Abstract
Background
Cardiovascular disease (CVD) is the main cause of death among hemodialysis (HD) patients. The effects of the dipeptidyl peptidase-4 inhibitor teneligliptin on CVD-related biomarkers in patients with type 2 diabetes mellitus (T2DM) receiving HD treatment are poorly understood. To determine whether teneligliptin has anti-CVD properties, we assessed its effects on soluble P-selectin (sP-selectin), platelet-derived microparticles (PDMPs), plasminogen activator inhibitor 1 (PAI-1), soluble E-selectin (sE-selectin), soluble vascular adhesion molecule 1 (sVCAM-1), and adiponectin plasma levels in HD and non-HD patients with T2DM.
Methods
Patients with T2DM eligible for teneligliptin monotherapy or combination therapy (eg, teneligliptin plus a sulfonylurea) were administered teneligliptin (20 mg/d) once daily for 6 months. Plasma levels of sP-selectin, PDMPs, PAI-1, sE-selectin, sVCAM-1, and adiponectin were measured by enzyme-linked immunosorbent assay at baseline and after 3 months and 6 months of treatment.
Results
Teneligliptin therapy significantly reduced plasma levels of sP-selectin, PDMPs, and PAI-1 compared with baseline levels, while significantly increasing adiponectin levels. sE-selectin and sVCAM-1 levels were significantly decreased only at 6 months. The reduction in sP-selectin, PDMPs, and PAI-1 was more significant in HD patients than in non-HD patients. However, the improvement in adiponectin levels was unchanged with HD treatment.
Conclusion
By modulating PDMPs or PAI-1, teneligliptin shows an antiatherothrombotic effect that may be beneficial in the primary prevention of CVD in patients with T2DM on HD.
Introduction
Historically, older patients have often been excluded from hemodialysis (HD) treatment. However, this changed dramatically in the last decade as a result of increased patient longevity and technical advances in HD therapies.Citation1 Diabetes is the biggest cause of chronic kidney disease in HD patients, and diabetes treatment is a key factor in the overall survival of these patients.Citation2–Citation5 In addition, cardiovascular disease (CVD) is the main cause of death in HD patients because several factors increase the risk of developing CVD in this patient population.Citation6,Citation7
Patients with type 2 diabetes mellitus (T2DM) typically display hypercoagulability and platelet hyperaggregability, along with increased levels of platelet activation markers.Citation8,Citation9 These changes are associated with an increased risk of cardiovascular events.Citation10,Citation11 Platelet-derived microparticles (PDMPs) are generated by platelet activation and play roles in normal hemostatic responses to vascular injury.Citation12–Citation14 It is thought that PDMPs contribute to thrombin generation and thrombus formation by generating tissue factor.Citation15,Citation16 Therefore, PDMPs may ultimately cause vascular complications in T2DM with the participation of the blood coagulation system.
Diabetes is also characterized by increased expression of cell adhesion molecules and elevation of plasminogen activator inhibitor 1 (PAI-1).Citation17,Citation18 These molecules are associated with vascular complications, along with increased serum levels of soluble P-selectin (sP-selectin), soluble E-selectin (sE-selectin), and soluble vascular adhesion molecule 1 (sVCAM-1) in patients with T2DM.Citation19,Citation20 High levels of PAI-1 have been demonstrated in atherothrombosis as PAI-1 contributes to thrombin generation and thrombus formation by generating tissue factor.Citation21–Citation23 The postprandial increase in blood glucose itself is also now considered a risk factor for the progression of atherosclerosis.Citation24
Adiponectin, the most abundant adipose tissue-specific protein, is exclusively expressed in and secreted by adipose tissue.Citation25 Plasma adiponectin concentrations, which are normally high, have been shown to be reduced in obese individualsCitation25,Citation26 and those with T2DMCitation27 and to be closely related to insulin sensitivity.Citation28 Adiponectin has been shown to stimulate nitric oxide (NO) production in vascular endothelial cells, ameliorating endothelial function.Citation29,Citation30 These observations suggest that the antiatherogenic properties of adiponectin may involve its NO-dependent antiplatelet effects.
