Abstract
Purpose
Elizabethkingia spp. infections have recently increased, and they are difficult to treat because of intrinsic antimicrobial resistance. This study aimed to investigate the clinical characteristics of patients with pulmonary infection with Elizabethkingia spp. and reveal the risk factors for infection and death.
Patients and Methods
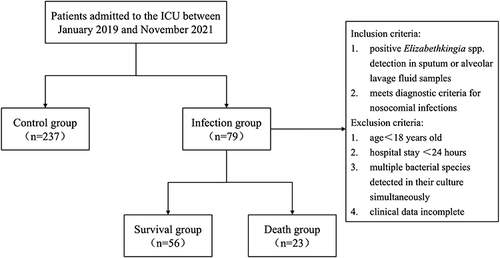
In this retrospective case–control study, patients were divided into infection and control groups based on the bacterial identification results. Patients in the infection group were further divided into survival and death groups according to their hospital outcomes. Clinical characteristics between different groups were compared. We further analyzed antimicrobial susceptibility testing results of the isolated strains.
Results
A total of the 316 patients were divided into infection (n = 79), 23 of whom died, and control (n = 237) groups. Multivariate logistic regression analysis showed that glucocorticoid consumption (OR: 2.35; 95% CI: 1.14–4.81; P = 0.02), endotracheal intubation (OR: 3.74; 95% CI: 1.62–8.64; P = 0.002), and colistin exposure (OR: 2.50; 95% CI: 1.01–6.29; P = 0.046) were significantly associated with pulmonary infection with Elizabethkingia spp. Advanced age (OR: 1.07, 95% CI: 1.00–1.15; P = 0.046), high acute physiology and chronic health evaluation (APACHE) II score (OR: 1.21; 95% CI: 1.01–1.45; P = 0.037), and low albumin level (OR: 0.73, 95% CI: 0.56–0.96; P = 0.025) were significantly associated with in-hospital mortality of infected patients. Elizabethkingia spp. was highly resistant to cephalosporins, carbapenems, macrolides, and aminoglycoside, and was sensitive to fluoroquinolones, minocycline, and co-trimoxazole in vitro.
Conclusion
Glucocorticoid consumption, tracheal intubation, and colistin exposure were associated with pulmonary infection with Elizabethkingia spp. for critically ill patients. Patients with advanced age, high APACHE II score, and low albumin level had higher risk of death from infection.
Introduction
Pulmonary infection is one of the most common infectious diseases, resulting in the fourth leading cause of death in the world in 2019 and the second cause of death in low-income countries.Citation1 Nosocomial pneumonia is defined as a pulmonary infection that occurs after 48 h of admission to the hospital and accounts for 22% of nosocomial infections.Citation2 It is also the most common intensive care unit (ICU)-acquired infection.Citation3 With the increase of drug-resistant bacteria in ICU,Citation4 treatment of nosocomial pneumonia in critically ill patients has become challenging.
Elizabethkingia spp., belonging to the Flavobacteriaceae family, were discovered in the 1950s and was once named Flavobacterium meningosepticum.Citation5 Elizabethkingia spp. are aerobic, non-motile, non-sugar-fermenting, oxidase-positive, and Gram-negative bacilli.Citation6 They widely present in natural environments, can survive in chloride-treated urban water systems, and can colonize in hospital environments, such as ventilator tubing, humidifiers, intravenous catheters, and refrigerators. Due to their intrinsic resistance to a variety of antibiotics,Citation7–16 Elizabethkingia spp. can cause serious opportunistic infections. Elizabethkingia spp. mainly infect the infants, older people, and immunocompromised patients, leading to pneumonia, meningitis, bacteremia, and skin infections.Citation17–20 The mortality rate of Elizabethkingia spp. infections were 13.5–70%.Citation7–10,Citation19–23
Elizabethkingia spp. infection are increasing in many countries,Citation10,Citation20,Citation24 and there are outbreaks of infection.Citation17,Citation21 A study in South Korea showed that the infection rate of Elizabethkingia spp. in inpatients of the Severance Hospital in Seoul increased from 0.002% in 2009 to 0.088% in 2017.Citation19 Another study in Taiwan showed that the infection rate of Elizabethkingia spp. in carbapenem-resistant non-fermenting, Gram-negative bacilli was only second to that of Acinetobacter baumannii.Citation25
Although there have been some studies on Elizabethkingia spp. infection in China, few of them focusing on the clinical characteristic, antibiotic resistance, and risk factors of pulmonary infection with Elizabethkingia spp. in critically ill patients. We aim to depict those aspects of Elizabethkingia spp. infection and provide scientific evidence for treatment.
