Abstract
Introduction
Moraxella catarrhalis previously considered as commensal of upper respiratory tract has gained importance as a pathogen responsible for respiratory tract infections. Its beta-lactamase-producing ability draws even more attention toward its varying patterns of resistance.
Methods
This was an observational study conducted to evaluate the prevalence and resistance pattern of M. catarrhalis. Patients aged 20–80 years admitted in the Department of Chest Medicine of Liaquat National Hospital from March 2012 to December 2012 were included in the study. Respiratory samples of sputum, tracheal secretions, and bronchoalveolar lavage were included, and their cultures were followed.
Results
Out of 110 respiratory samples, 22 showed positive cultures for M. catarrhalis in which 14 were males and eight were females. Ten samples out of 22 showed resistance to clarithromycin, and 13 samples out of 22 displayed resistance to erythromycin, whereas 13 showed resistance to levofloxacin. Hence, 45% of the cultures showed resistance to macrolides so far and 59% showed resistance to quinolones.
Conclusion
Our study shows that in our environment, M. catarrhalis may be resistant to macrolides and quinolones; hence, these should not be recommended as an alternative treatment in community-acquired lower respiratory tract infections caused by M. catarrhalis. However, a study of larger sample size should be conducted to determine if the recommendations are required to be changed.
Introduction
Moraxella catarrhalis is a gram-negative diplococcus, formerly known as Neisseria catarrhalis or Branhamella catarrhalis, that is found in the human upper respiratory tract as normal flora and was considered to occasionally cause infections.Citation1 Currently, M. catarrhalis is a recognized pathogen of upper and lower respiratory tract infections.Citation2 It has been found as the causative agent in infections, such as empyema, endocarditis, otitis media, and pneumonia, both in children and adults.Citation3,Citation4 The beta-lactamase-producing M. catarrhalis not reported before 1976 is the significant cause of varying patterns of resistance.Citation5 The increase in occurrence of beta-lactamase strains can be regarded as the fastest dissemination of beta-lactamases within a bacterial species.Citation6 M. catarrhalis has particularly become an important pathogen in patients with immunocompromised status and in patients with chronic pulmonary diseases.Citation7 The aim of this study is to determine the prevalence of M. catarrhalis in our setup in patients presenting with the diagnosis of community-acquired lower respiratory tract infection and to determine the pattern of antibiotic sensitivity and resistance in these cases.
Method
This was an observational study conducted in the Department of Chest Medicine of Liaquat National Hospital and Medical College from March 2012 to December 2012. Approval was obtained from the hospital administration to conduct this study. Patients aged between 20 years and 80 years with the diagnosis of community-acquired lower respiratory tract infection were included in the study. Microsoft Excel 2007 was used to analyze the data.
The inclusion criteria were patients aged between 20 years and 80 years; those with productive cough; those with positive infective markers such as high white blood cell count, fever, or high C-reactive protein (CRP); and those with cultures positive for M. catarrhalis in their respiratory sample collected on admission. The results reviewed were from inpatient records only. The exclusion criteria were patients referred from periphery hospital where they have spent 48 hours or more with a suspicion of hospital-acquired lower respiratory tract infection. It was mandatory to acquire at least three consecutive samples of sputum to rule out the commensal organisms. Patients with positive culture in less than two samples or with cultures positive for organisms other than or in addition to M. catarrhalis were excluded from the study.
A total of 36 sputum samples were evaluated, three from each patient, and after determining the true pathogen, only one sample from each patient was considered for the study giving us a total of twelve sputum samples. In addition three samples of bronchoalveolar lavage and seven samples of tracheal secretions were also evaluated. Purulent parts of the samples were examined and stained with gram stain. Number of epithelial and pus cells were noted along with Gram reaction, morphology, and arrangement of the predominant organism. Respiratory samples were then inoculated on simple mannitol salt agar (MSA), blood agar, and chocolate agar at 37°C for 18–24 hours. Isolates were identified for M. catarrhalis on the basis of various biochemical tests, including gram staining, oxidase test, catalase test, and butyrate esterase production, and their inability to ferment sugars. Antibiotic susceptibility was determined by Kirby–Bauer disk diffusion method. Mueller–Hinton agar was used for susceptibility testing, and the results were concluded as the organism is either susceptible or resistant to antibiotics. As Pakistan is a developing country, cost is a big issue in health care. Quantitative cultures were not performed for the BAL or tracheal secretions. Also, no specific test was performed to assess beta-lactamase production in the isolates. To differentiate between actual pathogen and colonization infective markers, chest X-ray (CXR) changes and clinical assessment were also taken into account.
