Abstract
Background
Nontyphoidal Salmonella (NTS) species are important food-borne pathogens that cause gastroenteritis and bacteremia, and are responsible for a huge global burden of morbidity and mortality. The aim of this study was to investigate the prevalent serogroups and antibiotic resistance of NTS in our region.
Methods
We reviewed the serogroup distribution and antimicrobial susceptibility patterns of NTS strains obtained from 158 stool specimens of patients with acute diarrheal infection attending the outpatient and inpatient department at a university hospital in the Eastern Province of Saudi Arabia in the period from September, 2008 to April, 2011. A retrospective analysis of the 158 patients with NTS infection was conducted to determine the most prevalent NTS serogroups causing acute gastroenteritis and their antimicrobial susceptibility patterns.
Results
At this teaching hospital, a total of 17,436 fecal samples were analyzed during the 2008–2011 study period. Of these specimens, 158 tested positive for NTS, giving an overall prevalence of 9.06 per 1,000. Of 158 NTS cases, serogroup D1 (25.3%) was the most prevalent, followed by serogroup B (19.6%), and serogroup C1 (18.9). One third of all NTS serogroup strains tested were resistant to tetracycline. The NTS strains showed resistance to ampicillin (31.3%), amoxicillin/clavulanic acid (29.9%), trimethoprim/sulfamethoxazole (20.9%), and cefotaxime (14.93%).
Conclusion
The findings of this study support the concern that use of antibiotics in animal feeds may contribute to acquisition of resistance in food-borne bacteria, such as Salmonella. Our study also concludes that the prevalence of NTS in the Eastern Province of Saudi Arabia is very low compared with other studies worldwide.
Introduction
Salmonella are motile Gram-negative facultative anaerobic bacteria in the family Enterobacteriaceae. The Salmonella genus consists of two species, ie, Salmonella enterica and Salmonella bongori.Citation1 Most pathogenic species of Salmonella causing illness in humans belong to the S. enterica species.Citation2 This species is further divided into six subspecies, ie, S. enterica subspecies enterica, S. enterica subspecies salamae, S. enterica subspecies arizonae, S. enterica subspecies diarizonae, S. enterica subspecies houtenae, and S. enterica subspecies indica. Nontyphoidal salmonellosis is caused by Salmonella species other than Salmonella typhi and Salmonella paratyphi. Nontyphoidal salmonellosis is one of the leading food-borne illnesses and accounts for considerable morbidity and mortality in both developed and developing countries. For instance, in the US, it was estimated that nontyphoidal salmonellosis accounted for 11% (rank number two) of food-borne illnesses, 35% (rank number one) of food borne-associated hospitalization, and 28% (rank number one) of foodborne-associated death.Citation3,Citation4
Nontyphoidal Salmonella (NTS) is recognized as one of the principal causes of food-borne infections worldwide.Citation5 Among the more than 2,000 Salmonella serovars, Enteritidis is one of the top serovars reported in Saudi Arabia.Citation6 Most cases of gastroenteritis caused by serovar Enteritidis occur sporadically or as limited outbreaks, but recent reports of large hospital-associated and nursing home-associated outbreaks emphasize the importance of serovar Enteritidis infection as a major public health problem.Citation5,Citation7,Citation8 NTS is an important bacterial cause of diarrhea and community-acquired bloodstream infection.Citation9,Citation10 Globally, NTS gastroenteritis is estimated to cause 93.8 million illnesses and 155,000 deaths each year.Citation11 Invasive NTS infection occurs when the organism spreads beyond the gastrointestinal mucosa to infect normally sterile sites, such as the bloodstream, meninges, bone, and joint spaces.Citation12
Identification of NTS in fecal samples from patients is the first step in treating patients. Usually, the first line of treatment used by physicians is antibiotics. However, misuse of antibiotics inevitably leads to antibiotic resistance. The US Centers for Disease Control have discovered that, since the 1990s, NTS has shown increasing resistance to antibiotics, including ampicillin and chloramphenicol.Citation13 Therefore, initial studies on NTS should not be restricted to prevalence, but should also include their antibiotic resistance. In the light of the above, the aim of the present study was to determine the prevalence and antimicrobial susceptibility of NTS serogroups at King Fahd Hospital of the University (KFHU), Al-Khobar, Saudi Arabia.