Materials and Methods
Research Subjects
This retrospective case–control study was conducted at the First Affiliated Hospital of Nanjing Medical University. The clinical data of critically ill patients with pulmonary infection with Elizabethkingia spp. who admitted to ICU between 1 January 2019 and 30 November 2021 were collected. Only the first episode was considered for patients with more than one positive Elizabethkingia spp. culture. Pulmonary infection with Elizabethkingia spp. criteria: (1) positive Elizabethkingia spp. detection in sputum or alveolar lavage fluid samples; (2) body temperature >38°C, white blood cell counts >12×109/L, and typical chest imaging features. Exclusion criteria: (1) hospital stay <48 h; (2) age <18 years old; (3) who had multiple bacterial species detected in their culture simultaneously; (4) clinical data incomplete.
Control group defined as selected patients with non-Elizabethkingia spp. infection who hospitalized in the same ward during the same time (at a 3:1 ratio to the infection group).
Clinical data, including age, gender, underlying diseases, Charlson comorbidity index (CCI), acute physiology and chronic health evaluation (APACHE) II score, sequential organ failure assessment (SOFA) score, vital signs, chest imaging results, laboratory results, antibiotic treatments, and invasive procedures, were collected from the electronic medical record system. The main outcome measure of this study was in-hospital mortality.
Recent surgery was defined as surgery performed within 14 days before the first diagnosis of Elizabethkingia spp. infection. The use of glucocorticoids was defined as at least 20 mg of prednisone per day or equivalent. Antibiotic exposure was defined as treatment with antibiotic intravenously or by nebulization for more than 24 h within 1 month before Elizabethkingia spp. infection. Susceptible antibiotic therapy was defined as the use of at least one antibiotic to which the Elizabethkingia spp. was susceptible according to the minimum inhibitory concentration (MIC) within 72 h of confirmed infection.
Bacterial Identification and Antimicrobial Susceptibility Tests
Specimens were cultured and isolated in accordance with the third edition of National Clinical Laboratory Procedures. Following incubation on 5% sheep blood agar and MacConkey agar plates (bioMerieux, Shanghai, China) and incubated at 35 °C for 18‒24 h, all positive cultures were subjected to Gram staining and microscopic examinations. Microbial identification was performed using the VITEK-2 system (bioMerieux, Marcy L’Etoile, France).
Susceptibilities of the isolates to antimicrobials were determined using epsilometer test (E-test) strips (bioMerieux, Marcy L’Etoile, France). The results of antimicrobial susceptibility testing (AST) were determined according to the Clinical and Laboratory Standards Institute (CLSI) M100 (2020) for “other non-Enterobacteriaceae” as there are no standard guidelines for reporting AST for Elizabethkingia spp.
Statistical Analysis
As mentioned above, all patients were divided into infection and control groups. Patients in the infection group were subdivided into death and survival groups according to their prognosis. Continuous variables are presented as median and interquartile ranges [M(P25, P75)] and were compared between groups using the Mann–Whitney U-test. Categorical variables are presented as frequency and percentile and were compared between groups using the chi-square test or Fisher’s exact test. The variance inflation factor (VIF) was calculated to assess the multicollinearity problem. Univariate logistic regression analysis was used to analyze the factors related to infection and death in the patients. Variables with a statistical significance of P < 0.1 and VIF < 2 were included in the multivariate logistic regression analysis to determine the risk factors. The results were presented as an adjusted odds ratio (OR) and 95% confidence interval (CI). All statistical analyses were performed using R 4.2.2 software (The R Project for Statistical Computing, Vienna Austria). A P < 0.05 was considered statistically significant.
Ethics
This retrospective study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2023-SR-412), which also exempted this trial from informed consent, considering that obtaining informed consent was impractical. Patient data was maintained with confidentiality. The study has been performed in accordance with the ethical standards laid down in the Declaration of Helsinki 1964 and its later amendments or comparable ethical standards.