Results
There were total 110 patients with diagnosis of community-acquired lower respiratory tract infection. Out of them, 22 patients had culture positive for M. catarrhalis. Of these 22, 14 were males and eight were females. The age distribution is listed in . The mean age of patients was 46.77 years with a range of 20–80 years.
Table 1 Sex-wise age distribution among patients
The isolates were 12 sputum samples, three BAL, and seven tracheal secretions.
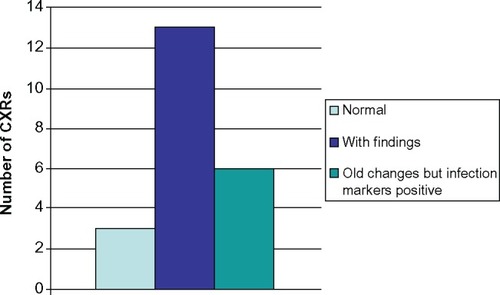
Out of 22 patients, three patients presented with normal CXR and six patients had old changes in their CXR but had a history of productive cough and had positive infective markers. The remaining 13 patients had positive findings on their CXR. The CXR findings are shown in .
Five patients were admitted in the intensive care unit (ICU), two patients in high dependency unit (HDU), and the rest of the 15 patients in ward.
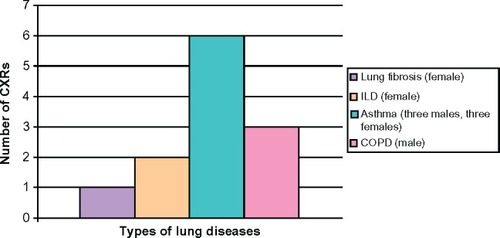
Out of 22 patients, six patients had no known comorbidities and were between the ages of 25 years and 42 years and six patients only had asthma and presented with acute exacerbation with ages between 25 years and 55 years. There were three patients with the ages of 42 years, 62 years, and 68 years presenting acute exacerbation of chronic obstructive pulmonary disease (COPD), two patients previously diagnosed with interstitial lung disease, and one patient with lung fibrosis as shown in . Other comorbidities of patients include diabetes, hypertension, and ischemic heart disease in one, five, and nine patients, respectively.
Figure 2 Distribution of lung etiologies in patients.
Abbreviations: CXRs, chest X-rays; ILD, interstitial lung disease; COPD, chronic obstructive pulmonary disease.
Regarding sensitivity patterns, M. catarrhalis was found to be sensitive to amoxicillin in 21 patients and ampicillin in eight patients as shown in , whereas it was 100% sensitive to ceftriaxone and 96% to cefuroxime. However, in terms of resistance patterns of M. catarrhalis, it was observed that it was resistant to ampicillin in 14 patients; clarithromycin in ten patients, out of which four patients were also resistant to erythromycin; and co-trimoxazole in 13 patients as shown in .