Materials and methods
Study design
Clinical records of Salmonella strains from the clinical microbiology laboratory at KFHU for the period September 2008 to April 2011 were retrospectively reviewed. The KFHU routinely collects fecal samples from all patients admitted with acute gastroenteritis and diarrheal illness.
Culture procedure
All fecal samples were cultured directly on Hektoen agar and xylose lysine deoxycholate agar, inoculated in selenite F broth (Oxoid Ltd, Basingstoke, UK), subcultured, and identified further using an automated card system (bioMérieux Vitek Inc, Hazelwood, MO, USA) and the API 20E (bioMérieux, Marcy l’Etoile, France). All isolates were identified as Salmonella according to standard microbiologic techniques.Citation13 The identified Salmonella isolates were then serogrouped using somatic group Salmonella A–G antisera (Murex Biotech Ltd, Dartford, UK).
Antibiotic susceptibility testing
Antibiotic susceptibility testing was determined using an automated Vitek machine with Gram-negative bacteria cards, which gave minimum inhibitory concentration results and interpretation of the results as resistant or susceptible according to the breakpoints for each antibiotic. Some antibiotic susceptibility testing was determined by means of the Kirby-Bauer disk diffusion method using the guidelines provided by the Clinical Laboratory Standards Institute (CLSI), formerly known as the National Committee for Clinical Laboratory Standards.Citation14 Susceptibility tests were done on Mueller Hinton agar (Oxoid Ltd) using the following concentrations (μg/disc) of antibiotics (Oxoid Ltd): ampicillin 10 μg, amoxicillin/clavulanic acid 20/10 μg, amikacin 30 μg, aztreonam 30 μg, cefotaxime 5 μg, ceftriaxone 30 μg, cephalothin 30 μg, ciprofloxacin 5 μg, gentamicin 10 μg, imipenem 10 μg, piperacillin 100 μg, and trimethoprim/sulfamethoxazole (1.25 μg/23.75 μg). Results were scored as susceptible, moderately susceptible, or resistant, according to CLSI criteria. Escherichia coli 25922 (American Type Culture Collection, Manassas, VA, USA) was used as the reference strain.
Statistical analysis
The data were analyzed using bivariate tables and scatter graphs. The change in distribution over the years was analyzed using the chi-square test for a trend in situations where it is applicable (zeros not being adjacent to each other or cell frequencies not being less than two). The similarity of the distribution of the serogroups across the different years was tested using the Kruskal–Wallis test. The chi-square goodness of fit test was used to assess how a distribution compared with uniform distribution. For all tests, a P-value <0.05 was considered to be statistically significant. Analysis was done using MS Excel 2007 (Microsoft, Redmond, WA, USA) and PAST statistical software (version 2.04).Citation15
Results
At this teaching hospital, a total of 17,436 fecal samples were analyzed during the 2008–2011 study period. Of these specimens, a total of 158 tested positive for NTS, giving an overall prevalence of 9.06 per 1,000. The figures for each year are shown in . As can be seen, the prevalence increased from 7.0 per 1,000 in 2008 to 9.89 per 1,000 in 2009; thereafter, the prevalence declined slightly between 2009 and 2011. Positive NTS samples during 2009 and 2010 remained constant at between 40 and 41 of total positive samples, but the trend varied among the different serogroups. Serogroup D remained the most frequent of the Salmonella serogroups. The annual prevalence of serogroup D increased by more than half in 2011 compared with 2008 ().
