Abstract
Objective
Klebsiella pneumoniae liver abscess (KPLA) is an invasive infectious disease with a considerable prevalence and complications. This study aimed to determine the predicted value of aspartate aminotransferase-to-platelet ratio index (APRI) and fibrosis-4 index (FIB-4) for positive blood cultures and sepsis in patients with KPLA.
Methods
We evaluated 248 consecutive participants diagnosed with KPLA. Demographic characteristics, clinical features, and laboratory test results of the participants were recorded. Multivariate logistic regression analysis was performed to identify the risk factors. Receiver operating characteristic (ROC) analyses were conducted to evaluate the discriminatory ability of APRI and FIB-4.
Results
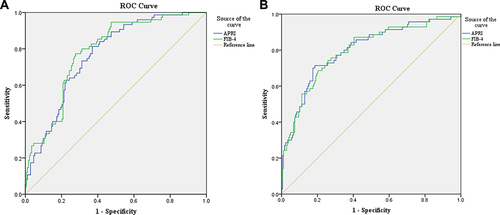
30.2% (75 of 248) KPLA patients presented with positive blood cultures, and 70 (28.2%) developed sepsis. Among the positive blood culture and sepsis groups, the APRI and FIB-4 showed statistically significant increases. Multivariate analysis showed that APRI (odds ratio [OR] = 1.190, 95% confidence interval [CI] 1.051–1.347, p = 0.006) and FIB-4 (OR = 1.110, 95% CI 1.046–1.179, p = 0.001) were independent prognostic factors for positive blood cultures. Both APRI (OR = 1.505, 95% CI 1.149-1.988, p = 0.004) and FIB-4 (OR = 1.187, 95% CI 1.054-1.336, p = 0.005) were independent risk factors for sepsis. The area under the ROC curve (AUC) of APRI and FIB-4 for predicting positive blood cultures of KPLA was 0.783 and 0.766, respectively. APRI had an AUC of 0.801, with a sensitivity and specificity of 71.4% and 81.5%, respectively, for predicting sepsis in patients with KPLA, and the prediction performance of APRI was better than that of FIB-4 (AUC = 0.798).
Conclusion
In our study, APRI and FIB-4 are effective methods for predicting KPLA patients with positive blood cultures and sepsis.
Introduction
Pyogenic liver abscess (PLA) is a common infectious disease of the digestive system that is caused by various pathogens. Klebsiella pneumoniae is the most common pathogen causing liver abscesses in East Asian countries, especially China and Korea.Citation1,Citation2 In the past 3 decades, there has been increasing evidence of KPLA, which has gained more and more clinical attention.Citation3,Citation4 KPLA is prevalent in diabetic patients and can cause extrahepatic metastatic complications such as sepsis, meningitis, endophthalmitis, and necrotizing fasciitis.Citation5,Citation6 Although the mortality rate of KPLA has decreased in recent years (from 3.5–20% to 2.8–10.8%), recent studies have shown that eye or neurological complications caused by KPLA could lead to unfavorable prognoses.Citation7 Therefore, development of reliable and convenient predictive tools is crucial.
The acute phase of PLA, accompanied by elevated levels of inflammatory markers, such as C-reactive protein (CRP) and procalcitonin (PCT), has been thoroughly studied. Compared with culture-negative PLA, culture-positive PLA presented more serious clinical characteristics.Citation8 However, new biomarkers need to be explored. Noninvasive liver fibrosis scores, including the APRI and FIB-4, have traditionally been used to assess the presence and severity of liver damage and fibrosis. Studies have indicated that APRI and FIB-4 have potential predictive values in the prognosis of many diseases, including non-infectious and infectious diseases.Citation9,Citation10 Recent evidence indicates that liver fibrosis scores can predict the risks of cardiovascular mortality in coronary artery disease.Citation9 A previous study indicated that the APRI can accurately and effectively predict the occurrence of sepsis-related liver injury.Citation10 FIB-4 levels have also been associated with cardiovascular disease severity in patients with metabolic dysfunction-associated fatty liver disease.Citation11
To date, there have been few studies on the association between liver fibrosis scores and prognosis in patients with KPLA. Therefore, in this study, we aimed to assess whether APRI and FIB-4 can be used as predictors of positive blood cultures and sepsis in patients with KPLA.
