Abstract
Objective
To preliminarily assess the prevalence and control effect of tuberculosis and drug-resistant tuberculosis (TB) in Anhui province, and analyze the trends in the changing drug resistance spectrum of Mycobacterium tuberculosis (Mtb) isolated in Anhui province from 2016 to 2022.
Methods
From 2016 to 2022, a total of 2336 culture-positive tuberculosis strains were collected from four drug resistance monitoring sites. Patient demographic information was collected and drug susceptibility testing was conducted.
Results
Among the 2336 Mycobacterium tuberculosis complex strains, 1788 (76.54%) were from male patients and 548 (23.46%) were from female patients. The majority were of Han ethnicity, from rural areas, and employed in agriculture, with 12.54% (285/2273) having diabetes. A total of 1893 (81.04%) strains were sensitive to all six anti-TB drugs tested, and 443 (18.96%) strains were resistant to at least one or more anti-TB drugs. The drug resistance rate for patients undergoing initial treatment was 16.80% (348/2071), and 35.85% (95/265) for those receiving retreatment. Among the six anti-TB drugs, the resistance rates from highest to lowest were: INH (10.55%, 236/2336), SM (8.18%, 183/2336), OFX (6.53%, 146/2336), RFP (5.95%, 133/2336), EMB (2.37%, 53/2336), KM (1.97%, 44/2336). Significant differences were observed in MDR strains across different ages, types, with or without diabetes, and geographical sources (χ2=14.895,76.534,6.032,5.109, all P<0.05).
Conclusion
The tuberculosis prevention and control measures have controlled the drug resistance rate of Mycobacterium tuberculosis to a certain extent. However, there are still statistical differences in drug resistance rates among TB patients with different categories, age groups, regions, and diabetic diseases. Early detection and prompt treatment of patients with drug-resistant TB remain critical to controlling the spread of this disease.
Introduction
Tuberculosis is considered the second deadliest communicable disease, primarily transmitted through respiratory droplets or aerosols. According to the 2023 WHO Tuberculosis Report, China holds the third-highest incidence of tuberculosis globally and ranks second in the prevalence of drug-resistant tuberculosis cases.Citation1 Subsequent to the implementation of the 13th Five-Year Plan for Tuberculosis Control and the Three-Year Tuberculosis Action Plan (2020–2022), there has been a significant reduction in the total number of tuberculosis cases in China. However, efforts to control drug-resistant tuberculosis have not yielded significant results. In particular, the treatment outcomes for multidrug-resistant tuberculosis (MDR-TB) have deteriorated when compared to the pre-COVID-19 pandemic data, presenting challenges for the prevention and control of both tuberculosis and its drug-resistant forms in China. To dynamically monitor the prevalence of both tuberculosis and its drug-resistant strains in China, the country has undertaken both a national baseline survey and ongoing monitoring of tuberculosis drug resistance. Anhui province hosts four national tuberculosis drug resistance monitoring sites aimed at preliminarily assessing the prevalence and control effectiveness of tuberculosis and its drug-resistant variants. The following analysis is the results of drug resistance in four drug resistance monitoring sites in Anhui province from 2016 to 2022.Citation2
Data and Methods
Bacterial Strain Source
Tuberculosis strains that tested positive in culture were consistently collected from four drug-resistance monitoring sites between 2016 and 2022. These strains were initially identified as belonging to the Mycobacterium tuberculosis complex through the use of PNB and MPB64 antigen tests. Drug susceptibility testing was conducted employing the proportion method in accordance with the “Tuberculosis Laboratory Testing Procedures”Citation3 In total, 2336 valid Mycobacterium tuberculosis strains were isolated.
Experimental Materials
All culture media required for tuberculosis culture and drug susceptibility testing were obtained from Zhuhai Beisuo Biotechnology Co., Ltd. The drugs assessed using the proportion method for drug susceptibility included isoniazid (INH), rifampicin (RFP), streptomycin (SM), ethambutol (EMB), ofloxacin (OFX), and kanamycin (KM).
Case Information
Following the acquisition of informed consent from tuberculosis patients, basic information was collected and systematically recorded using the National Tuberculosis Drug Resistance Monitoring Patient Information Form.Citation4 In total, completed information forms were collected from four monitoring sites. The data from these forms were then entered into a database using EPIDATA 3.1.
