Abstract
Malaria, a disease of poverty and high morbidity and mortality in the tropical world, has led to a worldwide search for control measures. To that end, good antimalarial chemotherapies have been difficult to find in the global market and those that seem to be most effective are rapidly becoming ineffective due to the emergence and spread of drug resistance. Artemisinin, a very effective yet expensive antimalarial, has quickly become the recommended drug of choice when all other possibilities fail. However, for all its promise as the next great antimalarial, the outlook is bleak. Resistance is developing to artemisinin while another effective antimalarial is not in sight. Malaria endemic areas which are mostly in developing countries must deal with the multifaceted process of changing and implementing new national malaria treatment guidelines. This requires complex interactions between several sectors of the affected society which in some cases take place within the context of political instability. Moreover, the cost associated with preventing and containing the spread of antimalarial resistance is detrimental to economic progress. This review addresses the impact of artemisinin resistance on the socioeconomic structure of malaria endemic countries.
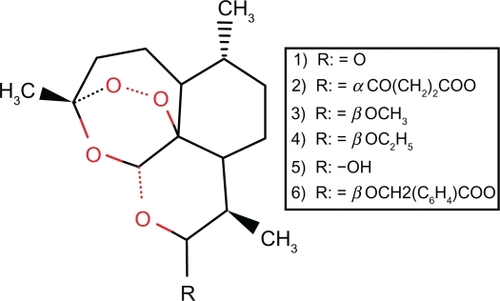
Malaria, a mosquito-borne parasitic disease, affects 510 million people causing almost 3 million deaths annually.Citation1 For more than 50 years, cinchona alkaloids and their derivatives were an integral part of malaria control. Indeed, chloroquine was one of the most effective synthetic antimalarial drugs ever produced. However, chloroquine-resistance falciparum malaria was first reported in South East Asia and South America and has now spread through Asia, Africa, and South America.Citation2 This has led to a global resurgence of malaria. Currently, these alkaloids are being replaced by the terpene Artemisia annua, also known as qing hao or sweetworm, whose active ingredient is artemisinin. Discovered in 1971 by Chinese scientists, artemisinin was introduced to the world in 1979.Citation3 Although quite expensive to produce, artemisinin is one of the most effective antimalarials. It is currently grown by farmers in China, Vietnam, and parts of Africa. With a long growing season, the process of extracting artemisinin from the leaves is complex and time consuming. Because of the difficulty in extracting it from the plant, a semi-synthetic version generated by the addition of chemical groups to extracted artemisinin is commonly used. Dihydroartemisinin (DHA) is the product of the first step; additional synthetic steps give rise to artesunate, artemether, and arteether which are metabolized back to dihydroartemisinin in the body (). The artemisinin derivatives possess greater antimalarial properties. They are active against multiple drug-resistant parasites and have a very low level of toxicity to humans. As an antimalarial drug, artemisinin has a broad range of action against different stages of the parasite. It kills young circulating ring-stage parasites as well as the mature stages that sequester on blood vessels.Citation3 Because of these properties, artemisinin is very useful in cases of severe malaria. Because of its broad range of action, dispensation of a single dose kills a large number of parasites. All the stages of the P. falciparum life cycle, including the gametocytes which transmit the infection to mosquitoes, are killed by artemisinin. Artemisinin is known to decrease the rate of gametocyte carriage and gametocyte density in a population.Citation3–Citation5
Figure 1 Chemical structure of artemisinin and derivatives. Diagram of artemisinin and its derivatives. 1, artemisinin; 2, artesunate; 3, artemether; 4, arteether; 5, dihydroartemisnin; 6, artelinic acid.
