Abstract
Syphilis is a complex, systemic infectious disease caused by Treponema pallidum subspecies pallidum. Secondary syphilitic lesions typically manifest within 3 months following initial exposure to T. pallidum. The predominant cutaneous manifestations of secondary syphilis are macula and papule. Certain individuals with syphilis may present with an atypical rash during the secondary stage owing to immunosuppression and other factors. Herein, we report a rare case of atypical recurrent secondary syphilis around the anus in a 65-year-old woman. Based on cerebrospinal fluid findings and skin biopsy results, the patient was ultimately diagnosed as neurosyphilis and recurrent secondary syphilis. Following intravenous antibiotic therapy, the patient’s rash improved significantly. This case underscores the importance for physicians to remain vigilant regarding the possibility of syphilis when encountering cases exhibiting unusual clinical manifestations, as a definitive diagnosis necessitates a comprehensive evaluation.
Introduction
Syphilis is a sexually transmitted disease caused by Treponema pallidum (T. pallidum), which can affect the skin and mucosa. Secondary syphilitic lesions usually manifest within 3 months after the initial exposure to T. pallidum. The symptoms of secondary syphilis may naturally resolve after 3–12 weeks without treatment, leading to a latent state known as latent syphilis. Although no clinical symptoms are present during this stage, spirochetes remain hidden in certain organs, nervous system or lymphatic system. In specific cases, symptoms reappear and become secondary recurrent syphilis, which can occur several times. Approximately 25% of patients experience relapses, of which 2/3 occur within 6 months. The recurrence rate within one year is 90%, and within two years it reaches 95%. Although serological relapse is relatively common, clinical relapse is infrequent in the penicillin era.Citation1 Distinguishing between relapse and reinfection can be challenging in clinical practice. The most frequent skin manifestations of secondary syphilis are macular and papular eruptions. However, other uncommon lesions, such as nodular, pustular, arcuate, follicular, and psoriasis-like lesions, have been occasionally reported.Citation2 Annular syphilid frequently occurs on the scalp, face, palm, sole, intertriginous and genital regions. Perianal annular syphilid is rare, and differential diagnosis should be made from granuloma annulare, cutaneous tuberculosis, contact dermatitis, and dermatophytosis.Citation3 Here we report a case of atypical recurrent secondary syphilis around the anus.
Case Presentation
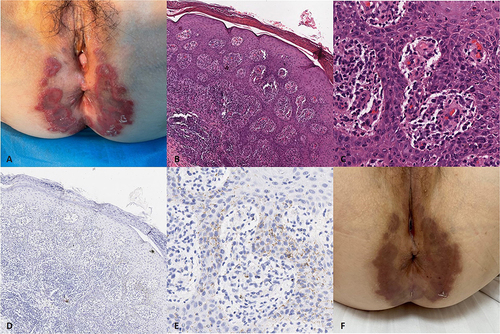
A 65-year-old woman presented with non-pruritic and painless red annular patches and plaques on her crissum that had appeared three months prior. Physical examination revealed patchy erythema of varying sizes around the anus, with circular raised plaques at the edges, and a few white scales overlying them (). No other skin or mucosal lesions or lymphadenopathy were observed. Microscopic examination and fungal cultures yielded negative results. Chest computed tomography showed old tuberculosis foci in both the upper lung lobes. Tumor indicators, autoantibodies, immunoglobulin levels, complement levels, and other indicators showed no significant abnormalities. Flow cytometry demonstrated lower than normal reference values for the total T, B, and NK cells. The CD4 T cell count was reduced to 213 cells/µL, and the CD4/CD8 ratio was 0.8. Further serum examinations showed TPPA was positive, and TRUST revealed a titer of 1:128. Human immunodeficiency virus (HIV) test result was negative. Tests for other sexually transmitted diseases such as mycoplasma, chlamydia, gonococcal, and human papillomavirus (HPV) infections were negative. Histopathological examination of the skin lesion revealed parakeratosis, epidermal hyperplasia, and a dense band of inflammatory cells in the lower part of the epidermis and dermo-epidermal junction, mainly lymphocytes and plasma cells ( and ). Immunohistochemical staining for T. pallidum confirmed positivity ( and ). PAS staining and acid-fast staining results were negative. To assess nervous system involvement, a lumbar puncture was performed to analyze cerebrospinal fluid, which revealed a VDRL titer of 1:16, along with elevated white blood cell count and total protein levels compared to normal reference values. Therefore, she was diagnosed with ”neurosyphilis and secondary syphilis, and administered 4 million U of benzylpenicillin sodium intravenously every four hours for 14 days. After two weeks of intravenous penicillin treatment, the perianal rash subsided, leaving pigmentation ().