Material and Methods
Study Population
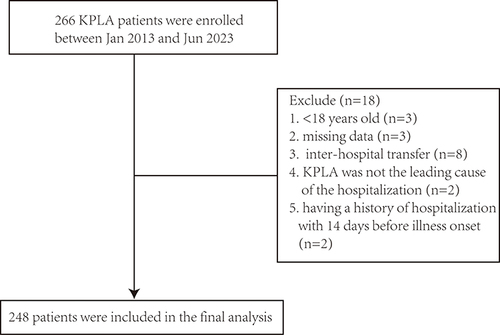
Patients admitted to Taizhou Hospital of Zhejiang Province and diagnosed with PLA were recruited between January 2013 and June 2023. The clinical diagnosis of PLA was based on the International Classification of Diseases, Clinical Modification 572.0. Patients who were identified with KPLA met the following criteria: (1) clinical symptoms, such as fever, chills, right upper abdominal pain, abdominal imaging showing liver abscess, and (2) Klebsiella pneumoniae bacterial cultures of blood or pus was Klebsiella pneumoniae. Patients were excluded: (1) age <18 years, (2) missing medical treatment data, (3) diagnosis of liver abscess as a complication (). The clinical definition of positive blood culture included microbial growth within 72 h of admission.Citation12 Sepsis was defined according to the Sepsis-3.0 criteria.Citation13 This study was approved by the Institutional Medical Ethics Committee of Taizhou Hospital of Zhejiang Province.
Microbiologic Data
Blood cultures were obtained within 24 h of admission and pus cultures were obtained using puncture-guided ultrasound. Blood cultures were incubated in the BacT/Alert (bioMeìrieux, France) system. Identifications and antimicrobial drug susceptibility of K. pneumoniae were used by VITEK 2 compact system (bioMeìrieux Vitek Inc., France). Clinical and Laboratory Standards Institute (CLSI) breakpoints were used to interpret antimicrobial susceptibility.
Data Collection
The clinical characteristics of all the included patients were retrospectively obtained from their electronic medical records. The researchers collected demographic (age and sex) and medical data, including clinical symptoms, complications, laboratory blood test data, treatment methods, antibiotic use, and clinical outcomes. 10mL of venous blood was collected within 24 h of admission. Routine blood tests were performed using BC-6800 plus an automatic blood cell counter (Mindray, China). Blood biochemical parameters were measured using an AU5800 automatic biochemical analyzer (Beckman Coulter, USA). PCT levels were quantified using Roche E801 (Roche, Switzerland). Coagulation was performed using a Fibrintimer II coagulometer and Multifibren U Kit (Stago, France).
The formulas for calculating the liver fibrosis scores are as follows:Citation14
The upper limit normal of AST was 40 U/L in our hospital.
Statistical Analysis
Categorical variables are presented as frequencies and percentages, and non-normally distributed variables are presented as medians (interquartile range, IQR). Categorical variables were compared using the chi-square test or Fisher’s exact test, whereas non-normally distributed variables were compared using the Mann–Whitney U-test. The variables of the univariate analysis with p < 0.1 were imported into the multivariate logistic regression model to screen for potential risk factors. ROC curves were plotted to predict the efficacy of the liver fibrosis scores. The optimal cut-off values were assessed using the Youden index. Statistical analyses were performed by using SPSS 23.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at p < 0.05.
Results
The baseline characteristics of the patients are summarized in . Among the 248 eligible patients, the median (IQR) age was 62.0(53.0-71.0) years, and male patients accounted for 63.7% (158/248). On bacteriologic analysis, blood cultures were obtained in 75 patients, with a positive culture rate of 30.2% and a positive pus culture rate of 83.1% (206/248). The most common comorbidity in the patients with KPLA was diabetes mellitus (n=120, 48.4%), followed by hypertension (n=97, 39.1%). Additionally, 70 patients (28.2%) developed sepsis and 29 patients (11.7%) developed metastatic infections. Eventually, four patients had a poor prognosis.
Table 1 Participant Characteristics for KPLA Patients
The basic characteristics of the study groups are shown in . No differences were found in age, sex, body mass index, or symptoms between the positive and negative blood culture groups. There was a higher proportion of various underlying diseases such as chronic renal insufficiency, malignant tumors, and liver insufficiency (p < 0.05) in the positive blood culture group. Additionally, compared to the negative blood culture group, the positive blood culture group had a higher proportion of patients with a history of surgical surgery. Sepsis was associated with older age and higher BMI index. In addition, patients with sepsis showed higher rates of chronic renal insufficiency, liver insufficiency, vomiting, frailty, and diarrhea.