Study Oversight
The study was approved by the Tuberculosis Research Ethics Review Committee of the China CDC and the Ethics Clerical Committee of Anhui Provincial Chest Hospital (No.KJ2014-010). The content of the study was in accordance with the principles of the Declaration of Helsinki, and relevant laws and regulations of medical ethics research requirements. Written informed consent was obtained from each participant. Patients with intellectual disability or those younger than 18 years of age provided informed consent together with parental/legal guardian consent, and a parent or legal guardian provided informed consent for infants.
Quality Control
Internal quality control for sputum smear analysis was implemented at all monitoring sites, with participation in inter-laboratory quality assessments, including blind re-examination of sputum smears, organized by clinical testing centers and provincial reference laboratories. Laboratory personnel conducting culture, strain identification, and drug sensitivity testing received comprehensive training at the national and provincial levels, concurrently performing internal quality control using the standard strain H37Rv, ensuring that the drug sensitivity tests met the national proficiency standards for antituberculosis drug susceptibility. All sputum smear analyses, cultures, and drug sensitivity tests were rigorously controlled and successfully passed inter-laboratory quality assessments, thereby ensuring the validity of the test results obtained. The standard Mycobacterium tuberculosis strain H37Rv was consistently provided by the National Tuberculosis Reference Laboratory.
Statistical
Statistical Analysis: Patient information and drug sensitivity test results were entered into a database using EPIDATA 3.1, with each entry double-checked by two independent researchers. Statistical analysis was conducted using SPSS version 23.0. Count data were expressed as proportions or percentages (%). Differences between groups were compared using the chi-square test. If there is a theoretical count less than 1 or sample size less than 40, Fisher’s exact test was used, considering a P-value of <0.05 as indicative of statistical significance.
Results
Demographic Profile
The cohort comprised 1788 male cases and 548 female cases among the 2336 Mycobacterium tuberculosis strains. Of these, 2071 strains (88.66%) were isolated from patients undergoing initial treatment of pulmonary tuberculosis, and 265 strains (11.34%) from patients undergoing retreatment. The vast majority of cases involved Han Chinese patients, representing 2326 cases (99.57%). A significant proportion of patients, 1535 cases (65.71%), resided in rural areas. Farming was the predominant occupation, encompassing 1483 cases (63.48%). Concurrent conditions included diabetes in 285 cases (12.20%) and hepatitis B in 38 cases (1.63%). provides detailed information on age, education, medical insurance, household size, and annual household income.
Table 1 Characteristics of 2336 Mycobacterium Tuberculosis Isolates from Anhui Province Drug Resistance Surveillance Sites, 2016–2022
Resistance Profile
Of the 2336 Mycobacterium tuberculosis strains under drug resistance surveillance, 1893 strains (81.04%) demonstrated sensitivity to all six antituberculosis drugs tested. This group included 1723 strains (83.20%) from new cases and 170 strains (64.15%) from retreatment cases, while 443 strains exhibited resistance to one or more antituberculosis drugs, with a resistance rate of 18.96% (443/2336), including rates of 16.80% (348/2071) in new cases and 35.85% (95/265) in retreatment cases. Of these, there were 98 multidrug-resistant (MDR) strains (4.20%), including 60 strains (2.90%) from new cases and 38 strains (14.34%) from retreatment cases. The resistance rates for the six antituberculosis drugs, in descending order, were: INH (10.55%, 236/2336), SM (8.18%, 183/2336), OFX (6.53%, 146/2336), RFP (5.95%, 133/2336), EMB (2.37%, 53/2336), and KM (1.97%, 44/2336). Refer to for more details.