Table 2 Sensitivity and resistance pattern with resistance %
Discussion
Global increase in prevalence of M. catarrhalis has drawn our attention to this commensal of upper respiratory tract as an important cause of lower respiratory infections for last 20–30 years.Citation8 A study done in Pakistan by Abdullah et al in 2013 to evaluate the prevalence of M. catarrhalis in Karachi city showed that out of 776 sputum cultures from Essa laboratories, 39 were positive for M. catarrhalis, which is 5%. Majority of the samples were from young individuals.Citation9 This study was based on patients being treated as outpatients, whereas our study was only from the in-patient data of the chest department of a tertiary care hospital, where the prevalence is 20%. This requires a larger study design to evaluate the true prevalence. This also defines that the majority of patients with M. catarrhalis infection require hospital admission, which can again be confirmed with a larger study design collecting data from all the hospitals in Karachi, Pakistan. Another study done in Rawalpindi, Pakistan, by Butt et al in 2005 showed 12% prevalence of M. catarrhalis in patients with pneumonia.Citation10
Most important factor being considered is the increase in production of beta-lactamase in M. catarrhalis. Studies done in the United States and Canada reported beta-lactamase production in M. catarrhalis to be in excess of 90%,Citation11–Citation13 thus explaining the increasing resistance. A European study done in 2002 showed that 98% of specimens produced beta-lactamase.Citation14 Most of the M. catarrhalis isolates in our study were resistant to ampicillin (63%), presumably due to the increase in beta-lactamase production. A study done in a single hospital over a period of 10 years from 1984 to 1994 suggested that an increase in the minimum inhibitory concentration of antibiotics was not due to the increased frequency of beta-lactamase-producing strains but rather occurred mainly within the beta-lactamase positive strains.Citation15 However, the resistance in our study was still low for amoxicillin–clavulanate (4%), ceftriaxone (0%), and cefuroxime (4%).
Recent studies also highlight the role of M. catarrhalis in the etiology of exacerbation of chronic respiratory diseases.Citation16–Citation18 In a study done in People’s Republic of China, 7% of patients with acute exacerbation of COPD had M. catarrhalis infection.Citation19 Another study done by Domenech et al in Spain evaluating the infectious etiology of severe COPD patients found M. catarrhalis to be the cause in 15.4%.Citation20 In our study, 13% of the patients presented with exacerbation of COPD, 31% with acute exacerbation of asthma in which 50% had a chronic history of asthma since childhood, 9% had interstitial lung disease, and only 4% had lung fibrosis.
M. catarrhalis patterns of sensitivity and resistance need continuous surveillance. A study done in Taiwan to compare the data between 1993–1994 and 2001–2004 revealed an increase in minimum inhibitory concentration for cefaclor, cefuroxime, tetracycline, and co-trimoxazole, hence indicating increase in resistance over the years.Citation21 A study done in Pakistan in 2002 by Tabassum and Ahmed determining the antibiotic susceptibilities showed 75% sensitivity to macrolides (clarithromycin and erythromycin) and 95% sensitivity to quinolones (ciprofloxacin),Citation22 whereas in our study sensitivity to clarithromycin and erythromycin has dropped to 45% and that for quinolone to 41%. These differences also raise the need to conduct larger study for surveillance of the resistance pattern of M. catarrhalis in our region.
Another important factor to be considered is the pathogenicity of M. catarrhalis. In our study, 22% of patients required ICU admission and 9% were admitted in HDU. By comparing our data with another study done in Karachi from a major laboratory based on outpatient population infected with M. catarrhalis,Citation9 our study being done in a single department of a tertiary care hospital has similar numbers, we may conclude that most of the patient requires hospital admission. Less than 10%–30% of patients developing pneumonia with M. catarrhalis are believed to develop bacteremia,Citation23 thus raising concerns about immunocompromised patients who develop lower respiratory infection with M. catarrhalis. Sugiyama et al reported a case of a 75-year-old female in Japan in 2000 who was immunocompromised due to agammaglobulinemia and was being treated at the hospital for acute pneumonia. Sputum culture grew M. catarrhalis as well as Pseudomonas aeruginosa; both were sensitive to imipenem, which was started immediately. Later, she developed infection of methicillin-resistant Staphylococcus aureus; despite continuous efforts, she failed to recover and died. On her autopsy, multiple lung abscesses of varying degrees were discovered indicating recurrent lung infections.Citation24
Some studies suggest prescribing newer macrolides and quinolones as a second-line therapy for M. catarrhalis.Citation25 Swanson et al compared the efficacy of 3 days treatment with azithromycin 500 mg once daily with the 10 days treatment of clarithromycin 500 mg twice daily in patients with chronic bronchitis, and found similar results.Citation26 However, another study done on a smaller scale evaluating the pharmacokinetics and pharmacodynamics of moxifloxacin in community-acquired pneumonia concluded moxifloxacin to have excellent efficacy in treating patients with community-acquired pneumonia.Citation27 But the resistance pattern of M. catarrhalis for these two drugs is yet to be evaluated.