Table 2 Demographic Characteristics of KPLA Patients with Positive Blood Culture and Sepsis
A comparative analysis of laboratory parameters between the different groups is presented in . PLT, blood urea nitrogen (BUN), creatinine (Cr), ALT, AST, total bile acid (TBA), CRP, PCT, APRI, and FIB-4 levels in patients with positive blood cultures were significantly higher than those in patients with negative blood cultures. By contrast, patients with positive blood culture results had significantly lower albumin (ALB) levels. Compared to the non-sepsis group, the sepsis group had higher levels of BUN, Cr, ALT, AST, total bilirubin (TBIL), TBA, CRP, PCT, APRI, and FIB-4 and lower levels of PLT and ALB.
Table 3 Laboratory findings of KPLA Patients with Positive Blood Culture and Sepsis
Variables with significant differences (p < 0.1) in the univariate analysis, including age, sex, BMI, and comorbidities, were included in the binary regression analysis model. Multivariate analysis suggested that the APRI (OR = 1.190, 95% CI 1.051–1.347, p= 0.006) and FIB-4 (OR = 1.110, 95% CI 1.046–1.179, p = 0.001) were significant independent variables for the prediction of positive blood cultures (). In addition, APRI (OR = 1.505, 95% CI 1.149-1.988, p = 0.004) and FIB-4 (OR = 1.187, 95% CI 1.054-1.336, p = 0.005) were independently associated with KLPA in patients with sepsis.
Table 4 Univariable and Multivariate Analysis for KPLA Patients with Positive Blood Culture and Sepsis
In the ROC analysis, the AUC of FIB-4 was 0.783(95% CI 0.724-0.842, cut-off point: 2.9), which was higher than that of the APRI 0.766 (95% CI 0.706-0.826, cut-off value: 0.7) between the positive and negative blood culture groups (, ). Between patients with and without sepsis, the APRI cut-off was 1.4, AUC 0.801(0.738-0.865) (p<0.001), and the FIB-4 cut-off was 3.3, AUC 0.798 (0.734-0.862) (p <0.001).
Table 5 Diagnostic Value of APRI for KPLA Patients with Positive Blood Culture and Sepsis
Discussion
KPLA is a life-threatening, invasive liver abscess. Approximately 20% of KPLA cases are complicated by extrahepatic metastatic infections.Citation15 Studies have shown that non-liquefied KPLA is prone to septic shock, which may eventually lead to multiple organ failure and be life-threatening.Citation16 To data, there are few clinical studies on KPLA and sepsis. Based on our previous research findings, KPLA patients with sepsis have higher rates of complications and metastatic infections.Citation3 Early warning biomarkers are essential for timely management of patients with KPLA to prevent the progression of metastatic infections. To our knowledge, this study is the first to demonstrate an association between liver fibrosis score and KPLA.
In our study, 248 KPLA patients were divided into positive and negative blood cultures, as well as sepsis and non-sepsis groups. On comparing the basic characteristics, the proportion of liver and kidney dysfunction in patients with positive blood cultures was significantly higher than that in the negative group. Similar results were observed for the sepsis group. Moreover, we found that higher values of AST, ALT, ALB, BUN, and Cr in patients with KPLA were associated with poor prognosis. Consistent with other studies,Citation17 the results showed that among patients with KPLA, those with liver and kidney dysfunction were more likely to develop bacteremia and sepsis.
A recent study revealed that diabetic patients are more likely to develop liver fibrosis.Citation18 Our results showed that the most common underlying disease was diabetes mellitus, accounting for 50.7% and 50.0% of the blood culture-positive and sepsis groups, respectively. Insulin regulates glucose intake in the liver. However, in patients with diabetes mellitus, insulin resistance can lead to lipid accumulation in the liver and abnormal glucose regulation, eventually resulting in liver fibrosis. Our findings suggest that patients with KPLA and diabetes should be promptly identified and treated accordingly.