Figure 1 (A) Red ring plaque around the patient’s anus. (B and C) Histopathological examination of the red patches of skin with ridges at the edges showed parakeratosis, epidermal hyperplasia, and a dense band of inflammatory cells, mainly lymphocytes and plasma cells, at the junction between the lower epidermal process and the true epidermis.(hematoxylin-eosin staining, original magnification X50, X200, respectively). (D and E) Immunohistochemical staining showing numerous spirochetes in the lower part of the epidermis (Immunostain spirochete stain, original magnification X50, X200, respectively) (F) After 2 weeks of penicillin intravenous treatment, the perianal rash subsided than before, leaving pigmentation.
Discussion
Syphilis shows a rapid and system-wide vasculitis caused by endothelial invasion of T. pallidum.Citation4 This vasculitis and systemic spread occur rapidly after primary infection and mark the beginning of the stage known as secondary syphilis. The most common manifestation at this stage is a generalized macular and papulosquamous eruption accompanied by palmar-plantar and mucosal involvement. The rash is typically described as macular and popular; however, atypical cutaneous manifestations are more prevalent than previously assumed, including annular, nodular, pustular, crusted necrotic, nodular-ulcerative (malignant), folliculitis, corymbiform, vitiligo-like rashes, psoriasiform rashes, persistent chancre during the secondary stage, and multiple anogenital lesions.Citation5,Citation6 Syphilis has historically been known as a great imitator with a diverse range of clinical presentations described above. Due to the diversity of potential cutaneous presentations of secondary syphilis, clinical diagnosis can be very challenging.Citation7 Serological tests or direct detection methods such as immunohistochemistry or Warthin Starry staining can be used for the clinical diagnosis of secondary syphilis regardless of the typicality of the rash presentation. Immunohistochemistry demonstrated higher sensitivity and specificity than Warthin Starry stain for diagnosing secondary syphilis. Neurosyphilis is a severe consequence of syphilis and can occur at any stage of infection, even in the earliest stage.Citation8 Diagnosis of neurosyphilis relies on complex cerebrospinal fluid (CSF) tests, with CSF-VDRL being the standard diagnostic test currently employed.Citation9 Our previous study revealed that 23.76% of secondary syphilis patients had detectable CSF abnormalities and 13.12% of secondary syphilis patients had positive CSF-VDRL.Citation10 It can be seen that the prevalence of neurosyphilis in patients with secondary syphilis occupies a certain proportion.
Our patient presented with red annular patches surrounding the anus and was previously diagnosed with genital herpes and skin infection. She was subsequently treated with oral antiviral drugs, antihistamines, topical antimicrobial agents, and glucocorticoid ointment; however, the rash did not improve. Upon further inquiry, she was admitted with a history of rash on the trunk, which was diagnosed as secondary syphilis two years ago. The patient was treated with benzathine penicillin G, 2.4 million units by intramuscular injection once a week for three consecutive weeks, with no follow-up after treatment. Simultaneously, her spouse, who engaged in extramarital sexual activity, was diagnosed with secondary syphilis too. The recent studies cited found that atypical manifestations of syphilis were statistically correlated with syphilis reinfection, especially annular lesions.Citation11,Citation12 Moreover, the presence of atypical manifestations of syphilis could be related to the circulation of different strains of T. pallidum.Citation13 The possibility of recurrent rash as reinfection of T. pallidum was considered based on our patient’s previous infection treatment and the medical history of her sexual partner. However, during the subsequent history taking, the patient asserts that she had been in a monogamous relationship for the past 40 years and denied any sexual contact for nearly two years after diagnosis as secondary syphilis which ruled out reinfection. Why does it relapse? The reasons for this relapse can be attributed to nervous system involvement in syphilis infections. When the immune system is compromised or considered defective, T. pallidum present in the nervous system re-enters the bloodstream circulation, leading to recurrence of the secondary syphilitic rash. Evidence supporting immune dysfunction includes decreased levels of T cells, B cells, and NK cells and a decline in the CD4/CD8 ratio, which results in a poor response to immunization and increases susceptibility to severe infections.Citation14,Citation15
Conclusion
In conclusion, determining the diagnosis for this patient requires combining information regarding sexual activity history, clinical manifestations, serological tests for syphilis, histopathological examination, and cerebrospinal fluid analysis due to its unusual and atypical presentations, making it challenging to diagnose. Due to its atypical and distinctive manifestations, syphilis poses a diagnostic challenge, necessitating physicians’ vigilance in considering the possibility of syphilis in cases involving the anal region that lack typical features, thereby requiring further investigation and laboratory tests.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of the Shanghai Skin Disease Hospital. Written informed consent for publication of her images and other clinical information were obtained from the patient. The authors confirm that our study complies with the Declaration of Helsinki.