Table 1 Prevalence of nontyphoidal Salmonella, 2008–2011
Table 2 Prevalence of Salmonella serogroups isolated during 2008–2011
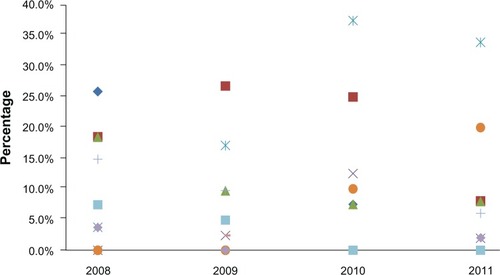
From 2008 to 2011, 158 strains of NTS were isolated from fecal samples of patients with gastroenteritis. Salmonella strains belonging to serogroup D1 had the highest prevalence (25.3%) followed by serogroup B (19.6%), and C1 serogroup (19%). Salmonella serogroup strains belonging to F (0.6%), G1 (1.3%), and H (1.3%) were the least prevalent (). The distribution of serogroups is shown in . The only serogroup showing a clear increase in trend is D1. The chi-square test for trend confirms that the only significant change in slope over the study period occurred in serogroup D1. The trend for D1 is fairly linear. The Kruskal–Wallis test does not show any significant difference in year-to-year distribution between the different serogroups (H=0.413, P=0.941).
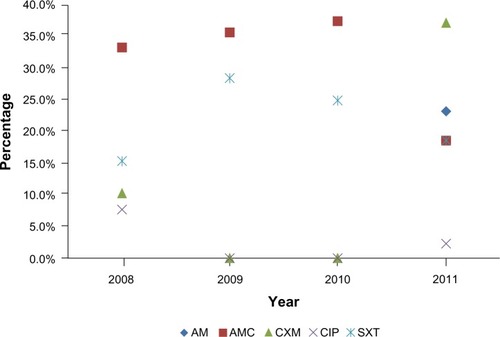
Resistance to ampicillin (31.3%) and amoxicillin/clavulanic acid (29.9%) was observed in most NTS strains. Resistance to sulfamethoxazole, trimethoprim, and cefotaxime was observed in 20.9% and 14.93% of strains (). Of all strains, the lowest resistance was noted with ciprofloxacin (3.0%, ). The Kruskal–Wallis test did not show any significant difference in year-to-year distribution between the different antibiotics (H=1.803, P=0.6205). All strains were susceptible to amikacin, aztreonam, ceftriaxone, cephalothin, gentamicin, imipenem, and piperacillin.
Table 3 Antibiotic resistance in Salmonella isolated during 2008–2011
Overall, antibiotic resistance in the NTS serogroup strains increased from 29.1% in 2008 to 32.1% in 2011. According to the chi-square goodness-of-fit test, this increase was not significantly different from the uniform distribution during the study period (P=0.065). Resistance to cefotaxime increased from 10.3% of all isolates in 2008 to 14.93% of all isolates in 2011 (). The number of isolates showing resistance to trimethoprim/sulfamethoxazole fluctuated between six and eight throughout the study period. There was an increase in the number of isolates showing resistance to trimethoprim/sulfamethoxazole from four in 2008 to 16 in 2011 (). The highest overall resistance (40.2%) was observed among strains belonging to serogroup B, followed by serogroups C2 (18.6%), C1 and D1 (10.4%), and C3 (8.2%, ).
Table 4 Overall antimicrobial resistance in Salmonella by serogroup during 2008–2011
Discussion
NTS infections are a leading cause of food poisoning and enteric infection, and are an important public health problem worldwide.Citation3,Citation9,Citation10,Citation16,Citation17Salmonella may cause gastroenteritis in people of all ages, and is responsible for severe invasive disease in infants, the elderly, and the immunocompromised.Citation18,Citation19 The frequency of antimicrobial resistance and number of resistance determinants in Salmonella has risen markedly.Citation20 Antimicrobial susceptibility to ampicillin, trimethoprim/sulfamethoxazole, and quinolones for Salmonella isolated from fecal specimens should be routinely tested and reported using the CLSI guidelines.