The APRI and FIB-4 are widely used to assess liver injury and fibrosis. They included four variables: age, ALT, AST, and PLT levels. Hepatocyte damage caused by a liver abscess can lead to an increase in transaminase (especially AST and ALT) levels, and its high concentration may indicate necrosis or swelling of the liver. In infectious diseases, platelets are the major inflammatory effector cells, and bacteria can help platelets adhere or promote platelet aggregation.Citation19 Decreased PLT levels are early prognostic indicators of disease severity. Further evaluation demonstrated that high APRI and FIB-4 levels were independent risk factors for KPLA patients with positive blood cultures and sepsis. Non-invasive liver fibrosis scoring systems have also recently been reported to have a predictive value for adverse outcomes in patients with other non-liver diseases. A previous study by Dou et al reported that increased APRI predicts the development of sepsis-associated liver injury in children.Citation20 He et al showed that the APRI on admission had predictive value in patients with hemorrhagic fever and renal syndrome.Citation21 Xiong et al suggested that the liver fibrosis score (FIB-4 and APRI) could predict the risk of cardiovascular disease (CVD) in a hypertensive population.Citation22
A recent study showed that sepsis patients with positive blood cultures had a higher severity of illness and mortality.Citation12 In the liver, it is very important to regulate immune defense through mechanisms such as bacterial clearance, production of acute-phase proteins or cytokines, and metabolic adaptation to inflammation. Nevertheless, the liver is also a target of sepsis-related injuries.Citation23 Sepsis manifests as liver dysfunction. A positive blood culture in patients with KPLA indicates the presence of bacteria in the bloodstream. This finding also indicates an increased risk of sepsis. In this study, 40 of 75 patients with KPLA with positive blood cultures developed sepsis. Our findings demonstrated that APRI and FIB-4 had predictive values in patients with KPLA with positive blood cultures and sepsis. In this study, for positive blood culture KPLA, the AUC of FIB-4 was 0.783 compared to 0.766 for APRI. In the present study, it showed that APRI≥0.7 and FIB-4≥2.9 were independently associated with positive blood culture, respectively. The optimal cutoff values for APRI and FIB-4 in predicting sepsis among KPLA population was 1.4 and 3.3, respectively. However, APRI was better than FIB-4 in predicting early stage of sepsis. Therefore, we recommend routine APRI and FIB-4 tests as promising tools for positive blood culture and sepsis in patients with KPLA to enable timely and effective management.
This study had several limitations. First, this was a single-center study, and bias could arise from the small sample size and the selection criteria. Large-sample multicenter studies on KPLA should be conducted in the future. Secondly, some patients were transferred from other hospitals and had a history of antibiotic use. The early use of antibiotics reduced the sensitivity of blood culture-positive detection.
Conclusion
In summary, a high proportion of patients with KPLA had positive blood cultures and sepsis. We provided evidence for significant associations between APRI, FIB-4, positive blood culture, and sepsis in patients with KPLA. Our results validated that the APRI and FIB-4 are useful predictive factors for patients with KPLA patients with positive blood cultures and sepsis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Ethics approval and consent to participate
The Institutional Medical Ethics Committee of Taizhou Hospital of Zhejiang Province granted approval for this retrospective study, and informed consent was waived because the medical records of the subjects were de-identified from the Medical Records and Statistics Room to ensure patient confidentiality. The study was conducted in accordance with the guiding principles of the Declaration of Helsinki.
Disclosure
The authors declare no competing interests.