Table 2 Drug Resistance Spectrum of 2336 Strains of Mycobacterium Tuberculosis in Drug Resistance Monitoring Sites of Anhui Province from 2016 to 2022
Trends in Antituberculosis Drug Resistance
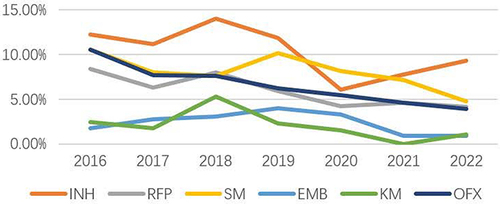
From 2016 to 2022, the resistance rate of ofloxacin decreased annually, with the following annual rates: 10.49%, 7.64%, 7.58%, 6.21%, 5.42%, 4.58%, and 3.89%, respectively. The resistance rate of rifampicin decreased from 8.39% in 2016 to 4.10% in 2022. In 2022, resistance rates for other antituberculosis drugs were lower than in 2016, and the multidrug resistance rate decreased from 4.55% in 2016 to 3.24% in 2022. For more details, please see and .
Table 3 Antimicrobial Resistance Trend Spectrum of 2336 Mycobacterium Tuberculosis Isolates from Anhui Province Surveillance Sites, 2016–2022
Resistance Profiles of Mycobacterium Tuberculosis from Diverse Sources
Among the 2336 strains isolated from 2016 to 2022, no significant difference was observed in the resistance rates to antituberculosis drugs between strains from different genders or annual household income levels (P>0.05). Strains from different categories exhibited statistically significant differences in resistance to all six antituberculosis drugs tested (P<0.05). Significant differences in resistance to INH, RFP, and SM were found among strains from various ages and regions (P<0.05). Resistance to KM also varied significantly across different age groups (P<0.05). Similarly, resistance to OFX differed significantly among strains from various regions (P<0.05). Statistically significant variations were also observed in multidrug-resistant (MDR) strains across age groups, categories, diabetes comorbidity, and regions of origin (P<0.05). Refer to for additional details.
Table 4 Antimicrobial Resistance Profiles of 2336 Mycobacterium Tuberculosis Isolates from Various Sources at Anhui Province’s Drug Resistance Monitoring Sites Between 2016 and 2022
Multidrug-Resistant Strain Analysis
Ninety-eight multidrug-resistant Mycobacterium tuberculosis strains were isolated between 2016 and 2022, and their specific resistance profiles are presented in . The resistance trend of these strains over the same period is depicted in and illustrates the distribution of these strains across different sources.
Table 5 Drug Resistance Spectrum of 98 Strains of MDR-TB in Drug Resistance Monitoring Sites of Anhui Province from 2016 to 2022
Table 6 Antimicrobial Resistance Trend Spectrum of 98 MDR-TB from Anhui Province Surveillance Sites, 2016–2022
Table 7 Distribution of 98 Strains of MDR-TB from Different Sources in Anhui Province from 2016 to 2022
Resistance Profile and Classification Variability in Mycobacterium Tuberculosis Coinciding with Diabetes
A total of 285 out of 2273 monitored Mycobacterium tuberculosis strains, which had associated diabetes information, exhibited concurrent diabetes. Resistance rates in these strains were 10.88% for INH, 9.12% for RFP, 8.77% for SM, 2.81% for both EMB and KM, and 8.42% for OFX, with 7.02% presenting multidrug resistance (MDR). When compared to Mycobacterium tuberculosis strains without diabetes, those with concurrent diabetes demonstrated elevated resistance rates for INH, RFP, SM, EMB, KM, OFX, and a higher incidence of MDR, with these differences reaching statistical significance (P<0.05). Detailed data can be found in and .
Table 8 Drug Resistance Spectrum of Mycobacterium Tuberculosis with Diabetes Mellitus
Table 9 Distribution of Mycobacterium Tuberculosis with Diabetes Mellitus
Discussion
Drug-resistant tuberculosis represents a significant challenge to global efforts in controlling tuberculosis.Citation1,Citation5 It has emerged as a major obstacle in both global and national tuberculosis prevention and control, with a treatment burden significantly greater than that of regular pulmonary tuberculosis. Dynamic monitoring of the drug-resistance spectrum in patients with drug-resistant tuberculosis is crucial for the precise prevention and control of the disease. The WHO guidelines on drug-resistance monitoring assert that analyzing the resistance patterns of tuberculosis bacteria is essential for the timely comprehension of prevalence and trends,Citation6 crucial for the accurate diagnosis and treatment of tuberculosis and for the early eradication of its epidemic.