Dipeptidyl peptidase-4 (DPP-4) is an enzyme involved in the degradation of the intact (active) incretin hormones, glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide, to their inactive metabolites. GLP-1 and glucose-dependent insulinotropic peptide are released by the intestine into the circulation in response to a meal, and both hormones increase glucose-dependent insulin secretion by inhibiting the degradation of active incretins. Teneligliptin is a DPP-4 inhibitor that increases active incretin concentrations, thereby enhancing their glucoregulatory effects.Citation31–Citation33 Teneligliptin exhibits stronger hydrophobic interactions with the active site of DPP-4, mediated by the “anchor lock domain,” which relates to the residence time of the inhibitor in DPP-4 and its long in vivo duration of action.Citation34 In addition, several clinical trials have shown that teneligliptin improves insulin resistance.Citation35–Citation37 However, the effects of teneligliptin on PDMPs, PAI-1, and adiponectin in patients with T2DM, whether on HD or not, are poorly understood. To determine whether teneligliptin has anti-CVD properties, we assessed its effects on PDMP, PAI-1, and adiponectin concentrations in HD and non-HD patients with T2DM.
Patients and methods
Patients
The study cohort included 103 patients with T2DM, 47 with and 56 without HD (), selected from among those admitted to our hospital between May 2012 and March 2015 for the treatment of hypertension, hyperlipidemia, and diabetes. The study protocol was approved by the institutional review board of Kansai Medical University, and written informed consent was obtained from each patient. Individuals were excluded if they had a history (within 3 months prior to enrollment) of inflammatory, coronary artery, or cerebrovascular disease or if they had clinically detectable hepatic dysfunction (elevated transaminases), infection (fever or an elevated white blood cell count), or malignancy (detected on ultrasound or computed tomography). Of the included patients, 13 were taking aspirin because of a previous cerebral infarction or angina pectoris, 28 were taking angiotensin II receptor blockers, 18 were taking Ca-antagonists, and 56 were taking statins (). The doses of these drugs were not adjusted, and there were no other changes to drug therapy, during this study.
Table 1 Demographic and clinical characteristics of the patients with diabetes with and without hemodialysis
Study design
Patients were eligible for teneligliptin if their diet/exercise therapy had continued unchanged for 3 months. Patients who had used a biguanide (metformin), a sulfonylurea (gliben-clamide or glimepiride), a thiazolidinedione (glitazone), or insulin for 3 months were eligible for combination therapy with that agent plus teneligliptin. Patients were administered teneligliptin (20 mg/d) once daily for 6 months. Clinical and biochemical data were obtained before and 3 months and 6 months after starting teneligliptin treatment.
Measurement of PDMP
PDMP levels were measured twice and mean values were recorded. Furthermore, some basic studies were carried out prior to this assessment using clinical specimens. An enzyme-linked immunosorbent assay (ELISA) kit (Otsuka Pharmaceutical, Tokyo, Japan) was used for PDMP measurements.Citation38
Measurement of soluble molecules and adiponectin
Blood samples from patients and controls under fasting conditions were collected into tubes with or without sodium citrate and allowed to clot at room temperature for a minimum of 1 hour. Citrated plasma or serum, respectively, was isolated by centrifugation at 1,000 × g for 20 minutes at 4°C and stored at −30°C until analyzed. Plasma concentrations of sP-selectin, sE-selectin, sVCAM-1, and PAI-1 were measured using monoclonal antibody-based ELISA kits (Thermo Fisher Scientific, Waltham, MA, USA), and plasma adiponectin was measured with adiponectin ELISA kits (Otsuka Pharmaceuticals Co. Ltd, Tokyo, Japan). The recombinant products and standard solutions provided with each kit were used as positive controls in each assay, and all procedures were performed according to the manufacturers’ instructions.
Statistics
Data were expressed as mean ± standard deviation. Between-group comparisons were analyzed using the Newman–Keuls test and Scheffe’s test. The significance of differences among variables was determined by analysis of variance. P-values <0.05 were considered statistically significant. All analyses were performed using the StatFlex program (version 6; Artech Co., Ltd., Osaka, Japan).