A surveillance study by Su et al demonstrated an obvious increase in overall antimicrobial resistance among Salmonella from 20%–30% in the early 1990s to as high as 70% in some countries at the turn of the century.Citation21 Conventional antibiotics, such as ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole, are no longer an appropriate choice for the treatment of invasive salmonellosis.Citation21 Increasing antimicrobial resistance in NTS is a global public health problem that complicates antimicrobial therapy, and is increasingly due to the overuse and misuse of antimicrobial agents in animal feeds.Citation22–Citation24 Several studies worldwide have reported increased morbidity and mortality in patients infected with resistant Salmonella strains.Citation25,Citation26 Resistance to antibiotics is posing a serious problem in the treatment of salmonellosis. In the present study, serogroup D1 (25.3%) was the most frequent and prevalent serogroup, followed by serogroup B (19.6%) and serogroup C1 (18.9%). There was an increase in gastroenteritis caused by serogroup D1 from 2008 to 2011 ( and ). Our study also confirms the emergence and rapid increase in cases of NTS infection with serogroup D1, particularly serovar Enteritidis. A similar study conducted by Chiu et al at a university hospital in Taiwan reported that the incidence of serogroup D Salmonella has been increasing in Taiwan.Citation5 The present study indicates that serogroup D was more prevalent than serogroup B and other serogroups, and if this trend were to continue, the incidence of NTS serogroup D would soon surpass that of serogroup B infection. Such a trend has been reported in the US, Europe, Taiwan, Malawi, Thailand, and Malaysia.Citation5,Citation8,Citation20,Citation27–Citation29 Serovar Enteritidis is known to be closely associated with layer and broiler flocks, and infection is generally believed to be derived from poultry and poultry products, including eggs.Citation8,Citation30
The current study findings are consistent with those of other studies reporting that most of the NTS (serovar Enteritidis) are resistant to a wide range of antimicrobial agents.Citation7,Citation30–Citation32 However, in our study, we found a higher rate of resistance to trimethoprim/sulfamethoxazole (17.7% of isolates during the period from September, 2008 to April, 2011, ). These findings are in agreement with those of a similar study on the emergence of Salmonella with extended spectrum β-lactamase enzymes that hydrolyze and confer resistance to cefotaxime in several European countries.Citation33,Citation34 In the present study, some of the strains (14.93%) were reported to be resistant to cefotaxime and ciprofloxacin (3%). Ciprofloxacin and cefotaxime are the antimicrobial agents recommended for treatment of invasive infections due to Salmonella.Citation35,Citation36
NTS species are important food-borne pathogens, with acute gastroenteritis being the most common clinical manifestation. However, invasion beyond the gastrointestinal tract occurs in approximately 5% of patients with NTS gastroenteritis, resulting in bacteremia.Citation12 In industrialized countries, NTS constitutes a well recognized public health problem that, in healthy subjects, is usually encountered clinically as self-limited gastroenteritis.Citation37,Citation38 In immunocompromised and debilitated hosts, NTS can become invasive, leading to bacteremia, sepsis, and focal infections (eg, meningitis).Citation38,Citation39 Invasiveness is also observed in infants younger than 3 months of age who become infected with NTS in industrialized countries, resulting in bacteremia and focal infections.Citation40 In sub-Saharan Africa, studies have documented the important role of NTS as invasive bacterial pathogens.Citation41–Citation44
We conclude that there is a need to establish standard first-line therapy for salmonellosis. Clinicians should be aware of the local epidemiology of NTS and carefully review the results of antimicrobial susceptibility testing once available from the clinical laboratory. Active monitoring of NTS serogroups for antibiotic resistance patterns is essential because of potential acquisition of resistance genes by pre-existing serovar Enteritidis strains via horizontal gene transfer.Citation5,Citation19,Citation20 Knowledge of the distribution of prevalence of Salmonella serogroups is potentially of epidemiologic and public health importance.