Drug-resistance monitoring data from 2016 to 2022 reveal that the prevalence of tuberculosis is higher in males than in females, with an increasing trend observed as age advances. The majority of patients are farmers, with most having an education level of junior high school or below and an annual household income of less than 40,000 yuan. This profile suggests that tuberculosis patients are predominantly characterized by low income and education, with the majority residing in rural areas, consistent with findings from other studies.Citation7–9 Among the monitored tuberculosis cohort, 12.54% had coexisting diabetes, while 1.68% were concurrently diagnosed with hepatitis B. Diabetes, a metabolic disorder, can cause metabolic dysregulation and impaired immune function, contributing to the onset of tuberculosis.Citation10 The current rate of latent tuberculosis infection in our country is approximately 20%, with diabetes also acting as an inducing factor for the disease in this patient population.
In the 2336 Mycobacterium tuberculosis strains isolated for drug-resistance monitoring, the resistance rates for six anti-tuberculosis drugs (INH, RFP, SM, EMB, KM, and OFX) were as follows: The trend in drug resistance for these tuberculosis drugs from 2016 to 2022 reveals a yearly decline in the resistance rate of ofloxacin, with rates decreasing from 10.49% to 3.89%, and a downward trajectory for rifampicin resistance, from 8.39% in 2016 to 4.10% in 2022. Resistance rates for the remaining four tuberculosis drugs were lower in 2022 than in 2016. These findings indicate that the implementation of control measures for multidrug-resistant tuberculosis has been notably effective in our province. Following years of dedicated tuberculosis prevention efforts, resistance rates to anti-tuberculosis drugs among patients have progressively declined. Compared to baseline resistance survey Results in our province,Citation11 there has been a significant reduction in the resistance rate to ofloxacin. The execution of tuberculosis prevention and control strategies has brought drug-resistant tuberculosis under a measure of control.
An analysis of 2336 Mycobacterium tuberculosis strains isolated for drug-resistance monitoring revealed no significant differences in resistance rates based on gender or annual household income. However, significant statistical differences were identified in the resistance to the anti-tuberculosis drugs INH, RFP, SM, and KM among strains from different age groups. Strains from patients initially treated for tuberculosis displayed markedly lower resistance rates to six anti-tuberculosis drugs compared to those from patients who had undergone retreatment, indicating that a history of anti-tuberculosis treatment might be one of the risk factors for the development of drug resistance, a finding that aligns with other studies.Citation12–14 In strains from patients with diabetes, the resistance rate to RFP was significantly higher than in strains from tuberculosis-only patients, but this pattern was not observed for the other five anti-tuberculosis drugs. Additionally, strains from rural areas showed significantly lower resistance rates to INH, RFP, SM, and OFX than those from urban areas, which may be due to the higher population density in urban settings and the consequent spread of drug-resistant strains.Citation15,Citation16
Among the 2336 Mycobacterium tuberculosis strains collected over seven consecutive years from diverse sources, there were no significant statistical differences in the resistance rates of the 98 isolated multidrug-resistant strains when analyzed by gender or annual household income. However, variations were observed in relation to age, treatment category, presence of diabetes, and geographic origin. These findings indicate that multidrug-resistant tuberculosis rates differ statistically across different ages, categories, and regions, and also depend on whether diabetes is present. The highest rates of multidrug resistance were found in strains from individuals aged 40–59, and previously treated patients exhibited higher resistance than those receiving initial treatment. Additionally, strains from patients with diabetes showed higher resistance than those from patients with tuberculosis alone. Urban-derived strains had higher multidrug resistance rates than those from rural areas, reflecting the general resistance trends seen in typical tuberculosis. This pattern is consistent with the resistance rates observed in Hunan Province and across the country.Citation7,Citation17