Results
Patients’ demographic and clinical characteristics are shown in . Sex and age were similar in the HD and non-HD groups, except for concentrations (). The levels of body mass index, fasting blood glucose, hemoglobin (Hb) A1c, total cholesterol, and low-density cholesterol were higher in non-HD than in HD patients (). However, high-density cholesterol was lower in non-HD than in HD patients ().
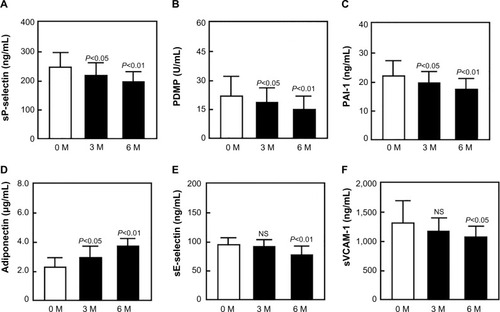
Administration of teneligliptin to 103 patients for 3 months significantly reduced fasting blood glucose and HbA1c levels (data not shown). In addition, both 3-month and 6-month administration significantly reduced plasma concentrations of sP-selectin, PDMPs, and PAI-1, relative to baseline (3 months, P<0.05; 6 months, P<0.01 each; ). Furthermore, teneligliptin treatment significantly increased adiponectin concentrations after 3 months (P<0.05) and 6 months (P<0.01), relative to baseline (). Teneligliptin also decreased sE-selectin and sVCAM-1 concentrations after 6 months, relative to baseline, although the differences were not significant after 3 months ().
Figure 1 Plasma concentrations of sP-selectin (A), PDMP (B), PAI-1 (C), adiponectin (D), sE-selectin (E), and sVCAM-1 (F) before and after teneligliptin treatment of patients with diabetes.
Abbreviations: sP-selectin, soluble P-selectin; PDMP, platelet-derived microparticle; PAI-1, plasminogen activator inhibitor; sE-selectin, soluble E-selectin; sVCAM-1, soluble vascular cell adhesion molecule; 0 M, 0 months (baseline); 3 M, 3 months after treatment; 6 M, 6 months after treatment; NS, not significant; SD, standard deviation.
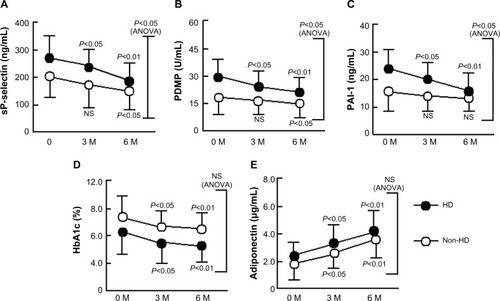
We divided patients with diabetes into two subgroups according to whether they were receiving HD treatment or not. HD patients showed significant reductions in plasma concentrations of sP-selectin, PDMPs, and PAI-1 relative to baseline (P<0.01 for each; ), and all three concentrations were significantly lower in HD than in non-HD after 3 months and 6 months of teneligliptin treatment (two-factor analysis of variance; P<0.05 each). However, there were no significant differences in HbA1c and adiponectin levels between HD and non-HD patients ().
Figure 2 Changes in sP-selectin (A), PDMP (B), PAI-1 (C), HbA1c (D), and adiponectin (E) in response to treatment with teneligliptin of patients with diabetes with and without hemodialysis.
Abbreviations: HbA1c, hemoglobin A1c; sP-selectin, soluble P-selectin; PDMP, platelet-derived microparticle; PAI-1, plasminogen activator inhibitor; HD, hemodialysis; 0 M, 0 months (baseline); 3 M, 3 months after treatment; 6 M, 6 months after treatment; NS, not significant; ANOVA, analysis of variance; SD, standard deviation.