Data Sharing Statement
The datasets analyzed in this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Luo M, Yang XX, Tan B, et al. Distribution of common pathogens in patients with pyogenic liver abscess in China: a meta-analysis. Eur J Clin Microbiol Infect Dis. 2016;35(10):1557–1565. doi:10.1007/s10096-016-2712-y
- Chung DR, Lee SS, Lee HR, et al. Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea. J Infect. 2007;54(6):578–583. doi:10.1016/j.jinf.2006.11.008
- Li SX, Yu SF, Peng MF, et al. Clinical features and development of Sepsis in Klebsiella pneumoniae infected liver abscess patients: a retrospective analysis of 135 cases. BMC Infect Dis. 2021;21(1):597. doi:10.1186/s12879-021-06325-y
- Feng CY, Di J, Jiang SF, et al. Machine learning models for prediction of invasion Klebsiella pneumoniae liver abscess syndrome in diabetes mellitus: a singled centered retrospective study. BMC Infect Dis. 2023;23(1):284. doi:10.1186/s12879-023-08235-7
- Lee SS, Chen YS, Tsai HC, et al. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 2008;47(5):642–650. doi:10.1086/590932
- Siu LK, Yeh KM, Lin JC, et al. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis. 2012;12(11):881–887. doi:10.1016/S1473-3099(12)70205-0
- Lin YT, Wang FD, Wu PF, et al. Klebsiella pneumoniae liver abscess in diabetic patients_ association of glycemic control with the clinical characteristics. BMC Infect Dis. 2013;13:56. doi:10.1186/1471-2334-13-56
- Yao L, Liu JQ, Fu L, et al. Demographics and Clinical Outcomes of Culture-Positive versus Culture-Negative Pyogenic Liver Abscess in an Asian Population. Infect Drug Resist. 2023;16:903–911. doi:10.2147/IDR.S395428
- Jin JL, Zhang HW, Cao YX, et al. Liver fibrosis scores and coronary atherosclerosis: novel findings in patients with stable coronary artery disease. Hepatol Int. 2021;15(2):413–423. doi:10.1007/s12072-021-10167-w
- Xie TH, Xin Q, Cao XR, et al. Clinical characteristics and construction of a predictive model for patients with sepsis related liver injury. Clin Chim Acta. 2022;537:80–86. doi:10.1016/j.cca.2022.10.004
- Lu C, Chen Y, Zhang Y, et al. Liver Fibrosis Scores and Coronary Artery Disease: Novel Findings in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease. Diabetes Metab Syndr Obes. 2023;16:2627–2637. doi:10.2147/DMSO.S426102
- Lal A, Rayes H, O’Horo JC, et al. Septic shock definitions and associated outcomes in blood culture positive critically ill patients. Ann Transl Med. 2023;11(5):192. doi:10.21037/atm-22-5147
- Singer M, Deutschman C, Seymour C, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
- Sterling RK, King WC, Wahed AS, et al. Evaluating Noninvasive Markers to Identify Advanced Fibrosis by Liver Biopsy in HBV/HIV Co-infected Adults. Hepatology. 2020;71(2):411–421. doi:10.1002/hep.30825
- Wang HR, Guo YW, Liu ZY, et al. The Type VI Secretion System Contributes to the Invasiveness of Liver Abscess Caused by Klebsiella pneumoniae. J Infect Dis. 2023;228(8):1127–1136. doi:10.1093/infdis/jiad166
- Lee YT, Wang CC, Li CF, et al. Utility of Acute Physiology and Chronic Health Evaluation (APACHE II) in Predicting Mortality in Patients with Pyogenic Liver Abscess: A Retrospective Study. J Clin Med. 2021;10(12):2644. doi:10.3390/jcm10122644
- Zhang SQ, Zhang XC, Wu Q, et al. Clinical, microbiological, and molecular epidemiological characteristics of Klebsiella pneumoniae-induced pyogenic liver abscess in southeastern China. Antimicrob Resist Infect Control. 2019;8:166. doi:10.1186/s13756-019-0615-2
- Guan LH, Li L, Zou YT, et al. Association between FIB-4, all-cause mortality, cardiovascular mortality, and cardiovascular disease risk among diabetic individuals: NHANES 1999-2008. Front Cardiovasc Med. 2023;10:1172178. doi:10.3389/fcvm.2023.1172178
- Dib P, Quirino-Teixeira A, Merij L, et al. Innate immune receptors in platelets and platelet-leukocyte interactions. J Leukoc Biol. 2020;108(4):1157–1182. doi:10.1002/JLB.4MR0620-701R
- Dou JY, Zhou YP, Cui Y, et al. AST-to-Platelet Ratio Index as Potential Early-Warning Biomarker for Sepsis-Associated Liver Injury in Children: A Database Study. Front Pediatr. 2019;7:331. doi:10.3389/fped.2019.00331
- He S, Han QY, Wang XY, et al. Aspartate aminotransferase to platelet ratio at admission can predict the prognosis of patients with hemorrhagic fever with renal syndrome. J Med Virol. 2023;95(10):e29126. doi:10.1002/jmv.29126
- Xiong SJ, Yin SZ, Deng WS, et al. Predictive value of liver fibrosis scores in cardiovascular diseases among hypertensive population. J Hypertens. 2023;41(5):741–750. doi:10.1097/HJH.0000000000003394
- Strnad P, Tacke F, Koch A, et al. Liver - guardian, modifier and target of sepsis. Nat Rev Gastroenterol Hepatol. 2017;14(1):55–66. doi:10.1038/nrgastro.2016.168