Acknowledgments
The authors thank their laboratory specialists (Lauro Bartolome, Piodennis Dasal, Bader Sager, Abdulrahim Osman) for contributing to this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- GrimontPADWeillFXAntigenic formulae of the Salmonellae serovars9th edGeneva, SwitzerlandWorld Health Organization2007 Available from: http://www.pasteur.fr/ip/portal/action/WebdriveActionEvent/oid/01s-000036-089Accessed September 1, 2013
- Crum-CianfoneNFSalmonellosis and the gastrointestinal tract: more than just peanut butterCurr Gastroenterol Rep20081042443118627657
- ScallanEHoekstraRMAnguloFJFoodborne illness acquired in the United States – major pathogensEmerg Infect Dis20111771521192848
- Centers for Disease Control and PreventionCDC Estimates of foodborne illness in the United States2011 Available from: http://www.cdc.gov/features/dsfoodborneestimates/Accessed September 1, 2013
- ChiuCHSuLHHungCCChenKLChuCPrevalence and antimicrobial susceptibility of serogroup D nontyphoidal Salmonella in a university hospital in TaiwanJ Clin Microbiol20044241544114715794
- PanhotraBRSaxenaAKAl-GhamdiAMEmerging nalidixic acid and ciprofloxacin resistance in non-typhoidal Salmonella isolated from patients having acute diarrheal diseaseAnn Saudi Med20042433233615573842
- LingJMKooICKamKMAntimicrobial susceptibility and molecular epidemiology of Salmonella enterica serotype Enteritidis strains isolated in Hong Kong from 1986 to 1996J Clin Microbiol199836169316999620402
- RodrigueDCTauxeRVRoweBInternational increase in Salmonella Enteritidis: a new pandemic?Epidemiol Infect199010521272200698
- CrumpJAMedallaFMJoyceKWEmerging Infections Program NARMS Working GroupAntimicrobial resistance among invasive nontyphoidal Salmonella enterica isolates in the United States: National Antimicrobial Resistance Monitoring System, 1996 to 2007Antimicrob Agents Chemother2011551148115421199924
- VoetschACVan GilderTJAnguloFJEmerging Infections Program FoodNet Working GroupFoodNet estimate of the burden of illness caused by nontyphoidal Salmonella infections in the United StatesClin Infect Dis200438S127S13415095181
- MajowiczSEMustoJScallanEInternational Collaboration on Enteric Disease ‘Burden of Illness’ StudiesThe global burden of nontyphoidal Salmonella gastroenteritisClin Infect Dis20105088288920158401
- HohmannELNontyphoidal salmonellosisClin Infect Dis20013226326911170916
- FarmerJJIIIEnterobacteriaceae: introduction and identificationMurrayPRBaronEJPfallerMATenoverFCYolkenRHManual of Clinical MicrobiologyWashington, DCAmerican Society for Microbiology Press1995
- Clinical and Laboratory Standards InstitutePerformance standards for antimicrobial susceptibility testing: 20th informational supplement. CLSI document 2010; M100-S20Wayne, PAClinical and Laboratory Standards Institute2010 Available from: http://www.techstreet.com/products/1662846Accessed September 1, 2013
- HammerOHarperDRyanPPast: Paleontological Statistics Software Package for Education and Data AnalysisPalaeontologia Electronica2001419
- SunSNegreaARhenMAnderssonDIGenetic analysis of colistin resistance in Salmonella enterica serovar TyphimuriumAntimicrob Agents Chemother2009532298230519332669
- MajowiczSEThe global burden of nontyphoidal Salmonella gasteroenteritisClin Infect Dis20105088288920158401
- RocourtJMoyGVierkKThe present state of foodborne disease in OECD countriesGeneva, SwitzerlandWorld Health Organization2003 Available from: http://www.who.int/foodsafety/publications/foodborne_disease/oecd_fbd.pdfAccessed September 1, 2013
- GoldbergMBRubinRHThe spectrum of Salmonella infectionInfect Dis Clin North Am198825715983074116
- World Health OrganizationThe medical impact of the use of antimicrobials in food animals: report and proceedings of a WHO meeting, Berlin, Germany, October 13–17, 1997Geneva, SwitzerlandWorld Health Organization1997 Available from: http://whqlibdoc.who.int/hq/1997/WHO_EMC_ZOO_97.4.pdfAccessed September 1, 2013
- SuLHChiuCHChuCOuJTAntimicrobial resistance in nontyphoid Salmonella serotypes: a global challengeClin Infect Dis20043954655115356819