Discussion
Postprandial hyperglycemia is an early manifestation of T2DM and is caused by the loss of early-phase insulin response.Citation39 Postprandial hyperglycemia in patients with diabetes may also be associated with the activation of platelets. In this study, PDMPs, sP-selectin, sE-selectin, sVCAM-1, and PAI-1 were increased in patients with T2DM. These markers decreased significantly with teneligliptin treatment; in particular, PDMPs and PAI-1, which are risk factors for CVD, were significantly decreased in HD patients with T2DM. Treatment with teneligliptin was shown to significantly reduce body mass index and waist circumference,Citation40,Citation41 as well as prevent nephropathic complications in patients with T2DM.Citation42 Thus, our results suggest that teneligliptin may lead to the improvement of atherosclerosis in patients with T2DM with HD by modulating PDMPs and/or PAI-1. Several factors are associated with the development of atherosclerosis in T2DM, one of which is oxidative stress.Citation43 Recently, Kimura et alCitation44 reported that the structure of teneligliptin has a scavenging activity on hydroxyl radical that may contribute to the prevention of diabetic complications, a finding that supports our results.
Plasma concentrations of adiponectin are lower in obese than in nonobese individualsCitation25 and are closely related to whole-body insulin sensitivity.Citation27 Adiponectin levels are also reduced in patients with T2DM.Citation27 Adiponectin has been reported to suppress the attachment of monocytes to endothelial cellsCitation45 and to play a role in protection against vascular injury, suggesting that hypoadiponectinemia is associated with endothelial dysfunction.Citation46 In this study, sE-selectin and sVCAM-1 increased in patients with T2DM, particularly those receiving HD treatment. Furthermore, these biomarkers decreased significantly after teneligliptin treatment. Hypoadiponectinemia has also been associated with platelet activation. Nitric oxide (NO) levels, which regulate platelet activation, are reduced in hypoadiponectinemia because adiponectin stimulates NO production by vascular endothelial cells.Citation29,Citation30,Citation47 Thus, platelet activation due to low NO concentrations occurs in hypoadiponectemic individuals. Therefore, the teneligliptin-induced increase in adiponectin may have an antiplatelet effect by enhancing NO production,Citation48 as demonstrated by the significant reduction in PDMPs and sP-selectin in patients with diabetes treated with teneligliptin.
Various posttranslational modifications, including the glycosylation of lysine residues, have been shown to be necessary for the multimerization of adiponectin.Citation49 These intracellular posttranslational processes may be affected by hyperglycemia, leading to functional impairment at the organ level in patients with diabetes.Citation50–Citation52 Therefore, the teneligliptin-induced improvement in postprandial hyperglycemia may alter the posttranslational modification of adiponectin. Patients in our study received teneligliptin monotherapy or teneligliptin in combination with other antidiabetic dugs. Therefore, it is unknown whether the therapeutic effects of teneligliptin observed in this study were related to monotherapy or not. However, Ito et alCitation36 reported that teneligliptin monotherapy improved homeostasis model assessment of insulin resistance.
The exact mechanism by which teneligliptin treatment increases circulating adiponectin concentrations remains unclear, although the gut-derived incretin hormone GLP-1 is likely involved. GLP-1 is rapidly degraded by DPP-4; therefore, teneligliptin treatment increases plasma concentrations of active GLP-1.Citation31 GLP-1-based therapies have been shown to reduce glucose concentrations and exert antiobesity effects in patients with T2DM.Citation53 Teneligliptin was found to enhance the secretion of active GLP-1, suggesting that the antidiabetic properties of teneligliptin depend, in part, on GLP-1.Citation54 In addition, GLP-1 was shown to promote adiponectin secretion,Citation55,Citation56 resulting in enhanced NO production.Citation48 Therefore, teneligliptin may inhibit the progression of atherothrombosis by promoting adiponectin- and NO-dependent reductions in plasma PDMPs, sP-selectin, sE-selectin, sVCAM-1, and PAI-1. However, further studies are necessary to elucidate the effects of teneligliptin itself on adiponectin production.