In our study, we saw that the patients presenting with pneumonia were mostly males. Comorbidities in majority of patients were chronic respiratory illnesses. The prevalence of M. catarrhalis is increasing in our community. More patients infected with M. catarrhalis require hospital admission rather than outpatient treatment.
When we observe the sensitivity and resistance pattern, the highest resistance was already anticipated for ampicillin, but observing resistance with similar percentage to clarithromycin and levofloxacin is alarming. Sanford guide for antimicrobials suggests clarithromycin and flouroquinolones as a second-line drug for M. catarrhalis and clarithromycin as the first choice of therapy in patients with comorbidities presenting with community-acquired lower respiratory tract infection.Citation28 Perhaps, we should consider newer macrolides (azithromycin) and quinolones (moxifloxacin) for the second-line treatment of M. catarrhalis, in view of increasing resistance patterns. Keeping in mind the increasing prevalence of patients being infected with M. catarrhalis in our region, a larger scale research should be conducted to evaluate resistance pattern of M. catarrhalis, and with more definite results, we need to review the drug susceptibility in our region, hence, prescribing the more sensitive drug at an earlier phase of infection and improving the outcome of our patients.
Acknowledgments
Dr Safia Bader Uddin Shaikh would like to make the following statement: I am grateful to my parents and siblings who have always been there encouraging me through my toughest moments.
I would like to express my deepest appreciation to all those who provided me with their help and support to complete my research, especially my supervisor Dr Zafar Ahmed and my HOD (head of the department) Dr Syed Ali Arsalan. Also I thank Dr Aneel Chauhan for his guidance, and last but not the least, Mr Waqar Ahmed who would always make time in his busiest schedule. I would also like to thank the HOD of microbiology department Dr Saba Qaiser for letting me review the records.
Disclosure
The authors report no conflicts of interest in this work.
References
- JhonsonMADrewWLRobertsMBranhamella (Neisseria) catarrhalis – a lower respiratory tract pathogen?J Clin Microbiol198113106610697251828
- AebiCMoraxella catarrhalis – pathogen or commensal?Adv Exp Med Biol201169710711621120723
- BrooksGFCarrollKCButelJSMorseSAMietznerTAChapter 16. Pseudomonas, acinetobacter, and uncommon gram-negative bacteriaJawetz, Melnick, and Adelberg’s Medical Microbiology26 ed.2013 Available from: http://www.accessmedicine.com/content.aspx?aID=57032597Accessed November 17, 2013
- SyMGRobinsonJLCommunity-acquired Moraxella catarrhalis pneumonia in previously healthy childrenPediatr Pulmonol20104567467820575092
- WallaceRJJrSteingrubeVANashDRBRO beta lactamases of Branhamella catarrhalis and Moraxella subgenus Moraxella, including evidence for chromosomal beta lactamases transfer by conjugation in B. catrarrhalis, M. nonliquefaciens, and M. lacunataAntimicrob Agents Chemother199833184518542514622
- KhanMANorthwoodJBLevyFBRO beta lactamases and antibiotic resistances in a global cross sectional study of Moraxella catarrhalis from children and adultsJ Antimicrob Chemother201065919719889789
- WrightPWWallaceRJJrShepherdJRA descriptive study of 42 cases of Branhamella catarrhalis pneumoniaAm J Med1990885A2S8S2111088
- TamangMDDeySMakajuRKJhaBKShivanandaPGBhramadatanKNPrevalence of Moraxella catarrhalis infections of the lower respiratory tract in elderly patientsKathmandu Univ Med J2005393944