Results
General Conditions
A total of 114 critically ill patients had Elizabethkingia spp. isolated from the respiratory tract from 1 January 2019 to 30 November 2021, of which 79 patients were included in the infection group. A total of 237 were included in the control group. Patients in the infection group were divided into a death group, including 23 patients, and a survival group, including 56 patients, based on hospitalization outcomes. Details are shown in . The median age of the infection group was 66 (52–72.5) years old, and 51 (64.6%) were males. Compared to the control group, more patients in the infection group use glucocorticoid (25.3% vs 13.5%), carbapenem antibiotics (63.3% vs 47.3%), and colistin (15.2% vs 5.49%) and have higher rates of invasive procedures such as indwelling central venous catheters (83.5% vs 67.5%), bronchoscopy (38% vs 20.7%), mechanical ventilation (81% vs 67.9%), and endotracheal intubation (88.6% vs 64.6%). Twenty-three (29.1%) infected patients died during hospitalization, a higher proportion than that of the control group, but the difference was not statistically significant. Compared to the surviving group, the mortality group had a higher proportion of patients with higher age (76 vs 64), disease severity score, coronary artery disease (34.8% vs 12.5%), kidney disease (47.8% vs 19.6%), and hemodialysis treatment (47.8% vs 14.3%), and lower recent surgery (30.4% vs 64.3%), hemoglobin (83 vs 95.5), platelets (106 vs 172), and serum albumin (31.3 vs 35.6). The demographic and clinical characteristics of the enrolled patients are detailed in and .
Table 1 Baseline Demographic and Clinical Characteristics Between Patients in Infection and Control Group
Table 2 Baseline Demographic and Clinical Characteristics Between Patients in Survival and Death Group
Risk Factors for Pulmonary Infection with Elizabethkingia spp
Univariate logistic regression analysis showed that patients in the infection group had higher APACHE II score and higher proportions of kidney diseases, glucocorticoid consumption, central venous catheterization, gastrointestinal intubation, bronchoscopy, renal replacement therapy (RRT), mechanical ventilation, endotracheal intubation, carbapenem exposure, and colistin exposure than patients in the control group (P < 0.1). Multivariate logistic regression analysis of the above variables showed that glucocorticoid consumption (OR: 2.35; 95% CI: 1.14–4.81; P = 0.02), endotracheal intubation (OR: 3.74; 95% CI: 1.62–8.64; P = 0.002), and colistin exposure (OR: 2.50; 95% CI: 1.01–6.29; P = 0.046) were associated with pulmonary infection with Elizabethkingia spp. ().
Table 3 Risk Factors for Pulmonary Infection with Elizabethkingia Spp
Risk Factors for Death in Infected Patients
Patients with pulmonary infection with Elizabethkingia spp. in the death group had higher age, APACHE II score, SOFA score, creatinine, proportions of with diabetes, coronary artery diseases, kidney diseases, use of RRT and mechanical ventilation than that in the survival group. In contrast, survival patients more likely to have higher levels of hemoglobin, platelets, albumin, and fluoroquinolones and susceptible antibiotic therapy (P < 0.1). Multivariate logistic regression analysis showed that advanced age (OR: 1.07, 95% CI: 1.00–1.15; P = 0.046), high APACHE II score (OR: 1.21; 95% CI: 1.01–1.45; P = 0.037), and low albumin level (0.73, 95% CI: 0.56–0.96; P = 0.025) were risk factors for death in the infected patients ().
Table 4 Risk Factors for Death in Patients with Pulmonary Infection with Elizabethkingia Spp
Drug Susceptibility Results
Elizabethkingia spp. isolated are resistant to commonly used antibiotics. The first antimicrobial susceptibility testing results for Elizabethkingia spp. isolated from infected patients are provided in .
Table 5 Results of Antimicrobial Susceptibility Testing of Commonly Used Antibiotics for Elizabethkingia Spp
Discussion
Critically ill patients with impaired immune function and high rates of antimicrobial drug use are prone to nosocomial infections. In this study, we determined the risk factors for pulmonary infection with Elizabethkingia spp. in critically ill patients by logistic regression analysis. We further analyzed the risk factors for death in critically ill patients infected with Elizabethkingia spp. Because Elizabethkingia spp. is resistant to commonly used antibiotics, we also statistically analyzed the resistance of Elizabethkingia spp. in our region. It provides a reference for clinicians to diagnose and treat Elizabethkingia spp. infections.