Among the 2336 Mycobacterium tuberculosis strains isolated for drug resistance monitoring, a diversity and complexity in the resistance profiles were observed, suggesting that clinicians should conduct timely drug susceptibility testing and tailor individualized anti-tuberculosis treatment plans based on the actual resistance profiles. The strains showed relatively high resistance rates to INH and SM, consistent with other similar studies.Citation18,Citation19 The highest resistance rate was for INH, potentially due to secondary resistance from its long-standing role as a primary first-line anti-tuberculosis drug in both prophylactic treatment of latent infections and in the widespread treatment of active cases. Studies have indicated that the routine use of SM in treating other infectious diseases may be clinically correlated with high tuberculosis resistance rates.Citation20 With the increased national focus on standardized antibiotic use this year, the previously high resistance rate to OFX has been somewhat controlled, exhibiting a significant decrease compared to the 2015–2016 baseline survey in our province, aligning with the findings of Li Jing et al.Citation21
In the 98 multidrug-resistant Mycobacterium tuberculosis strains isolated from various sources, the resistance spectrum was found to be similar to that of typical tuberculosis strains, also exhibiting diversity and complexity. From 2016 to 2022, the trend in multidrug resistance rates remained relatively stable, suggesting that clinicians should conduct prompt drug sensitivity testing and formulate personalized anti-tuberculosis treatment strategies according to the specific resistance profiles when treating tuberculosis or multidrug-resistant tuberculosis patients. No statistical differences in multidrug resistance rates were observed between patients of varying genders and household income brackets. However, statistically significant variations in multidrug resistance rates were found among strains differentiated by age, category, geographic location, and concurrent diabetes. Within the Mycobacterium tuberculosis strains coexistent with diabetes, statistical differences were only noted in the resistance rates to RFP and in the multidrug resistance (MDR) rates, while other anti-tuberculosis drugs showed no statistical variance. Moreover, strains from populations with and without concurrent diabetes exhibited statistically significant differences in resistance rates across various ages, genders, categories, and income groups, aligning with the research conducted by Mu Lin et alCitation22–24
In summary, the tuberculosis drug-resistance monitoring results in Anhui province reveal that following the implementation of the 13th Five-Year Plan for Tuberculosis Control and the 2019–2022 Action Plan to Curb Tuberculosis, the drug resistance rates of Mycobacterium tuberculosis have been somewhat controlled. However, due to the still large base of pulmonary tuberculosis patients, the incidence of drug-resistant tuberculosis remains relatively high. Statistical differences in drug resistance rates exist among tuberculosis patients of different types, ages, regions, and those with comorbid diabetes. In populations with weakened immunity and in crowded areas, there is a certain risk of transmission for both tuberculosis and drug-resistant tuberculosis. To prevent the spread of drug-resistant tuberculosis among the population, early detection and timely treatment of drug-resistant pulmonary tuberculosis patients remains an effective means to control its transmission.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- World Health Organization. Global Tuberculosis Report 2023. Geneva: WHO; 2023.
- Bao X, Liang S, Li J, et al. Analysis of Mycobacterium tuberculosis drug resistance monitoring in Anhui Province from 2016 to 2022[J]. Chin J Antitubercul. 2024;46(5):531–537. doi:10.19982/j.issn.1000-6621.20240029
- Zhao Y, Pang Y. Tuberculosis Laboratory Testing Procedures. Beijing: People’s Medical Publishing House; 2015.
- Wang S, Zhou Y, Ou X, et al. Current status of tuberculosis drug resistance in China: analysis of data from the national tuberculosis drug resistance surveillance in 2018 [J]. Chin J Antituberculosis. 2021;43(11):1141–1147. doi:10.19982/j.iscn.1000-6621.20220268
- Ministry of Health of the People’s Republic of China. National Baseline Survey on Tuberculosis Drug Resistance: 2007–2008. Beijing: People’s Medical Press; 2010.
- World Health Organization. Guidelines for Surveillance of Drug Resistance in Tuberculosis. 6th ed. Geneva: World Health Organization; 2021.
- Bai H, Guo JW, Hu PL, et al. Analysis of drug resistance surveillance results of Mycobacterium tuberculosis in drug resistance monitoring sites of Hunan province from 2014 to 2018 [J]. Chin J Antituberculosis. 2021;43(4):364–369.
- Zhou Y, Liu R, Du YG, et al. Drug susceptibility analysis of 128 multi-drug resistant Mycobacterium tuberculosis strains in Hainan province, 2014–2016. Chin J Trop Med. 2018;18(6):551–554.