- AbdullahFEAhjuaKRKumarHPrevalence and emerging resistance of Moraxella catarrhalis in lower respiratory tract infection in KarachiJ Pak Med Assoc201363111342134424392515
- ButtTRafiNAhmedSAhmedRNSalmanMMirzaSHCommunity acquired pneumonia in RawalpindiPak J Pathol200516614
- DorenGVJonesRNPfallerMAKuglerKThe Sentry Participant GroupHemophilis influenza and Moraxella catarrhalis from patients with community acquired respiratory tract infections: antimicrobial susceptibility patterns from SENTRY antimicrobials surveillance program (United States and Canada, 1997)Antimicrob Agents Chemother1999433853899925540
- JonesRNJacobsMRWashingtonJAPfallerMAA 1994–1995 survey of Hemophilus influenza susceptibility to ten orally administered agents. A 187 clinical laboratory center sample in the United StatesDiagn Microbiol Infect Dis19972775839147008
- DorenGVBrueggemannABPierceGHolleyHPRauchAPrevalence of antimicrobial resistance among 723 out patient clinical isolates of Moraxella catarrhalis in the United States in 1994 and 1995: results of a 30 center national surveillance studyAntimicrob Agents Chemother199640288428869124860
- SchmitzFJBeeckAPerdikouliMProduction of BRO beta lactamases and resistance to complement in European Moraxella isolatesJ Clin Microbiol2002401546154811923393
- WalkerESPrestonRAPostJCEhriicGDKalbfleischJHKingmanKLGenetic diversity among strains of Moraxella catarrhalis: analysis using multiple DNA probes and a single locus PCR restriction fragment length polymorphism methodJ Clin Microbiol199838197719839650948
- HunterMHKingDECOPD: management of acute exacerbations and chronic stable diseaseAm Fam Physician200164460361211529259
- LiebermanDLiebermanDBen-YaakovMInfectious etiologies in acute exacerbation of COPDDiagn Microbiol Infect Dis20014039510211502375
- SethiSMurphyTFBacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art reviewClin Microbiol Rev200114233636311292642
- YEFHeLXCaiBQSpectrum and antimicrobial resistance of common pathogenic bacteria isolated from patients with acute exacerbation of chronic obstructive pulmonary disease in mainland of ChinaChin Med J2013126122207221423786927
- DomenechAPuigCMartíSInfectious etiology of acute exacerbations in severe COPD patientsJ Infect20136751652324055804
- HsuSFLinYTChenTLAntimicrobial resistance of Moraxella catarrhalis isolates in TaiwanJ Microbiol Immunol Infect20124513414022154675
- TabassumNAhmedADetermination of anti-microbial susceptibilities of H. Influenza, S. pneumonia and M. catarrhalisJ Pak Med Assoc200252879012073719
- LevisonMEPneumonia including necrotizing pulmonary infections (lung abscess)FauciASBraunwaldEIsselbacherKJWilsonJDMartinJBKasperDLHarrison’s Principles of Internal Medicine14th edNew YorkMc Graw Hill199814371445
- SugiyamaHOgataEShimamotoYMoraxella catarrhalis pneumonia in a patient with immunoglobulin deficiencyJ Infect Chemother20006616211810533
- BandakSITurnakMRAllenBSAntibiotic susceptibilities among recent clinical isolates of H. influenzae and Moraxella catarrhalis from fifteen countriesEur J Clin Microbiol Infect Dis200120556011245326
- SwansonRNLainez-VentosillaADe SalvoMCDunneMWAmsdenGWOnce daily azithromycin for 3 days compared with clarithromycin for 10 days for acute exacerbation of chronic bronchitis: multicenter, double-blind, randomized studyTreat Respir Med200541313915725048
- YoshidaKOkimotoNKishimotoMEfficacy and safety of moxifloxacin for community acquired bacterial pneumonia based on pharmacokinetic analysisJ Infect Chemother201117567868521847518
- GilbertDNMoelleringRCJrChambersHFSaagMSThe Sanford Guide to Antimicrobial Therapy43 edSperryvilleAntimicrobial Therapy Inc2013