Although very little is known about the molecular mechanism of action of artemisinin and its derivatives, there are a few studies that give insight into its mechanism. For instance, after treatment of P. berghei-infected mice and P. falciparum parasites grown in human erythrocytes with artemisinin, trophozoites showed morphological changes, such as swelling and spiral deformation of the membrane of the food vacuole when blood samples were examined by electron microscopy.Citation5 Results of additional studies have shown that artemisinin is a blood schizontocide that has an inhibitory action on the parasite’s protein and nucleic acid metabolism.Citation6 While the mechanism of action of artemisinin has not been elucidated, it was recently revealed that the endoperoxide bridge is essential for arteminsinin killing (). The sarcoplasmic endoplasmic reticulum calcium adenosine triphosphatase (PfATPase 6) has been promulgated as the main target.Citation7 This assessment is based on mutational studies in the gene coding for PFATPase 6. P. falciparum parasites from French Guyana with point mutations in the gene encoding PfATPase 6 showed resistance to artemisinin derivatives.Citation8 Nevertheless, these findings have not been confirmed in parasites from other parts of the world.
Malaria drug resistance
The reemergence of malaria drug resistance is a major problem in the tropical and subtropical world. Several factors influence the reemergence of drug resistance. Among them is the level of immunity against the malaria parasite in the population.Citation9 For instance, in low or unstable transmission areas, drug resistance propagates rapidly. This is due to minimal immunity in a population, thus parasite infections lead to acute symptomatic disease which is most likely treated. Therefore, drug resistance is likely to propagate rapidly due to high drug pressure on existing parasites. In fact, certain mutations are prevalent as a result of high drug pressure in most sub-Saharan countries.Citation10 On the other hand, in areas where malaria transmission is high, the spread of drug resistance is restricted because of high levels of immunity. Here, there is less need for treatment in a population because there are fewer clinical symptoms. One study based in Tanzania showed that immunity enhanced drug efficacy.Citation10
Changing national malaria treatment policy
Malaria parasite resistance is a complex process that requires constant monitoring and strategic actions to save lives. New national malaria treatment policies have been slow to implement at the country level and therefore have not been very effective in relieving the burden of disease. Many malaria endemic countries have relied on chloroquine as a first-line of treatment against malaria for several decades. Chloroquine was the antimalarial drug of choice because of its low cost and efficacy. The spread of chloroquine resistance across malaria-endemic areas has caused an incredible challenge for the majority of endemic countries.Citation11–Citation14 National malaria control programs of endemic countries had to develop malaria treatment policies in response to elevated levels of drug resistance to chloroquine (CQ) and sulphadoxine-pyrimethamine (SP).Citation15–Citation19 This has led to an international effort to replace CQ with relatively more expensive but highly effective artemisinin-based combination therapies (ACTs). The drugs containing artemisinin show 100% effectiveness after a three to f ive day regimen. However, due to the intensive labor and length of production, these drugs are costly, making them inaccessible to the world’s poorest countries.Citation19
A change in international therapeutic recommendations does not always translate to an immediate policy change at country levels.Citation14,Citation20–Citation22 According to the World Health Organization (WHO), all African countries have switched from using chloroquine, except Cape Verde and Eritrea for treatment of falciparum malaria.Citation23 In Cape Verde, SP is used when chloroquine fails. Likewise, the Maldives Islands of South East Asia continue to use chloroquine-based antimalarial therapies with recourse to a combination of mefloquine and SP when treatment fails.Citation23 Most malaria endemic countries have entered into partnership with the World Health Organization (WHO) Roll Back Malaria program since 1998 and have thus made a concerted effort to control malaria.Citation24,Citation25 The result of this effort was the enactment through National Malaria Control Programs with recommendation of new antimalarials as first-line treatments. Since 1998, new policy suggested that malaria endemic areas change their first-line recommendations for the treatment of malaria at least twice before advocating the use of artemisinin-combination therapies.Citation21,Citation22 A good example of a country changing its policies is Tanzania. There, malaria is most commonly a disease of rural agricultural communities, and widespread antimalarial drug resistance has been reported.Citation12 Although a plan was initiated in Tanzania, the number of cases and deaths due to malaria are still increasing; this increase is thought to be due to resistance to antimalarial drugs. Chloroquine-resistant falciparum malaria is widespread in Tanzania, and sulfadoxine-pyrimethamine (SP) was only introduced in 2001. Despite this, resistance to SP has been found in a number of areas. The first-line treatment was changed again to artemisinin-based combination therapy in 2006.Citation14
Artemisinin resistance