- Zhao J, Jiang Y, Wu W, et al. Detection and analysis of drug resistance genes of Mycobacterium tuberculosis in three surveillance sites in Jiangxi province [J]. Dis Surveillance. 2022;37(1):127–131.
- Luo M, Zou X, Gao Y, et al. Effect of anti-tuberculosis treatment and lung injury in patients with tuberculosis complicated with underlying diseases [J]. J Shanghai Jiaotong Univ. 2023;43(8):1017–1023.
- Wang Q, Ma D, Liu J, et al. Analysis of baseline sampling survey results of drug resistance in smear-positive pulmonary tuberculosis patients in Anhui province [J]. Chin J Antitubercul. 2018;40(8):825–833. doi:10.3969/j.issn.1000-6621.2018.08.010
- Zhang J, Li H, Wang F, et al. Drug resistance analysis in retreated tuberculosis patients at tuberculosis control agencies in Beijing. J Clin Pulm Med. 2023;28(8):1185–1189.
- Ge Q, Zhang L, Huang X, et al. Efficacy verification of a novel treatment scheme for initial retreatment of sensitive pulmonary tuberculosis. Chin J Antitubercul. 2023;45(11):1078–1083. doi:10.19982/j.issn.1000-6621.20230192
- Yu X, Wang L. Analysis of Drug Sensitivity in 402 Clinical Isolates of Mycobacterium Tuberculosis. J Chin Health Inspect. 2023;33(19):2340–2342, 2346.
- Yang C, Luo T, Shen X, et al. Transmission of multidrug-resistant Mycobacterium tuberculosis in Shanghai, China: a retrospective observational study using whole-genome sequencing and epidemiological investigation. Lancet Infect Dis. 2017;17(3):275–284. doi:10.1016/S1473-3099(16)30418-2
- Gao Q, Mei J. Transmission is the main reason for the high drug resistance rate of tuberculosis in China. Chin J Antituberculosis. 2015;37(11):1091–1096. doi:10.3969/j.issn.1000-6621.2015.11.002
- Wang S, Zhao B, Song Y, et al. Risk Factors for Drug-Resistant Tuberculosis in China: an Analysis of Data from the 2007 National Baseline Survey on Tuberculosis Resistance. Chin J Antituberculosis. 2013;35(4):221–226.
- Gao WF, Yang Y, Wang WN, et al. Analysis of Tuberculosis Drug Resistance at Ten Drug Resistance Monitoring Sites in Sichuan Province, 2016–2017. J Prev Med Inf. 2019;35(7):681–686.
- Zhong MH, Yan L, Li WH, et al. Analysis of Drug Resistance Characteristics of Mycobacterium Tuberculosis in Dongguan City, 2018. J Guangdong Pharm Univ. 2020;36(2):259–265. doi:10.16809/j.cnki.2096-3653.2019121403
- Hang NT, Maeda S, Lien LT, et al. Primary Drug-Resistant Tuberculosis in Hanoi, Vietnam: present Status and Risk Factors. PLoS One. 2013;8(8):e71867. doi:10.1371/journal.pone.0071867
- Li J, Zhang YY, Wu J, et al. Trend of Drug Resistance of Tuberculosis in Shanghai from 2007 to 2012. Chin J Antituberculosis. 2014;36(1):25–30. doi:10.3969/j.issn.1000-6621.2014.01.006
- Lin M, Liao J, Gong Y, et al. Diabetes and Multidrug-Resistant Gene Mutations Associated with Tuberculosis in Zunyi, Southwest China. Ann Palliat Med. 2020;9(5):3152–3161. doi:10.21037/apm-20-1368
- Williams V, Vos-Seda AG, Haumba S, et al. Diabetes-Tuberculosis Care in Eswatini: qualitative Study of Opportunities and Recommendations for Effective Services Integration. Int J Public Health. 2023;68:1605551. doi:10.3389/ijph.2023.1605551
- Ozma MA, Rashedi J, Poor BM, et al. Tuberculosis and Diabetes Mellitus in the Northwest of Iran. Infect Disord Drug Targets. 2020;20(5):667–671. doi:10.2174/1871526519666190715142100