Studies have shown that more than 85% of patients with Elizabethkingia spp. infection have at least one underlying disease.Citation18,Citation26,Citation27 In addition, diabetes, hypertension, end-stage kidney disease, malignancy, immunosuppressive therapy, invasive operation, and history of antibiotic exposure are risk factors for Elizabethkingia spp. infection.Citation9,Citation10,Citation17–19,Citation23,Citation28 In our study, the proportions of use glucocorticoid, carbapenem antibiotics, colistin, and invasive procedures such as indwelling central venous catheters, bronchoscopy, mechanical ventilation, and endotracheal intubation in patients with Elizabethkingia spp. infection were high. In addition, glucocorticoid consumption, endotracheal intubation, and colistin exposure were risk factors for Elizabethkingia spp. infection. Elizabethkingia spp. can form biofilms,Citation11 facilitating their colonization in hospital environments, such as sinks and ventilator tubing that are difficult to remove. Glucocorticoids have multiple functions,Citation29 patients with asthma, autoimmune diseases, organ transplantation, etc., need to use glucocorticoids, and the surviving sepsis campaign guideline suggests that patients with septic shock can be treated with glucocorticoids.Citation30 However, glucocorticoids have significant side effects along with their therapeutic effects, such as elevated blood glucose, metabolic disorders, and suppression of immune function. Studies have shown that the incidence of serious and opportunistic infections increases with glucocorticoid use.Citation31 When patients are undergoing invasive procedures such as endotracheal intubation, the Elizabethkingia spp. can enter the body and induce opportunistic infections.Citation19 Carbapenem-resistant Enterobacteriaceae infections pose a major threat to human health due to limited treatment options. Colistin-based regimens have become a major treatment option,Citation32,Citation33 and long courses of colistin therapy have reduced 30-day mortality in critically ill patients.Citation34 However, Huang et al showed that patients who received nebulized colistin had a relatively high proportion of Elizabethkingia spp. infection,Citation25 and although the method of colistin use was different from that of our study, the results all demonstrated that the use of colistin was associated with Elizabethkingia spp. infections. Elizabethkingia spp. may become dominant and cause infection when using colistin due to its natural resistance to colistin. Hus et al showed that Elizabethkingia spp. isolated from approximately one of two adults and one of three infants were colonized bacteria.Citation35 In this study, among the 114 critically ill patients with Elizabethkingia spp. isolated from the respiratory tract, 79 patients (69.3%) were diagnosed with Elizabethkingia spp. infection. This rate was higher than in previous studies and may be related to the poor conditions, more invasive procedures and the high percentage of colistin use in critically ill patients.
The mortality rates of patients infected with Elizabethkingia spp. range from 13.5% to 70%.Citation7–10,Citation19–23 For example, 25 of 75 patients with Elizabethkingia spp. infection died during the outbreak of Elizabethkingia spp. in Wisconsin and Illinois in the United States in 2014–2016.Citation36 In 2019, four of six children with Elizabethkingia spp. infection in the pediatric ICU of a hospital in Turkey died.Citation21 In this study, the mortality of critically ill patients with pulmonary infection with Elizabethkingia spp. was 29.1% (23/79 cases). The results of the multifactor logistic regression showed that advanced age, high APACHE II score, and low albumin level were risk factors for death in patients with pulmonary infection with Elizabethkingia spp. Aging is associated with changes in physiological, biological, immunological, and behavioral. Increased age leads to a progressive loss of cellular function and tissue renewal and a decline in immune function, which increases susceptibility to infection.Citation37,Citation38 Previous studies have confirmed that high simplified acute physiological score (SAPS) II, elevated C-reactive protein-to-albumin ratio, and reduced hemoglobin level were correlated with death in patients with Elizabethkingia spp. infection.Citation10,Citation18,Citation22 SAPS II score and APACHE II score are tools for assessing the severity of disease in critically ill patients, and several studies have shown that the APACHE II score has a good predictive efficacy for patient prognosis.Citation39 Serum albumin plays an important role in volume expansion, maintenance of vascular endothelial integrity, and anti-inflammation.Citation40 Reduced serum albumin levels are strongly associated with mortality in patients with cardiovascular disease, heart failure, and cirrhosis.Citation41,Citation42
