant-spreading-18-percent-more-covid-19-delta-2966072. Accessed July 24, 2022.
- COVID-19: what is BA.2.75 sub-variant and how bad is it? Available from: https://www.freepressjournal.in/mumbai/covid-19-what-is-ba275-sub-variant-and-how-bad-is-it. Accessed July 24, 2022.
- Team TIE. New omicron sub-variant BA.2.75 sets alarm bells ringing; here’s all we know about its severity, transmissibility & more; 2022. Available from: https://weather.com/en-IN/india/coronavirus/news/2022-07-07-new-omicron-sub-variant-ba275-transmissibility-severity-faqs. Accessed October 20, 2022.
- Ars Technica. Sliding to mild? Nope—omicron BA.2 caused worse COVID symptoms than BA.1. Available from: https://arstechnica.com/science/2022/05/sliding-to-mild-nope-omicron-ba-2-caused-worse-covid-symptoms-than-ba-1/. Accessed July 24, 2022.
- NBC Chicago. What are the symptoms of the omicron subvariant BA.2? Here’s what experts say so far. Available from: https://www.nbcchicago.com/news/local/what-are-The-symptoms-of-The-omicron-subvariant-ba-2-heres-what-experts-say-so-far/2792800/. Accessed July 24, 2022.
- Chen LL, Abdullah SMU, Chan WM, et al. Contribution of low population immunity to the severe Omicron BA.2 outbreak in Hong Kong. Nat Commun. 2022;13(1):1–10. doi:10.1038/s41467-021-27699-2
- ABC7 San Francisco. COVID-19: doctors explain 5 reasons why omicron’s BA.5 will be the “worst” subvariant yet. Available from: https://abc7news.com/omicron-ba5-subvariant-transmissibility-latest-covid-variant-symptoms/12044541/. Accessed July 24, 2022.
- Tahmasebi S, Khosh E, Esmaeilzadeh A. The outlook for diagnostic purposes of the 2019‐novel coronavirus disease. J Cell Physiol. 2020;235(12):9211. doi:10.1002/jcp.29804
- Maisa A, Spaccaferri G, Fournier L, et al. First cases of Omicron in France are exhibiting mild symptoms. Infect Dis Now. 2022;52(3):160–164. doi:10.1016/j.idnow.2022.02.003
- Fortune. New Omicron subvariant BA 2.75, dubbed Centaurus, is being tracked by the WHO. It may be the most immune-evasive yet. Available from: https://fortune.com/2022/07/06/new-omicron-subvariant-centaurus-ba-2-75-world-health-organization-immune-evasive-expert/. Accessed July 25, 2022.
- Malik JA, Mulla AH, Farooqi T, Pottoo FH, Anwar S, Rengasamy KRR. Targets and strategies for vaccine development against SARS-CoV-2. Biomed Pharmacother. 2021;137:111254. doi:10.1016/j.biopha.2021.111254
- Scientific American. Omicron-Specific COVID Boosters Are Coming. Available from: https://www.scientificamerican.com/article/omicron-specific-covid-boosters-are-coming/. Accessed July 25, 2022.
- CBS News. COVID-19 vaccine for Omicron variant will be ready by August, Moderna CEO says. Available from: https://www.cbsnews.com/news/covid-vaccine-moderna-omicron-variant-booster-shot-august/. Accessed July 25, 2022.
- What to know about omicron-specific Covid vaccines arriving this fall. Available from: https://www.cnbc.com/2022/07/01/what-to-know-about-omicron-specific-covid-vaccines-arriving-this-fall.html. Accessed July 25, 2022.
- National Institutes of Health (NIH). Vaccine-Induced immune response to omicron wanes substantially over time. Available from: https://www.nih.gov/news-events/news-releases/vaccine-induced-immune-response-omicron-wanes-substantially-over-time. Accessed Jul 25, 2022.
- Tan SHX, Cook AR, Heng D, Ong B, Lye DC, Tan KB. Effectiveness of BNT162b2 vaccine against omicron in children 5 to 11 years of age. NEJM. 2022;387(6):525–532. doi:10.1056/NEJMoa2203209
- NPR. The omicron subvariant dominating U.S. COVID-19 cases is more vaccine-resistant. Available from: https://www.npr.org/2022/07/15/1111648759/covid-19-coronavirus-omicron-variant-ba5-cdc-vaccines-masks-mayo-clinic. Accessed July 25, 2022.
- CDC. COVID-19 Forecasts: hospitalizations. Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/forecasting/hospitalizations-forecasts.html. Accessed July 22, 2022.
- CDC. COVID Data Tracker: variant Proportions. Available from: https://covid.cdc.gov/covid-data-tracker/#variant-proportions. Accessed July 22, 2022.
- CDC. Ensuring COVID-19 vaccine safety in the US. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety.html. Accessed July 22, 2022.
- CDC. Stay up to date with your COVID-19 vaccines. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed July 22, 2022.
- Yarlagadda H, Patel MA, Gupta V, et al. COVID-19 vaccine challenges in developing and developed countries. Cureus. 2022;14(4). doi:10.7759/cureus.23951
- Doria-Rose NA, Shen X, Schmidt SD, et al. Booster of mRNA-1273 strengthens SARS-CoV-2 Omicron neutralization. medRxiv. 2021. doi:10.1101/2021.12.15.21267805
- Garcia-Beltran WF, Hoelzemer A, Lam EC, et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. medRxiv. 2021;183:457–466.
- CDC. COVID-19 by county. Available from: https://www.cdc.gov/coronavirus/2019-ncov/your-health/covid-by-county.html. Accessed July 22, 2022.
- CDC. How to protect yourself & others. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed July 22, 2022.
- CDC. COVID-19 testing: what you need to know. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html. Accessed July 22, 2022.
- Johns Hopkins Medicine. COVID variants: what you should know. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/a-new-strain-of-coronavirus-what-you-should-know. Accessed July 24, 2022.
- Sievers C, Zacher B, Ullrich A, et al. SARS-CoV-2 Omicron variants BA.1 and BA.2 both show similarly reduced disease severity of COVID-19 compared to Delta, Germany, 2021 to 2022. Eurosurveillance. 2022;27(22). doi:10.2807/1560-7917.ES.2022.27.22.2200396
- NBC Boston. BA.5 vs. BA.2.75: Boston doctors explain competing omicron subvariants. Available from: https://www.nbcboston.com/news/coronavirus/ba-2-75-boston-doctors-on-whether-we-should-worry-about-The-competing-omicron-subvariant/2772044/. Accessed July 24, 2022.