Artemisinin is currently playing an important role in the control of falciparum malaria. However, CQ and SP, used singly or in combination, remain the drugs of choice for the treatment of vivax malaria.Citation26 Artemisinin has a very short half-life and quickly clears from the body by glycoronidation, with CYP 2B6, the primary catalyst.Citation27,Citation28 This characteristic renders it useless as a prophylaxis.Citation6 However, it gave credence to the hypothesis that mutations will not arise against artemisinin very easily. Though artemisinin and its derivatives were initially used as monotherapies, they are now used in combination because of the high rate of emergence of resistance against several antimicrobial drugs given as monotherapies. Artemisinin is often given in combination with a variety of antimalarials including those with a longer half-life. Indeed, artemisinin combination therapy (ACT) is now the suggested treatment for falciparum malaria in all endemic areas. In 2006, the World Health Organization (WHO) issued guidelines for the treatment of malaria and recommended ACT as the first-line of treatment in all endemic areas.Citation3 The recommendations for global use of artemisinin derivatives were founded on their outstanding tolerability, safety, and efficacy. With no alternative drugs, artemisinin was to be protected from resistance by controlled rational use with the development and implementation of global policies. During a meeting of the WHO that took place in 1998 to review the use of artemisinin, the experts gave advice on the appropriate use of artemisinin in different epidemiological situations.Citation29 A report was generated outlining detailed recommended drug regimens, clinical use, and priority areas for research.Citation29 Drug regimens and clinical use were outlined for each country. A summary of the recommendations is shown in . Malaria endemic countries with the assistance of WHO have carefully developed and implemented policies aimed at controlling the use of artemisinin. It was recommended that public health services be the sole means of allowing artemisinin in the market.
Table 1 Recommended artemisinin combination therapies. Adapted from Roll Back Malaria Partnership: Facts on ACTs January 2006 Update
Long before these efforts to prevent resistance against artemisinin, resistance was first reported in Pailin, Cambodia in the 1970s.Citation30 This city has been the site of three successive waves of antimalarial resistance. Here, resistance first developed against chloroquine then sulfadoxine-pyrimethamine.Citation3,Citation31 Resistant parasites have extended not only throughout Cambodia and Asia but also to sub-Saharan Africa, rendering important weapons in the fight against falciparum malaria ineffective.Citation3 Antimalarial resistance is defined as the increased parasite clearance time following treatment whereas treatment failure is defined as the presence of fever and parasitemia after three days of treatment. It normally takes three days for parasites to clear in patients after drug treatment.Citation3 The first official report about the decreasing effectiveness of artemisinin was published by WHO in 2005.Citation32 In addition to four provinces in Cambodia, P. falciparum parasites are also believed to be resistant in two provinces in Thailand.Citation31 Countries such as Cambodia, Myanmar, and Vietnam, which have allowed artemisinin into the market without the supervision of the public health services, have tremendous problems with resistance. In fact, artemisinin has been used as a monotherapy in Western Cambodia for nearly 30 years. In 2009, scientists confirmed the emergence of P. falciparum parasites that have developed resistance to artemisinin derivatives in Pailin, Cambodia. This resistance has now spread to other cities of Cambodia as well as to the Thai-Myanmar border. In order to combat this dilemma WHO has suggested that countries employ the use of ACTs, to lower the risk of producing more artemisinin-resistant Plasmodium parasites.Citation24
Artemisinin combination therapies (ACTs) are a combination of an artemisinin derivative with another antimalarial such as piperaqine or amodiaquine. A list of artemisinin-based therapies is shown in . In 2001, WHO launched its “Roll Back Malaria Partnership”, a campaign that outlined the use of artemisinins in conjunction with medications such as lumefantrine, amodiaquine, mefloquine, sulfadoxine, or pyrimethamine.Citation24 A list of antimalarial drugs and their abbreviations can be found in . As of 2006, 56 countries in Africa, Asia, and South America adopted the use of WHO guidelines for treating malarial infections caused by Plasmodium falciparum with ACTs.Citation24 In 2007, the number of countries in Africa using ACTs increased by 41. The impact of ACT treatment on malaria transmission may vary among artemisinin combinations although the effect is synergistic.Citation33
Table 2 Abbreviations of currently used antimalarial drugs
Artemisinin has played a pivotal role in the control of malaria worldwide. The unwelcome possibility that Plasmodium parasites can develop complete resistance to artemisinin derivatives could be a catastrophe of monumental proportion for global health. Currently, there are no drugs in the pipeline to replace artemisinin, and it could take five or more years to find a replacement drug.Citation3,Citation34 The widespread resistance of Plasmodium parasite to artemisinin would spell disaster for sub-Saharan African countries that had made significant gain in reducing morbidity and mortality due to malaria.