Resistant to multiple antibiotics is one of the biological characteristics of Elizabethkingia.Citation9–13,Citation18,Citation26,Citation43 In our study, the rates of resistance to cephalosporins, aztreonam, imipenem, and meropenem reached 100%. Elizabethkingia spp. carries two types of antimicrobial resistance genes. These include blaCME, which encodes an extended spectrum β-lactamase that mainly mediates resistance to cephalosporins, and blaBlaB and blaGOB, which encode metallo-β-lactamase that mediates resistance to all β-lactam antibiotics, including carbapenems.Citation9,Citation10,Citation17 However, the susceptibility of Elizabethkingia spp. to antibiotics containing enzyme inhibitors varies considerably. The susceptibility of isolated strains to piperacillin–tazobactam was 72.2%, while their rates of resistance to cefoperazone–sulbactam and ceftazidime–avibactam were 72.7% and 66.7%, respectively. Elizabethkingia spp. also carries GCN5-related N-acetyltransferases (GNATs) and nucleoside transferase (ANT(6)), which mediate resistance to aminoglycoside antibiotics. Shirmast et al showed that the carrying rate of the ant(6) gene of this bacterial genus was 92.4–100%.Citation16 In this study, the isolate strains were 100% resistant to tobramycin and >90% resistant to amikacin and gentamicin. More than 83% isolated strains were resistance to vancomycin. Elizabethkingia spp. carry vanW and vanB genes, which encode metabolic enzymes to synthesize low-affinity precursors to eliminate vancomycin targets.Citation14,Citation44 The susceptibilities of isolated strains to ciprofloxacin and levofloxacin were 58.2% and 67.1%. Studies have shown multiple amino acid mutations in the quinolone resistance determination region (QRDR) of the DNA gyrase subunits or topoisomerase IV subunits of Elizabethkingia spp., leading to a decrease in the affinity or inability of binding between target proteins and drugs.Citation9,Citation17,Citation18,Citation26 In our study, Elizabethkingia spp. were susceptible to co-trimoxazole (70.9%) and minocycline (75%). In addition, Elizabethkingia spp. have multiple drug-resistance mechanisms via chloramphenicol acetyltransferase, ribosomal protection proteins, and multidrug efflux pumps, which are related to resistance to chloramphenicol, tetracycline, and erythromycin.Citation11,Citation14,Citation16
Moreover, the drug resistance of Elizabethkingia spp. varies in different regions. For example, more than 88% of Elizabethkingia spp. in the United States, South Korea, Taiwan, and Shanghai are susceptible to piperacillin–tazobactam.Citation7,Citation17,Citation18,Citation26,Citation45 However, 68.7% of the isolated Elizabethkingia spp. strains in the Australia are resistant to piperacillin–tazobactam.Citation14 In Taiwan, Elizabethkingia spp. had a susceptibility to fluoroquinolones of 78.6% in KaohsiungCitation13 and a resistance rate of 85% in Taipei.Citation26
How to treat patients infected with Elizabethkingia spp. is a tricky question. Previous studies suggest that removal of indwelling intravenous catheters improves the curative rate in patients with Elizabethkingia spp. infection.Citation21,Citation27 The early identification of these clinical factors in patients with Elizabethkingia spp. infection could be essential to improve prognosis. Lack of effective antibiotic treatment is an independent predictor of death.Citation35 Although Elizabethkingia spp. has been reported to be sensitive to minocycline, piperacillin–tazobactam, and fluoroquinolones, the benefits of using fluoroquinolonesCitation46,Citation47 and piperacillin-tazobactamCitation10,Citation21 have been conflicting in different studies. This may be related to the complex drug-resistance mechanism of Elizabethkingia spp., and the drug resistance of Elizabethkingia spp. varies among different strains and in different regions. Patients with Elizabethkingia spp. infection should be treated promptly according to the results of drug-susceptibility testing. Literature reports that the MIC value of Elizabethkingia spp. to vancomycin is usually 8–256 mg/L,Citation7,Citation18 and in this study, no vancomycin-sensitive Elizabethkingia spp. strains were isolated. However, other studies have shown that the combined use of vancomycin with other antibiotics achieved bacterial clearance and curative outcomes in clinical practice.Citation24 The mechanism may be that vancomycin controls Gram-positive bacterial infection while destroying the cell wall of Elizabethkingia spp., which facilitates the entry of other drugs into the bacteria for action.
Nevertheless, this study has certain limitations. First, there was no species classification or gene sequencing of the genus Elizabethkingia spp. Second, the results and conclusion of this single-center study may be affected by geographic location, hospital management strategies, and infection control policies. Furthermore, due to the retrospective research design, some key factors of Elizabethkingia spp. infection may have been overlooked, without intervention on the use of antibiotics. Finally, the relatively small sample size of this study may affect the reliability of the results.
Conclusion
Elizabethkingia spp. is a common pathogen in the ICU with multi-drug resistance and requires considerable attention in clinical practice. Patients with glucocorticoid, endotracheal intubation and colistin are prone to Elizabethkingia spp. infection. Patients with Elizabethkingia spp. infection, along with advanced age, high APACHE II score, and low albumin level, should be of particular concern. Minocycline, and co-trimoxazole can be used empirically.