Strengths and limitations
This study has two potential strengths. First, despite the treatment of many patients with T2DM with teneligliptin, no previous study had assessed the effects of teneligliptin on serum markers of disease such as PDMP and PAI-1. Second, it showed that investigation of appropriate serum markers can be used to address atherosclerosis in T2DM with HD. However, this study also had several limitations. First, changes in clinical parameters of atherothrombosis such as ankle brachial index were not routinely recorded. Second, we could not identify the causative differences in groups of HD and non-HD. HD patients had poorer serum values at the onset of teneligliptin treatment, suggesting a uremic factor associated with these differences. Third, we could not clarify the significance of PAI-1 and endothelial cell markers relative to atherosclerosis after teneligliptin treatment. Confirmation of these findings in larger and more particular studies would be useful. Finally, we were unable to evaluate the therapeutic effects of teneligliptin using glycated albumin (GA), a parameter used to assess glycemic control in HD patients with T2DM, given that HbA1c underestimates glycemic control in this patient population.Citation57 Recently, Wada et alCitation58 reported that teneligliptin improved GA and HbA1c in patients with T2DM undergoing HD. Therefore, the assessment of GA in teneligliptin-treated patients with T2DM would be beneficial.
Conclusion
Teneligliptin significantly reduced plasma levels of PDMPs and PAI-1 and increased circulating adiponectin concentrations in patients with T2DM, particularly those receiving HD treatment. In addition, teneligliptin treatment reduced sP-selectin, sE-selectin, and sVCAM-1 levels. Teneligliptin may be beneficial in the primary prevention of atherothrombosis in patients with T2DM.Citation59,Citation60 However, larger clinical trials are required to test this hypothesis.
Acknowledgments
This study was partly supported by a grant from the Japan Foundation of Neuropsychiatry and Hematology Research, a Research Grant for Advanced Medical Care from the Ministry of Health and Welfare of Japan, and a grant (13670760 to SN) from the Ministry of Education, Science, and Culture of Japan.
Disclosure
The authors report no conflicts of interest in this work.
References
- MikolasevicILukendaVRackiSMilicSSladoje-MartinovicBOrlicLNonalcoholic fatty liver disease (NAFLD) – a new factor that interplays between inflammation, malnutrition, and atherosclerosis in elderly hemodialysis patientsClin Interv Aging201491295130325143715
- KDOQIKDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney diseaseAm J Kidney Dis200749S12S15417276798
- IshimuraEOkunoSKonoKGlycemic control and survival of diabetic hemodialysis patients – importance of lower hemoglobin A1c levelsDiabetes Res Clin Pract20098332032619135755
- ShimaKKomatsuMKawaharaKMinaguchiJKawashimaSStringent glycaemic control prolongs survival in diabetic patients with end-stage renal disease on haemodialysisNephrology20101563263820883284
- NakamuraYHasegawaHTsujiMDiabetes therapies in hemodialysis patients: dipeptidase-4 inhibitorsWorld J Diabetes2015684084926131325
- VázquezESánchez-PeralesCGarcía-GarcíaFSudden death in incident dialysis patientsAm J Nephrol20143933133624751807
- HarmankayaOAkalinNAkayHComparison of risk factors for cardiovascular disease in hemodialysis and peritoneal dialysis patientsClinics20157060160526375560
- SchaferAIThe hypercoagulable statesAnn Intern Med19851028148283158262
- FradeLJGde la CalleHAlavaINavarroJLCreightonLJGaffneyPJDiabetes mellitus as a hypercoagulable state: its relationship with fibrin fragments and vascular damageThromb Res1987475335403118498
- SeshasalSRKaptogeSThompsonAEmerging Risk Factors CollaborationDiabetes mellitus, fasting glucose, and risk of cause-specific deathN Engl J Med201136482984121366474
- ScheenAJCardiovascular effects of gliptinsNat Rev Cardiol201310738423296071
- NomuraSOzakiYIkedaYFunction and role of microparticles in various clinical settingsThromb Res200812382318667228