Intervention efforts spearheaded by WHO, the national malaria control programs, and the Gates foundation to contain the spread of artemisinin resistance are currently underway.Citation35 The primary approach in containing the spread of artemisinin resistance is to control the sale of this anti-malarial in the private sector. This involves campaigns by the governmental agencies to inform the private sectors, which include pharmacies and shops, about the ban against artemisinin monotherapy. The removal of artemisinin monotherapy from the market will greatly reduce the pressure of a single drug on the parasite and cause them to revert to the wild type genotypes which are genetically more fit. The campaigns take the form of workshops and radio and television broadcasts.Citation33,Citation35 Law enforcement agencies are also involved in the effort. Their role is to make sure that the ban is enforced. Moreover, a concerted effort to remove antimalarial drugs from the local stores and to allow trained villagers to dispense the malaria drugs after proper diagnostic tests have been performed is underway.Citation33,Citation35 This insures that every case of fever is not treated with antimalarials. It is possible that this strategy may not be successful as it is dependent on infected individuals displaying symptoms. In endemic areas, many individuals, especially adults, are asymptomatic and carry a low parasite load. These asymptomatic individuals would still able to transmit artemisinin-resistant parasites. To counteract this, there are programs in place in Cambodia to screen and treat all patients who are positive for infection with drugs regardless of symptoms.Citation35 In addition, efforts are also aimed at prevention by intensifying the wide scale distribution of bednets. A population dynamic mathematical modeling framework was developed to explore the relative effectiveness of a variety of containment interventions in eliminating artemisinin-resistant malaria in western Cambodia.Citation36 The most effective intervention to eliminate artemisinin-resistant malaria was a switch of treatment from artemisinin monotherapy to ACT with 4 years being the average estimated time for elimination of the resistant parasites. However, with this approach it is predicted that elimination of artemisinin-resistant malaria using ACT can be achieved only by elimination of all malaria cases in the area. In this case various forms of ACT are more effective against infections with artemisinin-sensitive parasites, leaving the more resistant infections at an increasing proportion of the dwindling parasite population.Citation36,Citation37 That in and of itself is a daunting task. The emergence of artemisinin in South East Asia and the potential spread to all malaria endemic areas would pose both social and economic challenges for these countries.