Abbreviations
ICU, intensive care unit; CCI, Charlson comorbidity index; APACHE II, acute physiology and chronic health evaluation II; SOFA, sequential organ failure assessment score; MIC, minimum inhibitory concentration; AST, antimicrobial susceptibility testing; VIF, variance inflation factor; OR, odds ratio; CI, confidence interval; RRT, renal replacement therapy; COPD, chronic obstructive pulmonary disease; WBC, White blood cell count; Neu, Neutrophil count; Hb, Hemoglobin; PLT, Platelets; TB, total bilirubin; Alb: Albumin; Cr: Creatinine; Pct: Procalcitonin; SAPS II, simplified acute physiological score II; QRDR, quinolone resistance determination region.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2023-SR-412), with a waiver of informed consent. The study has been performed in accordance with the ethical standards laid down in the Declaration of Helsinki 1964 and its later amendments or comparable ethical standards.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- World Health Organization. The top 10 causes of death, Available from: http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed December 9, 2020.
- Magill SS, Edwards JR, Bamberg W, et al. Multistate Point-Prevalence Survey of Health Care–Associated Infections. N Engl J Med. 2014;370(13):1198–1208. doi:10.1056/NEJMoa1306801
- Torres A, Niederman MS, Chastre J, et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). Eur Respir J. 2017;50(3):1700582. doi:10.1183/13993003.00582-2017
- Zilahi G, Artigas A, Martin-Loeches I. What’s new in multidrug-resistant pathogens in the ICU? Ann Intensive Care. 2016;6(1):96. doi:10.1186/s13613-016-0199-4
- King EO. Studies on a Group of Previously Unclassified Bacteria Associated with Meningitis in Infants. Am J Clin Pathol. 1959;31(3):241–247. doi:10.1093/ajcp/31.3.241
- Nicholson AC, Gulvik CA, Whitney AM, et al. Revisiting the taxonomy of the genus Elizabethkingia using whole-genome sequencing, optical mapping, and MALDI-TOF, along with proposal of three novel Elizabethkingia species: Elizabethkingia bruuniana sp. nov. Elizabethkingia ursingii sp. nov. and Elizabethkingia occulta sp. nov. Antonie van Leeuwenhoek. 2018;111(1):55–72. doi:10.1007/s10482-017-0926-3
- Han MS, Kim H, Lee Y, et al. Relative Prevalence and Antimicrobial Susceptibility of Clinical Isolates of Elizabethkingia Species Based on 16S rRNA Gene Sequencing. J Clin Microbiol. 2017;55(1):274–280. doi:10.1128/JCM.01637-16
- Singh S, Sahu C, Singh Patel S, et al. Clinical profile, susceptibility patterns, speciation and follow up of infections by Elizabethkingia species: study on a rare nosocomial pathogen from an intensive care unit of north India. New Microbes New Infections. 2020;38:100798. doi:10.1016/j.nmni.2020.100798
- Wang L, Zhang X, Li D, et al. Molecular Characteristics and Antimicrobial Susceptibility Profiles of Elizabethkingia Clinical Isolates in Shanghai, China. IDR. 2020;13:247–256. doi:10.2147/IDR.S240963
- Chang Y, Zhang D, Niu S, et al. MBLs, Rather Than Efflux Pumps, Led to Carbapenem Resistance in Fosfomycin and Aztreonam/Avibactam Resistant Elizabethkingia anophelis. IDR. 2021;14:315–327. doi:10.2147/IDR.S294149
- Chen S, Soehnlen M, Blom J, et al. Comparative genomic analyses reveal diverse virulence factors and antimicrobial resistance mechanisms in clinical Elizabethkingia meningoseptica strains. PLoS One. 2019;14(10):e0222648. doi:10.1371/journal.pone.0222648
- Cheng YH, Perng CL, Jian MJ, et al. Multicentre study evaluating matrix-assisted laser desorption ionization–time of flight mass spectrometry for identification of clinically isolated Elizabethkingia species and analysis of antimicrobial susceptibility. Clin Microbiol Infect. 2019;25(3):340–345. doi:10.1016/j.cmi.2018.04.015
- Chiu CT, Lai CH, Huang YH, et al. Comparative Analysis of Gradient Diffusion and Disk Diffusion with Agar Dilution for Susceptibility Testing of Elizabethkingia anophelis. Antibiotics. 2021;10(4):450. doi:10.3390/antibiotics10040450