- NomuraSShimizuMClinical significance of procoagulant microparticlesJ Intensive Care2015721125705427
- NomuraSMicroparticle and atherothrombotic diseasesJ Atheroscler Thromb2016231926412494
- MiyazakiYNomuraSMiyakeTHigh shear stress can initiate both platelet aggregation and shedding of procoagulant containing microparticlesBlood199688345634648896411
- SinauridzeEIKireevDAPopenkoNYPlatelet microparticle membranes have 50- to 100-fold higher specific procoagulant activity than activated plateletsThromb Haemost20079742543417334510
- CominaciniLPasiniAFGarbinUElevated levels of soluble E-selectin in patients with IDDM and NIDDM: relation to metabolic controlDiabetologia199538112211248591829
- FestaAWilliamsKTracyRPWagenknechtLEHaffnerSMProgression of plasminogen activator inhibitor-1 and fibrinogen levels in relation to incident type 2 diabetesCirculation20061131753175916585388
- LimYCSnappKKansasGSCamphausenRDingHLuscinskasFWImportant contributions of P-selectin glycoprotein ligand-1-mediated secondary capture to human monocyte adhesion to P-selectin, E-selectin, and TNF-α-activated endothelium under flow in vitroJ Immunol1998161250125089725249
- NomuraSShouzuAOmotoSNishikawaMFukuharaSSignificance of chemokines and activated platelets in patients with diabetesClin Exp Immunol200012143744310971508
- ShenGXVascular cell-derived fibrinolytic regulators and atherothrombotic vascular disordersInt J Mol Med199813994089852242
- SobelBETaatjesDJSchneiderDJIntramural plasminogen activator inhibitor type-1 and coronary atherosclerosisArterioscler Thromb Vasc Biol2003231979198912920048
- ZhaoRMaXXieXShenGXInvolvement of NADPH oxidase in oxidized LDL-induced upregulation of heat shock factor-1 and plasminogen activator inhibitor-1 in vascular endothelial cellsAm J Physiol Endocrinol Metab2009297E104E11119401454
- NakagamiTHyperglycaemia and mortality from all cause and from cardiovascular disease in five populations of Asian originDiabetologia20044738539414985967
- OuchiNKiharaSAritaYAdiponectin, an adipocyte- derived plasma protein, inhibits endothelial NF-kappa B signaling through a cAMP-dependent pathwayCirculation20001021296130110982546
- AritaYKiharaSOuchiNParadoxical decrease of an adipose-specific protein, adiponectin, in obesityBiochem Biophys Res Com1999257798310092513
- HottaKFunahashiTAritaYPlasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetes patientsArterioscler Thromb Vasc Biol2000201595159910845877
- WeyerCFunahashiTTanakaSHypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemiaJ Clin Endocrinol Metab2001861930193511344187
- ChenHMontagnaniMFunahashiTShimomuraIQuonMJAdiponectin stimulates production of nitric oxide in vascular endothelial cellsJ Biol Chem2003278450214502612944390
- HattoriYSuzukiMHattoriSKasaiKGlobular adiponectin upregulates nitric oxide production in vascular endothelial cellsDiabetologia2003461543154914551684
- GodaMKadowakiTTeneligliptin for the treatment of type 2 diabetesDrugs Today20134961562924191255
- KishimotoMTeneligliptin: a DPP-4 inhibitor for the treatment of type 2 diabetesDiabetes Metab Syndr Obes2013618719523671395
- MorishitaRNakagamiHTeneligliptin: expectations for its pleiotropic actionExpert Opin Pharmacother20151641742625597385
- NabenoMAkahoshiFKishidaHA comparative study of the binding modes of recently launched dipeptidyl peptidase IV inhibitors in the active siteBiochem Biophys Res Commun201343419119623501107
- KusunokiMSatoDNakamuraTDPP-4 inhibitor teneligliptin improves insulin resistance and serum lipid profile in Japanese patients with type 2 diabetesDrug Res201565532534
- ItoRFukuiTHayashiTTeneligliptin, a dipeptidyl peptidase-4 inhibitor, improves early-phase insulin secretion in drug-naïve patients with type 2 diabetesDrugs R D20151524525126224337
- TsuchimochiWUenoHYamashitaETeneligliptin improves glycemic control with the reduction of postprandial insulin requirement in Japanese diabetic patientsEndocr J201562132025252844
- OsumiKOzekiYSaitoSDevelopment and assessment of enzyme immunoassay for platelet-derived microparticlesThromb Haemost20018532633011246556