Social impact of artemisinin resistance
The first change in malaria treatment in endemic areas involved shifting from the failing inexpensive CQ to SP, another inexpensive monotherapy.Citation23,Citation25 The spread of antimalarial resistance with the resulting challenges of implementing national malaria drug policies occurs in social contexts where self-medication, mistrust of government officials, and lack of compliance are common. The changes are introduced by the Ministry of Health of various governments which are often not trusted. In Tanzania, this took place in 2001.Citation14 There was some reluctance on the part of many to use SP when it was first introduced to replace CQ.Citation14,Citation18 Because CQ was used for several decades and was considered to be safe and effective, many households in Tanzania still had stockpiles of CQ. Moreover, health care practitioners there had developed a certain attachment to CQ. To make matters worse, mothers of sick children felt they were being forced to abandon CQ which they considered to be more effective than SP because the recommended dose of the new drug did not quickly relieve fever, the outward symptom of malaria. This led to not only suspicion and noncompliance, but a continued use of CQ, the failing drug.Citation21
Furthermore, the acceptance of new antimalarials by a community is dependent on the degree of knowledge about the new drug and its proper use. Most individuals are informed by health care practitioners or by materials displayed at health care facilities. In some cases, the media by way of television, and commonly radio and newspapers, play an important role in disseminating information about the new antimalarials. This can lead to fear since oftentimes the journalists emphasize the negative side effects of the new drugs. Successful transition to new antimalarials is strongly dependent on journalists being educated about the new drug in order to disseminate correct information to the general public. Once a negative opinion is formed about a drug, the general public develops a prejudice against it and it is a major challenge to accept the new antimalarial despite its effectiveness. It has been reported that mothers would not give the new antimalarials because of their perceived ill effects.Citation18,Citation21 They would go as far as inducing vomiting in their children to prevent them from consuming the new drug. This puts increased pressure on health care workers who have to closely monitor patients to ensure ingestion of the drug before being allowed to return to their home. In addition, changes to new drugs are always accompanied by anxieties on the part of the public regarding perceived or experienced adverse reactions. Although few individuals had experienced adverse reactions, every person interviewed had learned through the media about deaths following the use of SP.Citation21
When SP started to fail in 2003, introduction of artemisinin combination therapies (ACTs) was met with even greater resistance by members of the community, especially caregivers, because ACTs were not made available over the counter like chloroquine.Citation18,Citation21 It is very likely that similar reactions would be observed if a new regimen of antimalarials were to be recommended so soon after switching to ACT. It was expected that ACT would have a lifespan as long as chloroquine. The rise and spread of acquired resistance to artemisinin-based therapy might erode the trust of the population in the ability to provide a long-lasting drug against malaria. There were already thoughts of government conspiracy aimed at killing off the population or experimenting on the population with new antimalarials from some participants in a focus discussion group aimed at assessing the perception of various social groups in Tanzania about the recommendation of SP as the new first-line of treatment against malaria.Citation21
Economic impact of malaria
In our consideration of the economic impact of artemisinin resistant malaria, we first consider the impact of malaria itself on a country’s economy. We will then consider the impact from the use of artemisinin. Lastly, we consider the economic impact of artemisinin-resistant malaria.Citation38
First, we acknowledge that there are many factors that have an impact on a country’s economy other than malaria. Some of these factors that result in low incomes and low economic growth are poor soils, low agricultural productivity, tropical diseases other than malaria, trade barriers, weak institutions, poor economic policies, ethnic conflict, and the residue of colonization.Citation38 Although all these factors play a role in the economy of a country there are reports that consider the economic impact of malaria to be so high that it is considered the major cause of poverty.Citation39
The economic impact of malaria takes a toll on the population living in an endemic area. It is actualized in individual as well as government costs. To an individual, the cost can accumulate in the expense of medical treatment, travel to dispensaries and clinics, preventions, and burial upon death, as well as loss of income from days away from work and school. Malaria has even been implicated in learning disability in children by which the far reaching effects cannot be realized and calculated in the effect of malaria on an economy.Citation39 On the other hand, governments sustain costs in health care facility maintenance, drugs and supplies, insecticide spraying, and bednet distributions. They also sustain loss of income from sick workers, economic ventures, and lack of tourism. For example, peak periods of malaria transmission often coincide with the peak period of agricultural activity.Citation39 Farmers prefer to plant subsistent crops rather than more labor intensive cash crops.Citation24 These costs impede economic growth in malaria endemic countries. It is estimated that the economy of malaria endemic countries is 1.3% lower than countries without malaria. This estimate seems low. However, when it is taken into consideration that most malaria endemic (GDP) countries are developing with lower gross domestic product, defined as the market value of all final goods and services made within the borders of a country in a year, it is a major factor for endemic countries.Citation40