- Burnard D, Gore L, Henderson A, et al. Comparative Genomics and Antimicrobial Resistance Profiling of Elizabethkingia Isolates Reveal Nosocomial Transmission and ISusceptibility to Fluoroquinolones, Tetracyclines, and Trimethoprim-Sulfamethoxazole. J Clin Microbiol. 2020;58(9). doi:10.1128/JCM.00730-20
- Sun P, Xu YQ, Xia WY, et al. Distribution and antimicrobial susceptibility of Elizabethkingia meningosepticum strains isolated during 2012—2016 period. Chin J Infect Chemother. 2018;018(004):421–423. doi:10.16718/j.1009-7708.2018.04.013
- Shirmast P, Ghafoori SM, Irwin RM, et al. Structural characterization of a GNAT family acetyltransferase from Elizabethkingia anophelis bound to acetyl-CoA reveals a new dimeric interface. Sci Rep. 2021;11(1):1274. doi:10.1038/s41598-020-79649-5
- Perrin A, Larsonneur E, Nicholson AC, et al. Evolutionary dynamics and genomic features of the Elizabethkingia anophelis 2015 to 2016 Wisconsin outbreak strain. Nat Commun. 2017;8(1):15483. doi:10.1038/ncomms15483
- Lin JN, Lai CH, Yang CH, et al. Comparison of Clinical Manifestations, Antimicrobial Susceptibility Patterns, and Mutations of Fluoroquinolone Target Genes between Elizabethkingia meningoseptica and Elizabethkingia anophelis Isolated in Taiwan. JCM. 2018;7(12):538. doi:10.3390/jcm7120538
- Choi MH, Kim M, Jeong SJ, et al. Risk Factors for Elizabethkingia Acquisition and Clinical Characteristics of Patients, South Korea. Emerg Infect Dis. 2019;25(1):42–51. doi:10.3201/eid2501.171985
- Lau SKP, Chow WN, Foo CH, et al. Elizabethkingia anophelis bacteremia is associated with clinically significant infections and high mortality. Sci Rep. 2016;6(1):26045. doi:10.1038/srep26045
- Erinmez M, Buyuktas MA, Zer Y. Investigation of an outbreak of Elizabethkingia meningoseptica on a pediatric intensive care unit. GMSHygiene andInfection Control. 2021;16:Doc19. doi:10.3205/dgkh000390
- Seong H, Kim JH, Kim JH, et al. Risk Factors for Mortality in Patients with Elizabethkingia Infection and the Clinical Impact of the Antimicrobial Susceptibility Patterns of Elizabethkingia Species. JCM. 2020;9(5):1431. doi:10.3390/jcm9051431
- Umair A, Nasir N. Clinical features and outcomes of critically ill patients with Elizabethkingia meningoseptica: an emerging pathogen. Acute Crit Care. 2021;36(3):256–261. doi:10.4266/acc.2020.01158
- Tai IC, Liu TP, Chen YJ, et al. Outbreak of Elizabethkingia meningoseptica sepsis with meningitis in a well-baby nursery. J Hosp Infect. 2017;96(2):168–171. doi:10.1016/j.jhin.2016.11.018
- Huang YC, Wu PF, Lin YT, et al. Comparison of clinical characteristics of bacteremia from Elizabethkingia meningoseptica and other carbapenem-resistant, non-fermenting Gram-negative bacilli at a tertiary medical center. J Microbiol Immunol Infect. 2019;52(2):304–311. doi:10.1016/j.jmii.2018.06.007
- Jian MJ, Cheng YH, Chung HY, et al. Fluoroquinolone resistance in carbapenem-resistant Elizabethkingia anophelis: phenotypic and genotypic characteristics of clinical isolates with topoisomerase mutations and comparative genomic analysis. J Antimicrob Chemother. 2019;74(6):1503–1510. doi:10.1093/jac/dkz045
- Teng LC, Wang JM, Lu HY, et al. Elizabethkingia Intra-Abdominal Infection and Related Trimethoprim-Sulfamethoxazole Resistance: a Clinical-Genomic Study. Antibiotics. 2021;10(2):173. doi:10.3390/antibiotics10020173
- Chan JC, Chong CY, Thoon KC, et al. Invasive paediatric Elizabethkingia meningoseptica infections are best treated with a combination of piperacillin/tazobactam and trimethoprim/sulfamethoxazole or fluoroquinolone. J Med Microbiol. 2019;68(8):1167–1172. doi:10.1099/jmm.0.001021
- Cain DW, Cidlowski JA. Immune regulation by glucocorticoids. Nat Rev Immunol. 2017;17(4):233–247. doi:10.1038/nri.2017.1