- PolonskyKSGivenBDHirschLJAbnormal patterns of insulin secretion in non-insulin-dependent diabetes mellitusN Engl J Med1988318123112393283554
- Fukuda-TsuruSKakimotoTUtsumiHKiuchiSIshiiSThe novel dipeptidyl peptidase-4 inhibitor teneligliptin prevents high-fat diet-induced obesity accompanied with increased energy expenditure in miceEur J Pharmacol201472320721524309217
- NakagamiHPangZShimosatoTThe dipeptidyl peptidase-4 inhibitor teneligliptin improved endothelial dysfunction and insulin resistance in the SHR/NDmcr-cp rat model of metabolic syndromeHypertens Res20143762963524621463
- HalabiAMaatoukHSieglerKEFaisstNLufftVKlauseNPharmacokinetics of teneligliptin in subjects with renal impairmentClin Pharm Drug Dev20132246254
- MatsudaMShimomuraIIncreased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancerObes Res Clin Pract20137e330e34124455761
- KimuraSInoguchiTYamasakiTA novel DPP-4 inhibitor teneligliptin scavenges hydroxyl radicals: in vitro study evaluated by electron spin resonance spectroscopy and in vivo study using DPP-4 deficient ratsMetabolism20166513814526892525
- OuchiNKiharaSAritaYNovel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein, adiponectinCirculation19991002473247610604883
- ShimabukuroMHigaNAsahiTHypoadiponectinemia is closely linked to endothelial dysfunction in manJ Clin Endocrin Metab20038832363240
- NomuraSShouzuAOmotoSCorrelation between adiponectin and reduction of cell adhesion molecules after pitavastatin treatment in hyperlipidemic patients with type 2 diabetes mellitusThromb Res2008122394517920663
- GuptaAKVermaAKKailashiyaJSinghSKKumarNSitagliptin: antiplatelet effect in diabetes and healthy volunteersPlatelets20122356557022950787
- WangYLamKSChanLPost-translational modifications of the four conserved lysine residues within the collagenous domain of adiponectin are required for the formation of its high molecular weight oligomeric complexJ Biol Chem2006281163911640016621799
- FülöpNMarchaseRBChathamJCRole of protein O-linked N-acetyl-glucosamine in mediating cell function and survival in the cardiovascular systemCardiovasc Res20077328829716970929
- FülöpNMasonMMDuttaKImpact of type 2 diabetes and aging on cardiomyocyte function and O-linked N-acetylglucosamine levels in the heartAm J Physiol Cell Physiol2007292C1370C137817135297
- OchiaiHOokaHShidaCIshikawaTInoueDOkazakiRAcarbose treatment increases serum total adiponectin levels in patients with type 2 diabetesEndocrin J200855549556
- KnopFKVilsbøllTLarsenSMadsbadSHolstJJKrarupTNo hypoglycemia after subcutaneous administration of glucagons-like peptide-1 in lean type 2 diabetic patients and in patients with diabetes secondary to chronic pancreatitisDiabet Care20032625812587
- IshibashiYMatsuiTTakeuchiMYamagishiSSitagliptin augments protective effects of GLP-1 against advanced glycation end product receptor axis in endothelial cellsHorm Metab Res20114373173421932180
- PocaiACarringtonPEAdamsJRGlucagon-like peptide 1/glucagons receptor dual agonism reverses obesity in miceDiabetes2009582258226619602537
- Kim Chung leTHosakaTYoshidaMExendin-4, a GLP-1 receptor agonist, directly induces adiponectin expression through protein kinase A pathway and prevents inflammatory adipokine expressionBiochem Biophys Res Commun200939061361819850014
- InabaMOkunoSKumedaYOsaka CKD Expert Research GroupGlycated albumin is a better glycemic indicator than glycated hemoglobin values in hemodialysis patients with diabetes: effect of anemia and erythropoietin injectionJ Am Soc Nephrol20071889690317267743
- WadaNMoriKNakagawaCImproved glycemic control with teneligliptin in patients with type 2 diabetes mellitus on hemodialysis: Evaluation by continuous glucose monitoringJ Diabetes Complications20152981310131326298521
- FismanEZTenenbaumAAntidiabetic treatment with gliptins: focus on cardiovascular effects and outcomesCardiovasc Diabetol20151412926415691
- HashikataTYamaoka-TojoMKakizakiRTeneligliptin improves left ventricular diastolic function and endothelial function in patients with diabetesHeart Vessels Epub2015813