The GDP of a country is often positively correlated with the standard of living. The standard of living of persons living in a malaria endemic area can remain low because of malaria. Malaria disproportionately affects poor people who cannot afford treatment or have limited access to health care. These factors trap families and communities in a downward spiral of poverty.Citation20 The economic gap in prosperity between countries with and without malaria grows every year.Citation24 It is interesting to note that in almost all countries that have eradicated malaria, there was an immediate economic growth that was faster than neighboring countries. These examples stem from data collected from southern European countries such as Greece, Italy, and Spain.Citation40 The richest countries in Africa are free of malaria and located in the northern and southern extremes of the continent. The gross domestic product of malarial countries in 1995 was $1,526 compared to $8,268 in countries without malaria.Citation40
The economic impact of the use of artemisinin
The era of cheap effective antimalarials has ended but poverty has not. The cost of artemisinin combinational therapies is more than any other antimalarial monotherapy or non-artemisinin combinational therapy. In Tanzania $2.14 is spent on malaria control per person per year. This is a huge debt on the country’s economy. This number represents 39% of the health cost and 1.1% of the country’s GDP.Citation39 However, in the long run, treating sick people so that they can return to work and school will help the economy. This will translate to economic growth and poverty reduction. In Cameroon, the government subsidizing malarial combination treatment made drug therapy affordable for all people.Citation41 This greatly relieved both individuals and the government from the burden of malaria. Overall, this will result in economic development because workers can gain income and economic ventures and tourism will start to flourish.
The economic impact of artemisinin resistance
As with any antimalarial drug resistance, artemisinin drug resistance has a major impact on health services. With the increase of transmission and drug failures, medical care needs increase. There is a demand for more patient care, diagnostic procedures, and increased costs associated with combination treatments.Citation38 So the cycle continues as if the drug never existed. In some countries, chloroquine is still being used even with high failure when alternative drugs such as SP are available. This is a health policy failure, however, policy changes have been signif icantly associated in terms of cost with retraining health care workers, printing new drug regimens, and stocking new drugs.Citation42
Another cost of artemisinin resistance is the increase in morbidity and mortality in the tropical world.Citation43 It is estimated that the number of malarial deaths would double with the spread of artemisinin-resistant parasites. People suffer and die because they will not be able to treat them. The economic toll would topple the economy of any developing country providing health care to a great portion of the population of workers and students with no tax revenue in return. The economic prosperity of Thailand and Vietnam, the epicenter of drug resistance to other antimalarials, is threatened by the looming threat of artemisinin resistance. Dr Pascal Ringwald of WHO, who spoke at the ASTMH session in November of 2009 said: “The loss of artemisinin derivatives to resistance could have a devastating effect on health in tropical countries, and would threaten current global efforts to eliminate malaria, as there are very few innovative replacement therapies in the pipeline at the late stage of development”. The cost in human morbidity and mortality across the globe would be detrimental to economic development and could reverse any progress that antimalarial efforts have made.Citation44 Although the outlook is bleak, we are hopeful that some new drug or vaccine will come with billions of dollars put forth in the research effort. It is a matter of a race against time.
Future considerations
Looking forward, a multipronged approach against malaria, a formidable scourge to worldwide health, can be put in place. Given that artemisinin combination therapies are more expensive than current drugs, several strategies can be undertaken to prevent further emergence of resistance against this valuable antimalarial. First, some countries could switch to SP as an interim measure. This would delay the higher treatment cost of ACTs. However, SP resistance is expected to rise within a few years leading to increased morbidity and mortality.Citation42 Second, another source of artemisinin is from partial chemical synthesis. This will help ensure that ACT manufacturers have a consistent, reliable, high quality, and inexpensive supply of the compound. This idea was put forth by the US agency for International Development which commissioned the Institute of Medicine (IOM) in 2001 to ensure broad access to effective antimalarials. The IOM recommended a global subsidy program of ACTs treatment. Therefore, expensive ACTs (cost $2 USD per treatment) would cost 10 cents per treatment as did CQ and SP. Furthermore, only those patients with a proven case of falciparum malaria would receive ACTs.Citation45 Another intervention comes from local and international companies doing business in endemic areas. They are learning to support malaria control thus reducing absenteeism and losses in productivity.Citation24 Finally, the continued use of insecticide-treated bednets, and residual spraying should effectively control malaria and slow the spread of drug resistance. Although this multipronged approach maybe effective, they must be implemented and they also must be acceptable to the patients and health care workers. Moreover, patients must adhere to treatment. Some social interventions may be needed to increase successful malaria control.