- TsaiMHWuSRLeeHYRecognition of mechanisms involved in bile resistance important to halting antimicrobial resistance in non-typhoidal SalmonellaInt J Antimicrob Agents20124015115722743016
- SwartzMNHuman diseases caused by foodborne pathogens of animal originClin Infect Dis200234111122
- McDonaldLCChenMTLauderdaleTLHoMThe use of antibiotics critical to human medicine in food-producing animals in TaiwanJ Microbiol Immunol Infect2001349710211456367
- HelmsMVastrupPGerner-SmidtPMølbakKExcess mortality associated with antimicrobial drug-resistant Salmonella TyphimuriumEmerg Infect Dis2002849049511996684
- VarmaJKMolbakKBarrettTJAntimicrobial-resistant nontyphoidal Salmonella is associated with excess bloodstream infections and hospitalizationsJ Infect Dis200519155456115655779
- GordonMAGrahamSMWalshALEpidemics of invasive Salmonella enterica serovar Enteritidis and S. enterica serovar Typhimurium infection associated with multidrug resistance among adults and children in MalawiClin Infect Dis20084696396918444810
- KiratisinPBacteraemia due to non-typhoidal Salmonella in Thailand: clinical and microbiological analysisTrans R Soc Trop Med Hyg200810238438818321543
- DhanoaAFattQKNon-typhoidal Salmonella bacteraemia: epidemiology, clinical characteristics and its association with severe immunosuppressionAnn Clin Microbiol Antimicrob200981519445730
- OlsenSJBishopRBrennerFWThe changing epidemiology of Salmonella: trends in serotypes isolated from humans in the United States, 1987–1997J Infect Dis200118375376111181152
- LeeLAPuhrNDMaloneyEKBeanNHTauxeRVIncrease in antimicrobial-resistant Salmonella infections in the United States, 1989–1990J Infect Dis19941701281348014487
- ThrelfallEJWardLRSkinnerJARoweBIncrease in multiple antibiotic resistance in nontyphoidal salmonellas from humans in England and Wales: a comparison of data for 1994 and 1996Microb Drug Resist199732632669270996
- BatchelorMThrelfallEJLiebanaECephalosporin resistance among animal-associated Enterobacteria: a current perspectiveExpert Rev Anti Infect Ther2005340341715954857
- MeakinsSFisherISBergholdCEnter-net ParticipantsAntimicrobial drug resistance in human nontyphoidal Salmonella isolates in Europe 2000–2004: a report from the Enter-net International Surveillance NetworkMicrob Drug Resist200814313518366323
- ThrelfallEJAntimicrobial drug resistance in Salmonella: problems and perspectives in food- and water-borne infectionFEMS Microbiol Rev20022614114812069879
- AnguloFJJohnsonKRTauxeTWOrigins and consequences of antimicrobial-resistent nontyphoidal Salmonella: implications for the use of fluoroquinolones in food animalsMicrob Drug Resist20006778310868811
- VoetschACVan GilderTJAnguloFJFoodNet estimate of the burden of illness caused by nontyphoidal Salmonella infections in the United StatesClin Infect Dis200438S127S13415095181
- AdakGKLongSMO’BrienSJTrends in indigenous foodborne disease and deaths, England and Wales: 1992 to 2000Gut20025183284112427786
- KennedyMVillarRVugiaDJEmerging Infections Program FoodNetWorking GroupHospitalizations and deaths due to Salmonella infections, FoodNet, 1996–1999Clin Infect Dis200438S142S14815095183
- VugiaDJSamuelMFarleyMMEmerging Infections Program FoodNetWorking GroupInvasive Salmonella infections in the United States, FoodNet, 1996–1999: incidence, serotype distribution, and outcomeClin Infect Dis20043814915614679463
- BerkleyJALoweBSMwangiIBacteremia among children admitted to a rural hospital in KenyaN Engl J Med2005352394715635111
- IkumapayiUNAntonioMSonne-HansenJMolecular epidemiology of community-acquired invasive non-typhoidal Salmonella among children aged 2–29 months in rural Gambia and discovery of a new serovar, Salmonella enterica DingiriJ Med Microbiol2007561479148417965348
- SigaúqueBRocaAMandomandoICommunity-acquired bacteremia among children admitted to a rural hospital in MozambiquePediatr Infect Dis J20092810811319131902
- MandomandoIMaceteESigaúqueBInvasive non-typhoidal Salmonella in Mozambican childrenTrop Med Int Health2009141467147419793081