Disclosure
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Acknowledgments
The authors thank the patient for her cooperation in the diagnostic process.
Additional information
Funding
References
- Myint M, Bashiri H, Harrington RD, Marra CM. Relapse of secondary syphilis after benzathine penicillin G: molecular analysis. Sex Transm Dis. 2004;31(3):196–199. doi:10.1097/01.OLQ.0000114941.37942.4C
- Li F, Wang T, Wang L. Secondary syphilis primarily presenting with multiple nodules on the scalp: case report and published work review. J Dermatol. 2017;44(12):1401–1403. doi:10.1111/1346-8138.13965
- Li FG, Huang WB, Chen HS, Wang T, Fan YM. Clinicopathological, dermoscopic, and ultrastructural observation of annular secondary syphilis on the penis. Int J STD AIDS. 2020;31(7):699–701. doi:10.1177/0956462419900092
- Thomas DD, Navab M, Haake DA, Fogelman AM, Miller JN, Lovett MA. Treponema pallidum invades intercellular junctions of endothelial cell monolayers. Proc Natl Acad Sci U S A. 1988;85(10):3608–3612. doi:10.1073/pnas.85.10.3608
- Balagula Y, Mattei PL, Wisco OJ, Erdag G, Chien AL. The great imitator revisited: the spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol. 2014;53(12):1434–1441. doi:10.1111/ijd.12518
- Wöhrl S, Geusau A. Clinical update: syphilis in adults. Lancet. 2007;369(9577):1912–1914. doi:10.1016/S0140-6736(07)60895-2
- Lautenschlager S. Cutaneous manifestations of syphilis: recognition and management. Am J Clin Dermatol. 2006;7(5):291–304. doi:10.2165/00128071-200607050-00003
- Marra CM. Update on neurosyphilis. Curr Infect Dis Rep. 2009;11(2):127–134. doi:10.1007/s11908-009-0019-1
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1–187. doi:10.15585/mmwr.rr7004a1
- Shi M, Peng RR, Gao Z, et al. Risk profiles of neurosyphilis in HIV-negative patients with primary, secondary and latent syphilis: implications for clinical intervention. J Eur Acad Dermatol Venereol. 2016;30(4):659–666. doi:10.1111/jdv.13514
- Parodi M, Ciccarese G, Drago F, et al. Annular and arciform lesions of the palms as unique manifestations of secondary syphilis. Int J STD AIDS. 2020;31(13):1323–1326. doi:10.1177/0956462420948354
- Ciccarese G, Facciorusso A, Mastrolonardo M, Herzum A, Parodi A, Drago F. Atypical manifestations of syphilis: a 10-year retrospective study. J Clin Med. 2024;13(6):1603. doi:10.3390/jcm13061603
- Lieberman N, Lin MJ, Xie H, et al. Treponema pallidum genome sequencing from six continents reveals variability in vaccine candidate genes and dominance of Nichols clade strains in Madagascar. PLoS Negl Trop Dis. 2021;15(12):e0010063. doi:10.1371/journal.pntd.0010063
- Bruno G, Saracino A, Monno L, Angarano G. The revival of an “old” marker: CD4/CD8 ratio. AIDS Rev. 2017;19(2):81–88.
- Serrano-Villar S, Moreno S, Fuentes-Ferrer M, et al. The CD4:CD8 ratio is associated with markers of age-associated disease in virally suppressed HIV-infected patients with immunological recovery. HIV Med. 2014;15(1):40–49. doi:10.1111/hiv.12081