Disclosure
The authors report no conflicts of interest in this work.
References
- NojiEKThe global resurgence of infectious diseasesTrend Report20019223232
- PayneDSpread of chloroquine resistance in Plasmodium falciparumParasitol Today1987324124615462966
- WhiteNJQinghaosu (artemisinin): the price of successScience200832033033418420924
- ter KuileFWhiteNJHolowayPPasvolGKrishnaSPlasmodium falciparum: in vitro studies of the pharmacodynamic properties of drugs used for the treatment of severe malariaExp Parasitol19937685958467901
- ChenPQLiGQGuoXBThe infectivity of gametocytes of Plasmodium falciparum from patients treated with artemisininsChin Med J. (Engl.)19941077097117805466
- WhiteNJOlliaroPArtemisinin and derivatives in the treatment of uncomplicated malariaMed Trop1998585456
- PeterWSession 2: global perspectives of malaria changing pattern of antimalarial drug resistanceJ Royal Soc MedicineSupp 171989821316
- Eckstein-LudwigUWebbRvan GoethamDAArtemisinins target the SERCA of Plasmodium falciparumNature200342495796112931192
- JambouRLegrandENiangMResistance of Plasmodium falciparum field isolates to in vitro artemether and point mutations of the SERCA-type PfATPase6Lancet20053661960196316325698
- GreenhouseBSlaterMNjama-MeyaDDecreasing efficacy of antimalarial combination therapy in Uganda is explained by decreasing host immunity rather than increasing drug resistanceJ Infect Dis200919975876519199542
- EnevoldANkyaWMTheisenMPotential impact of host immunity of malaria treatment outcome in Tanzanian children infected with Plasmodium falciparumMalar J2007615316218021388
- DondorpAMNostenFYiPArtemisinin resistance in Plasmodium falciparum malariaN Engl J Med200936145567 Erratum in: N Engl J Med. 2009;361:171419641202
- SchönfeldMBarretoMISchunkMMolecular surveillance of drug-resistance associated mutations of Plasmodium falciparum in south-west TanzaniaMalar J20071562
- MboeraLEMakundiEAKituaAYUncertainty in malaria control in Tanzania: crossroads and challenges for future interventionsAm J Trop Med Hyg20077711211818165482
- MulliganJAMandikeRPalmerNThe costs of changing national policy: lessons from malaria treatment policy guidelines in TanzaniaTrop Med Int Health20061145246116553928
- MulliganJAMandikeRPalmerNThe costs of changing national policy: lessons from malaria treatment policy guidelines in TanzaniaTrop Med Int Health20061145246116553928
- ShrettaROmumboJRapuodaBASnowRWUsing evidence to change antimalarial drug policy in KenyaTrop Med Int Health2000575576411123822
- KamyaMRBakyaitaNNTalisunaAOWereWMStaedkeSGIncreasing antimalarial drug resistance in Uganda and revision of the national drug policyTrop Med Int Health200271031104112460394
- KindermansJMPecoulBPerez-CasasCBoerMDBermanDCoxIChanging national malaria treatment protocols in Africa: what is the cost and who will pay? Case studies: Burundi, Kenya, Rwanda, Tanzania and UgandaMedicins Sans Frontieres2002115
- WilliamsHADurrheimDNShrettaRThe process of changing national malaria treatment policy: lessons from country-level studiesHealth Policy Plan20041935637015459161
- MulliganJAMandikeRPalmerNThe costs of changing national policy: lessons from malaria treatment policy guidelines in TanzaniaTrop Med Int Health20061145246116553928
- World Health OrganizationAccess to antimalarial medicines: improving the affordability and financing of artemisinin-based combination therapiesGeneva, SwitzerlandWHO2003115
- AminAAZurovacDKangwanaBBThe challenges of changing national malaria drug policy to artemisinin-based combinations in KenyaMalar J200767217535417
- WilliamsHADurrheimDShrettaRThe process of changing national malaria treatment policy: lessons from country-level studiesHealth Pol Plan200419356370
- World Health OrganizationSusceptibility of Plasmodium falciparum to antimalarial drugs: report on global monitoring: 1996–2004WHO, Geneva
- World Health OrganizationFacts on ACTs (Artemisin-based Combination Therapies), January 2006 update2006 Available from: http://www.rollbackmalaria.org/cmc_upload/0/000/015/364/RBMInfosheet_9.htm. Accessed Jul 20, 2010.