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–1247. doi:10.1007/s00134-021-06506-y
- Youssef J, Novosad SA, Winthrop KL. Infection Risk and Safety of Corticosteroid Use. Rheum Dis Clin North Am. 2016;42(1):157–x. doi:10.1016/j.rdc.2015.08.004
- Katip W, Rayanakorn A, Sornsuvit C, et al. High-Loading-Dose Colistin with Nebulized Administration for Carbapenem-Resistant Acinetobacter baumannii Pneumonia in Critically Ill Patients: a Retrospective Cohort Study. Antibiotics. 2024;13(3):287. doi:10.3390/antibiotics13030287
- Katip W, Rayanakorn A, Oberdorfer P, et al. Comparative effectiveness and mortality of colistin monotherapy versus colistin-fosfomycin combination therapy for the treatment of carbapenem-resistant Enterobacteriaceae (CRE) infections: a propensity score analysis. J Infect Public Health. 2024;17(5):727–734. doi:10.1016/j.jiph.2024.03.010
- Katip W, Rayanakorn A, Oberdorfer P, et al. Short versus long course of colistin treatment for carbapenem-resistant A. baumannii in critically ill patients: a propensity score matching study. J Infect Public Health. 2023;16(8):1249–1255. doi:10.1016/j.jiph.2023.05.024
- Hsu MS, Liao CH, Huang YT, et al. Clinical features, antimicrobial susceptibilities, and outcomes of Elizabethkingia meningoseptica (Chryseobacterium meningosepticum) bacteremia at a medical center in Taiwan, 1999–2006. Eur J Clin Microbiol Infect Dis. 2011;30(10):1271–1278. doi:10.1007/s10096-011-1223-0
- Wisconsin Department of Health Services. Elizabethkingia. Available from: https://www.dhs.wisconsin.gov/disease/elizabethkingia.htm. Accessed July 25, 2023.
- López-Otín C, Blasco MA, Partridge L, et al. The Hallmarks of Aging. Cell. 2013;153(6):1194–1217. doi:10.1016/j.cell.2013.05.039
- Fulop T, Larbi A, Dupuis G, et al. Immunosenescence and Inflamm-Aging As Two Sides of the Same Coin: friends or Foes? Front Immunol. 2018;8:1960. doi:10.3389/fimmu.2017.01960
- Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive Value of Sequential Organ Failure Assessment, Quick Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation II, and New Early Warning Signs Scores Estimate Mortality of COVID-19 Patients Requiring Intensive Care Unit. Indian. J Crit Care Med. 2022;26(4):464–471. doi:10.5005/jp-journals-10071-24170
- Bihari S, Bannard-Smith J, Bellomo R. Albumin as a drug: its biological effects beyond volume expansion. Crit Care Resusc. 2020;22(3):257–265. doi:10.1016/S1441-2772(23)00394-0
- Manolis AA, Manolis TA, Melita H, et al. Low serum albumin: a neglected predictor in patients with cardiovascular disease. Eur. J Intern Med. 2022;102:24–39. doi:10.1016/j.ejim.2022.05.004
- Xu T, Liu W, Huang R. Can albumin reduce the mortality of patients with cirrhosis and ascites? A meta-analysis of randomized controlled trials. Eur. J Gastroenterol Hepatol. 2023;35(1):80–88. doi:10.1097/MEG.0000000000002447
- Lin JN, Lai CH, Yang CH, et al. Elizabethkingia Infections in Humans: from Genomics to Clinics. Microorganisms. 2019;7(9):295. doi:10.3390/microorganisms7090295
- Santona A, Paglietti B, Al-Qahtani AA, et al. Novel type of VanB2 teicoplanin-resistant hospital-associated Enterococcus faecium. Int J Antimicrob Agents. 2014;44(2):156–159. doi:10.1016/j.ijantimicag.2014.05.005
- Lin JN, Lai CH, Yang CH, et al. Genomic features, phylogenetic relationships, and comparative genomics of Elizabethkingia anophelis strain EM361-97 isolated in Taiwan. Sci Rep. 2017;7(1):14317. doi:10.1038/s41598-017-14841-8
- Huang YC, Lin YT, Wang FD. Comparison of the therapeutic efficacy of fluoroquinolone and non-fluoroquinolone treatment in patients with Elizabethkingia meningoseptica bacteraemia. Int J Antimicrob Agents. 2018;51(1):47–51. doi:10.1016/j.ijantimicag.2017.05.018
- Rice LB. Mechanisms of Resistance and Clinical Relevance of Resistance to β-Lactams, Glycopeptides, and Fluoroquinolones. Mayo Clin Proc. 2012;87(2):198–208. doi:10.1016/j.mayocp.2011.12.003