- World Health OrganizationA global strategy for malaria controlGeneva, SwitzerlandWHO1993
- World Health OrganizationWorld malaria report 2009Geneva, SwitzerlandWHO2009
- AshtonMNguyenDSNguyenVHArtemisinin kinetics and dynamics during oral and rectal treatment of uncomplicated malariaClin Pharmacol Ther1998634824939585803
- AsimusSElsherbinyDHaiTNArtemisinin antimalarials moderately affect cytochrome P450 enzyme activity in healthy subjectsFundam Clin Pharmacol20072130731617521300
- World Health OrganizationThe treatment of malariaGeneva, SwitzerlandWHO2006
- DondorpAMNostenFPoravuthDReduced in-vivo susceptibility of Plasmodium falciparum to artesunate in Western CambodiaN Engl J Med [In press.]
- SamarasekeraUCountries race to contain resistance to key antimalarialLancet200937427728019639670
- World Health OrganizationWorld malaria report 2005Geneva, SwitzerlandWHO2005
- FofanaBDijimdeAASagaraIImpact of artemisinin-based combination therapy on malaria transmission in Mali2009 (MIM16762172 www.minmalaria.org)
- WhiteNNostenFLooareesuwanSAverting a malaria disasterLancet19993531965196710371589
- DondorpAMYeungSWhiteLArtemisinin resistance: current status and scenarios for containmentNat Rev Microbiol2010827228020208550
- MaudeRJPontavornpinyoWSaralambaSThe last man standing is the most resistant: eliminating artemisinin-resistant malaria in CambodiaMalar J200983119228438
- World Health OrganizationGlobal malaria control and elimination: report of a meeting on containment of artemisinin toleranceGeneva, SwitzerlandWHO2008
- GallupJLSachsJDThe economic burden of malariaAm J Trop Med Hyg200164859611425181
- MboeraLEMakundiEAKituaAYUncertainty in malaria control in Tanzania: crossroads and challenges for future interventionsAm J Trop Med Hyg20077711211818165482
- SayangCGausseresMVernazza-LichtNMalvyDBleyDMilletPTreatment of malaria from monotherapy to artemisinin-based combination therapy by health professionals in urban health facilities in Yaoundé, central province, CameroonMalar J20092817619640292
- SayangCGausseresMVernazza-LichtNMalvyDBleyDMilletPTreatment of malaria from monotherapy to artemisinin-based combination therapy by health professionals in urban health facilities in Yaoundé, central province, CameroonMalar J2009817619640292
- LaxminarayanRACT Now or later: the economics of malaria resistance. Resources for the future2003 Discussion Paper. 3–51
- BjorkmanABhattaraiAPublic health impact of drug resistant Plasmodium falciparum malariaActa Trop20059416316915893289
- PanosianCEconomic access to effective drugs for falciparum malariaClin Infect Dis20054071371715714418